Abstract
Background Little is known about peoples’ self‐management experiences and their desires or expectations to engage in self‐management. As such, there is little understanding about individuals’ perceived cues and barriers to engagement in self‐management, particularly in people affected by cancer.
Objective To understand cues and barriers to people’s engagement in self‐management during chemotherapy treatment for colorectal cancer.
Design Secondary analysis of qualitative data from mixed methods, longitudinal study.
Setting and participants Eleven participants undergoing treatment for colorectal cancer. Semi‐structured interviews were conducted twice with each participant, at the start and end of a 6‐month course of chemotherapy treatment in a Scottish cancer centre.
Results Cues and barriers to engagement in self‐management appeared to stem from perceptions of the impact and associated severity of side effects experiences as well as the perceptions about the efficacy of chosen self‐management activities and perceptions of control in minimizing the consequences of cancer treatment. Severe, episodic or unexpected side effects coupled with perceptions of uncertainty, lack of control and lack of adequate preparation to engage in self‐management were identified as key barriers to engagement.
Discussion and conclusion Participants’ reflection on, or appraisal of, their treatment‐related experiences and personal abilities, confidence and preferences to manage the impact of these shaped their subsequent engagement in self‐management. The findings highlight the importance of understanding individual’s self‐management experiences, perceptions, preferences, priorities and needs to help support, prepare and enable them to feel capable and confident to engage actively and effectively in self‐management.
Keywords: colorectal cancer, engagement, patient‐centered care, secondary qualitative analysis, self‐management
Introduction
Increasing interest in self‐management within health‐services research, policy and practice has led to an emphasis on the importance of creating opportunities to encourage, support and to enhance engagement in self‐management – purportedly the crux of global long‐term condition management. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 People affected by cancer face complex challenges in managing the short‐and long‐term impact of undergoing cancer treatments. 12 Like in other long‐term conditions, people affected by cancer are often expected to follow complex treatment regimens, engage in careful monitoring of their condition or health status, make lifestyle changes and learn how to balance their self‐management priorities and preferences with those of professionals. 12 , 13 , 14 Although the terms self‐care and self‐management are often used interchangeably, the National Cancer Survivorship Initiative 15 recently described self‐management as the ‘awareness and active participation by the person in their recovery, recuperation and rehabilitation, to minimize the consequences of treatment, promote survival, health and well‐being’, clearly situating ‘cancer’ within the long‐term condition arena.
The increasing emphasis on self‐management for people affected by cancer and long‐term conditions appears to be situated within a policy context of recommendations focusing on the increasing roles for, and responsibilities of, patients in managing and maintaining their health and well‐being. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 These policies, both United Kingdom (England and Scotland) and global (including, Australia, Canada, United States of America), acknowledge the many factors behind this movement; increasing prevalence of chronic disease, our global ageing populations, the interplay between health and lifestyle and behavioural risk factors and improvements in survival from advances in medical treatments, therapies and techniques. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 Thus, there now exists a plethora of governmental policies, frameworks, publications and strategies from across the World targeting chronic disease and long‐term condition management. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 In each of these documents, moves towards supporting self‐management appear to be being encouraged at a local, national and international level and networks, frameworks, services and programmes being promoted, developed and redesigned to support and encourage people’s engagement in self‐management. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 Each attempt to outline key features and outcomes of successful self‐care/self‐management and call for a shift in focus away from a culture of care dependency and demand‐led behavior towards a culture of patient engagement, shared decision making and self‐management. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11
The global interest in self‐care, and self‐management, is further evidenced in the growing number of interventions designed to promote engagement in self‐management or to test the effectiveness of being actively engaged in self‐management on a range of physical and psychological outcomes. On the whole, however, these studies have failed to demonstrate anything other than modest effects on physical outcomes, cost‐saving potential and have had a particularly disappointing impact on the use of healthcare services. 16 , 17 , 18 , 19 What’s more, they have frequently failed to engage with significant groups of people such as older people and people from deprived backgrounds 20 , 21 – arguably, the people who may be in greatest need of self‐management support and who experience the greatest challenges in accessing it. 22 , 23 The emerging discourses and narratives around self‐care and self‐management also reveal that the expectation that patients will naturally assume more active roles and take on self‐management responsibilities do not often map neatly onto peoples’ actions, experiences, desires or personal expectations for engaging in self‐management. 24 , 25 , 26 Despite these issues, the concepts of self‐management and self‐care continue to feature as a prominent strategy of health policies around the World as a well rehearsed route towards improved health, well‐being and quality of life as well as cost efficiency of service delivery. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11
Theoretically, self‐management appears to be an inherently person‐centered and individualistic approach, however, the evidence base reveals that there is still a great deal about individuals’ engagement in self‐management that we do not know. In particular, we know little about how and why people engage (or do not engage) in self‐management and what it means to them, particularly among people with cancer. Indeed, one could argue that the poor impact of self‐management support interventions may be attributed to a failure to understand and address how peoples’ individual needs, experiences, expectations, perceptions and priorities shape their attitudes towards, and subsequent behaviours in, engaging in self‐management. Hence, this appears to go against the concept of patient‐centred care, defined by Rodgers et al. 27 as ‘responsiveness to patient needs and preferences, using the patient’s knowledge to guide actively the interaction and information given, and shared decision making’ (p226). Policy makers, researchers and practitioners who are designing and delivering self‐management interventions hope to engage as many people as possible. To this end, it is imperative that health professionals, policy makers and the others involved in the development and delivery of health services and self‐management support interventions, become more attuned and responsive to peoples’ self‐management needs and priorities and to the ways in which they can and wish to be supported to engage in self‐management. It is imperative, therefore, to start by seeking a more nuanced understanding of the potential factors that are likely to influence peoples’ engagement in self‐management. This article presents a secondary qualitative analysis of the findings from longitudinal, mixed methods, exploratory study into peoples’ experiences of self‐management while undergoing chemotherapy for colorectal cancer. The article aims to identify and contextualize possible cues and barriers to engaging in self‐management, in relation to ‘minimizing the consequences of treatment’. 15
Methods
Study design
This article reports on the secondary analysis of qualitative data from an existing data set which was collected by the author for the initial purposes of understanding how people undergoing chemotherapy treatment for colorectal cancer perceived and engaged in their self‐management. The research study was originally undertaken as part of the author’s doctoral research. The analytical focus of the research at this time was on understanding participants meanings of self‐management and the nature of the activities that they engaged in, 25 changes in engagement in self‐management activities over time 28 and the role of perceived behavioural control in shaping participants attitudes towards, and patterns of engagement in, self‐management. 29
Semi‐structured interviews were conducted at two time points: once at the beginning of their course of treatment (T1) and once the end of their course of treatment (6 months later) (T2). The interview schedule, although guided by the theoretical framework (see below), deliberately opened with a broad, ‘grand tour question’ 30 ; ‘can you tell me how things have been since you were diagnosed/during your treatment?’ before moving on to ask about self‐management activities and beliefs. The interviews did not set out to originally capture information on why people did not engage in their self‐management per se, however, it became clear during the emerging analysis that this was a feature of many of the participant’s narratives and could offer a rich insight into understanding into specific cues and barriers to participants’ engagement in self‐management. This secondary analysis, aims to shed light on some of the factors that appeared to be influential in participant’s self‐management decision‐making during their course of treatment. In this way, the secondary analysis aimed to generate ‘new’ findings from analysing old data with a different research question. 31 , 32 , 33
Data for the original mixed method study were collected at the Beatson West of Scotland Cancer Centre (Scotland, UK) between March 2005 and January 2007. Ethical approval for conducting the study was received from the Local NHS and University Ethics Committees. A mixed methods, longitudinal design was adopted to understand whether perceptions towards, and behaviours in, engaging (or not engaging) in self‐management changed over time. The findings from the analysis of the original study, however, reported no change over time in patterns of engagement in self‐management. Similarly, no changes over time were identified in the current secondary analysis of cues or barriers to engagement in self‐management. The following article, therefore, presents excerpts from the interviews treated as a whole rather than as a comparison between T1 and T2.
Theoretical framework
Leventhal et al.’s 34 , 35 , 36 Self Regulation Model (Fig. 1) was chosen as the theoretical framework for the study because of its ability to offer a theoretical understanding as to how individuals conceptualize the nature of, and develop beliefs or perceptions about, their illness and how these are used to frame their coping and self‐management behaviours. The framework was used to guide both the content of the interview schedules and to inform the data analysis.
Figure 1.
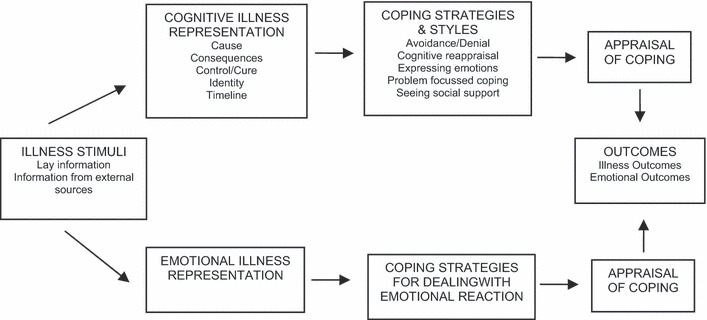
Leventhal’s Self Regulation Model.
Participants
All participants commencing a 6‐month course of chemotherapy treatment (the Mayo Clinic regimen: intravenous administration of 5‐flurouracil and leucovorin once per month for 6 months) were invited to participate in the research. The sample was restricted to ensure homogeneity in terms of treatment type so that individuals’ experiences of engaging in self‐management could be understood within a similar context. No additional inclusion criteria were applied to the sample. A convenience, consecutive sampling strategy was employed to ensure that as many people as possible, who were undergoing this particular treatment regimen, were invited to participate during the course of the study. This broad inclusive approach aimed to capture the plurality and diversity of experiences between men and women, of different ages, and from different socioeconomic backgrounds, who were undergoing the same course of treatment to provide a nuanced understanding of their engagement in self‐management. All eligible participants were introduced to the researcher by clinical staff who discussed the nature and requirements of the study with them. Willing participants gave written, informed consent.
In the original study, a total of 33 potentially eligible participants were approached to consider participating in the study; of these 31 consented to participate, and 24 were included in the final mixed method analysis. Table 1 shows the reasons for refusals to participate, withdrawals and exclusions during the course of the study. No significant differences were identified between those who participated and those who withdrew/were excluded during the course of the study.
Table 1.
Reasons why patients refused to participate, withdrew or were excluded from the study
| Reason | Frequency (n) |
|---|---|
| Refusals | |
| Had too much going on at that particular time (around diagnosis) | 1 |
| Did not wish to discuss their thoughts and feelings about their diagnosis and treatment | 1 |
| Withdrawals | |
| Study required too much focus on diagnosis and ensuing treatment | 2 |
| Exclusions | |
| Did not return any/complete data | 2 |
| Wished to discontinue all treatment | 1 |
| Mayo chemotherapy regimen discontinued because of renal failure (caused by severe toxicity) | 1 |
| Mayo chemotherapy regimen discontinued because of disease progression | 1 |
For the qualitative component in the original study, a subsample of 11 participants agreed to participate in the semi‐structured interviews. The demographic profiles of the participants are shown in Table 2. The majority of participants were men, aged between 60 and 70 years, reflected a spread of social classes and had been diagnosed with Dukes’ C stage (Stage 3) colorectal cancer (where the tumour has spread beyond the bowel wall and into the surrounding lymph nodes and is associated with a 48% 5‐year survival rate).
Table 2.
Demographic characteristics of patients who participated in the semi‐structured interviews
| Case | Age (years) | Gender | Social class | Stage of disease (Dukes’) | Performance status | Level of co‐morbidity | Social circumstances |
|---|---|---|---|---|---|---|---|
| 1 | 59 | Male | 4 | C | 1 | 1–2 | Lives with spouse/partner |
| 2 | 69 | Female | 6 | C | 0 | 1–2 | Lives with spouse/partner |
| 8 | 68 | Male | 6 | C | 0 | 3+ | Lives with spouse/partner |
| 10 | 74 | Male | 4 | C | 0 | 1–2 | Lives alone |
| 11 | 59 | Male | 7 | C | 0 | 0 | Lives with spouse/partner |
| 12 | 69 | Male | 7 | C | 0 | 1–2 | Lives with spouse/partner |
| 17 | 69 | Male | 5 | C | 0 | 0 | Lives with spouse/partner |
| 19 | 74 | Male | 2 | C | 0 | 1–2 | Lives with spouse/partner |
| 22 | 55 | Female | 3 | C | 0 | 1–2 | Lives alone |
| 24 | 49 | Female | 5 | B | 0 | 0 | Lives with spouse/partner |
| 31 | 76 | Male | 6 | C | 0 | 1–2 | Lives alone |
Interview procedure
Participants were invited to take part in two semi‐structured, face‐to‐face interviews with at the beginning and end of their course of treatment. Interviews were conducted in a hospital setting, lasted between 30–60 min and were tape recorded by the researcher for the purpose of transcription and analysis. The semi‐structured interview schedule, although guided by the theoretical framework, was flexible to respond to patients’ cues or responses as the interview progressed to encourage participants to lead the conversation and provide avenues for exploration during the interview.
Data analysis
The interview data were analysed using Framework Analysis which involved the following steps: familiarizing oneself with the data, developing a thematic framework, indexing, charting and mapping and interpretation. 37 The emerging thematic framework was broadly guided by the SRM and a process of open coding to identify key themes identified from the data itself. The original analysis ended following the 11th interviewee as the researcher was confident that no new themes were identified in relation to the original analytical focus. A sub‐sample of the transcripts (10%) was read and analysed by a second researcher for the purposes of verification of the emerging thematic framework. No disagreements were found between both researchers.
Results
The identified themes appeared to relate to the ‘representation’ and ‘appraisal’ stages of Leventhal’s Self Regulation Model. The ‘representation’ stage corresponds to the person’s interpretation of the threat posed by the illness; or in this case, the consequences brought about by undergoing treatment for cancer. The ‘appraisal’ stage corresponds to people’s evaluation of their coping behaviors; in this case, their evaluation of the success of, or their control over, their self‐management efforts. The identified themes and exemplars are presented in more detail in the following section; (i) consequences – the significance of side effect experiences, (ii) controllability – the importance of personal control, and, (iii) perceived effectiveness of engaging in self‐management.
Consequences – the significance of side effect experiences
This theme emerged in relation to the consequences of how participants’ treatment‐related experiences impacted upon them and their subsequent engagement in self‐management. A very distinct pattern emerged from the data between symptom severity and likelihood of engaging in self‐management. Several of the participants commented that they had experienced minimal, predictable or minor side effects throughout the course of their treatment and therefore, came to learn how to effectively manage these themselves. This appeared to enhance their perceptions of their abilities and confidence to cope with and self‐manage the side effects:
I know that some of the symptoms can change as you go through but I’ve not been like that. I’ve been fairly steady all the way through…just tiredness and a bit sick. I think when you go through the same things, you start to know what’s coming up and it’s fine if it stays like that then you know how to cope [with the side effects]. I just did the same things [self‐management] because they worked for me.
(Pt 1, male, age 59 years)
I knew what was coming. I had a week of chemo…you know it stopped on the Friday and by the Sunday or Monday, I had the sore mouth. It wasn’t mouth ulcers, it was just you couldn’t take anything hot so I used to drink liquids through a straw. The week after that was the week when you felt very tired and then the week after that you felt better. So I think because it was a kind of regular pattern, you got to know the pattern and I felt able to cope okay with it all.
(Pt 2, female, age 69 years)
On the other hand, those who experienced episodic, or increasingly severe, side effects talked of greater challenges in engaging in self‐management, possibly hindering their engagement. Some participants also reported difficulties in distinguishing whether the side effects they were experiencing were attributed to their treatment or to something else. As the following example illustrates, these experiences and perceptions often led to feelings of loss of control and reduced self‐efficacy (confidence in one’s own abilities) to engage in self‐management:
My side effects have fluctuated and changed each month. Some have been core ones you know but some different ones and at different times. It’s sometimes difficult to tell whether things are side effects of whether there is anything else wrong with me. I don’t feel totally in control of some of the things you know, I do the best I can to help with it but I’m aware that things flare up so no I don’t have control over it.
(P22, female, age 55 years)
Conversely, for a few of the participants, the experience of increasingly or unexpectedly severe side effects led some of the participants to engage in preventative self‐management (as opposed to ‘routine’ self‐management to ‘treat’ or manage their side effects). In these cases, people appeared to reflect upon their previous experiences (linked to the ‘appraisal’ stage of Leventhal’s Self Regulation Model) which informed their subsequent engagement in their future self‐management. For the more pro‐active self‐managers in the sample (e.g. Pt 24), who appeared to be more assertive and comfortable with regards to their self‐management decision making, this involved taking a high degree of personal responsibility for their self‐management and actively planning and adjusting preventative self‐management activities as necessary.
I had quite bad diarrhea [during treatment] but I chose not to do anything about it because I had a tendency to obstruct. I was concerned that if I took [the medication], it might go the opposite way and I didn’t want that to happen so next time it just lasted two or three days but it passed.
(P24, female, age 49 years)
For the more passive self‐managers in the sample (e.g. Pt 31), who appeared to be more reliant on health professionals for most aspects of their self‐management and self‐management decision making, this involved being led towards a new preventative self‐management regimen by medics. They often also spoke of their intentions to adhere consistently to this regimen in their future self‐management efforts (usually involving the use of medications predominantly to relieve side effects).
So then I started the chemo and I was okay but four days down the line I started being sick and the vomiting just got worse and it just became really horrendous. I went nearly a whole week where I was continually vomiting. When it came to the second lot of chemo, the doctor said we’ll start you on anti‐sickness pills and what we want you to do is take the pills before you feel sick because prevention is easier to cope with rather than waiting till the problems start. I said ‘well I know that now’…so I did exactly as the doctor suggested and everything went well. I felt that I was coping with the situation and what I was doing was the right things and it was preventing situations from getting out of hand.
(P31, male, age 76 years)
For others, engaging in ‘preventative’ self‐management appeared to be unlikely, mostly due to their perceptions surrounding the use of medications. Several of the participants spoke of their reluctance to take medication. This, they perceived, was mostly due to perceived lack of need, a preference to wait till the side effects passed, or fears of not knowing what medications to use.
I spoke to the nurse there, she’s recommended I take nausea pills…two, three times a day…but I’m the kind of person that doesnae like taking pills. I’d rather grin and bear it. Aye, I’m no’ a person that sort of likes to take medication, I’ll grin and bear it and if that doesn’t work or I feel it getting worse, then I might take it. The second lot [cycle of chemotherapy] I think I did have a sore head or something like that and I wasnae sure whether I’d be able to take medication…aspirin or whatever…
(Pt 11, male, age 59 years)
I used them [mouth pastilles] when I felt my mouth was sore…no I didn’t take anything to warden it off, I just waited till they came on and then took it…I’m no’ a great one for taking things if I don’t think they’re needed. No, I didn’t take them constantly, just when I felt I needed to take them.
(Pt 19, male, age 74 years)
Controllability – the importance of personal control
This theme related to the degree to which individuals believed that the effects of their treatment could be controlled and the part that they played in doing so. In the following example, one woman clearly states that although she engaged in self‐management, at no time during her treatment did she perceive herself as having control over influencing the onset and nature of her side effect experiences.
The main symptoms I remember feeling dreadful about were sickness, feelings of nausea and mouth ulcers…I felt that the anti‐sickness tablets helped me, I didn’t feel great but I knew I could get the tablets and mouthwashes and things like that but I started to dread each month because despite the fact I knew I could get these things I knew I would have the symptoms anyway…they wouldn’t stop. I didn’t feel it [her self‐management] was effective enough for me to think “I’m in control of this”.
(Pt 22, female, age 55 years)
Participants’ narratives revealed that ‘controllability’ was linked to three main aspects related to engaging in self‐management: uncertainty, expectation for responsibility for self‐management and preparation. As also shown in some of the earlier themes and exemplars, several of the participants voiced their fears at not being able to understand the nature of their side effects, not being confident in controlling these through their own self‐management and their uncertainty over when and how best to engage in self‐management; all of which may have hindered their engagement. The following examples reveal how perceptions of uncertainty can make it difficult for people to know how and when to engage in recommended self‐management activities:
There are times when you’re not sure if something is wrong. If it goes wrong and then levels out [the side effects], then you begin to think ‘well do I need to take these tablets now?’, ‘can I stop taking these?’…you’re never sure.
(P10, male, age 74 years)
I’ve taken anti‐diarrhoea tablets once where I had a few days that were bad but mostly I prefer not to take those cos I’m still coming to terms with the stoma and what it’s doing. Sometimes I know it’s maybe a different food I’ve tried and it’s not necessarily it [the chemotherapy]. That’s one of the things that you’re not sure about…whether it’s side effects of if it’s foods so I’m kind of laying off the anti‐diarrhoea tablets unless it becomes dire.
(Pt22, female, age 55 years)
Related to ‘controllability’ were peoples’ perceptions about, and expectations related to, responsibility attribution for their self‐management. While several of the participants appeared to be more ‘proactive’ self‐managers and expected to assume a degree of responsibility for their self‐ management, there were others who were regarded as more ‘passive’ self‐managers (e.g. Pt 10, Pt 17) because they regarded self‐management to be solely the responsibility of health professionals. Health professionals were frequently regarded as ‘health experts’:
If the staff or doctors suggested anything I would take it…what I tried to do was follow their advice because they know best, they’ve seen my condition before, I’ve never had it. So if they said to me try such and such, I said yes certainly and if it worked, I kept doing it.
(P10, male, age 74 years)
I don’t think I’ve got any control [over the side effects]…the nurses and the doctor were in charge of what was happening…she reduced my dosage [of chemotherapy] because I’d had diarrhea that was quite severe and that helped…but no, I’ve not had a great deal of control over it.
(Pt 17, male, age 69 years)
The analysis demonstrated that doubts about controllability and expectations were not uncommon amongst many of the participants. Moreover, however, their accounts revealed that many of them felt inadequately prepared to expect, or be able, to assume responsibility for their self‐management. It was commonly perceived that they had not been given sufficient or specific information about the nature of their treatment, its likely impact on them and their anticipated role in preventing or alleviating this impact through their own personal self‐management efforts:
I didn’t feel I had enough information the first time back at the very start when the symptoms hit me. I had no medication and I didn’t know what was happening. I didn’t know what to do…I knew symptoms were caused by the chemotherapy but I didn’t know how extensive they were going to be and how long it was going to last. I was completely flummoxed by it all.
(P31, male, age 76 years)
Participants accounts revealed that not only were they given little information at times to prepare them for assuming responsibility for their self‐management, but at times, also perceived little opportunity from health professionals to help them engage in self‐management. Several of the participants commented on the mismatch between their own and health professional’s ideas or priorities around self‐management and self‐management activities. In the following example, one woman reveals the tension experienced when articulating her personally defined self‐management needs and making these needs understood to her healthcare team:
I’ve got a stronger mouth wash [to treat mucositis] but I’m still trying to convince somebody to give me a throat spray…because they can’t understand why I can’t gargle [the mouthwash]…but if you’re feeling nauseous anyway and I’m not good at gargling at the best of times. It’s impossible.
(P22, female, age 55 years)
Perceived effectiveness of engaging in self‐management
As shown throughout the findings, participants’ reflections on, or appraisal of, particular experiences (i.e. the effectiveness of their self‐management) led them to view or engage in self‐management in a particular manner. For some of the participants, the effectiveness of medications for relieving or preventing side effects from occurring may have prompted further and prolonged use of these specific strategies. In the following example, one man implied that the effectiveness of the medication appeared to offer a sense of agency and prompted further use:
The second time I had very slight diarrhoea. I found I took [the medication] and the diarrhoea just stopped. Once I noticed it’s too liquidy, I took the [medication] and magic…so I felt very confident in that…all I have to do is take [the medication]. So now I’ve got the loperamide for the diarrhoea, the domperidone for the anti‐sickness and so I feel these are the tools I’ve got to combat the side effects.
(P31, male, age 76 years)
On the other hand, another participant’s account suggested that perceived effectiveness may be unrelated to continued engagement in self‐management. In this example, one woman comments that despite the fact that her self‐management often did little to prevent or alleviate her side effect experiences, she reports that she continued to engage in self‐management nonetheless:
It didn’t stop me doing the self‐care things…I did it because I know it alleviated the symptoms a little but at no point did I feel in control of it. I knew I could help with it but I knew I couldn’t stop the symptoms and prevent them and I felt really quite down and depressed about it. I always took all the remedies and did all the things like using mouth rinses and drinking, trying to eat healthily, but I was aware that it had a limited capacity to help me you know?
(P22, female, age 55 years)
Discussion
Overwhelmingly, just as is theorized in Leventhal’s Self Regulation Model, the findings offered a clear sense that people reflected on, or appraised, their experiences and focused on possibilities for, and the likelihood of, engaging in self‐management based on these. Like in self efficacy theory – relating to people’s confidence in engaging in self‐management – people’s actions appeared to be guided by previous experience and/or forethought 38 ; people formed beliefs about what they could do, what the likely outcomes of their engagement in self‐management would be and set goals for themselves accordingly. In particular, the findings revealed that engagement and indeed, non‐engagement, in self‐management may be influenced by peoples’ perceptions of the consequences and personal impact of their treatment and its effects, the controllability of such impact and their personal role in this, and the perceived effectiveness of their self‐management efforts.
In relation to symptom severity, the experience of minimal or anticipated side effects and the perceived control over, and possible effectiveness of, chosen self‐management strategies in alleviating or preventing these, appeared to shape the likelihood of peoples’ engagement in their self‐management. Subsequently, increasingly severe, episodic or unexpected side effect experiences, perceived lack of control over and inadequate preparation for assuming an active role in self‐management, have the likely effect of reducing peoples’ perceptions of control, confidence (or self‐efficacy) and perceived ability with which to successfully manage such effects. As a result, these experiences and perceptions may be more likely to lessen the likelihood of their engagement. A couple of caveats to this, however, were identified. It appears that there may be a distinction between ‘routine’ and ‘preventative’ self‐management, where the experience of increasingly severe side effects appeared to prompt engagement in self‐management rather than hinder it among several of the participants in the study. To explain further, the findings demonstrated that the severity, significance or impact of these experiences prompted several of the participants’ desire to engage in self‐management to help them feel in control and to prevent them from experiencing such side effects as intensely in the future. Therefore, rather than reducing agency and perceptions of control, these experiences actually intensified their sense of agency and perceptions of control to take charge of their self‐management, whether these were prompted by their own judgment or by medical advice. Conversely, these interpretations were supported in view of the fact that other participants who did not engage in preventative self‐management simply did not perceive that there was a need to focus on engaging in preventative behaviour. Other studies have also reported similar findings. 25 , 26 , 27 In relation to existing evidence, there has been a suggested link between side effect severity, perceptions of control and engagement in self‐management, 39 , 40 although equally there is evidence to suggest that increased perceptions of control and proactive engagement in self‐management are not necessarily a result of improvements in disease severity or symptom control. 18 , 41
It cannot also be concluded from the findings presented herein that perceived ineffectiveness of chosen self‐management strategies leads one to engage in less self‐management behaviour. Although the opposite finding – that perceived effectiveness prompted engagement in self‐management – clearly emerged from the secondary analysis of the data, even where participants perceived their self‐management to have been less effective they continued to engage in self‐management. One might question whether this is because they wish to continue to be seen as a ‘good patient’, like in Collins et al.’s 42 study of passive self‐managers who followed their prescribed self‐management routine but were less likely to proactively question this or adjust it in light of its ineffectiveness? Or is it because psychologically, it makes them feel as if they are attempting to take control over their self‐management regardless of its effectiveness? Additional examination of this relationship and the reasons behind this would be welcomed.
To our knowledge, this is the first study to offer an understanding about non‐engagement in self‐management during chemotherapy treatment for cancer. The secondary analysis of this existing data set raises some key questions and highlights areas for discussion and additional research. The findings make an important contribution to the evidence base on engaging in self‐management as they help to reveal additional insights into how we can help patients engage in self‐management but from a different angle to simply asking them what they do as part of their self‐management during treatment. On the one hand, the generalizability and potential transferability of the findings from this study are somewhat limited by its’ sampling framework – the focus on one small, specific group of patients with colorectal cancer, who were receiving a very particular treatment regimen and in one clinical site in the West of Scotland. On the other hand, situating ‘cancer’ within the context of the long‐term condition arena, means that the findings speak to the growing body of literature on engaging people with long‐term conditions in self‐management and potential barriers and facilitators to this. This secondary analysis highlights the nuanced account that can be achieved through a qualitative approach and the importance of this for understanding and highlighting how individuals and their perceptions, beliefs, priorities and needs may shape their engagement in self‐management. The findings are therefore highly relevant to any discussion on how to structure and design healthcare services and interventions to support and promote engagement of people with long‐term conditions through tailored and personalized self‐management support. They also contribute to the debates around the push towards encouraging self‐management, expectations that patients wish to, and can, assume responsibility for this role and the true patient‐centered nature of self‐management approaches. 43 Additional work exploring the issues identified here in people undergoing treatment for other cancers and indeed at the point of completion of treatment and in the survivorship periods beyond this, would be welcomed. In particular, a greater understanding of the relationship between side effect experiences and engagement in both preventative and routine self‐management would be valuable.
There is little evidence on barriers and facilitators to engaging in self‐management and the relevance and effectiveness of existing forms of self‐management support from the patients’ perspective, particularly those with cancer. It is helpful, however, to situate these findings within the wider context of supporting and sustaining engagement in self‐management where there are clear parallels with previous research findings on the illness experiences of people with diabetes, 42 heart failure, 16 , 44 and asthma 45 and other chronic illnesses. 46 Despite the growing literature base around self‐management, we know little about engagement in different types of self‐management or where the self‐management takes on a different purpose or goal, for example, the distinction reported here between engagement in routine or preventative self‐management. Several questions remain unanswered; what does self‐management actually mean to people? What self‐management do people do on a daily basis and how does this match with health professional’s perceptions of what constitutes self‐management? And, what roles do they assume in engaging in self‐management and in what contexts? The issue of what constitutes engagement in self‐management from different perspectives is an interesting one; is it about following prescribed regimens and advice from health professionals or about making a personal judgement about issues related to, and priorities for, self‐management even if these appear to go against the advice of medics or health professionals? The literature commonly alludes to this dichotomy, tending to view engagement in professionally‐led self‐management with compliance, 27 and consequently, non‐engagement as analogous with non‐compliance. Additional research, however, would be valuable to explore these issues in greater depth, as well as research which could help to further our understanding of the factors that influence or shape engagement in self‐management. This kind of formative work is important for informing the development and evaluation of patient‐centered, tailored and individualized mechanisms to promote, support and sustain engagement in self‐management.
The common thread arising from participants’ accounts in this study is the need to understand engagement, and non‐engagement, in self‐management from an individual perspective. The UK’s NHS is comparatively poor to other countries in providing individualized and tailored self‐management support to people. 25 Existing trials of self‐management support interventions have likely had such disappointing results because they have had little congruence with individuals’ own priorities for and preferences and perceptions towards engaging in self‐management. The findings from this secondary analysis concur with Lawn et al.’s 43 call for the need to respect patient choice, preferences and control. The heavy reliance on health professionals to take charge of symptom management during treatment is unsurprising when the findings here highlight how little people may be prepared to feel able and confident to meet the increasing expectation of assuming a proactive role in their self‐management. For many people, this role is simply not desired or possible. 43 Indeed, several studies have shown the different self‐management roles that people prefer to adopt and the common characteristics of these roles. 42 We need to be mindful of these preferences and rather than risk the danger of labelling people as ‘good’ or ‘bad’ self‐managers, identify ways to best support all individuals in light of their personal role preferences and capabilities for engaging in self‐management. The findings reported herein call for us to invite and unpack discourses on peoples’ experiences of engaging in self‐management, the contexts in which these occur and the external and internal forces that impact upon and shape attitudes towards, and engagement in, self‐management and with self‐management support.
Although the findings from this secondary analysis point us to directions for future research, the analysis is somewhat limited by the data which were available to examine a new research question or different angle of people’s experiences of self‐management. Indeed, as reported the original interview guide did not ask direct questions about people’s non‐engagement in self‐management. Direct probing of this would have been valuable for identifying additional insights into the issue of non‐engagement. Nor was it possible during a secondary analysis to combine simultaneous data collection and analysis, where new emerging insights could have been probed for additional detail or clarification. We also know little about whether or not cues and barriers to engagement in self‐management changed over time. Similarly, it is important to acknowledge that the perceptions of patients who declined to participate or withdrew from the original study may have had very different perceptions towards, and experiences of engaging (and not engaging) in self‐management. As a result, there are several new questions that arose during the secondary analysis that remain unanswered but do, however, provide avenues for future exploration.
The findings reported herein highlight that individuals’ differing perceptions, priorities, expectations, experiences and needs are likely to influence their patterns of engagement. Preparation for engagement in self‐management has to address these issues in an individualized and tailored manner for engagement to be truly meaningful and effective. The findings help to offer direction towards future research priorities and serve to remind us of the major challenges that lie ahead and that require additional research in this area to explore, understand and address. In particular, how do we ensure that self‐management support can be delivered in a patient‐centred, responsive and tailored manner? How do we ensure that self‐management priorities, needs and preferences as well as risk are assessed in a robust and clinically useful manner? And how do we encourage and prepare patients to view themselves as capable of taking responsibility for their own contribution to their recuperation and rehabilitation from illness and in improving their overall health and well‐being? Future discussion and research in this area would be particularly welcomed.
Funding and disclosure
This research was carried out as part of a post‐graduate studentship awarded by the Faculty of Human Sciences, University of Stirling. No conflicts of interest have been declared.
Acknowledgements
I would like to thank everyone who participated in the study and who gave their time and shared their experiences so willingly. I also wish to thank Professor Nora Kearney (University of Dundee), Professor Ronan O’Carroll (University of Stirling) and Dr Gill Hubbard (University of Stirling) for their supervision, and guidance with data collection and analysis. I also wish to thank Professor Paul Flowers (Glasgow Caledonian University) for his help with critical revising, editing and proof reading an early draft of the manuscript.
References
- 1. Department of Health . The Expert Patient: a New Approach to Chronic Disease Management for the 21st Century . London : Department of Health; , 2001. . [Google Scholar]
- 2. Scottish Executive . Partnership for Care: Scotland ’s Health White Paper . Edinburgh : Scottish Executive; , 2003. . [Google Scholar]
- 3. Department of Health . Supporting People with Long Term Conditions: an NHS and Social Care Model to Support Local Innovation and Integration . London : Department of Health; , 2005. . [Google Scholar]
- 4. Department of Health . Self‐care: a Real Choice . London : Department of Health; , 2005. . [Google Scholar]
- 5. Scottish Government . Improving Health and Wellbeing of People with Long Term Conditions in Scotland: an Action Plan . Edinburgh : Scottish Government; , 2009. . [Google Scholar]
- 6. Scottish Government . Better Health, Better Care . Edinburgh : Scottish Government; , 2009. . [Google Scholar]
- 7. National Health Priority Action Council (NHPAC) . National Chronic Disease Strategy . Canberra : Australian Government Department of Health and Ageing; , 2006. . [Google Scholar]
- 8. Queensland Health . Framework for Self‐Management 2008–2015 . Brisbane : Queensland Government; , 2007. . [Google Scholar]
- 9. British Columbia Ministry of Health . Primary Health Care Charter: a Collaborative Approach . British Columbia : Ministry of Health; , 2007. . [Google Scholar]
- 10. Wagner E , Austin B , Coleman C . It Takes a Region: Creating a Framework to Improve Chronic Disease Care . Oakland : California Healthcare Foundation; , 2006. . [Google Scholar]
- 11. Improving chronic illness care. ‘The Chronic Care Model’ . 2007. . Available at: http://www.improvingchroniccare.org/index.php?p=The_Chronic_Care_Model&s=2, accessed 17 January 2012 .
- 12. Davies N , Batehup L . Towards a personalized approach to aftercare: a review of cancer follow‐up in the UK . Journal of Cancer Survivorship , 2011. ; 5 : 142 – 151 . [DOI] [PubMed] [Google Scholar]
- 13. Hibbard JH , Mahoney ER , Stockard J , Tusler M . Development and testing of a short form of the Patient Activation Measure . HSR: Health Services Research , 2005. ; 40 : 1918 – 1930 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hibbard J , Greene J , Tussler M . Improving the outcomes of disease management by tailoring care to the patient’s level of activation . Ambulatory Journal of Managed Care , 2005. ; 15 : 353 – 360 . [PubMed] [Google Scholar]
- 15. NCSI, Research Work Stream Mapping Project . Summary and Reports for: Bowel Cancer, Breast Cancer, Lung Cancer, Prostate Cancer . London : National Cancer Survivorship Initiative; , 2009. . [Google Scholar]
- 16. Warsi A , Wang PS , LaValley MP , Avorn J , Solomon DH . Self management education programmes in chronic disease: a systematic review and methodological critique of the literature . Archives of Internal Medicine , 2004. ; 164 : 1641 – 1649 . [DOI] [PubMed] [Google Scholar]
- 17. Bury M , Newbould J , Taylor D . A Rapid Review of the Current State of Knowledge Regarding Lay‐Led Self Management of Chronic Illness: Evidence Review . London : National Institute for Health and Clinical Excellence; , 2005. . [Google Scholar]
- 18. Richardson G , Gravelle H , Weatherly H , Ritchie G . Cost effectiveness of interventions to support self‐care: a systematic review . International Journal of Technology Assessment in Health Care , 2005. ; 21 : 423 – 432 . [DOI] [PubMed] [Google Scholar]
- 19. Foster G , Taylor SJ , Eldridge SE , Ramsay J , Griffiths CJ . Self management education programmes by lay leaders for people with chronic conditions . Cochrane Database of Systematic Reviews , 2005. ; 4 : doi: 10.1002/14651858.CD005108 . [DOI] [PubMed] [Google Scholar]
- 20. Reeves D , Kennedy A , Fullwood C et al. Predicting who will benefit from an Expert Patient self management course . British Journal of General Practice , 2008. ; 58 : 198 – 203 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bower P , Blakeman T , Kennedy A et al. What Influences People to Self‐Care . Manchester : University of Manchester, National Primary Care Research and Development Centre; , 2009. . [Google Scholar]
- 22. Coulter A , Ellins J . Patient‐Focussed Interventions: a Review of the Evidence . London : Health Foundation; , 2006. . [Google Scholar]
- 23. Berzins K , Reilly S , Abell J , Hughes J , Challis D . UK self‐care‐support initiatives for older patients with long term conditions: a review . Chronic Illness , 2009. ; 5 : 56 – 72 . [DOI] [PubMed] [Google Scholar]
- 24. Clark AM , MacIntyre PD , Cruickshank J . A critical realist approach to understanding and evaluating heart health programmes . Health , 2007. ; 11 : 513 – 539 . [DOI] [PubMed] [Google Scholar]
- 25. Kidd L , Kearney N , O’Carroll R , Hubbard G . Experiences of self‐care in patients with colorectal cancer: a longitudinal study . Journal of Advanced Nursing , 2008. ; 64 : 469 – 477 . [DOI] [PubMed] [Google Scholar]
- 26. Cooper JM , Collier J , James V , Hawkey CJ . Beliefs about personal control and self management in 30–40 year olds living with Inflammatory Bowel Disease: a qualitative study . International Journal of Nursing Studies , 2010. ; 47 : 1500 – 1509 . [DOI] [PubMed] [Google Scholar]
- 27. Rodgers A , Kennedy A , Nelson E , Robinson A . Uncovering the limits of patient‐centredness: implementing a self‐management trial for chronic illness . Qualitative Health Research , 2005. ; 15 : 224 – 239 . [DOI] [PubMed] [Google Scholar]
- 28. Kidd L . An Exploration of Patients’ Perceived Control, Self Efficacy and Involvement in Self Care During Chemotherapy for Colorectal Cancer . Stirling : University of Stirling; , 2007. . [Google Scholar]
- 29. Kidd L , Hubbard G , O’Carroll R , Kearney N . Perceived control and involvement in self‐care in patients with colorectal cancer . Journal of Clinical Nursing , 2009. ; 18 : 2292 – 2330 . [DOI] [PubMed] [Google Scholar]
- 30. Spradley JP . The Ethnographic Interview . New York : Holt, Rinehart and Winston; , 1979. . [Google Scholar]
- 31. Gladstone BM , Volpe T , Boydell KM . Issues encountered in a qualitative secondary analysis of help‐seeking in the prodrome to psychosis . Journal of Behavioural Health Services and Research , 2007. ; 34 : 4 . [DOI] [PubMed] [Google Scholar]
- 32. Holland J , Thomson R . Gaining perspective on choice and fate: revisiting critical moments . European Societies , 2009. ; 11 : 3 . [Google Scholar]
- 33. Bornat J . Remembering and reworking emotions. The reanalysis of emotion in an interview . Oral History , 2010. ; 38 : 2 . [Google Scholar]
- 34. Leventhal H , Nerenz DR , Steel DJ . Illness representations and coping with health threats . In : Baum A , Taylor SE , Singer JE. ( eds ) Handbook of Psychology and Health , Vol 4 . New Jersey : Lawrence Earlbaum; , 1984. : 219 – 252 . [Google Scholar]
- 35. Leventhal H , Benyamini Y , Brownlee S et al. Illness representations: theoretical foundations . In : Petrie KJ , Weinman JA. ( eds ) Perceptions of Health and Illness: Current Research and Applications . Amsterdam : Harwood Academic Publishers; , 1997. : 19 – 45 . [Google Scholar]
- 36. Leventhal H , Leventhal EA , Cameron L . Representations, procedures and affect in illness self regulation: a perceptual‐cognitive model . In : Baum A , Revenson T , Singer J. ( eds ) Handbook of Health Psychology . New York : Earlbaum; , 2001. : 19 – 47 . [Google Scholar]
- 37. Ritchie J , Spencer L , O’Connor W . Carrying out qualitative analysis . In : Ritchie J , Lewis J. ( eds ) Qualitative Research Practice: a Guide For Social Science Students and Researchers . London : Sage Publications; , 2003. : 219 – 263 . [Google Scholar]
- 38. Bandura A . Self Efficacy: the Exercise of Control . New York : Freeman; , 1997. . [Google Scholar]
- 39. Bayliss EA , Steiner JF , Fernald DH , Crane L , Main DS . Descriptions of barriers to self‐care by persons with co‐morbid conditions . Annals of Family Medicine , 2003. ; 1 : 15 – 21 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pan LH , Tsai YF , Chen ML , Tang R , Chang CJ . Symptom distress and self‐care strategies of colorectal cancer patients with diarrhea up to 3 months after surgery . Cancer Nursing , 2011. ; 34 : E1 – E9 . [DOI] [PubMed] [Google Scholar]
- 41. Fraser DD , Kee CC , Minick P . Living with chronic obstructive pulmonary disease: insiders’ perspectives . Journal of Advanced Nursing , 2006. ; 55 : 550 – 558 . [DOI] [PubMed] [Google Scholar]
- 42. Collins MM , Bradley CP , O’Sullivan T , Perry IJ . Self‐care coping strategies in people with diabetes: a qualitative exploratory study . BMC Endocrine Disorders , 2009. ; 9 : 6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lawn S , McMillan J , Pulvirenti M . Chronic condition self‐management: expectations of responsibility . Patient Education and Counseling , 2011. ; 84 : e5 – e8 . [DOI] [PubMed] [Google Scholar]
- 44. Riegel B , Dickson V . A situation‐specific theory of heart failure self‐care . Journal of Cardiovascular Nursing , 2008. ; 23 : 190 – 196 . [DOI] [PubMed] [Google Scholar]
- 45. Loignon C , Bedos C , Sevigny R , Leduc N . Understanding the self‐care strategies of patients with asthma . Patient Education and Counseling , 2009. ; 75 : 256 – 262 . [DOI] [PubMed] [Google Scholar]
- 46. Anduluv A , Asplund K , Norbergh KG . Who’s in charge? The role of responsibility attribution in self management among people with chronic illness . Patient Education and Counseling , 2010. ; 81 : 94 – 100 . [DOI] [PubMed] [Google Scholar]


