Abstract
Background In recent years, self‐tests have become increasingly available to the general public, though their value is still being debated. Because these tests are available, consumers should have access to clear information about self‐testing. Examining experiences of self‐testers could contribute to the development of consumer information.
Objective Detailed exploration of consumers’ experiences with self‐testing for cardiovascular risk factors.
Methods Semi‐structured interviews with 20 consumers who had performed a self‐test for glucose, cholesterol or albuminuria. The main topics of the interviews were reasons for self‐testing, performing the self‐test, follow‐up behaviour and perceived need for information on self‐testing. Data were analysed using thematic content analysis.
Results Regarding the reason for self‐testing, three types of users were distinguished: those who engaged in self‐testing when a test was offered, either with or without previous knowledge about the disease or risk factor, and those who had actively decided to test and had searched for a self‐test themselves. Self‐testers had generally experienced no problems performing the test or interpreting the result and had considerable confidence in the result. They were easily reassured by a normal result, while an abnormal result did not automatically mean they consulted a doctor. Most participants did not feel the need for more information.
Conclusions Self‐testers often perform tests for reassurance, without considering the disadvantages, such as the absence of professional counselling and the risk of false‐positive or false‐negative results. Consumer information should promote more informed and deliberate choices for self‐testing.
Keywords: cardiovascular risk factors, interview study, self‐management, self‐test, self‐testing
Introduction
Self‐tests, tests on medical conditions which can be performed without the involvement of a health‐care professional, have become increasingly available to the general public. 1 , 2 In this study, we define a self‐test as an in‐vitro test on body materials, initiated by a consumer, with the aim of diagnosing a particular disease or identifying a risk factor. These tests, which include tests on cardiovascular risk factors, infectious diseases or cancer, are available as home tests, streetcorner tests, direct‐access or home collect tests (Table 1). 3 They give consumers the opportunity to assume responsibility for their own health and can offer people a convenient alternative to tests initiated by a doctor. 4 , 5 Nevertheless, there are concerns about the safety of self‐testing. 6 , 7 Some of the self‐tests have shown to be unreliable, 8 and there are concerns whether people consider the negative sides of self‐testing, such as the risk of false‐positive results, which could lead to anxiety and unnecessary medical investigations, or false reassurance in case of false‐negative results. 9
Table 1.
Explanation about tests described
| Ways of performing a self‐test | Explanation | |||
|---|---|---|---|---|
| Home test | Test can be bought for example on the Internet or in pharmacies. The test package contains everything needed for performing the test, including a pen needle (if a blood sample needs to be taken), a test cassette or test strip and an instruction leaflet how to perform the test | |||
| Street corner test | Tests are offered by organizations in public places, for example supermarkets, where the test is performed by trained personnel and a direct result of the test and advice what to do next is given | |||
| Direct‐access test | Consumers can go to a laboratory where a sample is taken. Consumers receive the results a few days later by mail or e‐mail | |||
| Home‐collect test | Consumers send body materials (for example blood or saliva) to a laboratory and receive the results a few days later by mail or e‐mail | |||
| Test | Measures | Condition | Most common ways of performing the test* | Mass media campaign or offering of free tests |
| Cholesterol | Total cholesterol or total cholesterol and HDL in blood | Cholesterol (risk factor for cardiovascular disease) | Streetcorner test/home test | Tests have been offered for free in streetcorner testing in supermarkets and other public places |
| Glucose | Glucose in blood | Diabetes | Home test/streetcorner test | Tests have been offered for free in streetcorner testing in pharmacies and other public places |
| Albuminuria | Albumin in urine | Kidney disorders (for example as a complication of diabetes or hypertension) | Home test | Media campaign by the Dutch Kidney Foundation and offering of free tests in 2006 |
*Based on: Ickenroth et al. 24
A survey among Dutch Internet users in 2006 showed that 16% of the respondents had ever used a self‐test, the most frequently used self‐tests being those for cardiovascular risk factors: 6.2% of the respondents had performed a glucose self‐test, and 5.4% had performed a cholesterol test without consulting a doctor first. 3 In September 2006, free home tests to detect albuminuria were offered to the Dutch public by the Dutch Kidney Foundation, accompanied by a mass media campaign on asymptomatic kidney disease. This self‐test was ordered by 7.8% of the Dutch adult population in the first thirty days of the campaign. 10
A survey among consumers who had had a cholesterol streetcorner test carried out showed that it was particularly the healthy and slightly worried consumers who took these tests (the ‘worried well’). 11 A problem of screening in low‐risk populations is the considerable rate of false‐positive results. Another concern is whether consumers can adequately interpret the results of self‐tests. Risks of developing cardiovascular diseases in particular have to be interpreted in the light of multiple risk factors. As a result, consumers are faced with difficult decisions to make, concerning indications for doing a test, understanding of the validity of the self‐test and deciding about appropriate follow‐up behaviour.
Because these tests are available to the general public, it is important that consumers have access to clear and easy to understand information about the pros and cons of self‐testing, the interpretation of test results and appropriate follow‐up behaviour. Developing such specific self‐test information requires knowledge about the experiences of people who have used self‐tests. The main objective of our qualitative study was to gain an in‐depth understanding of the experiences of self‐testers who had performed self‐tests for cardiovascular risk factors. The interview topic guide was based on earlier research, the Health Belief Model (HBM) 12 and topics considered important by the research team. According to the HBM, an individual’s decision to engage in health‐related behaviour is defined by the perceived severity of and the perceived susceptibility to a particular condition or illness and the evaluation of the effectiveness of a certain action that would reduce their susceptibility to or the severity of this condition. However, individuals are only inclined to perform a certain action if they perceive more benefits than barriers associated with that action and if certain cues (e.g. bodily or environmental events) are present that trigger action. Furthermore, the individual’s confidence in his or her capability to successfully perform a certain action (self‐efficacy) is an important concept within the HBM. 12 , 13 , 14 In the present qualitative study, in addition to these HBM‐concepts about determining to do the test, we also asked consumers what information they thought was important to enable them to correctly perform and interpret self‐tests.
Methods
Participants
Participants were recruited from an online access panel managed by Flycatcher, an ISO certified institute for online research associated with Maastricht University (http://www.flycatcher.eu). People can apply for the panel if they have an e‐mail address and are aged 12 years or over. In September 2008, a random sample of 6700 panel members received a questionnaire on self‐testing. They were asked whether they had ever used a self‐test, which self‐test they had performed, what the result of the test was and if researchers could contact them for further research. Of the 4416 respondents, 799 (18%) had used a self‐test at least once. The question if the respondent did not mind being contacted for an invitation to take part in a face‐to‐face interview received a positive response from 72 of the 198 respondents who had performed a cholesterol self‐test, 49 of the 232 glucose self‐testers and 78 of the 218 respondents who had performed an albuminuria test.
We selected all respondents who had performed a self‐test during the past 2 years and who were living within a 2‐h driving distance from Maastricht University (for logistical reasons). We deliberately sampled people with a range of characteristics in terms of gender, age, type of self‐test used and result of the self‐test. The selected self‐testers received an e‐mail explaining the goal of our research and the nature of the interview. We asked the respondents to reply to our mail whether they were willing to participate and contacted them by telephone to make an appointment. If they did not respond within a week, we sent a reminder. Participants received a gift voucher as an incentive to participate.
Ethical approval
The Medical Ethical Committee of Maastricht University indicated that no ethical approval was needed for this study.
Interview route
Themes and questions on self‐test behaviour were derived from earlier research, 3 from the Health Belief Model 12 , 15 and from topics considered important by the research team. The research team then reached consensus on the themes and questions that should be addressed during the interview. This resulted in four themes becoming the main topics of our interviews: the reason for performing a self‐test, performing the self‐test, the follow‐up behaviour and the perceived need for information about the self‐test. We asked open‐ended questions about the four main themes, encouraging respondents to talk about their experiences and stimulating them to express their opinion. In the interview plan, each main theme was addressed by questions on subthemes that had to come up during the interviews and that were used to further encourage participants to talk about their experiences. A general impression of users’ ideas on self‐testing was obtained by starting each interview with the open question how the respondent had experienced performing the self‐test. The complete topic guide for the interviews is described in our protocol article. 16
Interviews and analysis
The semi‐structured interviews took place at the participants’ homes and were conducted by one of the researchers or a final‐year medical student, between May and September 2009. Respondents were informed about the goal of the study and were asked whether they agreed to the conversation being audiotaped. Field notes were made after the interviews about the atmosphere of the interview, personal characteristics of the participant and any comments that were not on the audiotape (for example, statements made after the recorder had been switched off). To standardize the interviews, the researchers and the medical student used the same interview scheme. The scheme was piloted by interviewing medical students, and the interviewers practiced their interview skills by listening to each other’s interviews and giving feedback.
The recorded interviews were transcribed verbatim and analysed with NVivo 2.0, using thematic content analysis. 17 An initial set of codes was derived from the answers that were given to the questions in the interviews. To begin with, five interviews were analysed. They were independently coded by one researcher (MI) and a medical student (MT), and codes were discussed until consensus had been achieved. After these interviews had been coded, all codes were discussed and assigned to one of the main themes. Some codes with similar meaning were merged. This new coding scheme was then used to code the remaining interviews. Each interview was coded by two researchers (MI and JG) and discussed until consensus was reached. If a new topic was found, a new code was added. Respondents’ experiences with self‐testing were described by grouping together and analysing the codes that belonged to the same theme. The quotes included in this article were translated from Dutch into English by a professional translator.
Results
Eighty questionnaire respondents were invited by e‐mail for an interview. A total of 28 of them responded and were interviewed subsequently. During the interviews, we found eight of them not to have performed a self‐test according to our definition (for example, they were diabetics using diabetes monitoring tests, or the test had been initiated by a doctor) and were excluded for further analysis. Hence, 20 interviews were analysed (Fig. 1). Participants’ characteristics are listed in Table 2. Although some of the participants had performed multiple tests, the main topic during the interview was the test for which they had been invited, although they were given an opportunity to share their experiences with other tests they might have used.
Figure 1.
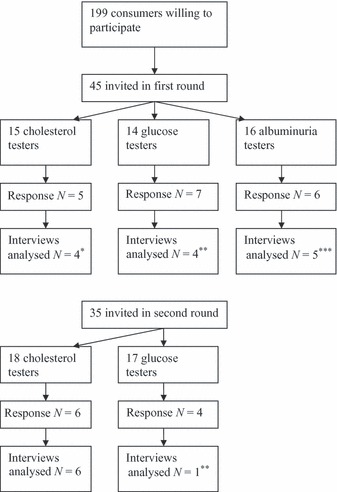
Selection of participants. *One respondent excluded; had not performed self‐test according to our definition; **Three respondents excluded; were using glucose monitoring tests; ***One respondent excluded; had not performed the test.
Table 2.
Participants’ characteristics
| Respondent | Gender | Age | Test (test result)* | Type of test | Other tests (test result)* |
|---|---|---|---|---|---|
| 1 | F | 56 | Cholesterol (positive) | Streetcorner | – |
| 2 | F | 53 | Cholesterol (negative) | Streetcorner | – |
| 3 | F | 72 | Cholesterol (negative) | Streetcorner | – |
| 4 | F | 45 | Cholesterol (negative) | Home test | – |
| 5 | F | 24 | Cholesterol (negative) | Home test | – |
| 6 | F | 41 | Cholesterol (negative) | Streetcorner | Albuminuria (positive) |
| 7 | F | 58 | Cholesterol (negative) | Home test | Albuminuria (negative) |
| 8 | F | 45 | Cholesterol (negative) | Streetcorner | – |
| 9 | M | 40 | Cholesterol (positive) | Lab test | – |
| 10 | F | 42 | Cholesterol (negative) | Streetcorner | Albuminuria (negative) |
| 11 | F | 58 | Albuminuria (negative) | Home test | Cholesterol (positive) |
| 12 | M | 55 | Albuminuria (positive) | Home test | – |
| 13 | F | 52 | Albuminuria (negative) | Home test | Cholesterol (positive) |
| 14 | F | 33 | Albuminuria (positive) | Home test | – |
| 15 | F | 44 | Albuminuria (negative) | Home test | – |
| 16 | M | 63 | Glucose (negative) | Home test | Cholesterol (negative) |
| 17 | F | 55 | Glucose (negative) | Home test | Cholesterol (negative) |
| 18 | F | 74 | Glucose (negative) | Home test | Albuminuria (negative) |
| 19 | F | 35 | Glucose (positive) | Home test | – |
| 20 | F | 56 | Glucose (negative) | Home test | – |
*Test result as perceived and remembered by the respondent.
There was a considerable amount of overlap between the three tests in terms of the themes emerging from the interviews, and data saturation occurred after fifteen interviews.
Five main themes emerged from the data, corresponding to a large extent to the main themes of our interview plan. The themes were as follows: the reason to perform a self‐test, performing and interpretation of the test, follow‐up behaviour, information needs and confidence in the test result. The results of the interviews are discussed below for each of the main themes (Table 3).
Table 3.
Summary of themes and main outcomes
| Reasons for self‐testing | Performing and interpreting the test result | Confidence in test result | Follow‐up | Information needs |
|---|---|---|---|---|
| Test was offered/media attention | Generally no problems | Test is offered by well‐known organization | Normal test result: Reassurance, no further action | Explanation about disease |
| Curious | Problems experienced | Tests are also used by professionals | Discuss test with doctor | Types of cholesterol |
| Asymptomatic disease | Using the pen needle | Personal experience with test | Doubts about validity | Information on different risk factors |
| Personal experience with disease | Comparing colours of dipstick with chart | Repeated tests gave same results | Was test performed correctly? | Indications for test |
| Serious disease | What to do with low‐positive result | Test worked properly | Obligation to discuss test with doctor | How to perform the test |
| Reassurance/health status | Test measures only total cholesterol | Package indicated test is reliable | Test is of little value | Test involves pen needle |
| Individual risk for disease/complaints | Tests are developed to be of good quality | Abnormal result: Not worried | Reliability | |
| Need valid reason to see doctor | Test is random indication | Discuss test with doctor | What can influence test result | |
| Can do the test at any time | Physicians doubt self‐tests | Did not see doctor: | Test is random indication | |
| No need for making appointment | Test result not what was expected | Can only change diet | Point‐of‐sale information | |
| Doctor refused to do test | Tests are still being developed | Test did not work properly | What to do after test | |
| Commercially available | Mild abnormality | |||
| Test is too cheap or too easy to be of good quality | Is only point estimate | |||
| Feeling healthy | ||||
| Lifestyle changes: already trying to eat a healthy diet or hard to change |
Reasons for self‐testing
Three types of testers were distinguished. The first was the passive self‐tester who became aware of the risk factor or disease when a self‐test was offered; the second was the passive self‐tester who was already aware of the risk factor or disease and the third was the active self‐tester, who had actively sought an opportunity to self‐test, or had bought one.
The first type of self‐tester had never had the intention to do a test for a particular disease or risk factor until they were confronted with the opportunity to test. Media, commercials and streetcorner tests had made respondents aware of the fact they could have a risk factor without knowing it and gave them the opportunity to do a self‐test. The respondents then became curious about these tests and thought it would be good to know whether they had the disease or risk factor. This was the most common reason in the group of respondents who had taken an albuminuria self‐test.
It was offered to me. I was given something somewhere and I could apply for a kidney test, for free, so I thought, well, why not. It’s just to check yourself. Especially when you’re getting on a bit, you start to take more notice of your body. So you think, well, such a check‐up, that’s like, is everything still OK with those kidneys. And well, you could always decide later, you know, if there’s an unfavourable result, or a less favourable one, you can still go see your general practitioner.
(Female, age 44, albuminuria, normal test result)
The second type of self‐testers, mostly those using cholesterol self‐tests, already had some knowledge about the disease or risk factor, for example because of some kind of personal involvement with the condition (e.g. having family or friends with cardiovascular disease, or because they had had a cholesterol test carried out before), or were already conscious of the importance of a healthy lifestyle. These respondents wanted to do the test to get more information about their health status, to confirm that they were in good health, or because they were seeking reassurance. On the other hand, they had not actively sought medical advice, because they did not have any complaints and were feeling healthy; they said they would only go to a doctor if they had good reason to think something might be wrong. Others felt no need to see a doctor when they did not have any complaints, but might ask for a test in future when they had to see their general practitioner (GP) for some other reason. Some respondents did not want to take up their doctor’s time without (in their opinion) having a valid reason. When a self‐test was offered, they saw this as an easy opportunity to be tested, because there was no need to make an appointment and they could do the test whenever they wanted to.
Well, you know, not necessarily having it tested at the doctor’s, but just because I wanted to know. Because, well, not that I’m fat or whatever, but you might still have high cholesterol. […] And your GP, well, you go see him when you don’t feel well, right, then you think I’d better go see my doctor and have it checked. But actually I feel OK, and so I’d still want to know if it might be too high or if it’s good; I also want to know if it’s OK.
(Female, age 53, cholesterol, normal test result)
The third type, the active self‐testers, had actively decided to do a self‐test and had looked for opportunities to do one, often resulting in home tests. The reasons to do a test were mainly the same as those for the second type (looking for confirmation that they were in good health or having some personal involvement with the disease), or because they thought they were at risk for developing cardiovascular disease, considered the disease to be a serious condition, or had certain complaints. These respondents also said they needed a valid reason to go to a GP: some participants thought they would have to justify why they wanted to do the test, and the doctor might refuse to have it done. Other reasons to purchase a self‐test included that their doctor had previously refused to do the test at their request, that self‐tests give immediate results, that they could do the test whenever they wanted, that they did not have to make an appointment and that they did not have to go to the hospital to have fasting blood samples taken without having had breakfast.
Well, as I said, you know, it’s a bit easier, not having to make another appointment. The GP might ask do you really want to have that checked again; you’ve had it checked and it was OK. So I sort of wanted to know if the result was still the same. And yes, I didn’t want to bother my GP again, that sort of thing.
(Female, age 58, cholesterol, normal test result)
Performing the self‐test and interpreting the result
Most self‐testers had not experienced any problems in performing the self‐test. Some cholesterol self‐testers who had performed a home test indicated they had had problems using the pen needle and reported that it was difficult to use it on oneself. They indicated that the packaging should explain that a pen needle had to be used, or that it was easier to ask someone else to help you.
Some of the self‐testers who had performed the albuminuria test had experienced difficulties in comparing the colour of the dipstick with the colour chart to determine the level of albumin in their urine. This had to be carried out in daylight, because the results were difficult to read in artificial light. Because the test had to be performed with first void urine and the test was distributed in winter, when it is still dark in the morning, not all testers were able to decide the results correctly, because of lack of daylight. The albuminuria test also caused some problems regarding the interpretation of the test result. The result could be negative (no albumin in urine), low positive (trace of albumin) or high positive (albuminuria). Testers with a low‐positive result did not know exactly what to do; one consulted a doctor for further explanation of the result, while another respondent said a low‐positive result was nothing to worry about, especially since he was feeling healthy, and therefore did not take any further action.
Some cholesterol testers were disappointed that the test measured only total cholesterol and said it left them without information about their ‘bad’ cholesterol. They thought the test had not been very useful.
Confidence in the test result
Many self‐testers had considerable confidence in the test result. Reasons for this confidence in self‐tests were that the test was offered by a well‐known organization (for example the Dutch Kidney Foundation) that they thought these tests were also used by professionals or that they had had previous experience with the tests. Further reasons to trust the test result were that the test had worked properly, that the package indicated that the test was reliable, and some just assumed that such tests were developed to high standards. For example, a female respondent indicated she had confidence in the self‐test for the following reasons:
Well, I’m thinking it’s from the Heart Foundation, you know. So I thought that’s a reliable organisation, right? And I mean, well, I guess these self‐tests have been carefully developed so they’re really reliable. It feels safe to me.
(Female, age 42, cholesterol, normal test result)
Some respondents reported using strategies to ensure valid results, such as repeating the test or having it repeated by a GP; if the result remained same, they would consider the test to be reliable.
Some of the respondents, particularly those using cholesterol self‐tests, realized that the test only gave an indication and that it should be repeated because test results vary over time. Reasons to doubt the test result were that doctors have expressed doubts about self‐tests, that self‐tests are still under development or that the test result was not what they had expected (for example receiving an abnormal test result while not having complaints). Some respondents had doubts because the tests were commercially available or thought that cheap tests that are very easy to perform might be of poor quality.
Of course I’m, well yes, I’m a bit sceptical about it, not 100%, you know, as it’s still, it’s in its infancy, and you don’t hear much about it, and you still think, well, I did the test, the result was normal, that’s good. But is it really OK? But I don’t dwell on that too long. I think, well, it’s OK, or it would have found at least some minor abnormality.
(Female, age 44 albuminuria, normal test result)
Follow‐up behaviour after performing a self‐test
Respondents were easily reassured by a normal test result. The test provided a sense of safety, and respondents felt they no longer had to worry about having a disease. Most of them did not discuss the test result with a doctor, although some did make an appointment with their family doctor, because they doubted whether they had performed the test correctly or were not sure about the validity of the test. Other reasons to see a doctor despite a normal test result were that they felt obliged to discuss medical concerns with their doctor and did not want to hide things from their doctor or doubted the value of the test because it only measured one risk factor for cardiovascular disease. Most respondents did not change their lifestyle: they were already trying to live a healthy lifestyle or found it difficult to change anything. Those respondents who did change their lifestyle improved their dietary habits. Some respondents indicated they would use the self‐test again in future, because they knew the outcome could change over time. One female respondent explained why she did not want to see a doctor after a normal test result:
When I’m reassured, and I see there’s no need. Then it’s OK. Then I’m not going to get it done again at the GP’s. I really wouldn’t do that, no, because then I might just as well go to my GP straightaway. No, I didn’t do that, no. Of course if it had been too high or whatever, then I’d go to the doctor. But if I see that the value is what it’s supposed to be, I really don’t go see my GP. No, I’m reassured, and I think: Oh good. So I just go on.
(Female, age 55, glucose, normal test result)
After an abnormal test result, respondents were not very alarmed. Some made an appointment with their general practitioner to discuss the test result and to have the test repeated, but were reassured by the knowledge that the condition was being diagnosed at an early stage and could be treated. Other reasons not to be alarmed were that respondents felt healthy and thought their condition was probably not very serious. Several respondents who had an abnormal result decided nevertheless not to see a doctor. The reasons they gave were that all they could do was to start eating a healthier diet, that they doubted whether the test had worked properly, that the test result showed only mild abnormality, that test results were liable to change over time, that they felt healthy, or that they had not got the right information about how to interpret the result and what to do next and did not take any further action.
So well, it actually came out pretty bad, this test, and so I asked our GP, and he checked my urine and it, well, it was fine. I didn’t really worry about it, because I thought well, I have no complaints, so it’s probably not serious. But then, err, you never know. It’s inside your body and you don’t notice it. So yes, I guess it might be a good idea to consult the doctor.
(Female, age 41, albuminuria, abnormal test result)
Yes, it wasn’t quite 100% OK. But it was, sort of, what shall I say, a bit below average. But then I thought, well, those colours weren’t 100% clear, and so I didn’t do anything about it. […] Well if it had been really clear, a clear signal that, you know, something’s wrong here, then I’d certainly have seen my general practitioner. Sure. But then it would have to be, err, have to be really clear. Not this sort of in‐between case as it was in my case, as I saw it. […] And well, I don’t have any complaints in that department.
(Male, age 55, albuminuria, abnormal test result)
Some respondents said they would do further self‐tests in future, because they thought it is important to have regular check‐ups or because the tests are offered for free. Others did not intend to do more self‐tests if they were expensive; they preferred to see a doctor who could give them advice or they did not want to diagnose a serious condition themselves. Some had been discouraged from doing more tests by their family doctor.
Respondents would recommend self‐tests to others, because they thought it was important to check for risk factors regularly, especially because these tests are easy to perform and easily accessible. Reasons not to engage in self‐testing included fear of panic and worries, the fact that mistakes can easily be made, or that self‐tests are considered not to be very reliable. One male participant would not recommend doing a self‐test to all people:
Well, I think it’s easy to make a mistake. And if someone’s like, at the very first sign, thinking Oh my God, I’ve got a terrible disease, well, I wouldn’t recommend such a test to someone like that, no. In that case I’d say, sort of, never mind, ignorance is bliss.
(Male, age 55, albuminuria, abnormal test result)
Need for information
Most respondents were satisfied with the information provided with the test. They indicated that if the test result was normal, they felt no need for more information.
Some of the cholesterol testers would have liked more information on the different types of cholesterol, about other cardiovascular risk factors, about the fact that test results can change over time and about using the pen needle.
Two respondents had bought their home test at a drug store. They were surprised that there was no point‐of‐sale information (for example, the shop assistant did not give any additional information when the test was bought), which one of them would have preferred.
Respondents generally thought that information should be given on indications for doing a test and on how to perform it, as well as explanations about the disease, that the disease can be asymptomatic, and about what to do after performing the test. They would also like to get information on lifestyle factors. The aspect of test reliability was mentioned by three respondents, who thought it was important to have information on factors that could influence the reliability of the test. Others did not think this was very important, because they assumed the quality of the test to be good.
If respondents needed more information, they preferred to receive it via Internet sites operated by well‐known and independent organizations. One female respondent indicated she did not feel she needed more information after doing a streetcorner test.
No, because I would have just thrown it away anyway, as I just know that I’m living a healthy lifestyle. So no, no. And I don’t usually take away leaflets anyway, as you just end up throwing them all in the wastepaper basket. […] No, I wouldn’t have, well, except if it wasn’t good. Then I’d have wanted it very much. I think that’s when it’s really important. If it’s bad news. But it was actually good, so that’s the end for me then, finished.
(Female, age 42, cholesterol test, normal test result)
Discussion
Main findings
In‐depth interviews with consumers who had performed a self‐test on cardiovascular risk factors revealed three types of testers: those who engaged in self‐testing when a test was offered, either with or without previous knowledge about the disease or risk factor, and those who had actively decided to test and had searched for a test themselves. Reasons for consumers to perform these self‐tests included wanting to be reassured about their health, responding to commercials or media campaigns, having personal experience with a disease and having symptoms. Self‐test behaviour often seemed to be rather straightforward: consumers came across self‐tests and used them because they were looking for reassurance or were curious about the test. We found that respondents did not want to see a doctor without having a ‘valid reason’; this was the main reason to do a self‐test instead of seeing a doctor, because they did not have complaints and felt healthy.
Respondents had experienced no major problems in performing and interpreting the test. They generally had considerable confidence in the test result and were generally reassured after a normal test result. Many respondents with a normal test result were already trying to live a healthy lifestyle and would not change this, although some intended to improve dietary habits. The self‐testers who had tested positive did not experience distress: they generally contacted their family doctor to discuss this result. Nevertheless, several did not contact a doctor despite an abnormal result.
Most respondents thought the information provided with the test was sufficient. If they needed more information, they would like to receive it preferably on the Internet, on sites operated by well‐known and independent organizations.
Strengths and limitations
Participants were deliberately sampled to cover a broad range of characteristics such as age, gender and type of test performed. Hence, we were able to interview self‐testers about different types of tests, test results and personal characteristics. The response to our invitation to participate in the interviews was 35% (28/80). The actual number of interviews analysed was 20, because several participants appeared to be either diabetics using monitoring tests or had performed tests that were not self‐tests according to our definition (the test having been initiated by a doctor). Most participants said to feel healthy and to already pay attention to a healthy lifestyle, although these self‐reports might be influenced for example by participants giving socially acceptable answers. Earlier research showed that self‐testers in general are more likely to engage in health‐related behaviour, but report lower health status. 3 During the interviews, most of our respondents indicated they worked or had had working experience, in health care, which may have biased our data, because we therefore probably interviewed a more informed population than the average user of self‐tests. Because of these participants’ characteristics, we might have interviewed a population that is probably better informed and feeling healthier than the average self‐test user.
Comparison with other studies
The reasons for self‐testing seem to fit in with the Health Belief Model. Perceived susceptibility and perceived severity of the disease were mentioned as reasons for self‐testing, especially among glucose self‐testers. Cues to action included media campaigns, but also friends or relatives who had a cardiovascular disease. Respondents were often already conscious of the risk caused by factors like high cholesterol, which induced them to do a self‐test.
Ryan et al. 18 found similar reasons for self‐testing: reassurance, out of curiosity or looking for a diagnostic outcome. They also reported that people frequently perform these tests simply because they are confronted with them. In their interview study, respondents indicated that they would not like to see a doctor without knowing something is wrong and were afraid to waste the doctor’s time.
In our study, respondents said they wanted to take responsibility for their own health and be reassured about being in good health. This suggests that it is especially the worried well, that is, those consumers who already have a healthy lifestyle and actually have a lower risk of developing cardiovascular disease, who engage in self‐testing. On the other hand, those truly at risk but unaware of their health status do not benefit from self‐testing. It is known that unrealistic optimism among high‐risk patients and unjustified pessimism in the low‐risk population are frequently found in the assessment of cardiovascular risk. 19
Little distress was experienced by participants who had tested positive. They realized that the test was intended to screen for a risk factor or disease and that they were supposed to discuss a positive test result with their family doctor. They felt that the risk factor would be modifiable and were not very alarmed. These findings are in line with earlier research on diabetes and microalbuminuria screening. 20 , 21 A negative test result was generally perceived as reassuring, not necessitating further action. Negative test results can, however, lead to a false sense of reassurance, and the perception of a ‘certificate of health’, which may induce or prolong unhealthy behaviour. 22 In our study, there were no respondents who indicated they felt no need to improve their lifestyle, as was also reported by Paddinson et al. 23 for diabetes screening. By contrast, Tijmstra found some evidence for this ‘certificate of health’ perception in screening for microalbuminuria. 21
Conclusions and implications for further research
In this study, we found that consumers have great confidence in self‐tests. They generally do not doubt the test result, unless performing the test is difficult or the test result deviates from what they expect. When we discussed the validity of the test, our respondents generally did not mention the possibility that the test can give a false‐positive or false‐negative result. Moreover, consumers do not seem to weigh the pros and cons before engaging in self‐testing. This stresses the need for easy‐to‐understand consumer information on the pros and cons and validity of self‐tests. We found that some self‐testers did not visit a doctor even when receiving an abnormal test result: one of the reasons for this was not having appropriate information on what to do with the result. The results regarding the perceived need for information, combined with expert opinions on adequate consumer information, should be used to develop new, accessible information for consumers who are considering performing a self‐test for cardiovascular risk factors.
Source of funding
This study was financially supported by the Netherlands Organization for Health Research and Development (ZonMw, The Hague, the Netherlands) and CAPHRI, the School for Public Health and Primary Care (Maastricht, the Netherlands).
Conflicts of interests
The authors declare they have no competing interests.
References
- 1. Ryan A, Wilson S, Greenfield S, Clifford S, McManus RJ, Pattison HM. Range of self‐tests available to buy in the United Kingdom: an Internet survey. Journal of Public Health (Oxford, England), 2006; 28: 370–374. [DOI] [PubMed] [Google Scholar]
- 2. CVZ‐rapport. Diagnostische zelftests op lichaamsmateriaal. Aanbod, validiteit en gebruik door de consument [Diagnostic self‐tests on bodymaterial. Supply, validity, and use by the consumer], 2007.
- 3. Ronda G, Portegijs P, Dinant GJ, Buntinx F, Norg R, Van der Weijden T. Use of diagnostic self‐tests on body materials among Internet users in the Netherlands: prevalence and correlates of use. BMC Public Health, 2009; 9: 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pavlin NL, Gunn JM, Parker R, Fairley CK, Hocking J. Implementing chlamydia screening: what do women think? A systematic review of the literature. BMC Public Health, 2006; 6: 221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Skolnik HS, Phillips KA, Binson D, Dilley JW. Deciding where and how to be tested for HIV: what matters most? Journal of Acquired Immune Deficiency Syndromes, 2001; 27: 292–300. [DOI] [PubMed] [Google Scholar]
- 6. Campbell S, Klein R. Home testing to detect human immunodeficiency virus: boon or bane? Journal of Clinical Microbiology, 2006; 44: 3473–3476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Borriello SP. Science, medicine, and the future. Near patient microbiological tests. BMJ, 1999; 319: 298–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. van Dommelen L, van Tiel FH, Ouburg S et al. Alarmingly poor performance in Chlamydia trachomatis point‐of‐care testing. Sexually Transmitted Infections, 2010; 86: 355–359. [DOI] [PubMed] [Google Scholar]
- 9. Ryan A, Greenfield S, McManus R, Wilson S. Self‐care – has DIY gone too far? British Journal of General Practice, 2006; 56: 907–908. [PMC free article] [PubMed] [Google Scholar]
- 10. Nielen MM, Schellevis FG, Verheij RA. The usefulness of a free self‐test for screening albuminuria in the general population: a cross‐sectional survey. BMC Public Health, 2009; 9: 381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Deutekom M, Aziz Y, van DisI, Stronks K, Bossuyt PM. [The Dutch National Cholesterol Test: participants mainly healthy]. Nederlands Tijdschrift voor Geneeskunde, 2008; 152: 2425–2429. [PubMed] [Google Scholar]
- 12. Janz NKCV, Strecher VJ. The Health Belief Model In: Glanz KRB, Lewis FM. (ed.) Health Behavior and Health Education: Theory, Research, and Practice, 3rd edn San Francisco: Jossey‐Bass, 2002: 45–66. [Google Scholar]
- 13. Bartolomew LK, Parcel GS, Kok G, Gottlieb NH. Behavior‐oriented theories used in health promotion In: Bartolomew LKPG, Kok G, Gottlieb NH. (ed.) Planning Health Promotion Programs: An Intervention Mapping Approach, 1st edn San Francisco, CA: Jossey‐Bass, 2006: 81–135. [Google Scholar]
- 14. Rosenstock IM, Strecher VJ, Becker MH. The health belief model and HIV risk behavior change In: DiClemente R, Peterson JL. (ed.) Preventing AIDS: Theories and Methods of Behavioral Interventions. New York, NY: Springer, 1994: 5–24. [Google Scholar]
- 15. Janz NK, Becker MH. The Health Belief Model: a decade later. Health Education Quarterly, 1984; 11: 1–47. [DOI] [PubMed] [Google Scholar]
- 16. Grispen JE, Ickenroth MH, de Vries NK, Dinant GJ, Ronda G, van der Weijden T. Improving behaviour in self‐testing (IBIS): study on frequency of use, consequences, information needs and use, and quality of currently available consumer information (protocol). BMC Public Health, 2010; 10: 453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Green J, Thorogood N. Qualitative Methods for Health Research. London: SAGE publications Ltd, 2004. [Google Scholar]
- 18. Ryan A, Ives J, Wilson S, Greenfield S. Why members of the public self‐test: an interview study. Family Practice, 2010; 27: 570–581. [DOI] [PubMed] [Google Scholar]
- 19. van der Weijden T, Bos LB, Koelewijn‐van Loon MS. Primary care patients’ recognition of their own risk for cardiovascular disease: implications for risk communication in practice. Current Opinion in Cardiology, 2008; 23: 471–476. [DOI] [PubMed] [Google Scholar]
- 20. Adriaanse MC, Snoek FJ. The psychological impact of screening for type 2 diabetes. Diabetes Metabolism Research and Reviews, 2006; 22: 20–25. [DOI] [PubMed] [Google Scholar]
- 21. Tijmstra T, Spijkers W, Broer J, Janssen WM, de Jong PE. [Psychosocial consequences of screening for microalbuminuria and for some other risk factors]. Nederlands Tijdschrift voor Geneeskunde, 2000; 144: 2460–2464. [PubMed] [Google Scholar]
- 22. Tymstra T, Bieleman B. The psychosocial impact of mass screening for cardiovascular risk factors. Family Practice, 1987; 4: 287–290. [DOI] [PubMed] [Google Scholar]
- 23. Paddison CA, Eborall HC, Sutton S et al. Are people with negative diabetes screening tests falsely reassured? Parallel group cohort study embedded in the ADDITION (Cambridge) randomised controlled trial. BMJ, 2009; 339: b4535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ickenroth MH, Ronda G, Grispen JE, Dinant GJ, de Vries NK, van der Weijden T. How do people respond to self‐test results? A cross‐sectional survey. BMC Family Practice, 2010; 11: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]


