Abstract
Background Socioeconomically deprived women are at greater risk of adverse pregnancy outcomes. Research tends to focus on access of services. Yet access may not equate with the equity of services for women from different socioeconomic backgrounds.
Objectives To determine whether pregnant women’s perceptions of antenatal provision differed in relation to their socioeconomic deprivation ranking (determined by the Scottish Index of Multiple Deprivation 2006).
Design A longitudinal, qualitative study with comparative antenatal case studies between January 2007 and April 2009.
Setting/Participants Cases were primigravida women from ‘least deprived’ (n = 9) and ‘most deprived’ (n = 12) geographical areas within one local authority in Scotland.
Analysis Data were analysed using case study replication analysis.
Results There was little difference in access to antenatal services between the ‘least’ and ‘most’ deprived groups. Perception of care differed in relation to the level of ‘engagement’ (defined using constructs of: language and personalization of care; power and relationships; and health literacy). Engagement was evidenced in most of the ‘least deprived’ cases and almost none of the ‘most deprived’ cases. Specifically, socioeconomically deprived women described less evidence of personal connection to their own care, effective communication and the opportunity for shared decision making.
Conclusion In women from socioeconomically deprived areas, access may be a less useful indicator than engagement when assessing antenatal service quality. As engagement levels may be one method by which to predict and improve health outcomes, a more equitable antenatal service may need to be developed through the early identification of those women at risk of non‐engagement.
Keywords: antenatal care, case study, engagement, health inequalities, health literacy, socioeconomic deprivation
Introduction
Evidence demonstrates health inequalities operating from the earliest point in utero and continuing cumulatively throughout life. 1 , 2 , 3 The result is a cycle of deprivation whereby some women may start pregnancy with poorer health, and babies in utero may start life on a poorer health trajectory. The neonatal impact is reflected in pregnancy outcomes for mothers and babies: socioeconomically deprived women have a higher maternal death rate than socioeconomically affluent women; and a woman living in an area of high deprivation is three times more likely to have a low birth weight baby (<2500 g) than a woman living in an area of low deprivation. 4 , 5 A socioeconomic imbalance has also been evidenced in antenatal care uptake. For example, around 20% of all maternal deaths are attributed to ‘marginalized women’ (such as those from areas of deprivation) who have not accessed ‘adequate antenatal care’. 6 , 7 , 8
In response, the approach has been to ‘target’ antenatal care to those most in need. 4 Intuitively, targeting seems appropriate, but systematic reviews conclude that there has been little good quality evidence regarding how best to incorporate socioeconomic deprivation into the provision of antenatal care. 9 , 10 Policy approaches continue to focus on clinical obstetric risk factors and provide no clear directive around incorporating socioeconomic risk. 11 , 12 , 13 Without an evidence base to underpin socioeconomic targeting, effort has tended to focus on ‘access’ to services. 4 However, access may not relate to the relevancy or equity of antenatal care for women from differing socioeconomic backgrounds. To address this evidence gap, it was necessary to gather baseline evidence that explored the abilities of the current antenatal system to relate to socioeconomic factors. Therefore, the aim of our study was to determine whether pregnant women’s perceptions of current antenatal provision differed according to their socioeconomic deprivation background.
Methodological approach
A qualitative approach contextualized the socioeconomic background of each individual. 14 A multiple ‘two‐tailed’ case study explored the socioeconomic impact at the level of the individual pregnant woman, or case. 15 By using several cases residing in extremes of socioeconomic deprivation, perceptions were compared from each individual case and from two distinct case groups or tails. University and NHS Ethical approval was obtained.
Method
The research was set within one local authority area in West Central Scotland, with a residential population of 172 876 (2001 census). The area comprises several urban conurbations and villages but has only one maternity unit. Potential cases were identified using the Scottish Index of Multiple Deprivation (SIMD). 16 The SIMD measures deprivation as a composite of seven ‘domains’ that any individual or household can experience. These domains include income, health, crime and housing statistics. The index is based on small area statistical geography called datazones. Each datazone represents a population of between 500 and 1000 household residents and is considered sufficiently localized to identify ‘pockets’ of deprivation that may have been missed in previous forms of analyses. 16 The datazones in Scotland are ranked from one (most deprived) to 6505 (least deprived) with the bottom 20% of datazones being considered to be living in relative deprivation.
Within the maternity unit under study, the SIMD allowed identification of those cases residing in the top and bottom 20% datazones. From these datazones, the inclusion criteria was restricted to English speaking primigravidas receiving standard ‘low risk’ antenatal care, aged over sixteen with no known cognitive difficulties. Potential cases were identified from postcode data at each ‘booking’ clinic. Each postcode allowed the provisional allocation into the ‘least deprived’ or ‘most deprived’ case study tail. Following completion of the clinical appointment, potential cases were provided with study information by the researcher and informed that the researcher was independent of the maternity unit under study with no involvement in the provision of their care. With permission, contact details were taken and the researcher contacted women after 48 h to explore their willingness to consent or not.
Sample
The planned sample size was based on the replication expectations of case study analysis – literal replication (similarity between cases) and theoretical replication (contrast between cases). 15 This replication approach allowed for each case to be compared with every other case in the sample set to determine similarities and differences. The aim was to recruit 15 cases from each group and aim for five or six replications from within each tail. Between January 2007 and December 2008, forty women were approached to participate (16 least deprived and 24 most deprived). All agreed to be contacted after 48 h but five subsequently declined to participate and fourteen could not be contacted after 48 h. The recruitment flow is illustrated in Fig. 1. Of the 40 women initially approached, the mean age of the least deprived group indicated they were significantly older (29.5 years) than those in the most deprived group (25.2 years; P = 0.0237). However, there was no significant difference in the mean age of the two groups that actually participated in our research. Thus, younger women from the most deprived target group were less likely to participate in the study. Nine ‘least deprived’ and twelve ‘most deprived’ cases were recruited. This was less than targeted but, over the recruitment period, concurrent data analysis was reflecting the required replication.
Figure 1.
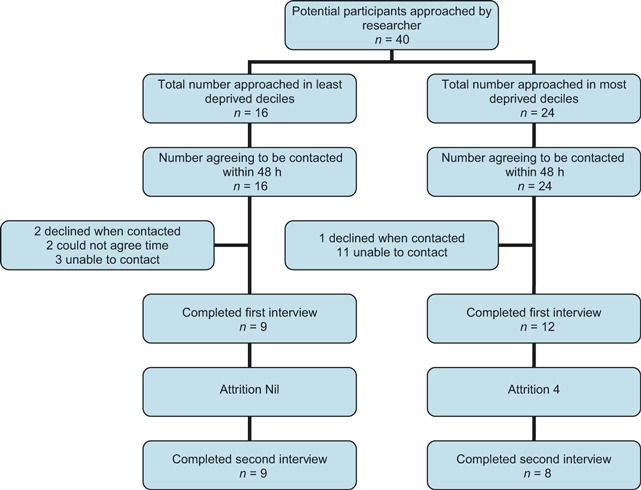
Research recruitment flow.
Data collection
To strengthen the quality of the research, case data were collected from three sources 15 : SIMD information; researcher observation of geographical locality; and two semi‐structured interviews (one in each of the first and third trimesters). The interview schedule was piloted on two antenatal women from a locality bordering the most deprived area, and changes were made to ensure the research questions could be fully addressed. During the study, there was no attrition from the least deprived group; four ‘most deprived’ cases did not participate in the second interview. Demographic variables were collected including gestation at booking, smoking status, marital status, housing tenure, education and employment. These details were used to compile a database and case record. With consent, all interviews were audiotaped and transcribed.
Data analysis
Data analysis was underpinned by a five‐stage strategy facilitated by NVivo7 software. 15 , 17 , 18 Stage one ordered each case according to collated demographic variables. Stage two ordered qualitative data into a priori codes based on key antenatal contacts, and stage three explored this qualitative data within and between case tails. The fourth, inductive, stage of analysis reviewed the concepts emerging from the preliminary stages and developed a theoretical proposition on which to base the final substantive analysis. This substantive fifth stage analysed the relationship between the demographic case variables and the theoretical proposition of engagement. This process is discussed more fully within the results section below.
Results
Case demographics
The demographic characteristics for participants in each tail are illustrated in 1, 2. The women in the least deprived tail were aged from 17 to 40 years. The youngest case in the least deprived tail was largely atypical in that she lived with her parents, did not plan her pregnancy or own her own house. She was also a smoker. The women in the most deprived tail were aged 17–39 years. There was some homogeneity in relation to employment type but none in housing tenure, education level, smoking status or planned pregnancy.
Table 1.
Demographic characteristics of least deprived sample group
| Case | Age | Deprivation decile | Education level | Employment* | Partner employment* | Marital status | Booking gestation (weeks) | Planned pregnancy | Smoking status | Housing tenure |
|---|---|---|---|---|---|---|---|---|---|---|
| LD1 | 30 | 9 | Postgraduate | Associate Professor & Technical | Not Recorded | Married | <10 | Yes | Non | Owner |
| LD2 | 17 | 9 | Standard | Personal Service Occupations | Not Applicable | Single | 10–12 | No | Smoker | With Parents |
| LD3 | 31 | 9 | HNC/HND | Associate Professor & Technical | Professional Occupations | Married | 10–12 | Yes | Non | Owner |
| LD4 | 29 | 9 | Degree | Professional Occupations | Professional Occupations | Married | 10–12 | Yes | Non | Owner |
| LD5 | 31 | 9 | Higher | Professional Occupations | Professional Occupations | Co‐habit | 13–15 | Yes | Non | Owner |
| LD6 | 34 | 10 | Postgraduate | Managers & Senior Officials | Professional Occupations | Married | 13–15 | Yes | Non | Owner |
| LD7 | 26 | 10 | Degree | Professional Occupations | Professional Occupations | Married | 10–12 | Yes | Non | Owner |
| LD8 | 31 | 10 | Degree | Admin & Sec Occupations | Professional Occupations | Married | 10–12 | Yes | Non | Owner |
| LD9 | 40 | 9 | HNC/HND | Admin & Sec Occupations | Professional Occupations | Married | 10–12 | Yes | Non | Owner |
*Based on Registrar General Standard Occupational Classification 2000.
Table 2.
Demographic characteristics of most deprived sample group
| Case | Age | Deprivation decile | Education level | Employment* | Partner employment* | Marital status | Booking gestation (weeks) | Planned pregnancy | Smoking status | Housing tenure |
|---|---|---|---|---|---|---|---|---|---|---|
| MD1 | 20 | 2 | No Qualifications | Process, Plant & Machine Ops | Not Recorded | Co‐habit | 10–12 | Yes | Smoker | Renting |
| MD3 | 36 | 2 | Degree | Admin & Sec Occupations | Professional Occupations | Married | >15 | Yes | Non | Owner |
| MD4 | 30 | 2 | HNC/HND | Admin & Sec Occupations | Personal Service Occupations | Co‐habit | 10–12 | Yes | Non | Owner |
| MD5 | 20 | 1 | HNC/HND | Unemployed | Unemployed | Single | 10–12 | No | Non | Renting |
| MD6 | 30 | 2 | Postgraduate | Professional Occupations | Professional Occupations | Married | 10–12 | Yes | Non | Owner |
| MD7 | 17 | 1 | Standard | Elementary Occupations | Elementary Occupations | Single | 10–12 | No | Smoker | With Parents |
| MD8 | 39 | 1 | Standard | Admin & Sec Occupations | Professional Occupations | Married | 10–12 | Yes | Non | Owner |
| MD9 | 30 | 2 | HNC/HND | Professional Occupations | Professional Occupations | Married | 10–12 | Yes | Non | Owner |
| MD10 | 18 | 1 | Standard | Sales & Customer Services | Unemployed | Single | 10–12 | No | Non | With Parents |
| MD11 | 25 | 1 | Degree | Professional Occupations | Professional Occupations | Married | 10–12 | Yes | Non | Owner |
| MD12 | 22 | 2 | Standard | Unemployed | Student | Married | 10–12 | Yes | Non | Owner |
| MD13 | 29 | 1 | Postgraduate | Sales & Customer Services | Admin & Sec Occupations | Married | 10–12 | No | Non | Owner |
MD2 (allocated but not used).
*Based on Registrar General Standard Occupational Classification 2000.
The case tails differed in terms of employment status. The least deprived tail and their partners had higher status occupations and the potential associated income appeared to be reflected in the deprivation status of their areas of residence. These areas of residence had recorded population differentials in terms of health, environmental, social and economic indicators and strengthened the likelihood that each tail reflected their wider population SIMD ranking. 16 However, between tails, age and educational qualification appeared less differentiated than expected. The age similarity was largely because of the atypically young age of one participant in the least deprived tail and to the lack of younger participation in the most deprived tail. This resulted in a higher than expected age distribution in the most deprived tail and increased the potential for perceptions of care to be more similar between each tail.
All cases accessed antenatal care in a similar manner in that they attended for clinical appointments as requested. However, subtle but discernable differences in language emerged between the case tails in the way that they described their care and experience. To help understand this, literature on discourse analysis was reviewed prior to progressing the analysis. 19 The most notable difference was their perception of care at the end of the first trimester. On one level, cases in both tails spoke in positive terms:
So they’re obviously explaining that about it… Hypnotherapy and things like that, you know the things that were available to you, that’s really interesting so I’ve put my name down for some of that. [Least Deprived (LD) 1]
I think I thought there might have been more happening in the early weeks but I can see why they don’t really. I'll continue to be impressed and quite happy being treated. [Most Deprived (MD) 8]
However, there seemed to be a fundamental difference in the way that cases placed themselves ‘within’ the antenatal system. In the ‘least deprived’ quote above, certain words and phrases, such as ‘really interesting’ and ‘I’ve put my name down’, described a level of involvement extending beyond passive recipient to active participant. Replication of this terminology was noted in several cases in the least deprived group. In contrast, the ‘most deprived’ quote above contained passive terminology and did not seem to represent a woman actively involved in her own care. Replication of this passive approach was noted in several ‘most deprived’ cases:
I don’t really know. I haven’t really thought about it… I don’t know because I don’t really ask a lot of questions when I go to the appointments so. (MD5)
The use of passive terminology led us to consider the possibility that ‘active’ and ‘passive’ may be indicators of how women progress through their antenatal care. As the concepts of activeness and passiveness feature prominently in the literature on engagement, the theoretical proposition was developed that considered ‘engagement’ or ‘non‐engagement’ to be a factor in any perceived differences in care between the case groups. 20 , 21 Thus, the substantive analysis was underpinned by three themes that emerged from a review of the literature on engagement:
Engagement as language and personalization of care
In this theme, language is considered to represent a responsive interaction to the system in which it occurs. In any system, language may not be neutral but constitutive and adaptable. However, the level of adaptability, and thus involvement, may potentially be influenced by perceived constraints within specific systems such as the health‐care system. 19 , 20 , 21 Therefore, we considered that adaptability to the antenatal system may be represented in language used by each case. An analysis of the case data would evidence engagement in terms of understanding their care, perceiving being involved and perceiving a personalized approach (personalization).
Engagement as power and relationships
In this theme, it is considered that the perceived relationship between the care provider and the care receiver underpins engagement. To develop and sustain engagement, health professionals need to recognize prior knowledge and use strategies such as a natural approach, empathy, social conversation and physical touch. 20 , 21 , 22 Therefore, for engagement to be present we sought evidence of a perceived equality in terms of care, the case perceiving a relationship building aspect to the consultations; a feeling of friendly relaxation; or of prior knowledge being recognized.
Engagement as health literacy
In this theme, health literacy is defined as ‘the ability to make sound health decisions in the context of everyday life’ and is considered fundamental to engagement. 23 Health literacy emphasizes an extension beyond basic aspects of literacy to encompass a set of functional and conceptual skills which include the ability to ‘seek out, understand, evaluate and use health information to make informed choices’. 24 Therefore, for engagement to be present we sought evidence of a case perceiving good communication with health professionals, perceiving a value in the quality and relevance of educational information and evidence of shared decision making.
A degree of crosscutting was evident in each theme but the themes were considered sufficiently distinct for literal and theoretical replication analysis within and across case tails.
The findings: language and personalization
In the least deprived tail, six cases presented evidence of engagement at the end of the first trimester. For example,
The midwife had said to me if you’re ever, if there’s anything you’re ever worried about they gave me those two numbers and it was like they really meant it. (LD3)
Of the six ‘engaged’ cases each was comparable in terms of the variables of deprivation status, planned pregnancy, age above 29 years, housing tenure and non‐smoking status. In the least deprived tail, three cases showed no evidence of engagement. Of these, one was under 20 years of age, smoked, did not own her own house, was unmarried, had not planned her pregnancy and had no post‐secondary education. The other two cases were married, non‐smokers, had university level education, planned their pregnancy and owned their own house. One was also aged over 29 years.
Therefore, based on the engaged and non‐engaged case demographics, the variables of deprivation status, education level, housing tenure, age above 29 years, planned pregnancy and marital status did not provide evidence in the least deprived tail that they were influencing factors to support engagement. Three variables – age 26 or under (in terms of LD2 and LD7), smoking status and housing tenure (in terms of LD2) – may have suggested some evidence that they were potentially negative indicators of engagement. However, LD2 was atypical of her case tail in a number of variables and in LD7 there was a further factor that may have acted as a negative influence: prior knowledge. LD7 was a medical professional who had worked within the antenatal service. As such, she would likely have had a higher than average knowledge of both the antenatal system and the process of pregnancy and her perceived needs at the outset were primarily for reassurance. As such both LD2 and LD7 may have had a degree of predictability about their lack of ‘fit’ in a standardized antenatal service.
LD8 was the one case that seemed unique in the least deprived tail. She was similar to the six cases who did engage with the service in terms of age, accommodation, housing tenure and higher educational qualifications. LD8 also presented as talkative. As such there may have been an expectation that this case would engage with the service. However, the data suggested little evidence of engagement and her language and personalization were contradictory from the outset. For example:
Being up at the hospital they were really, really busy you know so I don’t know yea it was good. I mean I didn’t come out any different from when I went in I suppose. (LD8)
There were potential barriers in this case (related to the woman’s perception of poor communication between antenatal staff and poor communication from antenatal staff to the woman herself) that may have prevented engagement in the later stages but these were not present in the first trimester. As such, there was no clear explanation for a lack of engagement in the first trimester.
In the most deprived tail, only one case (MD11) presented evidence for engagement and active involvement at the first trimester: For example, the use of the word ‘my’ is notable as is a level of shared communication:
I got my booklet, my notes and we went through any matters. (MD11)
MD11 was not unique within her tail in the majority of demographic variables. She was not the youngest or eldest; she was university educated as were three other cases; she owned her own house as did seven other cases; she was married as were six other cases; her pregnancy was planned as it was in seven other cases; and she was a non‐smoker as were ten other cases. The only compiled factor that differentiated MD11 from the remainder of the most deprived tail was the fact that she was a health professional; though, she had never worked within the antenatal system other than for a brief period as a student. She was, however, familiar with the hospital involved in this study.
Eleven ‘most deprived’ cases presented no evidence to suggest engagement. Their language and personalization of care tended to suggest a detached, uninvolved experience:
I didn’t really know what was happening about antenatal classes and things like that, what to actually do about that. I can remember them being mentioned at some point but I’m not sure if it’s something I should arrange. (MD13)
In these eleven cases, there was very little homogeneity in the demographic variables. For example, they had different ages, housing tenure, marital status, education level and occupational grouping. The only commonality noted in the collated data was their shared deprivation status based on area of residence.
The findings: power and relationships
In the least deprived tail, only two cases (LD5 and LD6) suggested evidence of engagement in terms of a perceived equality in terms of care provision:
I’m quite a strong enough person to say no this isn’t what I want to do if I didn’t want to do it so. (LD5)
There was a mixed presentation in the data in relation to describing a friendly, relaxed approach. For example, only LD6 described a relaxed approach to antenatal care that was not contradicted by other data:
She was very normal, very down to earth, very practical, she was actually pregnant herself and that was like the first thing she said you know I’m actually pregnant… She was very natural. (LD6)
In the remaining seven cases, there was little evidence of equality in terms of the antenatal process. For example, despite the presence of patient held records, the content of the records was not necessarily seen as a shared process and looking at records was almost viewed as an illicit or hurried act:
You can have a wee quick look through it if you’re wanting. You’re not thinking what are they writing about me and I’m not seeing it. (LD1)
There was also a reported feeling of being afraid to feel stupid in relation to their own care across a number of least deprived cases:
I wish there was a helpline you could just phone, you’re not bothering anybody with really stupid questions. (LD8)
Although the midwives have said that, don’t hesitate to phone even if you think it is a silly thing but I don’t know whether I would. (LD9)
With LD7, the hesitation to contact the midwives may have related more to a perception that the information from medical staff would be more beneficial. This may also have suggested a perceived imbalance in the relationship in terms of equality – only in this example the case may have perceived the greater power (especially in terms of knowledge):
Perhaps anything medical the consultant needs to you know take the time with me rather than [the midwife]. (LD7)
LD8 was again an interesting case within the least deprived tail. She described a positive perception of the midwifery staff at times; however, this did not appear to translate into a positive antenatal experience:
The ladies have been really nice. Everyone I’ve spoke to has been really nice. (LD8)
The woman that we spoke to, she was going on about you know about protein in your urine or whatever and all this stuff and I just didn’t have a clue what you’re talking about. It is all very, I know they must do it all the time. (LD8)
Recognition and acknowledgement of prior knowledge was not evidenced in the data. In two cases, both health professionals, their level of professional knowledge was not considered and this may have had a negative impact:
I know probably they do have certain things that they’ve got to say to you… I mean I’d read about it in the leaflets and things like that and I felt they didn’t need to go on about it quite so much. (LD4)
Each time with the midwives before it kind of works into it that we are health professionals. It’s really incredibly basic. (LD7)
In the most deprived tail, there was only one case that suggested evidence of engagement. This was the same case (MD11) that had evidenced engagement in the previous theme. The remaining eleven ‘most deprived’ cases either evidenced non‐engagement or there was insufficient data to reach a conclusion. In common with the least deprived tail, there was also a perception they might be considered ‘stupid’:
I was not sure what was happening and did not want to seem stupid. (MD5)
The findings: health literacy
In the least deprived tail, three cases did not suggest evidence of engagement. These were the same three cases (LD2, LD7 and LD8) that failed to demonstrate engagement in the first theme of language and personalization. However, the six cases that evidenced engagement under language and personalization also appeared to evidence engagement in terms of health literacy. For example, communication and its connection to decision making were evident:
She told me just about basically the different options of like how to have your baby about whether you wanted consultant led or midwife led and explained the difference between the two… so I kind of made a choice that I was just going to go with midwife led. (LD4)
In the most deprived tail, only MD11, as in the previous themes, suggested any evidence of engagement. Again this was noted in the communication and decision‐making processes:
She just explained the whole process and she offered me the options of the CMU [community midwifery unit] or the Consultant led unit and explained them in detail and just again we talked through any of my anxieties. (MD11)
The remaining eleven cases of the most deprived tail did not present any evidence to suggest engagement at the end of the first trimester. In some cases, there was an overestimation of knowledge and lack of communication:
Sometimes there is quite a lot of jargon and when I go to my appointments you know when I’m being measured and stuff like that and they’re checking for the foetal position and stuff they’re not really back to me, I’ve got to come back and check my notes. (MD 9)
There may also have been a suggestion that some decisions were led by midwifery staff:
The midwives said to me but you’re low risk, you don’t need that and you can have a birthing pool and all this. (MD6)
By the end of the first trimester, across all three themes, engagement may have been more likely in the least deprived tail. Six of nine least deprived cases suggested evidence of engagement. In the most deprived tail, engagement appeared unlikely. Eleven of twelve cases suggested no evidence of engagement across any of the three themes. The one engaged case, MD11, was a health professional familiar with the hospital under study. The analysis of the remaining eleven non‐engaged cases suggested only one collated commonality that was consistent across all eleven cases: their socioeconomic deprivation status based on area of residence.
Engagement in the final trimester
The analysis indicated that within the least deprived tail, there may have been aspects in some ‘engaged’ cases that suggested a weakening of engagement towards the end of pregnancy. This may have related to a greater awareness of their own needs in the later stages of pregnancy and a realization that certain aspects of care were not as personalized as they initially perceived:
I thought maybe they would talk to you more about things like for example in my notes I’ve got like a labour plan and stuff like that and I wonder what stage they would start to talk about this. (LD4)
This weakening of engagement may have also reflected levels of health literacy in this tail such as their prior knowledge and ability to seek out additional information:
Yea well that’s why for some people it would have been useful, but I know myself like what to do if I’ve got constipation or heartburn or stuff like that so for me it probably wasn’t that useful. (LD 4)
However, across both tails, cases who failed to engage by the end of the first trimester never appeared to demonstrate engagement with the antenatal service at any subsequent stage of pregnancy.
In summary, whilst both case tails accessed the antenatal service in almost identical fashion, there was a difference in the way each tail perceived this antenatal care. The difference in perception related to engagement with the results suggests the following:
-
1
Women who reside within areas of low socioeconomic deprivation may be more likely to engage with the antenatal service.
-
2
Women who reside within areas of high socioeconomic deprivation may be less likely to engage with the antenatal service.
-
3
Women who do not engage by the first trimester may not engage at all with the antenatal service.
Discussion
There were limitations in our study. The sample number, although sufficient to attain replications within each tail, was small. This also meant that the sample size of some categorical subsets was particularly small. As such, the findings are treated with some caution. There were a number of recruitment factors. Direct researcher recruitment may have increased the potential for women to feel obliged to participate; though, the delay between contact and consent should have minimized this. The lack of researcher availability at each antenatal clinic lengthened the recruitment period and may also have resulted in eligible cases not having an opportunity to participate. However, throughout the study period the same antenatal protocols were in operation and a similar pattern of care was reported irrespective of recruitment timing.
The SIMD is open to a degree of interpretation and criticism not least because of the inclusion of ‘non‐deprived’ individuals within areas of deprivation rankings. To some extent, this inclusion was evident in our study. However, the SIMD has been shown to be statistically valid and appropriate for targeting resources; it is an improvement on previous indices; and it is an effective measure for identifying concentrated and multiple deprivation. 25 Each datazone is also likely to exhibit substantially more homogeneity in respect of socioeconomic characteristics than larger geography, such as electoral wards. 26 As such, the SIMD is the most robust measure available for determining deprivation status based on readily obtainable information.
A further limitation was that those who declined to participate in the study may have differed from those who participated. There was some evidence of this in that the case tails were more similar than might have been expected. However, this limitation may, paradoxically, strengthen the case tail comparison in that real differences may be greater than presented here. Lastly, attrition occurred between the first and third trimester interviews in the most deprived tail. In the four cases who did not complete the second interview, three were aged twenty or under and only five from the total sample were in this age group. This had the effect of weakening the strength of third trimester evidence from younger participants. However, the findings tentatively suggest that the first trimester may be the important period in terms of initiating and sustaining engagement, and therefore, as the dataset was complete for the first trimester, the results are as robust as they could be for the first trimester findings.
Our study suggests that engagement may be a factor in influencing women’s perceptions of antenatal care. Those who did not engage were more likely to live in socioeconomically deprived areas and, considering access was similar across groups, it appeared that a woman’s level of engagement was unrelated to their access of antenatal care. It is already known that pregnancy outcomes are poorer in those from deprived backgrounds. 4 , 5 What our research adds is that antenatal care, even for those who fully access the service, is perceived poorly by women from socioeconomically deprived areas. The impact of this poorly perceived care on pregnancy outcomes has yet to be researched. However, exploring the aspects underpinning engagement may well be a potentially important strategy for creating more equitable care. Importantly, the findings presented here relate to those women from socioeconomically deprived areas who attended for antenatal care. These women may not have represented the most vulnerable or socially excluded women who are known to make less use of antenatal care.
Specifically, our findings suggested that women residing in socioeconomically deprived areas displayed a greater detachment from antenatal care and had less understanding of the systemic processes. They also perceived that care was not personalized to their individual needs and reported a poor perception of the midwifery approach to care delivery. Overall, patient–professional relationship quality and a confidence imbalance were factors that may help explain non‐engagement. In other antenatal studies, midwives made little effort to explore or accommodate individual needs and women rarely sought clarification on aspects of their care as ‘powerful non‐verbal cues’ from the midwives suggested they had little time. The result was the dissemination of irrelevant information. 27 , 28 , 29 Furthermore, midwives are reported to attain a position of power over women through factors such as language use and controlling access to choices and that they may use words to legitimize their knowledge and understanding as a means of exercising power. 30 , 31 , 32 , 33 It has also been suggested that a disciplinarian approach is more likely when there is a perceived social or cultural difference between patient and professional. 34 , 35
Importantly, in these earlier studies and our own, women with a lower level of education were more likely to report being emotionally dissatisfied. Education, or at least its influence on health literacy, may be a key component in dissatisfaction as there is a suggested relationship between low health literacy and socioeconomic deprivation and between health literacy and engagement. 36 , 37 , 38 , 39 In our study, the health literacy analysis (with one exception), suggested that it was unlikely for participants in the most deprived tail to present any evidence that their communication and interaction with the antenatal service could support engagement particularly in terms of shared decision making. The data suggested there was no attempt made to assess prior knowledge in either case tail and some of the most deprived cases reported their existing knowledge to be overestimated. The relationship between components of health literacy such as prior knowledge and decision making has been noted empirically. Specifically it has been suggested that antenatal decisions may be ‘directed’ to ensure that they comply with local preferred policies or midwife preference and thus knowledge adequate for decision making is not being achieved. 32 , 36 The data in our study support this.
Furthermore, health literacy is now being linked to health outcomes with evidence suggesting that adapting approaches to suit those with low literacy improves health outcomes in chronic disease. 40 , 41 As yet, the importance of health literacy and engagement in antenatal terms (particularly outcomes) has not been researched. However, our study suggests that the current professional antenatal approach, particularly in relation to components of health literacy such as communication, assessment of prior knowledge and decision making, is not adaptive to individual need. Those who may be more affected by this inadaptability are women from lower socioeconomic backgrounds.
We suggest several areas for further research. Attention may need to be directed to potential mechanisms for personalizing care and for approaches that can actively involve women, particularly from lower socioeconomic backgrounds, in their antenatal care. This will include a focus on the potential impact of the clinical relationship and its role in enhancing or limiting engagement in women. Importantly, this should incorporate observing the process of engagement from both midwife and client perspective with a view to determining aspects of care that seem to be impeding engagement at present. There is also an argument for reviewing whether early assessment of health literacy levels can improve subsequent engagement in antenatal care; reviewing whether early and accurate identification of deprivation status increases professional awareness of socioeconomic risk in pregnancy and improves engagement; and establishing whether improvement in antenatal engagement leads to improvement in pregnancy outcomes.
Conclusion
Women residing in the opposite extremes of socioeconomic deprivation accessed the antenatal service in a similar manner but appeared to differ in how they perceived and interacted with the service. Women from higher socioeconomic backgrounds may have been more likely to engage with the antenatal service than women from lower socioeconomic backgrounds. As engagement levels may be one method by which to predict and improve pregnancy outcomes, a more equitable antenatal service may need to be developed through the early identification of those women at risk of non‐engagement. This early identification, in conjunction with an adaptation of care, towards the modifiable aspects of engagement such as the professional approach and the recognition of health literacy levels are key areas for future research.
Conflict of interest
There are no conflicts of interest.
Source of funding
This research was unfunded other than employer funding to complete a Doctor of Nursing Degree.
References
- 1. Barker DJP, Lackland DT. Prenatal influences on stroke mortality in England and Wales. Stroke, 2003; 34: 1598–1603. [DOI] [PubMed] [Google Scholar]
- 2. Kawachi I, Subramanian SV, Almeida‐Filho N. A Glossary for Health Inequalities. Journal of Epidemiology and Community Health, 2002; 56: 647–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hertzman C, Power C. Child development as a determinant of health across the life course. Current Paediatrics, 2004; 14: 438–443. [Google Scholar]
- 4. Royal College of Obstetricians and Gynaecologists . Why Mothers Die: Confidential Enquiry into Maternal and Child Health. London: RCOG Press, 2004. [Google Scholar]
- 5. Information & Statistics Division . Birth & Babies [Online], 2009. Available: http://www.isdscotland.org/isd, accessed 1 February 2009. [Google Scholar]
- 6. Kupek E, Petrou S, Vause S, Maresh M. Clinical, provider and sociodemographic predictors of late initiation of antenatal care in England and Wales. British Journal of Obstetrics and Gynaecology, 2002; 109: 265–274. [DOI] [PubMed] [Google Scholar]
- 7. Petrou S, Kupek E, Vause V, Maresh M. Clinical, provider and sociodemographic determinants of the number of antenatal visits in England and Wales. Social Science and Medicine, 2001; 52: 1123–1134. [DOI] [PubMed] [Google Scholar]
- 8. Downe S, Finlayson K, Walsh D, Lavender T. Weighing up and balancing out: a meta‐synthesis of barriers to antenatal care for marginalised women in high income countries. BJOG: An International Journal of Obstetrics and Gynaecology, 2009; 116: 518–529. [DOI] [PubMed] [Google Scholar]
- 9. Bull J, Mulvihill C, Quigley R. Prevention of Low Birth Weight: Assessing the Effectiveness of Smoking Cessation and Nutritional Interventions. London: Health Development Agency Evidence Briefing, 2003. [Google Scholar]
- 10. Rowe R, Garcia J. Social class, ethnicity and attendance for antenatal care in the United Kingdom: a systematic review. Journal of Public Health Medicine, 2003; 25: 113–119. [DOI] [PubMed] [Google Scholar]
- 11. Scottish Executive . A Framework for Maternity Services in Scotland. Edinburgh: Scottish Executive, 2001. [Google Scholar]
- 12. Expert Group on Acute Maternity Services (EGAMS) . Expert Group on Acute Maternity Services Reference Report. Edinburgh: Scottish Executive Health Department, 2002. [Google Scholar]
- 13. NHS Quality Improvement Scotland . Clinical Standards: Maternity Services. Edinburgh: NHS Quality Improvement Scotland, 2005. [Google Scholar]
- 14. Schwandt TA. Three Epistemological Stances for Qualitative Inquiry In: Denzin NK, Lincoln YS. (eds) Handbook of Qualitative Research. California: Sage, 2000: 189–214. [Google Scholar]
- 15. Yin RK. Case Study Research: Design and Methods, 3rd edn London: Sage, 2003. [Google Scholar]
- 16. Scottish Executive . The Scottish Index of Multiple Deprivation. Edinburgh: Scottish Executive, 2006. [Google Scholar]
- 17. QSR International . Nvivo [online], 2008. Available: http://www.qsrinternational.com/products_nvivo.aspx, accessed 1 September 2008. [Google Scholar]
- 18. Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. London: Sage, 1994. [Google Scholar]
- 19. Coulter A. Engaging Patients in Their Healthcare: How is the UK Doing Relative to Other Countries? Oxford: Picker Institute, 2006. [Google Scholar]
- 20. Coulter A, Ellins J. Patient Focused Interventions: A Review of the Evidence. London: Health Foundation, 2006. [Google Scholar]
- 21. Wetherall M, Taylor S, Yates SJ. (eds). Discourse as Data: A Guide for Analysts. London: Sage, 2001. [Google Scholar]
- 22. Beeber LS, Cooper C, Van Noy BE et al. Flying under the radar: engagement and retention of depressed low income mothers in a mental health programme. Advances in Nursing Science, 2007; 30: 221–234. [DOI] [PubMed] [Google Scholar]
- 23. Kickbusch I. Health literacy: an essential skill for the twenty‐first century. Health Education, 2008; 108: 101–104. [Google Scholar]
- 24. Jochelson K. Health Literacy Review Paper. London: National Social Marketing Centre, 2007. [Google Scholar]
- 25. Bramley G. Scotland’s Index of Multiple Deprivation: assessing its statistical validity, and its appropriateness as a mechanism for targeting resources on deprivation Research Report to the Scottish Parliamentary Corporate Body. Edinburgh: Heriott Watt University, 2005. [Google Scholar]
- 26. Scottish Executive . The Scottish Index of Multiple Deprivation. Edinburgh: Scottish Executive, 2004. [Google Scholar]
- 27. Staniszewska SH, Henderson L. Patient’s evaluations of the quality of care: influencing factors and the importance of engagement. Journal of Advanced Nursing, 2005; 49: 530–537. [DOI] [PubMed] [Google Scholar]
- 28. Hildingsson I, Radestad I. Swedish women’s satisfaction with medical and emotional aspects of antenatal care. Journal of Advanced Nursing, 2005; 52: 239–249. [DOI] [PubMed] [Google Scholar]
- 29. Stapleton H, Kirkham M, Thomas G, Curtis P. Language use in antenatal consultations. British Journal of Midwifery, 2002; 10: 273–277. [Google Scholar]
- 30. Richards N, Coulter A. Is the NHS Becoming More Patient Centred? Trends From the National Surveys of NHS Patients in England 2002–07. London: Picker Institute, 2007. [Google Scholar]
- 31. McKenzie PJ, Oliphant T. Informing evidence: claimsmaking in midwives and clients talk about interventions. Quality Health Research, 2010; 20: 29–41. [DOI] [PubMed] [Google Scholar]
- 32. Furber CM, Thomson AM. The power of language: a secondary analysis of a qualitative study exploring English midwives’ support of mother’s baby feeding practice. Midwifery 2008; 26: 232–240. [DOI] [PubMed] [Google Scholar]
- 33. Svensson J, Barclay L, Cooke M. Antenatal Education as Perceived by Health Professionals. The Journal of Perinatal Education. Winter, 2007; 16: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. McCourt C. Supporting choice and control? Communication and interaction between midwives and women at the antenatal booking visit. Social Science and Medicine, 2006; 62: 1307–1318. [DOI] [PubMed] [Google Scholar]
- 35. Rowe RE, Garcia J, Macfarlane AJ, Davidson LL. Improving communication between health professionals and women in maternity care: a structured review. Health Expectations, 2002; 5: 63–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Green JM, Hewison J, Bekker HL, Bryant LD, Cuckle HS. Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review. Health Technology Assessment, 2004; 8: 33. [DOI] [PubMed] [Google Scholar]
- 37. Parker S, Kupek E, Vause V, Maresh M. Health literacy: a policy challenge for advancing high quality health care. Health Affairs, 2001; 22: 147–152. [DOI] [PubMed] [Google Scholar]
- 38. Andrus MR, Roth MT. Health Literacy: a review. Pharmacotherapy, 2002; 22: 282–302. [DOI] [PubMed] [Google Scholar]
- 39. Sihota S, Lennard L. Health Literacy: Being Able to Make the Most of Health. London: National Consumer Council, 2004. [Google Scholar]
- 40. Nix RL, Bierman KL, McMahon RJ. How attendance and quality of participation affect treatment response to parent management training. Journal of Consulting and Clinical Psychology, 2009; 77: 429–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Schillinger D, Piette J, Grumbach K et al. Closing the loop: physician communication with diabetic patients who have low literacy. Archives of Internal Medicine, 2003; 163: 83–90. [DOI] [PubMed] [Google Scholar]


