Abstract
Context In a time of economic austerity, one of the most daunting questions is who decides on healthcare rationing? In the current study, we sought to examine if the public can in fact provide meaningful information regarding healthcare policy issues. Based on theories of public policy, this paper tries to find out if patients behave akin to ‘responsible citizens’ and can provide differentiated expectations between three healthcare dimensions.
Methods One thousand two‐hundred eleven individuals participated in a telephone interview. Participants were asked two series of questions, one regarding their views on the primary care, prevention and promotion practices they experience with their healthcare provider and one regarding the importance of these practices to them. We calculated a difference score representing the gap in each healthcare dimension.
Findings In all three healthcare dimensions, the mean gap is in the positive side of the axis indicating that the public does not receive what it expects to receive, or in policy terms there is ‘a responsiveness deficit’. The mean gap in relation to primary care is significantly lower than the mean gap in both preventive care and health promotion.
Conclusions The public can provide meaningful information even in areas of endless demand and can provide an addition point of view to be considered by policy makers in complicated healthcare rationing decisions.
Keywords: health policy, healthcare dimensions, responsivness gap
Introduction
In a time of economic austerity and escalating healthcare costs, one of the most daunting questions facing governments, healthcare professionals and the public alike is that of healthcare rationing. Experts and scholars who have written on the issue agree that some form of rationing is needed; but who should be responsible for making the necessary decisions? Policy makers, physicians, healthcare administrators and taxpayers (i.e. the public) have all been proposed as the most appropriate agents to set healthcare priorities. 1 , 2 , 3 Often, the public denotes patients, who, after all, are both the consumers of healthcare services and those who typically finance the healthcare system. Yet many policy makers and, especially, healthcare providers have argued that the public cannot be responsible for healthcare rationing, because consumers’ demand for healthcare services is infinite. 4 , 5 In other words, the argument goes, the public is not capable of prioritizing different healthcare needs, as individuals will typically demand ‘only the best’ in all areas. In the current study, we set out to actually examine whether the public indeed wants ‘only the best’ in all areas or if when called attention to the fact that resources are scarce can provide differentiations in expectations regarding healthcare provision. Thus, we sought to understand if data from the public can be considered input when policy makers seek to make complicated priority decisions.
Healthcare experts, as well as social scientists working in areas of public administration and policy, value the democratic notion of being responsive to public needs. 6 , 7 , 8 , 9 , 10 , 11 Democratic theory holds that a responsive government is one that takes into account public needs and expectations when setting binding policy objectives, and the quality of democratic government performance depends on the extent to which there is public influence on such policy decisions. Policy outcomes that are distant from public needs and expectations result in what political scientists refer to as a ‘responsiveness deficit’. 12 , 13 , 14 , 15 , 16 , 17 , 18 In healthcare, such a deficit might occur where differences exist between patients’ experiences and their expectations. Yet, healthcare scholars have largely overlooked the importance of identifying the deficit in different healthcare dimensions as a guide for setting healthcare policy priorities.
The question of what role the public should take in formulating healthcare policy has also been influenced by the current trendy shift away from the traditional, ‘paternalistic’ approach in patient care towards one in which patients are seen as autonomous decision makers. Proponents of this approach envision a patient‐centred care which obliges doctors to respond to their patients’ preferences, including their preferences regarding treatment. 19 Empirical evidence suggests that in fact, only a small percentage of patients subscribe to the autonomous patient manifesto. In one study of some 2800 patients in Canada, for instance, most expressed a preference to share decision making with their doctors, and nearly all the rest said they would prefer a passive role. 20 However, the autonomous patient debate is something of a red herring in terms of the question raised in this paper. The degree to which patients want to take part in decisions about their own medical care is distinct from their desire or ability to provide input to healthcare policy decision making. Based on their experience as consumers of healthcare, citizens learn the system, and can both provide information in regard to the quality of the service they received as well as what services are important to them and thus would expect to receive. That is, the question at issue here involves not micro‐level participation in medical decisions, but macro‐level civic conduct: are patients, as citizens, able to provide differing expectations in different health policy dimension that will constitute meaningful information for policy makers confronted with rationing decisions?
This paper examines whether patients are indeed prepared to behave as ‘responsible citizens’, by measuring the degree to which individuals empirically differentiate their expectations between three healthcare dimensions: primary care, preventive care and health promotion. According to a recent conceptualization by the OECD, 21 these three dimensions comprise core functions of any healthcare system. Primary care is regarded as ‘the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients and practicing in the context of family and community’. 22 The preventive dimension focuses on disease prevention and health maintenance, and includes issues related to early diagnosis of disease, identification of people at risk of developing specific problems and interventions designed to avert health problems. Screening tests, health education and immunization programs are common examples of preventive care. 23 Health promotion denotes various population‐based strategies that target major risk factors for disease, primarily through efforts to change health‐related lifestyles and behaviours. 21 This dimension includes any activity that seeks to improve a person’s or population’s health by providing information about and awareness of ‘at risk’ behaviours associated with various conditions. 24
One thousand two‐hundred eleven Israeli adults were surveyed regarding (i) their experience with the primary care, prevention‐related and promotion‐related practices, and (ii) the importance they attribute to each. In our analyses, we aimed to identify whether there are gaps between patients’ reported experiences and expectations in these three healthcare dimensions, indicating a healthcare responsiveness deficit. We sought to examine whether any such observed gap patterns vary as a function of the distinct healthcare dimensions. Finally, we aimed to examine whether any observed variations are associated with respondents’ ethnicity by differentiating in our sample between Jews and Arabs, who constitute an ethnic minority in Israel.
Method
The setting
The study was conducted in Israel, which operates under a system of universal health coverage. Under a National Health Insurance Law passed in 1995, all citizens are required to enrol in one of four not for profit sick funds, which compete for members. Israel’s Ministry of Health regulates the system and also owns some services, including some hospitals, psychiatric health services, and maternal and child health centres. The government covers the cost of a Uniform Benefits Package for all citizens regardless of their financial means; individuals may choose to pay for additional services and treatments not in the basic package.
Sampling and data collection
Employees of a professional telephone survey firm contacted a random sample of Israeli households during October and November of 2010, using computer‐assisted telephone interviewing. Interviewers asked the first person they spoke to in each household who was 18 or older if they would be willing to discuss their views on healthcare. Interviews were conducted in Hebrew, Russian or Arabic, according to the participant’s native language. A pilot study was conducted in September with 43 participants to make sure the questions were clear and that the respondents indeed could prioritize the different healthcare issues.
The sample comprised 1211 individuals above the age of 18, with a response rate of 55%. Respondents included 636 females and 575 males, with an average age of 47.5. Eight hundred and three of the respondents were Jewish and 408 were Arab. Arabs make up about 20% of the Israeli population, meaning that a representative sample comprising 1000 participants would have included around 200 Arabs. As we were interested in examining whether preferences regarding healthcare differ between Arabs and Jews, we added an additional 200 Arab respondents, enabling us to compare the two populations based on statistically sufficient samples. However, when examining the entire sample, we used weights so as to make the sample representative of the Israeli population as a whole.
Measures
Demographic variables included participants’ age in years, sex, educational level, ethnicity (Jewish or Arab) and religiosity (secular, traditional or observant).
Healthcare experiences and preferences
Participants were asked two sets of questions on practices related to primary care (14 items), preventive care (2 items) and health promotion (3 items). The first set elicited respondents’ perceptions of the practices they experience with their healthcare provider, and the second elicited the practices that are important to them, indicating expectations. The first set was introduced as follows: ‘I will read a number of sentences regarding your healthcare provider. Please rate on a scale from 1 to 7 to what extent you agree with each sentence with 7 indicating you completely agree and 1 indicating you completely disagree’. The second was introduced in this way: ‘As you know, healthcare providers lack resources such as manpower and money, and therefore cannot provide everything that is required. Please rate what is important to you, while thinking of your priorities (what is more and what is less important to you). Take into consideration that it is not realistic to receive the best of everything in every area. I will read the sentences again regarding your healthcare provider. Please rate from 1 to 7 to what extent each one is important to you, with 7 indicating that it is most important and 1 indicating that it is very unimportant’. The items and their response rates are presented in Table 1.
Table 1.
Percentage of respondents who chose each response option for each item and mean gap for each item between expectations and experiences
| Experiences Please rate on a scale from 1 to 7 to what extent you agree with each sentence | Expectations Please rate from 1 to 7 to what extent each sentence is important to you | Mean Gap | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | Not Relevant | Missing | 1 | 2 | 3 | 4 | 5 | 6 | 7 | Not Relevant | Missing | ||
| 1. The clinic has up‐to‐date equipment | 2.6 | 1.2 | 3.1 | 8.4 | 22.9 | 19.1 | 33.6 | 5.5 | 3.7 | 1 | 0.3 | 1.2 | 1.7 | 8.2 | 14.3 | 71.3 | 1.2 | 0.8 | 0.87 |
| 2. The clinic’s physical facilities are visually appealing | 1 | 1.4 | 3 | 5.5 | 15.6 | 23.5 | 49.9 | 0.2 | 1.1 | 1.1 | 1.5 | 4 | 14.2 | 15 | 62.4 | 0.2 | 0.4 | 0.23 | |
| 3. The clinic’s medical and technical equipment is in keeping with the type of services provided | 2.5 | 1.2 | 2.9 | 6.3 | 18.3 | 25.1 | 37.7 | 3.8 | 2.2 | 0.4 | 0.1 | 0.6 | 1.2 | 5.5 | 13.8 | 76.7 | 0.9 | 0.9 | 0.86 |
| 4. The amount of money you pay for medication & other prescribed treatment is appropriate. | 11.4 | 6 | 7.7 | 12.8 | 19.7 | 15.3 | 23.3 | 3.7 | 0.7 | 0.7 | 1.1 | 1.3 | 3.6 | 11.2 | 15.4 | 65.2 | 1.1 | 0.4 | 1.66 |
| 5. The amount of time you wait for a scheduled appointment with your regular doctor is short. | 8.7 | 4.5 | 8.5 | 10.7 | 17.3 | 19.2 | 29.2 | 1.5 | 0.4 | 0.7 | 0.7 | 1.2 | 2.7 | 11.3 | 21 | 61 | 0.7 | 0.6 | 1.32 |
| 6. The amount of time you wait at your doctor’s office for your appointment to start is short. | 8.1 | 4.9 | 9 | 14.9 | 22.9 | 20.6 | 18.3 | 0.8 | 0.4 | 1.2 | 0.8 | 1.2 | 2.9 | 13.4 | 21.6 | 57.6 | 0.7 | 0.7 | 1.49 |
| 7. The amount of time you wait for someone to answer the phone when you call your doctor’s office is short. | 5.7 | 4 | 6.4 | 9.2 | 16.4 | 20.4 | 29.2 | 7.1 | 1.5 | 1.4 | 0.7 | 1.8 | 4.6 | 12.6 | 20.4 | 54 | 3.5 | 0.9 | 0.92 |
| 8. The doctor spends enough time for examination and explanations. | 2.4 | 2.3 | 3.3 | 4.4 | 12.1 | 22.8 | 52.3 | 0.1 | 0.3 | 0.2 | 0.4 | 0.7 | 0.9 | 7.9 | 16.6 | 72.2 | 0.3 | 0.7 | 0.58 |
| 9. When you go to the doctor, you always see your regular doctor (not an assistant or partner). | 2.3 | 2 | 1.7 | 4.3 | 7.7 | 16.3 | 64.2 | 0.9 | 0.7 | 1.1 | 0.3 | 1.2 | 2.7 | 11.5 | 15.5 | 66.6 | 0.3 | 0.7 | 0.17 |
| 10. Your doctor respects you. | 0.7 | 0.4 | 0.7 | 1.5 | 4.3 | 12.8 | 79.2 | 0.2 | 0.2 | 0.8 | 0.1 | 0.2 | 1.2 | 4.8 | 11.1 | 81.1 | 0.2 | 0.5 | 0.05 |
| 11. The doctor’s explanations regarding your health problems or needed treatment are clear. | 1.3 | 0.9 | 1.6 | 3.7 | 10.7 | 17.8 | 63.3 | 0.2 | 0.6 | 0.3 | 0.1 | 0.4 | 0.6 | 3.5 | 10.6 | 83.6 | 0.3 | 0.6 | 0.47 |
| 12. Your doctor has enough patience for your questions or worries. | 1.6 | 1.3 | 1.7 | 3.5 | 10 | 18.1 | 63.4 | 0.2 | 0.3 | 0.5 | 0.1 | 0.4 | 0.7 | 6 | 13.8 | 77.4 | 0.4 | 0.7 | 0.38 |
| 13. Your doctor’s office location is convenient. | 3.2 | 1.5 | 2.1 | 4 | 12.2 | 18.2 | 57.8 | 0.7 | 0.2 | 1.7 | 1.2 | 2.1 | 6.4 | 22.6 | 19.2 | 45.1 | 1.1 | 0.7 | (−0.18) |
| 14. Your doctor’s office opening hours are convenient. | 3.7 | 2.7 | 4.9 | 8.1 | 18.7 | 19.7 | 41.5 | 0.3 | 0.4 | 0.4 | 0.6 | 1.1 | 2.8 | 13.2 | 21.3 | 59.5 | 0.2 | 0.8 | 0.71 |
| 15. Your doctor is interested in your way of life, and asks question regarding your lifestyle (such as diet, exercise habits and smoking or drinking problems). | 12.1 | 5.8 | 6.9 | 10 | 16.5 | 14.3 | 33.1 | 0.9 | 0.4 | 3.4 | 1.9 | 4.3 | 6.9 | 19.9 | 20.4 | 41.9 | 0.5 | 0.7 | 0.81 |
| 16. Your doctor gives you clear explanations about healthier lifestyles (such as proper diet, exercise habits and the effects of smoking or drinking). | 14.5 | 6.2 | 7.7 | 9.7 | 16.9 | 14.6 | 28.2 | 1.2 | 2.2 | 3.1 | 2.1 | 3.5 | 7.3 | 17.5 | 20.2 | 44.8 | 0.7 | 0.8 | 1.11 |
| 17. Your doctor offers you additional treatment in order to help you have a healthier lifestyle (such as smoking or drug‐use cessation counselling or workshops on diet and nutrition). | 18.6 | 6.8 | 9 | 9.7 | 16 | 12.1 | 24.9 | 1.8 | 1 | 3.4 | 1.8 | 8.2 | 7.3 | 17.2 | 18.5 | 47.2 | 0.7 | 1 | 1.46 |
| 18. Your doctor encourages you to get immunizations. | 19.2 | 4.5 | 6 | 6.9 | 10.3 | 12.9 | 36.7 | 2.7 | 0.7 | 4.8 | 2.1 | 3.6 | 6.3 | 16.4 | 17.2 | 47.3 | 1.5 | 1 | 1.01 |
| 19. Your doctor sends you for a regular check‐up routine, regardless of any physical problem (such as blood pressure measurement, testicular examination or mammography, or sight and hearing check‐ups). | 18.8 | 5.3 | 5.4 | 7.5 | 12.1 | 13.5 | 34.8 | 1.5 | 1.1 | 2.9 | 1.2 | 1.5 | 3.6 | 13 | 18.1 | 57.9 | 0.3 | 1.6 | 1.42 |
The items regarding primary care were adopted from the Primary Care Assessment Survey 25 and the SERVQUAL scale, which measures perceptions of service quality. 26 The promotion‐related items were adopted from Mcavoy, Kaner, Lock, Heather and Gilvarry 27 and Stott and Pill 28 . Finally, the items dealing with prevention were adopted from the questionnaire developed by Hutchison, Abelson, Woodward and Norman. 29
Results
As we were interested in the gap between experiences and expectations for each item, we calculated a difference score Q, defined as Q = Expectation‐Experience, of a given respondent for a given item. We then averaged the difference scores for primary care, promotion and prevention for each respondent. Table 1 shows the mean gaps for each item, and Fig. 1 depicts the distribution of the gaps for each of the three dimensions. We found that for all three dimensions the mean gap was significantly different from zero (mean gap primary care = 0.68, t 1002 = 23.38, P < 0.001; mean gap promotion = 1.12, t 992 = 16.99, P < 0.001; mean gap preventive care = 1.23, t 990 = 18.03, P < 0.001), indicating that indeed, the Israeli healthcare system is characterized by a deficit in healthcare provision.
Figure 1.
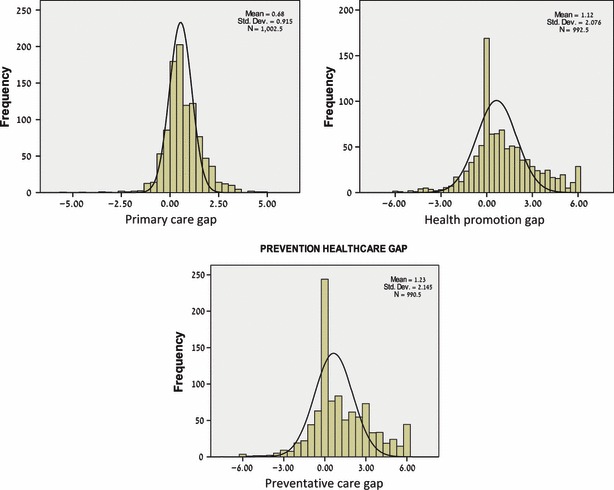
Distribution of the mean gap between expectations and experiences for each healthcare dimension.
To examine whether the observed gap patterns vary as a function of the different healthcare dimensions and whether the variations are dependent on ethnicity, we conducted a repeated measures anova, with the gaps by dimension as the within‐subject effect and ethnicity as a between‐subject effect. The results showed that at least two of the healthcare dimensions differed significantly in terms of the gap between experience and expectations (F = 45.4, d.f. = 2, 1185, P < 0.001). Post hoc tests revealed a significant difference between primary care and both prevention and promotion in this respect: Bonferroni multiple comparisons produced a significant difference between the mean gaps for primary care and promotion of 0.43 (SD = 0.06, P < 0.001), and a significant difference between the mean gaps for primary care and prevention of 0.53 (SD = 0.06, P < 0.001). No difference was found between the mean gaps for prevention and promotion (mean difference = 0.10, SD = 0.06, NS). The comparison between the three gap distributions is depicted in Fig. 2 through box‐plot graphs. Finally, no significant effect was found for the ethnicity by gap interaction (F = 0.35, d.f. = 2, 1185, NS), indicating that the gap patterns do not vary between Jews and Arabs.
Figure 2.
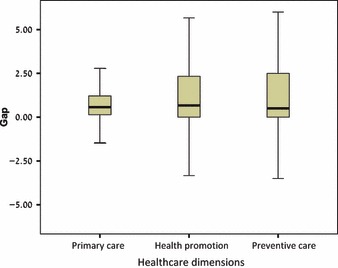
Box plots depicting the comparison between the mean gaps for each healthcare dimension.
Discussion
Our first objective was to examine whether there is a deficit in required healthcare provision in Israel, in the form of a gap between patients’ reported experiences and their expectations in three core healthcare dimensions: primary care, health promotion and preventive care. We found that in all three dimensions there was indeed a gap between expected and experienced care. As in all three dimensions the mean gap is in the positive side of the axis, it is apparent that the public is not receiving what it expects – or in policy terms, there is ‘a responsiveness deficit’.
Our second objective was to examine whether the observed gap patterns vary as a function of these distinct healthcare dimensions. We found that the mean gap in relation to primary care is significantly lower than the mean gap in both preventive care and health promotion (with no difference between the two latter dimensions). A possible implication of these findings is that members of the public are capable of providing varied expectations in areas of (theoretically) endless demand. More specifically, patients can distinguish between different functions or areas of healthcare, understand the importance of prevention and promotion, and identify a greater deficit in prevention and promotion than in primary care. From a public policy perspective, putting more emphasis on prevention and promotion has been found to produce cost savings in the long run. 30 , 31 It thus appears that by investing resources in preventive care and health promotion, policy makers may be able to both improve long‐term results and adhere to the public’s expectations.
The broader implication of these findings is that despite the popular idea that patients will always demand only the best in all areas of healthcare, citizens are capable of providing meaningful information to be considered when forming healthcare policy regarding rationing. In addition to the information provided by professionals, politicians, economists and other interest groups, taking account of ‘responsiveness gaps’ identified by citizens may add valuable information to be considered in health policy‐making processes. This information is valuable for a number of reasons. First, considering the public’s voice strengthens democratic values. Second, if the policy makers actually take into account this information, as part of their policy decisions, it may revitalize their legitimacy to continue to serve as health policy makers in financially harsh times. Finally, it provides an additional point of view, an experience‐based point of view which is less influenced by political, economic and medical considerations, in the complicated rationing decisions.
Our final objective was to examine whether any variations in the patterns we identified are dependent on ethnicity. Our results show no difference in these patterns between the majority Jewish population and the minority Arab population in Israel. Both populations have similar expectations and perceive the gaps between experience and expectations in the three dimensions in a similar manner. This finding is especially interesting, as researchers have identified significant differences between the two populations in regard to both expectations and satisfaction from public services in most other policy areas. 32 Our findings suggest that healthcare is a unique area in which divisions and conflict between the Jewish and Arab populations become insignificant, and do not affect the provision of healthcare on the one hand or perceptions of the experience on the other.
One limitation of our study concerns the generalizability of our findings. The Israeli healthcare system differs from those of many other nations in important respects, such as its particular feature of public funding managed by non‐governmental sick funds. It therefore is possible that our results are specific for the Israeli population. However, while different healthcare systems may perceive individuals in different ways – e.g. as patients vs. customers – there is no reason to expect that citizens cannot demonstrate the ability to differentiate expectations no matter what healthcare system they belong to. It is our belief that citizens should be asked both about their experiences and about their expectations and not merely regarding how satisfied they are with what is delivered or simply what they prefer. 33 , 34
References
- 1. McKie J , Shrimpton B , Hurworth R , Bell C , Richardson J . Who should be involved in health care decision making? A qualitative study Health Care Analysis , 2008. ; 16 : 114 – 126 . [DOI] [PubMed] [Google Scholar]
- 2. Torgenson D , Gosdon T . Priority setting in health care: should we ask the tax payer? British Medical Journal , 2000. ; 320 : 1699 . [PMC free article] [PubMed] [Google Scholar]
- 3. Jordan J , Dowswell T , Harrison S , Lilford R , Mort M . Health needs‐ assessment: whose priorities? Listening to users and the public British Medical Journal , 1998. ; 316 : 1668 – 1670 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bruni R , Laupacis A , Martin D . Public engagement in setting priorities in health care . Canadian Medical Association Journal , 2008. ; 179 : 15 – 18 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rosen P , Karlberg I . Opinions of Swedish citizens, Health‐care politicians, administrators and doctors on rationing and health‐care financing . Health Expectations , 2002. ; 5 : 148 – 155 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Soroka SN , Lim ET . Issue definition and the opinion‐policy link: public preferences and health care spending in the US and UK . British Journal of Politics and International Relations , 2003. ; 5 : 576 – 593 . [Google Scholar]
- 7. Vigoda E . From responsiveness to collaboration: governance, citizens, and the next generation of public administration . Public Administration Review , 2003. ; 62 : 527 – 540 . [Google Scholar]
- 8. Manza J , Cook FL , Page BI . Navigating Public Opinion: Polls, Policy, and the Future of American Democracy . New York : Oxford University Press; , 2002. . [Google Scholar]
- 9. Barzelay M . The New Public Management: Improving Research and Policy Dialogue . Berkeley & Los Angeles : University of California Press; , 2001. . [Google Scholar]
- 10. Lynn LE Jr . The new public management: how to transform a theme into a legacy . Public Administration Review , 1998. ; 58 : 231 – 237 . [Google Scholar]
- 11. Hood C . A public management for all seasons? Public Administration , 1991. ; 69 : 3 – 19 . [Google Scholar]
- 12. Burstein P . Why estimates of the impact of public opinion on public policy are too high . Social Forces , 2006. ; 84 : 2273 – 2289 . [Google Scholar]
- 13. Hobolt SB , Klemmemsen R . Responsive government? Public opinion and government policy preferences in Britain and Denmark Political Studies , 2005. ; 53 : 379 – 402 . [Google Scholar]
- 14. Cope GH . Bureaucratic reform and issues of political responsiveness . Journal of Public Administration Research and Theory , 1997. ; 7 : 461 – 471 . [Google Scholar]
- 15. Durant RF . The democratic deficit in America . Political Science Quarterly , 1995. ; 110 : 25 – 47 . [Google Scholar]
- 16. Erikson RS , Wright GC , McIver JP . Statehouse Democracy: Public Opinion and Policy in the American States . Cambridge : Cambridge University Press; , 1993. . [Google Scholar]
- 17. Lijphart A . Democracies: Patterns of Majoritarian and Consensus Government in Twenty‐One Countries . New Haven and London : Yale University Press; , 1984. . [Google Scholar]
- 18. Dahl RA . Pluralist Democracy in the United States: Conflict and Consent . Chicago : Rand McNally; , 1967. . [Google Scholar]
- 19. Coulter A . The Autonomous Patient: Ending Paternalism in Medical Care . London : Nuffield Trust; , 2002. . [Google Scholar]
- 20. Deber R , Kraetschmer N , Urowitz S , Sharpe N . Do people want to be autonomous patients? Preferred roles in treatment decision‐making in several patient populations Health Expectations , 2007. ; 10 : 248 – 258 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Marshall M , Leatherman S , Mattke S . Selecting indicators for the quality of health promotion, prevention and primary care at the health systems level in OECD countries . OECD Health Technical Papers , 2004. ; 16 : 1 – 49 . [Google Scholar]
- 22. Donaldson M , Yordy K , Vanselow N , eds . Defining Primary Care: An Interim Report . Washington, DC : National Academy Press; , 1994. . [PubMed] [Google Scholar]
- 23. Mosby Elsevier . Mosby’s Medical Dictionary , 8th edn . St Louis, MO : Mosby; , 2009. . [Google Scholar]
- 24. Segen JC. McGraw‐Hill Concise Dictionary of Modern Medicine . New York : McGraw‐Hill; , 2002. . [Google Scholar]
- 25. Safran DG , Kosinski M , Tarlov AR et al. The Primary Care Assessment Survey: tests of data quality and measurement performance . Medical Care , 1998. ; 36 : 728 – 739 . [DOI] [PubMed] [Google Scholar]
- 26. Parasuraman A , Berry L , Zeithaml VA . SERVQUAL: a multiple‐item scale for measuring consumer perceptions of service quality . Journal of Retailing , 1988. ; 64 : 12 – 40 . [Google Scholar]
- 27. McAvoy BR , Kaner EF , Lock CA , Heather N , Gilvarry E . Our healthier nation: are general practitioners willing and able to deliver? A survey of attitudes to and involvement in health promotion and lifestyle counselling British Journal of General Practice , 1999. ; 49 : 187 – 190 . [PMC free article] [PubMed] [Google Scholar]
- 28. Stott NCH , Pill RM . “Advise yes, dictate no.” Patients’ views on health promotion in the consultation . Family Practice , 1990. ; 7 : 125 – 131 . [DOI] [PubMed] [Google Scholar]
- 29. Hutchison BG , Abelson J , Woodward CA , Norman G . Preventive care and barriers to effective prevention. How do family physicians see it? . Canadian Family Physician , 1996. ; 42 : 1693 – 1700 . [PMC free article] [PubMed] [Google Scholar]
- 30. Goetzel R . Do prevention or treatment services save money? The wrong debate . Health Affairs , 2009. ; 28 : 37 – 41 . [DOI] [PubMed] [Google Scholar]
- 31. Cohen J , Neuman P , Weinstein M . Does preventive care save money? Health economics and the presidential candidates New England Journal of Medicine , 2008. ; 358 : 661 – 663 . [DOI] [PubMed] [Google Scholar]
- 32. Smooha S . Ethnic democracy: Israel as an Archetype . Israel Studies , 1997. ; 2 : 198 – 241 . [Google Scholar]
- 33. Alford J . Defining the client in the public sector: a social – exchange perspective . Public Administration Review , 2002. ; 62 : 337 – 346 . [Google Scholar]
- 34. Alford J . Rethinking the public: paying attention to citizens and clients [online] . In : Glover D , Patmore G , Jungwirth G ( eds ) For the People: Reclaiming Our Government . Sydney : Pluto Press in association with the Australian Fabian Society; , 2000. : 56 – 6 . [Google Scholar]


