Abstract
Objectives To explore patients’ perceptions regarding prospective telerehabilitation services and the factors that facilitate or impede patients’ intentions to use these services.
Design Using semi‐structured interviews, patients reflected on the pros and cons of various scenarios of prospective telerehabilitation services. Patients’ arguments were first arranged according to the Unified Theory of Acceptance and Use of Technology (UTAUT). Next, using inductive analysis, the data for each UTAUT component were analysed and arranged into subthemes.
Setting and participants Twenty‐five chronic pain patients were selected from a rehabilitation centre in the Netherlands.
Results Overall, participants considered telerehabilitation helpful as a complementary or follow‐up treatment, rather than an autonomous treatment. Arguments mainly related to the UTAUT constructs of ‘performance expectancy’ and ‘facilitating conditions’. Patients valued the benefits such as reduced transportation barriers, flexible exercise hours and the possibility to better integrate skills into daily life. However, many patients feared a loss of treatment motivation and expressed concerns about both reduced fellow sufferer contact and reduced face‐to‐face therapist contact. Few arguments related to ‘social norms’ and ‘effort expectancy’.
Conclusions The effect of telerehabilitation on healthcare strongly depends on patients’ willingness to use. Our study showed that chronic pain patients valued the benefits of telerehabilitation but hesitate to use it as an autonomous treatment. Therefore, future initiatives should maintain traditional care to some degree and focus on patients’ attitudes as well. Either by giving information to increase patients’ confidence in telerehabilitation or by addressing reported drawbacks into the future design of these services. Further quantitative studies are needed to explore patients’ intentions to use telerehabilitation.
Keywords: exercise, home care, patient acceptance of healthcare, technology acceptance, telemedicine, therapy
Introduction
Chronic pain is a common condition that occurs in at least 19% of adult Europeans, and varies from moderate to severe intensity. 1 As well as having personal consequences, chronic pain puts pressure on society as it affects direct healthcare costs as well as indirect costs such as social compensation, pensions and a loss of productivity. 2 , 3 , 4
At present, it is acknowledged that physical exercises should be part of chronic pain treatment. Therapeutic exercises prove beneficial for chronic pain patients as they reduce pain and disability. 5 , 6 , 7 , 8 , 9 Despite the benefits, adherence to the exercise programs is often suboptimal. Dropout rates have ranged from 10 to 36% and many patients’ exercise adherence levels decline even further once they have completed their programme. 10 Geographical and transportation barriers, socio‐ economic factors and financial constraints might be important determinants of this non‐adherence. 11 Therefore, it is important to look for alternative models of health service delivery that could better meet patients’ preferences and, in so doing, enhance exercise treatment compliance.
Home‐based telerehabilitation, providing care at home via communication technologies, 12 is one such alternative model. Telerehabilitation is supposed to have several advantages over traditional care as patients have the opportunity to rehabilitate within their own social environment, 13 can avoid transportation issues, 14 are able to personally adjust exercise hours 15 , 16 , 17 and are encouraged to manage their disease themselves.
Results from empirical effect studies coincide with the idea that telerehabilitation services are beneficial to patients. Brattberg et al. 18 used the internet to provide videofilms for the rehabilitation of people on long‐term sick leave due to chronic pain and/or burnout. Over half of the experimental group reported an increased work capacity, compared with thirteen percent in the control group. In addition, Buhrman et al. 19 showed in their controlled trial that an internet‐based cognitive behavioural intervention with telephone support for chronic back pain patients leads to significant improvements in health.
Despite this, within the field of chronic pain and telerehabilitation, no attention has been given to the patients’ perspective on telerehabilitation services. As patients’ judgements whether the treatment is relevant, meaningful and likely to be successful are linked with their compliance, 20 , 21 it is important to develop interventions that meet patients’ underlying value systems. Therefore, the aim of this study is to explore chronic pain patients’ perceptions of prospective home telerehabilitation services and understanding the factors seen as important from their perspective by means of qualitative interviews.
Method
Setting and sampling
A convenience sample of 25 chronic pain patients was selected from a rehabilitation centre.
The following inclusion criteria were applied: (i) Patients were receiving or had received physical therapy, (ii) patients had sufficient communication skills and a basic knowledge of the Dutch language, and (iii) only adults were asked to participate. The sample included maximum variation, including a balance of men and women, older and younger participants, and patients with and without experience with the traditional rehabilitation program. Interviews took place at the research facilities near the rehabilitation centre. Participants unable to visit the research department were visited at home. Written and verbal consent to participate was obtained from all participants.
Semi‐structured interviews
Interviews were conducted by KC (communication scientist) and ESB (psychologist), lasted between 30 and 90 min, and were guided by a semi‐structured interview guide. The guide explored the perceived advantages and disadvantages of potential exercise‐based telerehabilitation services with a focus on cognitive behavioural treatment and patients’ intention to use these services. Although areas for exploration were defined, the semi‐structured interview allowed for flexibility and deeper examination of issues arising. To facilitate the interview process patients first discussed the pros and cons of their past and current treatments. Patients were then shown cards, providing a brief description and picture of four home‐based treatments, including three prospective telerehabilitation treatments. The scenarios did not represent full and realistic treatments, but each depicted a different functionality of telerehabilitation. The rationale behind this was that this would help patients to gradually become familiar with the broad concept of telerehabilitation. In addition, the scenarios represented telerehabilitation as a total replacement of clinic‐based care. The first and final consultation would take place at the clinic, giving patients face‐to‐face contact with their therapist. This ‘extreme’ proposition was expected to trigger patients’ perceptions of telerehabilitation and to help them to elaborate on the pros and cons.
The functionalities presented were: (i) a home‐based treatment with home visits by a therapist, (ii) a home‐based treatment by means of webcam therapist consultations, (iii) a sensor‐based treatment that made use of a system with incorporated sensors generating feedback about a patient’s movements during exercising, and (iv) a home‐based treatment through the use of a web‐based tailored exercise program with video instruction files. At the end of each interview patients filled out a short personal characteristics questionnaire.
Analysis
Interviews were audio recorded and transcribed verbatim with participants’ permission. First, two coders (KC and ESB) separately read all transcripts to familiarize themselves with the data. Data were then arranged according to a thematic framework based on the Unified Theory of Acceptance and Use of Technology (UTAUT). We used this as it has been proven a robust and parsimonious framework to understand the drivers of user’s intentions to accept ICT. 22 According to UTAUT, ‘performance expectancy’, ‘effort expectancy’, ‘social influence’ and ‘facilitating conditions’ are the key predictors of ICT acceptance.
Next, the data for each UTAUT component were analysed and arranged into subthemes using an inductive process, meaning that patterns, themes and categories arise from the data. 23 Differences were discussed and resolved during discussion meetings. The credibility of the analysis was aided by ongoing discussion with two additional reviewers CHCD (health promotion scientist) and LMAB (health scientist), both having experience with qualitative analysis. To ensure confidentiality, we removed all identifying information from the quotes.
Results
Sample characteristics
Table 1 outlines the characteristics of the research sample which consisted of 25 chronic pain patients of whom thirteen were female patients. Participants ranged in age from 22 to 77 years, with a mean of 40 years. A total of five participants had a high level of formal education, six an intermediate level and fourteen a lower level. Seven participants were single; the remaining eighteen were married or cohabiting. Thirteen patients were unemployed.
Table 1.
Characteristics of the research sample
| Demographics | |
|---|---|
| Gender male (n) | |
| Female | 13 |
| Male | 12 |
| Age (years) | |
| Years (mean ± SD) | 39.8 ± 14.1 |
| Range | 22–77 |
| Education (n) | |
| Low | 14 |
| Middle | 6 |
| High | 5 |
| Marital status (n) | |
| Single | 7 |
| Married/cohabiting | 18 |
| Employment (n) | |
| Employed | 12 |
| Unemployed | 13 |
Interview results
There was much similarity in the characteristics that participants associated with prospective telerehabilitation services, although they differed in the value they attached to these characteristics.
The results are structured according to the constructs: (i) performance expectancy, (ii) effort expectancy (iii) social influence (iv) facilitating conditions and (v) intention to use, all derived from the Unified Theory of Acceptance and Use of Technology. 22 An overview of all themes and subthemes is provided in Fig. 1. The majority of the patients looked at telerehabilitation in the light of performance expectancy and facilitating conditions. Fewer subthemes emerged regarding the constructs of social influence and effort expectancy.
Figure 1.
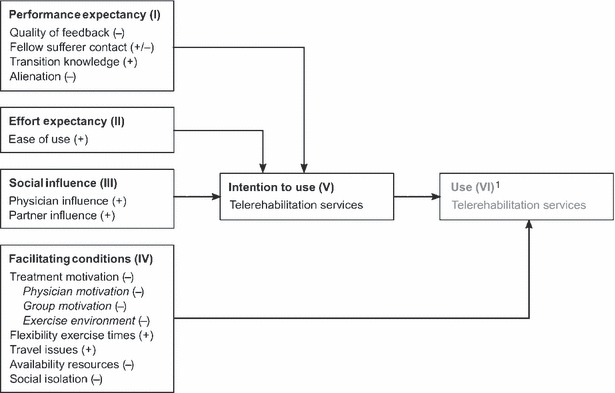
Revealed themes, using the UTAUT as organising structure, relating to patients’ perceptions of prospective home telerehabilitation services (the − and + signs indicate whether these perceptions were negative or positive). ¹The UTAUT construct ‘use’ was not explored during this research.
Performance expectancy (I)
Performance expectancy relates to the degree that a patient believes the use of telerehabilitation would improve his or her health outcome. With regard to all home‐based telerehabilitation scenarios presented, patients perceived the benefit of learning skills outside the clinic. However, a majority of the patients also expressed worries concerning the quality of feedback, the possibility of fellow sufferer contact and the feeling of alienation.
Quality of feedback First, all of the patients were concerned with the quality of feedback provided regarding their movement when exercising at home without their therapist physically present. For all scenarios presented, the majority stressed the importance of receiving feedback from a therapist during each exercise session. Patients felt insecure about their own exercise abilities and were afraid something would go wrong in absence of the face‐to‐face supervision of a therapist. With respect to the web camera scenario a patient mentioned “…Then you’re at home with a video screen and he explains something to you…what if you don’t do it right and you can’t correct yourself, then what?” (female participant, 23). Generally, patients expected their therapist to touch them during therapy. “A physiotherapist just tries to explain to you accurately which muscles you have to tense and also lets you feel it. Via the Internet that is impossible” (female partcipant, 59).
However, feedback by means of touching and feeling did not seem equally important to everyone: “I mean, the therapist doesn’t always have to touch you of course” (male participant, 37). In addition, some patients indicated that their need for physical contact diminished during their treatment as they became more familiar with their exercises. These patients had less concerns about the quality of feedback provided at a distance, as with the web camera consultation scenario; however, their perceptions of the sensor feedback scenario differed greatly. One half of the sample doubted the prospective sensor system could provide correct feedback about their exercise performances. The other half was positive about the sensor system. They thought it could provide even more accurate feedback than a therapist. Nevertheless, most of them still preferred face‐to‐face contact to discuss the feedback. Concerning the web‐based exercise scenario, patients were enthusiastic about the video files used for exercise instructions, but stressed the need for feedback from their therapist during their exercise sessions.
Fellow sufferer contact Some patients perceived all the telerehabilitation scenarios disadvantageous with respect to fellow sufferer contact, as none of the scenarios offered fellow sufferer contact. They considered this contact important for the provision of emotional support during the rehabilitation process: “because…, with a physiotherapist you can open up your heart, but he doesn’t know what you feel, how you feel. And then at home you can, as in my case, tell your mother and your sister, but they don’t really get it” (female participant, 23). In addition, contact with fellow sufferers gave patients the opportunity to share advice: “You learn from each other… you can give each other a bit of advice” (female participant, 55) and to learn from each other by watching and copying during exercise. One male patient (participant, 23) suggested that contact with fellow sufferers could be preserved within telerehabilitation by organizing chat sessions with other patients or by developing a forum. Not every patient, however, appreciated fellow sufferer contact. These patients perceived all telerehabilitation scenarios to be beneficial, with respect to the lack of fellow‐sufferer contact, as they felt they had plenty of problems of their own and had no need to hear other patients’ problems. “All of these people moaning. Some people complain about it a lot, don’t they?” (female participant, 54).
Transition knowledge The majority of the patients perceived the advantage of acquiring the exercise skills at home, outside the rehabilitation setting. For them, all telerehabilitation scenarios would make it easier to integrate exercise as a routine into their daily life. Patients expected this to enhance the effectiveness of their treatment.
Alienation In addition, the majority of the patients commented on the effects of home‐based telerehabilitation on the patient‐therapist relationship. Patients thought the limited face‐to‐face contact with their therapist would limit emotional bonding and subsequently treatment results. They considered pain rehabilitation as both a physical and emotional process. As a consequence, it was important for them to talk to their therapist in person and to share their feelings. Although web camera consultation would enable communication with their therapist, most patients expressed a feeling of alienation when they imagined themselves communicating remotely. “It’s just so… detached” (female participant, 26). Some felt that when communicating via web camera, the therapist might fail to notice emotions as well as new complaints about pain. In addition, others felt it would be more difficult to share feelings with someone by means of a webcam than with in vivo contact. In general, telerehabilitation was associated with an impersonal approach: “I feel that with [the webcam scenario]… you are a bit like a number” (female participant, 26).
Some patients, however, acknowledged their feelings about alienation that could be the result of their unfamiliarity with remote communication systems. “Perhaps it takes getting used to it” (male paticipant, 23). Patients who did not feel the need for an emotional bond with their physiotherapist, pointed out that video communication could work well.
Effort expectancy (II)
Alongside the construct of performance expectancy, patients reflected on themes relating to the UTAUT construct of effort expectancy. This construct is defined as the degree of ease that a patient associates with the use of telerehabilitation. With regard to all telerehabilitation scenarios, most patients expected that the software or equipment would be easy to use or would be designed to be user friendly.
For both the web camera consultation and web‐based exercise scenario, operating the video communication system and the use of internet was considered easy by most patients. Some of them had already experienced this form of communication. One patient expressed reservations about the use of a webcam: “Well, I think that the camera brings about a lot of clumsiness” (male participant, 27). With regard to the sensor‐based scenario, the majority of participants thought that the use of the sensors would not be problematic. One patient mentioned she did not want to spend time learning how to work with technology, “… because I don’t have that much understanding [of technology], I will have to learn it all first. If I have to spend my time on it then I have better things to do regarding my treatment” (female participant, 59).
Social influence (III)
In this study, social influence, the third UTAUT construct, is defined as: patients’ perceptions, whether people that are important to them think that they should choose a certain treatment. These norms are influenced by peers such as family, friends and partners on the one hand, and by professionals on the other hand.
For all home‐based scenarios, participants stated that it would be pleasant for them if their social environment held a positive attitude towards the treatment but that this would not be a deciding factor.
In addition, some participants associated the clinic with professionalism. As a result, they would rely on the advice of the rehabilitation clinic and their therapist: “There is so much knowledge around. You [the rehabilitation clinic] will know better what works best” (female participant, 59).
Facilitating conditions (IV)
Finally, patients reflected on themes relating to the facilitating conditions construct of the UTAUT, which embodies three different constructs of ‘perceived behavioural control, ‘facilitating conditions’ and ‘compatibility’. These constructs capture the user’s perceptions of their ability to perform the behaviour and measure the degree to which the treatment fits with the user’s existing values, previous experiences and current needs. 22
Patients, who did not consider themselves very self‐disciplined in particular, reflected on the construct of perceived behavioural control. For all telerehabilitation scenarios, they expected telerehabilitation to negatively affect their treatment compliance because of reduced motivational stimulus resulting from remote therapist and fellow sufferer contact and training in the home environment. In addition to the perceived internal barrier of motivation, some patients reflected on external barriers (facilitating conditions) as they found resources were lacking, such as exercise space and telerehabilitation equipment. Finally, a majority of the patients perceived benefits such as reduced travel times and flexibility of exercise times, both relating to the compatibility construct. These patients thought telerehabilitation would be more compatible with their needs and way of life, compared to traditional care. On the other hand, some patients reflected negatively on the compatibility construct as they thought telerehabilitation would lead to social isolation.
Treatment motivation The majority of the patients felt that all telerehabilitation scenarios would negatively affect their treatment motivation. Patients reflected on three sources from which they derived motivational stimuli, namely their therapist, fellow sufferers and their exercise environment.
Therapist motivation Some patients considered their therapist as the one who could motivate them at times when they had difficulties with exercising. These participants often stressed the importance of supervision by their therapist: “Well, in my case there must always be someone around, because I feel like… I can’t do it… you know … then I quit” (male participant, 23). Therefore, some patients considered both the web‐based exercise and the sensor‐based scenario motivating as their efforts were tracked. With regard to the web‐based exercise scenario, patients commented on the fact that the system required them to log on to a personal account. While this seemed to motivate some, others pointed out the possibility of fooling the system: “And that he [the therapist] can see, based on your login and your exercises, how often and when you exercise, and things like that. I find that… very risky as I could think ‘I’m not in the mood for performing exercises but I’ll just log in so [the therapist] will think that I’ve done them anyway’” (female participant, 23).
There was also a group of patients who thought it was their job to motivate themselves. “It is me I am doing this therapy for, not the physiotherapist” (male participant, 44). This group did not foresee any problems in training individually with distant supervision.
Group motivation Furthermore, patients who did not consider themselves as self‐disciplined in particular, found it motivating to train in groups. For these patients it was important to be motivated by others: “…you stir each other up a little and you don’t want to be inferior to one another” (female participant, 23). They thought that all home‐based exercise scenarios would be less motivational than group training at a clinic. Nonetheless, some participants preferred treatment in the home setting because they considered the group process to be inhibiting. One female participant (47) thought she would express feelings more openly during individual treatment. One male participant (23) expressed feeling shame when exercising in a group. He felt de‐motivated by the fact that he, a younger person surrounded by older people, was so disabled.
Exercise environment Patients highlighted the fact that all scenarios presented would have an impact on their motivation to exercise. Most patients felt more hesitation to cancel an appointment at the clinic, than to decide to skip exercise at home in the case of telerehabilitation. : “… I mean, I have to sit at home and exercise a little bit, this may be easy, but… but it’s also the going out, that you go somewhere and that you have an appointment, and then you must do it” (female participant, 41). In addition, some patients considered the house a more distracting environment: “Someone might just ring the doorbell. People can call” (female participant, 36). Some patients stressed they wanted to keep their home environment separate from their treatment environment. “Well, and then you go [to the clinic]. You forget about work. You do have to follow therapy and everything…It affects my state of mind. You are completely out of your home environment” (male participant, 44). Though some patients favoured a separation of their home and rehabilitation environment, there were patients who preferred a home‐based treatment because they found the home environment more private and comfortable.
Availability of resources All participants mentioned the necessity of resources for the use of home telerehabilitation programs. Some patients reported a lack of exercise space, lack of exercise equipment or the absence of a personal computer and internet connection. However, the majority of the patients reported exercise space would be available to them and expected that the technical resources and equipment would be provided by the rehabilitation clinic.
Flexibility exercise times Participants perceived flexibility as the main advantage of the telerehabilitation scenarios. Telerehabilitation was expected to be more compatible with daily life: “No longer hurried, I have to go [to the clinic]. You can fit your treatment into your own rhythm” (female participant, 47). Patients liked the idea of being able to perform their exercises early in the morning or late in the evening, before and after work as they were not reliant on their clinic’s or therapist’s availability. This perceived advantage applied most particularly to the web‐based and sensor‐based telerehabilitation scenario. One male patient (participant, 28) even proposed the possibility of exercising at work. Although most people thought of flexibility as an advantage, a minority still preferred exercising at fixed times. They thought that otherwise they would fail to give priority to exercising or would just forget to exercise.
Travel issues Some participants stressed the physical and mental exhaustion of travelling to the clinic: “Well, at the time [of treatment] I had a lot of trouble with driving. Especially when it’s somewhat busier then it’s hard. Then you are already tired by the time you arrive…” (male participant, 28). Others experienced physical pain during the journey from their homes to the clinic. “Every bump I take hurts” (female participant, 23). In addition, patients who relied on others to get to the clinic felt they were being a burden to their care givers. Participants with a job or other commitments in particular, perceived the advantages of reduced travel time and reduced travel expenses with respect to the telerehabilitation scenarios.
Social isolation Some patients considered social isolation as a consequence of home‐based exercise treatment. Going to the clinic was considered as an opportunity to get out of the house: “Yes, then you’re sitting at home… for me that plays a role, you know, because if I don’t take precautions, as I am not studying and don’t have a job, then I will be at home all day long” (male participant, 27). In addition, the clinic‐based treatment offered them the opportunity of meeting other people.
Intention to use (V)
Finally, we asked patients about their intentions to use any of the potential telerehabilitation services presented to them. With respect to all telerehabilitation scenarios patients were willing to use the technologies described. However, they attached greater value to therapist face‐to‐face contact and would rather not use these technologies as replacement of clinic‐based care. Instead they preferred to use these technologies during follow‐up care or as additional care to complement their regular care at the clinic.
Discussion
The central aim of this study was to explore chronic pain patients’ perceptions of prospective telerehabilitation services and to determine the factors important to them.
Patients perceived telerehabilitation to have certain benefits over traditional care. However, at present none of the participants would consider telerehabilitation as an autonomous treatment as they expressed concerns relating to UTAUT construct of performance expectancy. For instance, patients highly valued face‐to‐face contact with their therapist as they considered being touched by a professional essential for effective feedback and exercise instructions. This was especially important during the first phases of treatment and diminished for some when they became more confident with exercising. A study of Escolar‐Reina et al. 24 confirms the importance of adequate feedback and instructions to reduce pain patients’ insecurity when exercising at home.
Some participants were willing to accept less physical presence later on in their treatment, if feedback about their movements was provided by means of a sensor‐based system. Half of the participants, however, remained skeptical about the quality of feedback that such a system would provide. This skepticism is probably the result of a lack of exposure to telerehabilitation technologies 25 and the fact that patients still consider physiotherapy as a predominantly ‘hands on’ practice.
Secondly, face‐to‐face contact with a therapist was considered important for receiving emotional support during treatment. This coincides with the role psychological behavioral mechanisms play in chronic pain. 26 Patients expressed concerns that remote communication would lead to a feeling of alienation. This concern could be the effect of unfamiliarity with working with remote communication systems. 27 In addition, some patients expressed dependence on the physical presence of their therapist to motivate them to finish their exercise regimen. These patients were concerned that telerehabilitation treatment could result in a loss of motivation and therefore be less effective. This dependence on medical professionals is documented in earlier research about chronic low back pain. 28 , 29 A smaller number of patients indicated they did not feel the need to be motivated by others.
In addition to face‐to‐face therapist contact, fellow‐sufferer contact arose as an important theme, grouped under the construct of performance expectancy. This fellow‐sufferer contact was considered particularly important for emotional support and for exchange of illness related information. This finding fits with previous studies on the importance of support groups. 30 , 31 , 32 In addition, most patients made use of the group to motivate themselves to work harder and to adhere to their exercise regimen. This is explained by the social comparison theory of Festinger. 33 This theory states that individuals, especially in western cultures, have the desire to evaluate their performance in comparison with others who are similar to them and draw motivation from this as they feel pressure to improve their abilities accordingly. 34
Patients valuing fellow sufferer contact expressed concerns that telerehabilitation would reduce fellow sufferer contact and their motivation to exercise. Although one patient pointed out the possibility of virtual support groups, most patients stressed the importance of the physical presence of one another. Further research is needed to investigate if virtual group support could replace the need for the physical presence of fellow sufferers. Some patients on the other hand, felt that group exercise was inhibiting. This effect is also found in bladder patients 35 and in chronic low back patients who expressed feelings of embarrassment when training in a group. 36 For these patients, telerehabilitation treatment would address their desire to exercise privately. Patients also valued individual treatment as they felt their individual needs would not be addressed during group exercises.
Besides the UTAUT construct of performance expectancy, most of the subthemes arose under the construct facilitating conditions. Among them was flexibility which the participants regarded as the most important advantage of home based telerehabilitation. Patients stated they could exercise whenever they liked and avoid travelling to the clinic during working hours. In addition, the home environment was preferred by some as it offered privacy and a relaxing environment. Some patients considered training in the home environment beneficial as exercise skills would be acquired at home and could be implemented in daily life. These findings are confirmed by other studies. 37 , 38
Nonetheless, for most participants the flexibility of time and location was inferior to the advantages of the traditional treatment. Although travelling to the clinic could be exhausting and time‐consuming, some patients found it a good way ‘to get out of the house’ and meet other people. This finding accords with other research. 39 As half of our research sample was unemployed, this could be a possible explanation for their need for social contacts. In addition, some patients stated they wanted to keep their home environment separate from their treatment environment and would therefore accept the travel time. A review regarding home‐based rehabilitation elucidates this possible intrusion caused by home based care as it brings clinical care to the ‘safe haven’ of the home environment. 40
In addition, patients thought that the atmosphere in the clinic kept them more focused than they would be in their home environment. For them, training in the home environment would result in a loss of motivation to exercise. This is explained by Hale et al. 41 who state that within the home environment there is the need for internal motivation, while in the clinical setting, the motivation for therapy may come from the setting itself.
Finally, some patients stressed that it would be difficult to engage in telerehabilitation as their homes were not suited to becoming exercise areas due to a lack of space. These results are in concordance with a study by Stephenson and Wiles. 42
These results make it clear that the UTAUT constructs perceived usefulness and facilitating conditions offer a good starting point in structuring and understanding patients’ perceptions of prospective telerehabilitation services. In relation to the UTAUT constructs social norm and ease of use, fewer themes arose. Those that did were of less concern according to the interviewed patients. Few patients commented on the way their peers would react to telerehabilitation and if so, they commented that their peers would support them during their treatment. In addition, most of the patients did not expect to have problems when using the software or equipment needed for telerehabilitation. This is in concordance with earlier literature. Taylor and Todd 43 point out that, users without prior experience are more likely to view the use of technology in terms of perceived usefulness.
Limitations
The sample size of this study is small, which limits the ability to generalize these findings. However, the use of maximum variation allowed for a wide range of perceptions regarding prospective telerehabilitation services. Future quantitative studies are needed to further explore patients’ perceptions of these services and to investigate whether patterns in the patients’ characteristics might explain their perceptions regarding telerehabilitation.
In addition, we intentionally used scenarios that each depicted a different functionality of telerehabilitation, thereby representing telerehabilitation as a total replacement of clinic‐based care. Although this method has provided insight into patients’ perceptions about the pros and cons of telerehabilitation, future studies should investigate patients’ perceptions with regard to more realistic scenarios by, for example, exploring patients’ perceptions of telerehabilitation as a partial replacement of clinic‐based care and by presenting scenarios that combine different modalities of telerehabilitation (e.g. a webbased exercise program with sensor monitoring).
Furthermore, patients who participated in this study had no prior experience with telerehabilitation services. As limited telerehabilitation services exist at this point in time, patients’ perceptions regarding telerehabilitation are solely based on their expectations. However, all participants were familiar with physiotherapy treatment; twelve participants already experienced the clinicbased rehabilitation program. Therefore, they were able to elaborate on the pros and cons of traditional vs prospective telerehabilitation services. Further research should investigate the role of prior experience with telerehabilitation on patients’ perceptions regarding these services.
Conclusions
A central aim of this study was to explore chronic pain patients’ perceptions towards future telerehabilitation services and to determine the factors important to them. The main findings reveal that patients valued the benefits of telerehabilitation and considered telerehabilitation especially helpful as a complement or follow up to traditional treatment. However, none of them would consider telerehabilitation as an autonomous treatment as they as they felt that the perceived benefits do not override their perceived barriers regarding the use of telerehabilitation. These barriers included doubts about the effectiveness of telerehabilitation because of diminished face‐to‐face therapist contact, fellow sufferer contact and feelings of alienation. In addition, patients mentioned the internal barrier of motivation, stressing that telerehabilitation would result in a loss of motivational stimuli eventually leading to lower treatment compliance. Future research should investigate whether these perceived barriers are the result of unfamiliarity with telerehabilitation services and could therefore be overcome by giving more information to increase patients’ confidence in these services and eliminate misunderstandings about it. In addition, research should focus on careful selection of appropriate target groups and on the adaptation and design of technologies to overcome reported drawbacks.
Our research also shows that the UTAUT 22 is a useful organising structure in which to study patients’ willingness to use prospective telerehabilitation applications and has made the UTAUT constructs more context‐specific for telerehabilitation. Future quantitative studies are needed to further explore patients’ intention to use prospective telerehabilitation services.
Sources of funding
Roessingh Research & Development, Enschede, The Netherlands.
References
- 1. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. European Journal of Pain, 2006; 10: 287–333. [DOI] [PubMed] [Google Scholar]
- 2. Lahad A, Malter AD, Berg AO, Deyo RA. The effectiveness of four interventions for the prevention of low back pain. The Journal of the American Medical Association, 1994; 272: 1286–1291. [PubMed] [Google Scholar]
- 3. Jensen MP, Nielson WR, Turner JA, Romano JM, Hill ML. Changes in readiness to self‐manage pain are associated with improvement in multidisciplinary pain treatment and pain coping. Pain, 2004; 111: 84–95. [DOI] [PubMed] [Google Scholar]
- 4. Blyth FM, March LM, Brnabic AJ, Cousins MJ. Chronic pain and frequent use of health care. Pain, 2004; 111: 51–58. [DOI] [PubMed] [Google Scholar]
- 5. Rainville J, Hartigan C, Martinez E, Limke J, Jouve C, Finno M. Exercise as a treatment for chronic low back pain. The Spine Journal, 2004; 4: 106–115. [DOI] [PubMed] [Google Scholar]
- 6. Fordyce W, McMahon R, Rainwater G et al. Pain complaint‐exercise performance relationship in chronic pain. Pain, 1981; 10: 311–321. [DOI] [PubMed] [Google Scholar]
- 7. van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain. A systematic review of randomized controlled trials of the most common interventions. Spine, 1997; 22: 2128–2156. [DOI] [PubMed] [Google Scholar]
- 8. van Tulder MW, Malmivaara A, Esmail R, Koes BW. Exercise therapy for low back pain. Cochrane Database of Systematic Reviews (Online), 2000; 2: CD000335. [DOI] [PubMed] [Google Scholar]
- 9. Ostelo RW, van Tulder MW, Vlaeyen JW, Linton SJ, Morley SJ, Assendelft WJ. Behavioural treatment for chronic low‐back pain. Cochrane Database of Systematic Reviews (Online), 2005; 1:CD002014. [DOI] [PubMed] [Google Scholar]
- 10. Blanchard CM, Courneya KS, Rodgers WM et al. Is the theory of planned behavior a useful framework for understanding exercise adherence during phase II cardiac rehabilitation? Journal of Cardiopulmonary Rehabilitation, 2003; 23: 29–39. [DOI] [PubMed] [Google Scholar]
- 11. Rimmer JH, Wang E, Smith D. Barriers associated with exercise and community access for individuals with stroke. Journal of Rehabilitation Research & Development, 2008; 45: 315–322. [DOI] [PubMed] [Google Scholar]
- 12. Rosen MJ. Telerehabilitation. Neuro Rehabilitation, 1999; 12: 11–26. [Google Scholar]
- 13. Temkin AJ, Ulicny GR, Vesmarovich SH. Telerehab. A perspective of the way technology is going to change the future of patient treatment. Rehab Management, 1996; 9: 28–30. [PubMed] [Google Scholar]
- 14. Agrell H, Dahlberg S, Jerant AF. Patients’ perceptions regarding home telecare. Telemedicine and E-Health, 2000; 6: 409–415. [DOI] [PubMed] [Google Scholar]
- 15. Ruland CM, Moore SM. Eliciting exercise preferences in cardiac rehabilitation: initial evaluation of a new strategy. Patient Education and Counseling, 2000; 44: 283–291. [DOI] [PubMed] [Google Scholar]
- 16. van Baar JD, Joosten H, Car J et al. Understanding reasons for asthma outpatient (non)‐attendance and exploring the role of telephone and e‐consulting in facilitating access to care: exploratory qualitative study. Quality & Safety in Health Care, 2006; 15: 191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jones M, Jolly K, Raftery J, Lip GY, Greenfield S. ‘DNA’ may not mean ‘did not participate’: a qualitative study of reasons for non‐adherence at home‐ and centre‐based cardiac rehabilitation. Family Practice, 2007; 24: 343–357. [DOI] [PubMed] [Google Scholar]
- 18. Brattberg G. Internet‐based rehabilitation for individuals with chronic pain and burnout: a randomized trial. International Journal of Rehabilitation Research, 2006; 29: 221–227. [DOI] [PubMed] [Google Scholar]
- 19. Buhrman M, Faltenhag S, Strom L, Andersson G. Controlled trial of internet‐based treatment with telephone support for chronic back pain. Pain, 2004; 111: 368–377. [DOI] [PubMed] [Google Scholar]
- 20. Kotarba JA, Seidel JV. Managing the problem pain patient: compliance or social control? Social Science & Medicine, 1984; 19: 1393–1400. [DOI] [PubMed] [Google Scholar]
- 21. Donovan JL, Blake DR. Patient non‐compliance: deviance or reasoned decision‐making? Social Science & Medicine, 1992; 34: 507–513. [DOI] [PubMed] [Google Scholar]
- 22. Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Quarterly, 2003; 27: 425–478. [Google Scholar]
- 23. Patton MQ. Qualitative Evaluation and Research Methods. London: Sage Publications Ltd, 1990. [Google Scholar]
- 24. Escolar‐Reina P, Medina‐Mirapeix F, Gascón‐Cánovas JJ et al. How do care‐provider and home exercise program characteristics affect patient adherence in chronic neck and back pain: a qualitative study. BMC Health Services Research, 2010; 10: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Theodoros D, Russell T. Telerehabilitation: current perspectives. Studies in Health Technology and Informatics, 2008; 131: 191–209. [PubMed] [Google Scholar]
- 26. Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain, 1998; 77: 231–239. [DOI] [PubMed] [Google Scholar]
- 27. Harrison R, MacFarlane A, Murray E, Wallace P. Patients’ perceptions of joint teleconsultations: a qualitative evaluation. Health Expectations, 2006; 9: 81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Klaber Moffett JA, Richardson PH. The influence of the physiotherapist‐patient relationship on pain and disability. Physiotherapy Theory and Practice, 1997; 13: 89–96. [Google Scholar]
- 29. Cook FM, Hassenkamp A‐M. Active rehabilitation for chronic low back pain: the patients’ perspective. Physiotherapy, 2000; 86: 61–68. [Google Scholar]
- 30. Ng P, Chan W. Group psychosocial program for enhancing psychological wellbeing of people with systemic lupus erythematosus. Journal of Social Work in Disability and Rehabilitation, 2007; 6: 75–87. [DOI] [PubMed] [Google Scholar]
- 31. Subramaniam V, Stewart MW, Smith JF. The development and impact of a chronic pain support group: a qualitative and quantitative study. Journal of Pain and Symptom Management, 1999; 17: 376–783. [DOI] [PubMed] [Google Scholar]
- 32. Weis J. Support groups for cancer patients. Supportive Care in Cancer, 2003; 11: 763–768. [DOI] [PubMed] [Google Scholar]
- 33. Medina‐Mirapeix F, Escolar‐Reina P, Gascón‐Cánovas JJ, Montilla‐Herrador J, Collins SM. Personal characteristics influencing patients’ adherente to home exercise during chronic pain: a qualitative study. Journal of Rehabilitation Medicine, 2009; 41: 347–352. [DOI] [PubMed] [Google Scholar]
- 34. Festinger L. A theory of social comparison processes. Human Relations, 1955; 7: 117–140. [Google Scholar]
- 35. Wood JV. Theory and research concerning social comparisons of personal attributes. Psychological Bulletin, 1989; 106: 231–248. [Google Scholar]
- 36. Karvinen KH, Courneya KS, Venner P, North S. Exercise programming and counseling preferences in bladder cancer survivors: a population‐based study. Journal of Cancer Survivorship, 2007; 1: 27–34. [DOI] [PubMed] [Google Scholar]
- 37. Cooper K, Smith BH, Hancock E. Patient‐centredness in physiotherapy from the perspective of the chronic low back pain patient. Physiotherapy, 2008; 94: 244–252. [Google Scholar]
- 38. Hale L, Bennett D, Bentley M, Crawshaw A, Davis H. Stroke rehabilitation – comparing hospital and home‐based physiotherapy: the patient’s perception. New Zealand Journal of Physiotherapy, 2003; 31: 84–92. [Google Scholar]
- 39. Tamm M. What does a home mean and when does it cease to be a home? Home as a setting for rehabilitation and care. Disability and Rehabilitation, 1999; 21: 49–55. [DOI] [PubMed] [Google Scholar]
- 40. Thomas C, Parry A. Research on users’ views about stroke services: towards an empowerment research paradigm or more of the same? Physiotherapy, 1996; 82: 6–12. [Google Scholar]
- 41. Hale L, Bennett D, Bentley M, Crawshaw A, Davis H. Stroke rehabilitation – comparing hospital‐ and home‐based physiotherapy: the patients’ perception. New Zealand Journal of Physiotherapy, 2003; 31: 84–92. [Google Scholar]
- 42. Stephenson S, Wiles R. Advantages and disadvantages of the home setting for therapy: views of patients and therapists. British Journal of Occupational Therapy, 2000; 63: 59–64. [Google Scholar]
- 43. Taylor S, Todd P. Assessing IT usage: the role of prior experience. MIS Quarterly, 1995; 19: 561–570. [Google Scholar]


