Abstract
Objective To study how physicians feel about patients’ efforts to be engaged in shared decision making (SDM).
Study setting and design Survey of physicians from distinctly different medical disciplines (238 psychiatrists and 169 vascular surgeons). Participants were requested to judge which patient behaviours they find helpful and which behaviours detrimental for SDM.
Results Psychiatrists and surgeons had rather positive attitudes about active patient behaviours. However, there were quite a few patient behaviours (e.g. searching the Internet, being assertive towards the doctor) which provoked ambivalent or negative attitudes.
Discussion and conclusions Physicians are generally quite open towards active patient behaviour in the consultation. They, however, do consider it as less helpful and become more annoyed if patients insist on their preferences and doubt their doctors’ recommendations. Physicians must realize that SDM implies giving up decisional power and try to be more flexible in their interactions with patients.
Keywords: doctor–patient communication, patient autonomy, shared decision making
Introduction
Shared decision making (SDM) is increasingly demanded by health‐care leaders, researchers and patients, 1 , 2 , 3 , 4 and there is an increasing body of research on how SDM can be implemented in clinical practice. While it has been argued that both physicians and patients should commit to SDM and engage in a mutual decision process, 5 there has been much more emphasis on the skills and tasks of the physicians 6 and on possibly helpful decision aids 7 than on what patients could do to facilitate SDM. 8
The few studies that focused on patient participation or the patients’ side of SDM primarily deal with the notion of communicative competencies that can facilitate patient participation like asking questions, providing information and verifying it. 9 , 10 , 11 It has been argued that patients need to be more assertive in order to motivate their physicians for a more patient‐centred style. 12
While there is good reason to consider these behaviours as generally helpful for SDM, in daily practice many physicians might have a different view and prefer a more paternalistic style particularly under time constraints or when in doubt about their patients’ decisional capacity. 13 , 14 Under such conditions, a more active participation of patients runs the risk of irritating and annoying doctors instead of facilitating SDM. 15
The aim of this study is to investigate which patient behaviours physicians from two distinctly different medical disciplines (psychiatry, surgery) consider to be helpful for SDM, which behaviours they believe to be helpful for arriving at a medically reasonable decision and which behaviours they are more likely to find annoying (and therefore detrimental to SDM) in clinical routine.
Methods
In order to analyse differences between medical disciplines, we investigated two distinctly different groups of physicians, psychiatrists and vascular surgeons. As previous research suggests, surgeons and psychiatrists are good examples of two very different medical specialties with surgery being more prestigious and considered to be an ‘active’ discipline (‘cutting’, ‘fixing’ and ‘doing’), while psychiatry is generally judged as less prestigious and as a ‘passive’ discipline (‘listening’, ‘talking’ and ‘waiting’). 16 , 17 In vascular surgery for most medical problems, a decision has to be made whether to initiate/continue with medical therapy, or to perform minimally invasive endovascular procedures or open bypass surgery. Frequent decisions in psychiatry involve the decision whether or not to start with drug treatment, to choose the appropriate drug, to initiate psychotherapy or to plan psychosocial matters.
We recruited psychiatrists attending the annual congress of the German Psychiatric Association and vascular surgeons attending the annual meeting of the German Association of Vascular Surgery both held in autumn 2009. Both congresses are major events for specialized clinicians of the respective specialties. The response rate at both congresses was approximately 80%.
The questionnaires included items on participants’ age, gender, length of experience in the medical discipline field and type of institution participants were employed. Participating physicians were asked to indicate which of three styles of physician–patient decision making they were employing most frequently with their patients. These three styles have been identified as paternalistic (‘You inform your patients about the most important treatment options and then try to convince the patients to accept the treatment option that you consider to fit the patient’s needs best’), SDM (‘You inform your patients about the pros and cons of the most important treatment options. Then you encourage the patients to develop preferences upon which you and your patient develop a joint decision’) and informed choice (‘You inform your patients about the pros and cons of the most important treatment options. Then you encourage the patients to develop preferences and strictly aim at implementing them’). 18
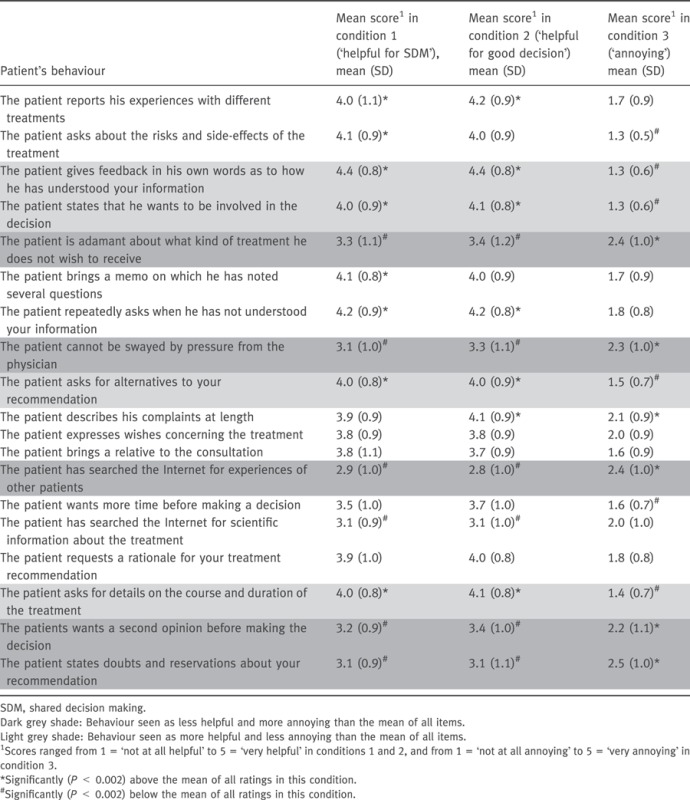
Physicians were asked to imagine an outpatient for whom a decision about his further treatment is to be made and to rate 19 possible behaviours of this patient (Table 2).
Table 2.
Patient’s behaviours seen as helpful or annoying
Participants of the study randomly received one of three questionnaires (experimental conditions).
-
1
Condition 1: physicians were asked to rate whether the patient’s behaviour would be helpful for reaching a shared decision with the patient
-
2
Condition 2: physicians were asked to rate whether the patient’s behaviour would be helpful for reaching a medically‘good’decision (style of decision making not mentioned).
-
3
Condition 3: physicians were asked to rate whether the patient’s behaviour could be seen as ‘annoying’ in clinical practice.
The 19 items (e.g. ‘the patient asks about risks and side‐effects of the treatment’) had to be rated on 5‐point scales ranging from 1 = ‘not at all helpful’ to 5 = ‘very helpful’ in conditions 1 and 2, and from 1 = ‘not at all annoying’ to 5 = ‘very annoying’ in condition 3.
The 19 items were obtained by searching the literature on SDM (e.g. 5 , 8 ) and on related fields (e.g. 9 , 10 ). A preliminary list of items was presented to five psychiatrists and five vascular surgeons with regard to wording and clinical relevance and was subsequently refined.
Statistical analysis
Doctors’ characteristics and ratings were described using frequencies and means. Differences in physicians’ characteristics were analysed using chi‐square‐tests and t‐tests. Mean ratings in the three conditions were calculated by adding the ratings of all 19 items and dividing them by 19 (Crohnbach’s α was >0.88 for all three conditions).
The ratings of the 19 items were compared between physician groups (psychiatrists vs. vascular surgeons) using t‐test for independent samples.
To evaluate whether single items’ ratings differed from the mean of all ratings (i.e. to test whether physicians rated any items as ‘outstanding’), we compared the single item ratings to the mean ratings of the three conditions using one‐sample t‐tests. For these two analyses, we carried out a Bonferoni‐adjustment for multiple testing (P < 0.002).
To test whether the physician’s preferred decision style (paternalistic, SDM, informed choice) correlated with how helpful/annoying the doctors perceived the patient’s behaviours, we compared the mean scores in the three conditions between the three decision styles by using an analysis of variance.
Results
Overall, N = 169 vascular surgeons and N = 238 psychiatrists participated in the study. Psychiatrists had slightly less work experience, were more likely to work in private practices and there were more female doctors in the psychiatrists’ group (Table 1). In addition, there was a trend for psychiatrists to be less paternalistic than vascular surgeons.
Table 1.
Characteristics of the participants
| Psychiatrists (n = 238) | Vascular surgeons (n = 169) | ||
|---|---|---|---|
| Age, mean (SD) | 46.1 (SD = 9.4) | 44.4 (SD = 9.4) | P = 0.08# |
| Gender (female) | 109 (46%) | 40 (27%) | P < 0.001* |
| Work experience, years, mean (SD) | 14.4 (SD = 10.1) | 16.7 (SD = 9.5) | P = 0.03# |
| Workplace (% hospital) | 178 (75%) | 159 (94%) | P < 0.001* |
| Main decision style | P = 0.06* | ||
| Paternalistic | 110 (46%) | 98 (58%) | |
| SDM | 89 (37%) | 53 (31%) | |
| Informed choice | 33 (14%) | 15 (9%) | |
| Experimental condition | P = 0.47* | ||
| Helpful for SDM | 73 (31%) | 58 (34%) | |
| Helpful for good decision | 87 (37%) | 52 (31%) | |
| Annoying | 78 (33%) | 59 (35%) | |
| Mean score in the three conditions (SD) | |||
| Helpful for SDM | 3.7 (SD = 0.6) | 3.7 (SD = 0.5) | P = 0.92# |
| Helpful for good decision | 3.8 (SD = 0.6) | 3.8 (SD = 0.4) | P = 0.94# |
| Annoying | 1.8 (SD = 0.5) | 1.8 (SD = 0.5) | P = 0.96# |
SDM, shared decision making.
# t‐test, *χ2‐test.
Doctors’ ratings of patients’ behaviours
The patients’ behaviours were on average rated as predominantly ‘helpful for arriving at a shared decision’ (condition 1, M = 3.7), as ‘helpful for arriving at a good decision (condition 2, M = 3.8) and as only very little ‘annoying’ (condition 3, M = 1.8).
As can be seen from Table 2, some behaviours were considered more or less helpful or more or less annoying than the mean of all behaviours. Thus, it was seen as especially positive by the physicians (more helpful and less annoying) if the patient gave feedback and stated whether they wanted to be involved in the decision. In addition, asking for alternatives and asking for details of the treatment was also seen as especially positive.
In contrast, physicians regarded it as less helpful and as more annoying if the patient expressed doubts, insisted on his ideas, wanted a second opinion, searched the Internet for other patients’ experiences or if he had resisted pressure from the physician.
Correlation between doctors preferred style of decision making and their ratings of patients’ behaviours
In condition 1 (helpful for SDM), there were no differences between physicians with different decision styles. However, there were significant differences in the two other conditions. Seeing an active patient behaviour as more helpful for reaching good decisions was related to the physicians’ general decision style (higher scores for physicians who generally prefer a less paternalistic style) and an active patient behaviour was seen as more annoying by more paternalistic doctors (Table 3).
Table 3.
Differences with respect to mean ratings of patient behaviour between doctors who indicated that they prefer paternalism, SDM or informed choice (anova)
| Mean (SD) | F | Overall P‐value | Eta | Post hoc (mean difference, P‐value) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Paterna‐listic | SDM | Informed choice | Paternalistic vs. SDM | SDM vs. Informed choice | Paternalistic vs. informed choice | ||||
| Condition 1 (helpful for SDM) | 3.7 (0.6) | 3.7 (0.5) | 3.9 (0.5) | 0.9 | 0.40 | 0.02 | −0.05, 0.90 | −0.16, 0.60 | −0.20, 0.40 |
| Condition 2 (helpful for good decision) | 3.7 (0.5) | 3.9 (0.6) | 4.0 (0.4) | 3.2 | 0.04 | 0.05 | −0.21, 0.10 | −0.11, 0.83 | −0.31, 0.19 |
| Condition 3 (annoying) | 1.9 (0.5) | 1.7 (0.4) | 1.6 (0.3) | 5.6 | 0.005 | 0.08 | 0.20, 0.10 | 0.15, 0.51 | 0.36, 0.01 |
SDM, shared decision making.
Differences between the ratings of psychiatrists and vascular surgeons
Psychiatrists and vascular surgeons did not differ with respect to their mean ratings in the three experimental conditions. Regarding single items, there were only very few significant (P < 0.002) differences between the two groups of physicians:
-
1
In condition 1, psychiatrists found it more helpful for SDM than vascular surgeons if the patient reported his experiences with different treatments.
-
2
In condition 2, again psychiatrists found it more helpful for reaching a good decision than surgeons if the patient reported his experiences, whereas vascular surgeons found it more helpful than psychiatrists when the patient asked for a second opinion.
-
3
In condition 3, vascular surgeons considered it more annoying when the patient expressed specific wishes concerning the treatment and psychiatrists considered it more annoying when the patient asked for a second opinion.
Discussion
Overall, psychiatrists and vascular surgeons were quite positive about an active participation of patients in clinical decision making, whether they were asked particularly about SDM or – more general – about reaching a medically good decision. However, physicians rated some patient behaviours as more annoying or less helpful. Apparently, the categorization of the physicians’ own style of decision making was quite consistent with their ratings of specific patient behaviours.
Limitations
We surveyed doctors attending congresses who might be different from the overall population of German psychiatrists/vascular surgeons, and thus, they might be more interested in innovations and scientific findings. Thus, our sample might be biased by selection.
Additionally, we studied attitudes not behaviour in clinical situations. Physicians might behave differently in clinical practice compared to what they gave as ratings in our questionnaires. Even doctors with a paternalistic style may not admit being annoyed by patients with a given behaviour because it might appear unprofessional (social desirability bias). Physicians might, in their clinical practice, have more expressed reservations about active patient behaviour.
Finally, it is unclear whether our results might also hold true for other medical disciplines. We considered psychiatrists and vascular surgeons as highly distinctive with respect to traditional styles of behaviour. Nevertheless, the differences between the two groups in their ratings were largely negligible.
Overall, psychiatrists and vascular surgeons rated most patient behaviours as helpful for reaching a shared as well as a good decision. Although social desirability might have inflated the positive responses, these results may indicate that physicians from very different fields do not expect to see passive patients, but respect active patient behaviour. Finally, physicians did not differentiate between patient behaviours that are useful for SDM in particular and patient behaviours that help to reach medically (scientifically) sound decisions. The physicians surveyed thus apparently have to a considerable extent incorporated patient‐centred medicine.
Nevertheless, a comparison of individual items showed that doctors, despite being generally open towards patient autonomy, become more annoyed and see it as less helpful if patients disagree with them or insist on what they believe to be best for them. In addition, doctors dislike patients searching the Internet and informing themselves about other patients’ experiences.
Congruent with previous research, 13 , 19 physicians appear to be open to SDM, but not under all circumstances. Thus, if a patient resists a doctor’s recommendation that the doctor believes to be reasonable and in the patient’s best interest, doctors become afflicted by doubts whether a paternalistic decision might not be better in the long‐term interest of the patient.
Here, it becomes clear that a consequent implementation of SDM implies that physicians have to ‘accept that the patient has the right to decide not to take a medicine, even if’ (…the physician does…) ‘not agree with the decision, as long as the patient has the capacity to make an informed decision and has been provided with the information needed to make such a decision’. 4
And for the patients it is important to know that with some behaviours they are more likely to risk annoying their doctors, especially those who still prefer the paternalistic role of doctor–patient interaction. While this is a disappointing finding, it might reflect with what many patients experience when speaking up in the consultation, e.g., by insisting on their preferences or by citing search results from the Internet.
Here, the patients probably should not only speak up for their preferences and rights, but should also address the patient–doctor relationship. Hence, it has been argued that it is also of importance for a successful shared decision‐making process that patients look after the therapeutic alliance, show respect, listen to the doctor and are able to compromise. 5 , 8
While these patient competencies are surely helpful, it should rather be up to the physicians to find ways how to deal with active patient behaviour without getting annoyed. One approach might be physicians becoming more flexible in their interactions with patients. It thus has been suggested that tailoring decision‐making styles (e.g. SDM vs. paternalistic) to the expectancies and preferences of individual patients might improve doctor–patient communication and also treatment outcomes. 20
Finally, we were surprised that there were so few differences between the two physician groups. The few differences found can be explained by specifics of the two disciplines. Thus, it makes more sense to talk about patients’ experiences with different psychotropic medications than to discuss patients’ experiences with different surgical procedures. Likewise surgeons are more used to patients who demand a second opinion than psychiatrists.
Conclusion
Physicians must become aware that SDM implies giving up decisional power. Doctors should also become more flexible in their interaction with patients (e.g. ‘paternalistic’ vs. SDM) and should not misunderstand active patient behaviour (e.g. seeking for information on the Internet, second opinion) as distrust or annoying.
Sources of funding
This study received no funding.
Conflict of interest
None.
References
- 1. Elwyn G, Edwards A, Kinnersley P. Shared decision‐making in primary care: the neglected second half of the consultation. British Journal of General practice, 1999; 49: 477–482. [PMC free article] [PubMed] [Google Scholar]
- 2. Hamann J, Leucht S, Kissling W. Shared decision making in psychiatry. Acta Psychiatrica Scandinavica, 2003; 107: 403–409. [DOI] [PubMed] [Google Scholar]
- 3. Tariman JD, Berry DL, Cochrane B, Doorenbos A, Schepp K. Preferred and actual participation roles during health care decision making in persons with cancer: a systematic review. Annals of Oncology, 2010; 21: 1145–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nunes V, Neilson J, O’Flynn N et al. Clinical Guidelines and Evidence Review for Medicines Adherence: Involving Patients in Decisions about Prescribed Medicines and Supporting Adherence. London: National Collaborating Centre for Primary Care and Royal College of General Practitioners, 2009. [PubMed] [Google Scholar]
- 5. Towle A, Godolphin W. Framework for teaching and learning informed shared decision making. BMJ, 1999; 319: 766–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Elwyn G, Edwards A, Wensing M, Hood K, Atwell C, Grol R. Shared decision making: developing the OPTION scale for measuring patient involvement. Quality and Safety in Health Care, 2003; 12: 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. O’Connor A, Rostom A, Fiset V et al. Decision aids for patients facing health treatment or screening decisions: systematic review. BMJ, 1999; 319: 731–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lown BA, Clark WD, Hanson JL. Mutual influence in shared decision making: a collaborative study of patients and physicians. Health Expectations, 2009; 12: 160–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cegala DJ, McClure L, Marinelli TM, Post DM. The effects of communication skills training on patients’ participation during medical interviews. Patient Education and Counseling, 2000; 41: 209–222. [DOI] [PubMed] [Google Scholar]
- 10. Harrington J, Noble LM, Newman SP. Improving patients’ communication with doctors: a systematic review of intervention studies. Patient Education and Counseling, 2004; 52: 7–16. [DOI] [PubMed] [Google Scholar]
- 11. Kinnersley P, Edwards A, Hood K et al. Interventions before consultations to help patients address their information needs by encouraging question asking: systematic review. BMJ, 2008; 337: a485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cegala DJ, Post DM. The impact of patients’ participation on physicians’ patient‐centered communication. Patient Education and Counseling, 2009; 77: 202–208. [DOI] [PubMed] [Google Scholar]
- 13. Hamann J, Mendel R, Cohen R et al. Psychiatrists’ use of shared decision making in the treatment of schizophrenia: patient characteristics and decision topics. Psychiatric Services, 2009; 60: 1107–1112. [DOI] [PubMed] [Google Scholar]
- 14. Legare F, Ratte S, Gravel K, Graham ID. Barriers and facilitators to implementing shared decision‐making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Education and Counseling, 2008; 73: 526–535. [DOI] [PubMed] [Google Scholar]
- 15. Katz RC. Difficult patients as family physicians perceive them. Psychology Reports, 1996; 79: 539–544. [DOI] [PubMed] [Google Scholar]
- 16. Album D, Westin S. Do diseases have a prestige hierarchy? A survey among physicians and medical students Social Science & Medicine, 2008; 66: 182–188. [DOI] [PubMed] [Google Scholar]
- 17. Hinze SW. Gender and the body of medicine or at least some body parts. The Sociological Quarterly, 1999; 40: 217–239. [Google Scholar]
- 18. Charles C, Gafni A, Whelan T. Shared decision‐making in the medical encounter: what does it mean? (or it takes at least two to tango). Social Science & Medicine, 1997; 44: 681–692. [DOI] [PubMed] [Google Scholar]
- 19. Seale C, Chaplin R, Lelliott P, Quirk A. Sharing decisions in consultations involving anti‐psychotic medication: a qualitative study of psychiatrists’ experiences. Social Science & Medicine, 2006; 62: 2861–2873. [DOI] [PubMed] [Google Scholar]
- 20. Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision‐making and interpersonal behavior: evidence, models and interventions. Patient Education and Counseling, 2006; 61: 319–341. [DOI] [PubMed] [Google Scholar]


