Abstract
Background
The behaviour of hospitalized older adults can contribute to falls, a common adverse event during and after hospitalization.
Objective
To understand why older adults take risks that may lead to falls in the hospital setting and in the transition period following discharge home.
Design
Qualitative research.
Setting and participants
Hospital patients from inpatient medical and rehabilitation wards (n = 16), their informal caregivers (n = 8), and health professionals (n = 33) recruited from Southern Health hospital facilities, Victoria, Australia.
Main variables studied
Perceived motivations for, and factors contributing to risk taking that may lead to falls.
Main outcome measures
Semi‐structured, in depth interviews and focus groups were used to generate qualitative data. Interviews were conducted both 2 weeks post‐hospitalization and 3 months post‐hospitalization.
Results
Risk taking was classified as; (i) enforced (ii) voluntary and informed and (iii) voluntary and mal informed. Five key factors that influence risk taking behaviour were (i) risk compensation ability of the older adult, (ii) willingness to ask for help, (iii) older adult desire to test their physical boundaries, (iv) communication failure between and within older adults, informal care givers and health professionals and (v) delayed provision of help.
Discussion and Conclusion
Tension exists between taking risks as a part of rehabilitation and the effect it has on likelihood of falling. Health professionals and caregivers played a central role in mitigating unnecessary risk taking, though some older adults appear more likely to take risks than others by virtue of their attitudes.
Keywords: behaviour, falls, hospital, older adult, risk taking
Introduction
Falls in the elderly are a considerable health issue for older adults, hospitals and the community more broadly. One in three people over the age of 65 years fall each year, and approximately 20% of them require medical attention.1, 2 Falls are a particular problem for older adults who have been admitted to hospital, where inpatient rates of falls between 3 to 20 falls per 1000 occupied bed days have been reported.3, 4, 5 Once people have left hospital, however, the rates of falls have continued to be high, with up to 7.5 falls per 1000 days being reported.6, 7
Falls prevention research paradigms have historically focussed on intrinsic and extrinsic factors for falls in the older adults.8 A new behavioural/risk taking paradigm is emerging where it is the decision making of older adults in response to their risk factors that is potentially more important.9 Further work, however, is required to better understand this behavioural/risk taking paradigm as it applies to falls prevention.
Risk taking has previously been defined in many ways. We define risk taking as the act of implementing a goal‐directed option where (i) the behaviour in question could result in more than one option, and (ii) some of these outcomes are undesirable or even dangerous.10 Early research in risk taking was based upon models of rational choice11 and widely described using economic behaviour models.12 Research conducted on understanding risk taking has commonly been based on expected utility theory13 and been categorized in three ways (i) those that explain the differences between people who take risks and those that do not, (ii) those that explain the differences between situations that promote risk taking in most people and situations that promote risk aversion, and (iii) those that explain both types of differences.14 Previous research amongst older hospital inpatients has sought to identify factors associated with higher self‐perceived risk of falling (i.e. conceptually, probability of a ‘fall’ outcome during hospitalization) and a higher self‐perceived risk of injury if a fall were to occur (i.e. conceptually, utility lost from the ‘fall’ outcome).15 Multiple regression models highlighted that older age and having better cognitive function were independently associated with a lower self‐perceived risk of falling. Older adults who had poorer motor function, a lower perception of the proportion of other hospital patients who fall, and a higher perception of the proportion of such falls that result in injury were independently associated with higher self‐perceived risk of injury if one were to fall. Further research has found that older hospital inpatients generally have an accurate impression of the probability of falling while in hospital, but underestimate the rate of injury associated with falls.16 In the community setting, it has been found that people with type A (risk taking) personality types tend to fall more frequently,17 and that extroverted people who are fallers or who fear falling participate in more activities outside the house.18 Thus, some formative research has been conducted to identify differences between people that may predispose them to taking more risk in this context more than others. However, very little is known of the differences between situations that promote risk taking, or factors that may predispose some people to take risks in some situations and not others. It is also likely that simplistic frameworks that only consider the decision making of the individual older adult will be limited in their ability to explain risk taking in contexts such as the hospital setting or the post‐discharge period where health professionals, care‐givers and family members may influence the risks taken by the individual.
This study aims to identify factors and pathways that might explain why older adults take risks that may lead to falls in the hospital setting and in the transition period following being discharged home.
Method
Design
The prior research and clinical experiences of the investigators led them to anticipate that multiple, potentially conflicting perspectives would be held on falls' risk taking behaviour by older adults and those who care for them (health professionals, partners, family members and other care‐givers) that would need to be incorporated to gain a broader understanding of this phenomenon. Also, given the paucity of literature in regard to falls' risk taking by older adults and its antecedent factors, a paradigm of enquiry that would allow for discovery and expansion of pre‐existing conceptualizations held by the investigators would be required. Thus, the aims of the study were addressed using a qualitative, phenomenological, constructivist approach that was exploratory and descriptive. Phenomenology seeks to understand the meaning or structure of the lived experience of this phenomenon for a person or group of people.19 Constructivist ontology (philosophical study of reality) takes the approach that there are multiple and sometimes conflicting social realities constructed by human intellects that can change as their constructors become more informed.20 Data were collected using face to face interviews, telephone based interviews, and focus group interviews. All interview schedules were semi‐structured utilizing predominantly open‐ended questions.
Initial interview questions were initially designed by all the investigators, and were intended to be broad in scope so as to capture a wide range of descriptions of experiences in patient care and falls related matters. The questions were subsequently refined by TH and DAL after data analysis of the first few interviews in each participant group to explore in greater depth the area of risk taking in regard to falls and the interaction of the older adult, the environment (including health professionals and caregivers) and the tasks being performed which may affect such risk taking behaviour in the hospital and in the post‐discharge period.
Participants and setting
There were three groups of participants in this study.
The ‘older adult’ group comprised of adults 65 years of age or above and who were admitted to in‐ patient medical, rehabilitation or geriatric evaluation and management wards. Patients whose discharge destination were not their own home, or patients who were non English speaking or cognitively impaired were excluded for interview purpose. The ‘caregiver’ group was family or other support people that the patient identified as their main support person. The ‘health professional’ group was health professionals who care for the target patient group during inpatient and post‐discharge periods.
Participants were recruited from tertiary hospitals, a rehabilitation hospital and community‐based rehabilitation programs with the Southern Health healthcare network in Victoria, Australia. The number of participants recruited were; (i) tertiary hospitals, 11 patients, 5 caregivers and 12 health professionals (ii) rehabilitation hospital, 5 patients, 3 caregivers and 16 health professionals (iii) community based rehabilitation program, 5 health professionals.
Procedure
The study commenced after receiving ethics approval from the Southern Health Human Research Ethics Committee and Monash University Research Ethics Committee.
Recruitment of all three groups occurred between March 2011 and June 2011.
Advertising posters were posted on wards calling for suitable patients and family carers as participants. Nurse unit managers and allied health professionals of the respective wards were also approached for identification of suitable patients and/or family caregivers for interviews. All older adult subjects (n = 16) and caregivers (n = 8) were recruited through the staff identification process. There were five male older adults and three male caregivers. The mean (SD) age of older adults was 75.4 (6.9) years and 72.0 (10.1) years for caregivers the reasons for admission to hospital were fracture/orthopaedic (n = 9), stroke (n = 1), hyponatremia (n = 1), ischaemic colitis (n = 1), falls (n = 3), acute delirium (n = 1). All older adult participants bar 2 had either had a fall as a part of their presenting condition, had a history of falls within the past 6 months, or had fallen on the ward prior to being recruited. The two that did not have a history of falls had neurological diagnoses (stroke, delirium) that placed them at high risk of having falls. All caregivers recruited lived with the older adult participant, all cared for them full‐time, six were spouses and two were daughters. Health professionals (n = 33) were recruited by expression of interest in response to e‐mail advertising and by ‘snowball’ sampling. ‘Snowball’ sampling involved asking health professionals who had already been recruited into the study to identify additional health professionals who may participate in the study. The health professionals recruited included nurses (n = 12), occupational therapists (n = 7), physiotherapists (n = 10), social workers (n = 1), podiatrists (n = 1) and case managers (n = 2).
Consent to participate was gained before interviews and focus groups were conducted. Interviews were conducted by an investigator (DAL) who is an experienced physiotherapist in the field of gerontology. All interviews and focus groups followed the same interview schedule within each group of participants, and all were recorded with a digital audio recorder.
Data gathering
Participants in the patient group received two interviews. The first interview was conducted one to 2 weeks post‐discharge from the hospital, and focussed on the inpatient experience. We waited until the patient had been discharged, so they would not feel pressured to provide responses that reflect positively upon the hospital and hospital staff as if they had still been inpatients. A second interview was conducted 3 months after discharge and focussed on the experience of the transition period post‐discharge. A face to face interview took place in the patient's home on both occasions unless the patient's residence was geographically remote, in which case a telephone interview conducted. The interviews ranged from 30 to 60 min in duration. The total number of interviews for this group was 30 (n = 16). Two patients did not complete a second interview, one due to ill health and the other did not wish to participate.
Participants in the caregiver group received two interviews. Both interviews were conducted at the same time as the patient group, and ranged from 30 to 60 min in duration. The total number of interviews for this group was 14 (n = 8). One caregiver declined the second interview due to ill health, and another refused to participate further. Patient and caregiver were allowed to be in the same room at the time of the interview; however they were discouraged from engaging in the other person's interview. The investigators recognized that this may limit the degree of disclosure by older adults or their care‐givers with regards to areas of disagreement or tension between them. However, the investigators felt that offering these participants the choice as to whether they would be present or not for others’ interview would be empowering them and help build trust with the investigators, rather than building a perception that they were being ‘checked up on in secret’.
Topics of discussion in the first interview included patient/caregivers’ general impressions of the hospitalization experience, and engaging with hospital staff and the hospital environment, patient/caregivers’ perceptions of why falls occur in hospitals, how patients responded to risk of falls, why they took risks, factors driving risk taking behaviour that may result in falls, patient/caregiver's recollection of and reaction to involvement in patient care during hospitalization and in planning for transition home. An example of a direct question used to elicit description of a risk‐taking activity was ‘Did you do anything that you think put you at risk of falling over while in hospital?’ which was followed by probing and prompting to elicit a narrative account of the activity, its antecedents and outcomes. Topics of discussion in the second interview focussed on risk taking and falls during the post‐hospitalization period.
Participants in the health‐professional group attended one of six focus groups. Each had five to six participants, and was purposefully structured to have three different health professional disciplines. The focus groups ranged from 30 to 60 min in duration. Topics of discussion included health professional perceptions of their role in preventing patient falls during and after hospitalization, perceptions of why patients fall, why patients take risks, the factors underlying risk taking and recollections of what health professionals say to patients and their support persons for the prevention of falls during hospitalization and in preparation for the transition period.
Analysis
A framework analysis approach was utilized to familiarize investigators with the data, to identify a thematic framework to separate the data, to index and apply codes to the data, to group codes into categories and link these to the appropriate part of the thematic framework and identify association between individual categories, broader category groupings and other concepts within the framework.21 We did not seek to triangulate individual issues between stakeholder perspectives as evidence of their existence as the investigators anticipated that the perspectives held by some stakeholders would directly conflict with that of others. For example, when asked about why a patient tried to walk to the toilet on their own when they had been told to ask for help, a staff member might say the patient is being ‘non‐compliant’ with instructions whereas the patient might say that the staff do not come when you ask for them to come and that they are not providing the assistance they promised. A constructivism approach to building understanding encourages these divergent individual recollections to be coalesced into a broader understanding of the phenomenon than any one individual perspective allows,20 and was thus pursued in this analysis.
nvivo computer statistical software 9.1 (QSR International Pty Ltd, Doncaster, Vic., Australia) was used to assist with coding, charting, and mapping data from the audio recordings. Analysis, coding, and mapping of data were led by DAL and TH collaboratively. Data analysis was on‐going during the data collection process, and was iteratively used to refine the questions; prompts and redirections that were used as the study progressed.
Our intent was to gather and synthesize emic (insider) views on the risk‐taking phenomenon, however, the investigators recognized the possibility that pre‐existing etic (outsider) investigator views may influence how the data were coded, and subsequently analysed. Member checking was performed with five (two older adults, three health professionals) participants following completion of data coding to examine whether investigator coding and interpretation of data were consistent with that of the participants. Minor disagreements were resolved following clarification and explanation of the codes, thus the framework analysis continued without recoding of data.
Sample size consideration
The study was designed to allow for recruitment of up to 36 hospitalized older adults, 24 family caregivers and 36 health professionals. The iterative data collection and analysis approach identified that saturation of themes and data codes had been reached after analysis of 30 interviews with the 16 patients, 14 interviews with 8 carers and 6 focus groups involving the 33 health professionals.
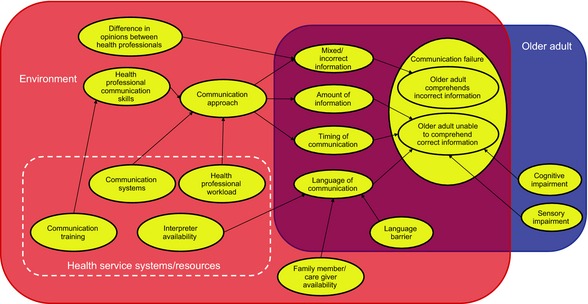
Findings
We first identified three broad categories of data, representing constructs, relating to risk taking behaviour. The first broad category was considered to be the base elements of risk taking. These were the older adult, their environment, and the task that may be attempted by the older adult while in hospital or after discharge. The environment consisted of both the physical environment and the older adult's significant others (health professionals and caregivers). None of the participants directly referred to these elements in this way, rather, these elements implicitly emerged from descriptions of risk taking provided. For example, one participant described wanting to go the toilet (activity), but that they were in a hurry (the older adult) and that an over‐toilet chair was out of position (environment) (Table 1, statement 2). These factors were therefore considered to interact and were conceptualized as three overlapping concepts in our framework (Fig. 1). The tasks related to risk taking tended to differ between the hospital and post‐discharge settings. In hospital, description of taking risks related to toileting and mobilizing around the bedroom area and toilet. Post‐discharge, there was the addition of outdoor activities such as gardening, and household activities.
Table 1.
Participant quote table
| Statement no. | Participant no. | Participant group | Quote |
|---|---|---|---|
| 1 | 12 | Older adult | ‘…when you've got to go to the toilet, you've got to go…’ |
| 2 | 7 | Older adult | ‘When I went in the toilet, I was usually in a hurry and that thing (the over‐toilet seat) was out of position. I used my crutches to drag it over the toilet, I could have easily fallen … I could have asked for help, asked somebody to put back the toilet. (But I thought) No, I won't bother and I did it myself quickly. I did. Luckily I didn't fall, but I could have.’ |
| 3 | 7 | Older adult | ‘If I were to do risky things, it would be in the garden, carrying heavy pots.’ |
| 4 | 6 | Occupational therapist | ‘Patients have cognitive issues and do not realize that they need assistance and are therefore getting up without the assistance or walking aid they need when they are walking’ |
| 5 | 4 | Occupational therapist |
Interviewer: ‘So when she went back home, she went back to the original way she was walking’ Participant: ‘Yes, that's right. And cognitively she is on to it’ Interviewer: ‘Why do you think she does that if she is cognitively intact?’ Participant: ‘ (It could) be denial’ |
| 6 | 7 | Older adult | ‘And the ward where I was, did have a lot of stuff in the corridor. The blood pressure monitor, machines and trolleys and all sorts of things, it was horrible if I wasn't paying attention I could have tripped over’ |
| 7 | 5 | Case manager | ‘They might feel competent. We might make them feel very protected here in a hospital environment or in the community when people are coming in or TCP (transitional care program) when they have got regular visitors. We might load them with a false sense of security, we might make them feel confident but then they are on their own that they may overstep them’ |
| 8 | 4 | Occupational therapist | ‘…the patient just left the walking frame outside the door and started to use her single point stick or furniture walk which she had been doing for a while now. ’ |
| 9 | 8 | Older adult | ‘When you are at home, you are in familiar surroundings; you take chances, take risk and do things without thinking things through whereas in hospital, you are aware of the risk step by step by step.’ |
| 10 | 17 | Caregiver | ‘She always thinks she is bothering people … I think she's too scared to ask sometimes because other patients seemed to need more help than mum did. She would have felt that I won't ring the buzzer because the patient over there probably needs more help and they are busy with that one. That's the sort of person she is.’ |
| 11 | 14 | Occupational therapist | ‘They (patients who are unable to speak English) can't verbalize what they want’ |
| 12 | 3 | Physiotherapist | ‘They may have different expectations. I know in some Asian backgrounds, you are expected to do everything on your own in hospital and family members will provide the care including showering, dressing and feeding and everything. Whereas in our culture, nursing staff have to do all those tasks … ’ |
| 13 | 7 | Older adult | Participant: ‘He (another patient) was ringing his bell a lot, but that was just because he needed a lot of help. He couldn't see where things were, whereas I didn't ring my bell, not because I didn't need help, but because I knew if you ring too much they get cross with you … they came and they would lean against the wall, (Staff would say) ‘what is it now’ with a bad tempered attitude like you are a nuisance.’ |
| 14 | 7 | Older adult |
Interviewer: ‘Did it put you off asking for help later on?’ Participant: ‘It probably put me off when I saw their attitude to him and I realised if you ask for too much help, some people would get very resentful’ |
| 15 | 12 | Older adult | ‘I had been to the toilet three times and I wanted to go again and when she came, she went (profanity) and put her hand up and flopped it down to show ‘not you again’ |
| 16 | 7 | Older adult | ‘…the patient in the next bed, he was asking for help. They (hospital staff) said ‘oh you didn't ask for help’, so that's a good thing. Made me think they like you better if you don't ask for help.’ |
| 17 | 7 | Older adult | ‘Sometimes I needed help, I will wait for a nurse nearby who looks friendly and ask ‘can you help me to get out of bed?’ But if a nurse is not nearby or you think the nurse is not friendly enough… I tried myself to walk and do things that I probably shouldn't have done.’ |
| 18 | 7 | Older adult | ‘Because you feel embarrassed, in my case I used to do everything for myself, I haven't been in hospital for 20 years; I just didn't want to ask anyone to help me. I want to do it for myself.’ |
| 19 | 6 | Occupational therapist | ‘but some people make that conscious decision… “I know it's a risk but I am going to do it anyway” because it is a lifestyle choice, they don't want to be that restricted whatever their situation is’ |
| 20 | 24 | Older adult | ‘In hospital… you are conscious of wanting to get well to get out and sometimes do too much’ |
| 21 | 21 | Physiotherapist | ‘The family members and friends not being aware of what the patient's capability are now and they are expecting more and then ask for more of the patient’ |
| 22 | 4 | Occupational therapist | ‘They (family members) say “Mum is okay, dad is okay, they don't need the shower chair, and they don't need the rail”, whereas in actual fact they do. The patient says “I don't normally use the frame, I can walk with nothing” … Family will often think similarly. ‘No, mum normally doesn't need that at home, she's okay’ |
| 23 | 21 | Physiotherapist | ‘…to progress the patient's ability so we are pushing them a little bit further than they normally do. Sometimes that skill may go beyond of what they are used to, and they may lose their balance’ |
| 24 | 22 | Older adult | ‘The minute you become confident, you start to do things that you shouldn't be doing and that's how falls occur’ |
| 25 | 27 | Nurse | ‘I am a nurse so I go in and I assess things from a nursing point of view so I will say, do these do that. Don't do this, don't do that and then the physio might come in and see things slightly different in their perspective because they see things with the physio brain working with them and so they have different emphasis on what is important … Might be you are giving slightly different messages with different focus.’ |
| 26 | 3 | Physiotherapist | ‘There are multiple occasions I have seen doctors get patients up and walk them in stockings. I come up to them and I say you may want to consider wearing slippers or bare feet or something and I come back the next time, they still do the same thing, so it is one of those things. Possibly they don't like being told or whether they have official training you know, you should not walk patients on socks, I don't know if this happens’ |
| 27 | 31 | Older adult |
Older adult: ‘I didn't talk to them about the fall… When I fell down, they picked me up and put me to bed, that's all, never talked to them anymore.’ Interviewer: ‘But why didn't you talk to them?’ Older adult: ‘Not enough nurses. There is no time for the nurses’ |
| 28 | 9 | Nurse | ‘… educating staff on reading mobility boards … we get a lot of agency and bank staff that don't do rehab who don't know these things and we as permanent staff forget to tell them to be aware of how the chart works, how the colour (coding system) works because many times you see people walking when they shouldn't be and the nurse had no idea of what the red meant or the blue meant at all’ |
| 29 | 3 | Physiotherapist | ‘Patients who are non‐English speaking. You say “call me if you want to get up.” Obviously that message hasn't got through………Unless you have an interpreter right there which I would dare say doesn't happen unless you have a family member that's more appropriate……So in the first instance, it is a problem already. That problem will carry on until someone explains it to them’ |
| 30 | 10 | Nurse | ‘Today we are under staffed; we are down a staff member. You are running to try and give them their meds, let alone to try and toilet them, you just don't have the time in the day. We do our best but sometimes we are running nonstop let alone going back every two hours to toilet them. We are being pushed to our extreme that the nurse can't keep up anymore’ |
| 31 | 10 | Nurse | ‘A lot of them fall because we can't see them the way the ward is set up, we just can't see them… a lot of the patients who can't press the buzzer, don't want to press the buzzer or they are confused and they don't know how to, we can't see them if they are trying to get up.’ |
| 32 | 27 | Nurse | ‘They are not here very long, whereas ten years ago, they may have a ten day stay for something we are now sending them home in 3 days, 4 days. So they are still not medically there, so we send them home with antibiotics rather than giving them the whole course in the hospital. I don't know if that is what used to happen but the length of stay for patient is much shorter, so they are going home and they are still a little bit sick … they are not quite 100%. They may be 90%; therefore that 10% is the bit that will make them fall at home.’ |
| 33 | 25 | Caregiver |
Participant: ‘My girls came in and looked after her’ Interviewer: ‘In what ways?’ Participant: ‘Well we only went for 8 days and one did 4 days and the other one did the other 4 days and their husbands would come in the evenings to have dinner and see the children and they would go home … They didn't have to do anything, just help to get her meals.’ |
Figure 1.
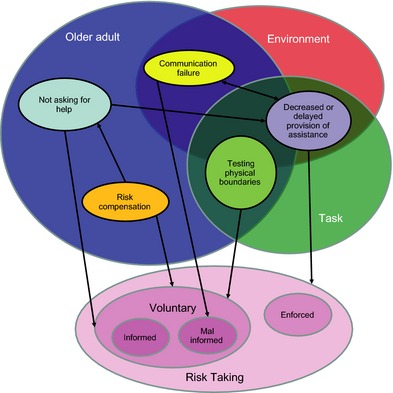
Overall conceptual framework of risk taking by older adults during hospitalization and following discharge.
The second broad category was considered to be the nature of risk taking itself. We conceptualized two categories of risk; voluntary and enforced risk taking. Enforced risk taking was defined as instances where an older adult felt they have no alternative, but to attempt to perform the task (Table 1, statement 1). Voluntary risk taking was conceptualized as instances where an individual felt they had a choice as to whether they performed the activity or not (Table 1, statement 2). Voluntary risk taking was also a feature of the post‐discharge period (Table 1, statement 3). Voluntary risk taking was further conceptualized as having subcategories of informed and mal‐informed voluntary risk taking. Informed, voluntary risk taking was considered to be when the individual decided to take a risk when he or she was aware of the risks involved. Voluntary, mal‐informed risk taking was considered to be when the individual decided to take a risk when not fully aware of the risks involved. It should be noted that these classifications refer to actions rather than as terms to classify/characterize individuals as a person may at one time take a mal‐informed risk and then an informed risk at another.
We present enforced risk and voluntary risk taking as distinct areas, whereas in reality it may be more of a continuum depending on the activity the individual performs. There is overlay between the perception of being essential by the older adults and that of others, e.g. although a health professional might believe gardening is optional, a patient may believe it to be essential. For the purpose of this analysis, we focused upon the perceptions of the older adult as they were in most instances the decision maker as to whether an activity was attempted and the associated risks this task posed.
The third broad category group was factors that described how the elements of risk taking combined to result in the subcategories of risk taking described. There were five key sub‐categories identified within this set that we refer to as nodes, which were interconnected between themselves, the elements of risk taking and the subcategories of risk taking creating pathways of risk taking described. Development of these pathways was initially driven by combining statements by participants under the central code for that pathway (e.g. for the ‘risk compensation’ pathway, the central code was driven by health‐professional statements that some older adults did not have insight into their reduced physical capacity). These codes were then separated and connected to related codes to reveal a deeper understanding of that concept (e.g. statements that patients were in ‘denial’ [Table 1, statement 5] revealed that some patients may be aware of their physical limitations, but did not to accept these cognitions, resulting in the same outcome as those who did not recognize their physical limitations) and factors influencing that concept. Both direct statements by participants and etic conceptualizations of the investigators were used to build the frameworks that described these pathways. Interconnections between these pathways are conceptualized in Fig. 1. Each of these five nodes and the pathways surrounding them are now described in detail.
Node (i): risk compensation
The pathway involving the node of ‘risk compensation’ is conceptualized in Fig. 2. We defined risk compensation as the adjustment of behaviour in response to the risk perceived by the older adult so that the task can be performed in a safe manner. When the older adult does not have sufficient ‘ability to perform a task’ relative to the ‘difficulty of the task’, the older adult needs to use ‘risk compensation’ to safely complete or avoid the task. The older adult's ‘ability to perform a task’ is likely to be lower than that experienced pre‐morbidly, owing to their ‘health’ (illness, injury or surgery which led to the hospitalization). This creates the need for the older adult to have ‘awareness of self and ability’ and their reduced level of capacity. Hospital staff openly questioned whether many older adults had the ability to recognize this due to ‘cognitive decline’ (Table 1, statement 4).
Figure 2.
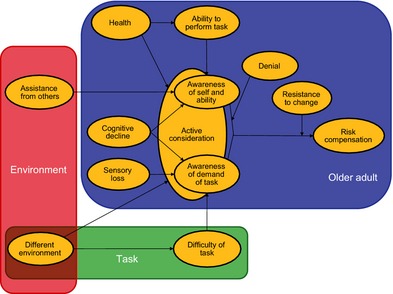
Conceptualization of risk compensation ability pathway.
Performing tasks in a ‘different environment’ to what they are used to may increase ‘difficulty of the task’ and requires that older adults give ‘active consideration’ to these demands. These environmental differences were spoken of in relation to the hospital environment being different and increasing ‘difficulty of the task’ (Table 1, statement 6). Where there was ‘awareness of demand of a task’ and this was given ‘active consideration’ patients reported ‘risk compensation’ however, familiarity with the home environment may have contributed to less ‘risk compensation’ following discharge from hospital (Table 1, statement 9).
Health professionals perceived that some older adults may also experience a false sense of security through the presence of potential ‘assistance from others’, that because there were hospital staff nearby, they were safe when they attempted activities (Table 1, statement 7).
Changing behaviour in light of changed physical capacity appeared to be impeded by previous habits and ‘resistance to change’ (Table 1, statement 8).
Node (ii): asking for help
We defined the node of ‘asking for help’ as occasions where older adults needed to seek assistance to perform activities due to reduced ability to complete the task on their own. This node was considered to be a step following on from the ‘risk compensation’ node (Fig. 1), where appropriate risk compensation often prompted older adults to ask for help. Factors specific to the older adult were related mainly to their attitudes and beliefs (Fig. 3). Some had ‘belief that they can perform the task without help’ or had a very strong ‘desire for independence’.. Others reported ‘not wanting to be a burden’ to significant others, particularly hospital staff (Table 1, statement 10).
Figure 3.
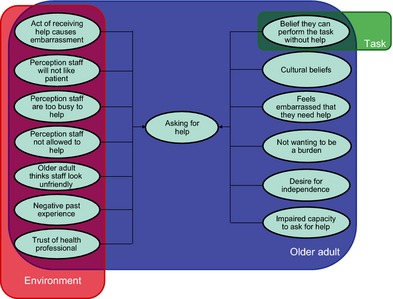
Conceptualization of asking for help pathway.
Health professionals perceived that some older adults had ‘impaired capacity to ask for help’ (Table 1, statement 11).
Health professionals also identified an overlay of ‘cultural beliefs’ regarding the role older adults’ thought they should have as patients, the role of staff and of their family (Table 1, statement 12).
Factors relating to the interaction between older adults and their social environment were predominantly perceptions held or experiences had by older adults that were influenced by their interactions with staff. Some had a ‘perception that staff are too busy to help’, a ‘perception that staff are not allowed to help’ if lifting was involved or a ‘perception staff will not like them’ if they asked for help too often. Although one could speculate that these perceptions were ill‐informed, examples were provided where these had been influenced by interactions with staff (Table 1, statements 13, 14 and 15). These and other ‘negative past experiences’ may reduce ‘trust in the health professional’ and provide disincentive for older adults to seek help again in future.
It is possible that some communications between staff and other older adult hospital inpatients may have been misinterpreted, and this perpetuated misconceptions about asking for help (Table 1, statement 16). Older adults’ perception of the demeanour of the staff and whether the ‘older adult thinks staff look unfriendly’ affected their willingness to ask for help. It is possible this may also have been related to negative past experiences (Table 1, statement 17).
Some older adults felt the ‘act of receiving help causes embarrassment’ (particularly with toileting), while others reported they ‘feel embarrassed that they need help’ (Table 1, statement 18).
Node (iii): testing physical boundaries
Attempting to perform activities that the older adult had not previously attempted as they had become ill or had surgery is an important element of the rehabilitation process. This emerged as a central concept in several descriptions of risk taking from all groups of participants where the older adults attempted a previously performed activity that was beyond the older adult's present physical capability. The risk taking pathway involving the node of ‘testing physical boundaries’ in the rehabilitation or recovery process is presented (Fig. 4). The motivation for an older adult to test their own physical boundaries appeared to be largely internally generated. Older adults described being motivated by a ‘desire to be independent’, ‘desire to go home’ and ‘desire to return to their previous lifestyle’. Health professionals and some older adults thought that older adults were consciously aware of when risks were being taken for this reason (Table 1, statements 19 and 20).
Figure 4.
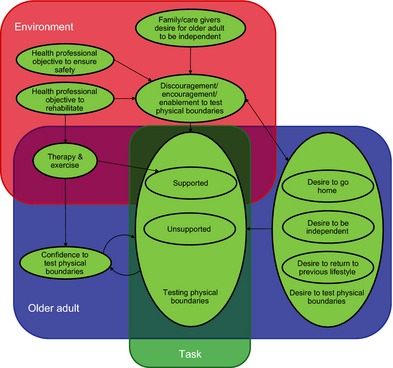
Conceptualization of testing physical boundaries pathway.
Caregivers and health professionals also encouraged this to varying degrees, at times creating a three‐way dialogue on this issue (‘discouragement/encouragement/enablement to test physical boundaries’). Disagreements between the older adult and the caregivers/family, the family/caregivers and health professionals and between the health professionals and the older adults were described. Often in these disagreements, the health professionals were more conservative in the level of risk they were prepared for the older adult to take when testing their physical boundaries when on their own. Care‐givers expressed ‘desire for the older adult to be independent’ while health professionals expressed competing demands to ensure the older adult was rehabilitating (‘health professional objective to rehabilitate’) but in a safe manner (‘health professional objective to ensure safety’). Thus, if the older adult and/or family members were more willing to test physical boundaries than the health professional was, the health professional would recommend against what they viewed as excessive risk taking. Health professionals cited genuine concern for the safety of the older adult and argued that others did not fully appreciate the risk that was there (Table 1, statement 21 and 22).
Health professionals were not always trying to discourage older adults from testing their physical boundaries. Some described actively working with patients through ‘therapy and exercise’ and provision of functional retraining activities to assist them to test their physical boundaries (Table 1, statement 23).
An important distinction here between therapist facilitated and older adult independently initiated testing of physical boundaries was the presence of the health professional to assist the older adult if they did lose their balance, providing a more protected environment in which to take this risk. Thus, it became apparent that there were subgroups of testing physical boundaries; testing that took place in a supported environment (‘supported testing of physical boundaries’) and ‘unsupported testing of physical boundaries’.
When an older adult successfully completed an activity where they tested their physical boundaries, they often described their ‘confidence to test physical boundaries’ as improving. This often encouraged further testing of physical boundaries. This could become problematic where repeated iterations of testing physical boundaries continued with increasingly difficult activities until a failure or near miss occurred (Table 1, statement 24).
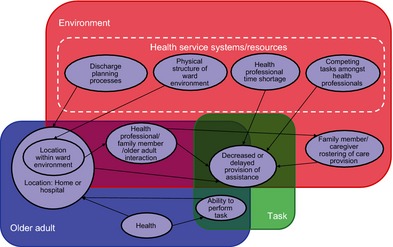
Node (iv): failure of communication directed to older adult
‘Communication failure’ between older adults, caregivers, family members and health professionals were often criticized as being a central component of why older adults take risks (Fig. 5). Several factors were identified as driving the need for frequent, accurate and clear communication of information between and within the different stakeholder groups. Handing‐over of responsibility for the care of the older adult between shifts and between the hospital and post‐discharge period created need for communication between health professionals and caregivers. The dynamic nature of older adults’ physical abilities (both reduction in ability initially followed by gradual improvement during recovery and rehabilitation) also created ongoing need for discussion between the stakeholder groups.
Figure 5.
Conceptualization of failure of communication directed to older adult pathway.
‘Differences in opinion between health professionals’, which may have been mediated by differing professional backgrounds, philosophies, professional power differentials or levels of experience, created potential for inconsistent, ‘mixed or incorrect information’ being given to older adults (Table 1, statement 25 and 26).
Insufficient communication (‘amount of information’) was a common problem identified by all study participant groups, and was thought to be largely driven by time and resourcing restrictions on health professionals (‘health professional workload’) (Table 1, statement 27).
Deficiencies in ‘health professional communication skills’ were identified as contributing to communication failure. The ‘communication systems’, routines and procedures in place to facilitate communication between health professionals and with other stakeholders were identified as important factors that required health professionals to understand and employ these systems (Table 1, statement 28).
Some factors related to the older adult were seen to impede communication, specifically whether the patient had a ‘cognitive impairment’, and whether the patient was able to communicate in English (‘language barrier’). However, if an interpreter was available (family member or professional interpreter), the impact of being from a non‐English speaking background on communication failure was reduced (Table 1, statement 29).
Node (v): decreased or delayed provision of assistance
‘Decreased or delayed provision of assistance’ was a common factor leading to all forms of risk taking (Fig. 6). Conceptually, this node can follow on from risk taking pathways through the nodes relating to risk compensation and asking for help (Fig. 1). However, assistance can be provided even when help is not explicitly requested; indicating that decision making of family, caregivers and hospital staff independently of the older adult can play a role in managing risks taken by the older adult. Indeed, provision of assistance could override even intentional risk taking efforts by the older adult.
Figure 6.
Conceptualization of decreased or delayed provision of assistance pathway.
Factors related to decreased or delayed provision of assistance following request appear to be environmental or based upon the interaction between the older adult and the person whose assistance they are seeking. The environmental factors involving health professionals were ‘health professional time shortage’ and ‘competing tasks amongst health professionals’. Participants from each stakeholder group identified that hospital‐based health professionals had difficulty at times providing assistance requested by older adults at the time requested or within a timeframe expected by the older adult. Hospital staff cited that often they had competing tasks to perform, that staffing shortages compounded this problem, and that it was particularly difficult when multiple older adults were requesting assistance at once (Table 1, statement 30).
The ‘physical structure of the ward environment’ was also cited by health professionals as a reason for decreased or delayed provision of assistance. This was particularly the case if the staff did not have direct vision of the patient from the nurses’ station, and the effect on the risk of an older adult falling was amplified if the patient did not or could not use the nurse buzzer system (Table 1, statement 31).
‘Health professional/family member/older adult interaction’, primarily through asking for help, was conceptualized as affecting whether older adults received assistance or not. If an older adult did not ask for help in hospital, they were less likely to receive it. Thus, the node of provision ‘decreased or delayed provision of assistance’ was closely linked to the node of asking for help (Fig. 1).
Health professionals described ‘discharge planning processes’ as influencing whether patients receive sufficient assistance while at home with particular criticism that patients are discharged too early. Concern was raised that patients do not have sufficient ‘health’ and physical ‘ability to perform tasks’ they will need to perform in their home environment and that this influences whether they are sent home. Hospital staff described a change in discharge planning processes over the past decade such that older adults were being placed in a position of greater enforced risk over the past decade (Table 1, statement 32).
Support was described as being provided by formal and informal caregivers during the post‐discharge period in response to the needs of the older adult. An example of a highly organized ‘family member/caregiver rostering of care provision’ response from an older adult's family was described (Table 1, statement 33).
Discussion
There are many factors that influence risk taking behaviour in older adults who have been hospitalized. This research has developed a framework for understanding risk taking behaviours of older adults in relation to falls that advances upon previous work in this field because it has explicitly sought to incorporate the role of significant others within the framework and does not assume a rational choice is being made by an informed individual as previously assumed.11, 12, 13, 14
We do not contend that risk taking behaviour, of itself, is a problem. Our data have highlighted that risk taking is an important part of the rehabilitation process and returning to independence by the older adult. However, the possibility that risk taking will be excessive and result in falls with subsequent injury creates problems for older adults, their caregivers and health professionals alike. The challenge instead appears to be ensuring that risk taking by the older adult is informed and voluntary where possible, rather than mal‐informed or enforced, and that risk taking be undertaken in a supported environment. Health services, health professionals and caregivers can support this by addressing problems associated with communication failures, by creating opportunities for risk taking to be undertaken in controlled, supported environments, and by facilitating older adults to actively consider their risk of falling with specific tasks so that they can appropriately compensate for their physical limitations.
Enforced risk taking was conceptualized as largely being attributable to decreased or delayed provision of assistance, combined with the perceived necessity of the older adult to perform the activity and the limited physical capacity of the older adult to perform the activity. Health‐service policies aiming to reduce the length of inpatient admissions were identified by health professionals as contributing to this. Funding policies have generally tightened in developed nations in recent years to try to limit growth in public health care expenditures,22 thus, it is not surprising that pressures to minimize length of stay and subsequent cost exist. However, this creates a trade‐off between the level of enforced risk that older adults have to take, and the health resource savings that have been sought after, and may be a factor involved in hospital re‐presentation due to a fall following an initial presentation.
The findings of this research are consistent with findings from quantitative research approaches used in this population. For example, the inter‐relation between some patient‐related factors in our framework, specifically cognitive impairment and risk compensation ability, were concordant with the early research findings in this area. A trial of one‐to‐one patient education based on the health belief model aiming to modify how high risk activities were performed on a hospital ward (risk compensation) demonstrated that falls could be reduced amongst cognitively intact older adults in the hospital setting, and that goals could be set to modify how specific activities were performed.23 However, this program was not beneficial for older adults who were cognitively impaired, highlighting the importance of the cognitive impairment factor on risk compensation ability. Previous work has also highlighted that people with risk factors for falls following discharge can experience lower rates of falls if support services are provided to them,7 a finding consistent with our framework.
This research was limited as it was conducted within one geographic region and multiple hospitals within one health service. Hence, it is possible that some of the factors identified may be relevant only to this particular context. Recruitment of only participants who could speak English may have limited the insights potentially gained from older adults with culturally and linguistically diverse backgrounds, though some insights were gained on this issue from the health professional perspective. The first patient and caregiver interview was conducted 1–2 weeks post discharge, specifically so that older adults would feel free to give an open and honest account of their experiences in hospital. However, this may also have led to some recall bias, and reprioritization of the importance of some issues as they were perceived at that point in time.
Interpretation of our study findings and conclusions should pay heed to the background experiences and perspectives of the investigators that may have influenced them in this task. Each of the investigators had a clinical background with varying levels of experience working older adults in hospital. They may therefore have more readily highlighted factors expressed by health professionals that impact on the ability of hospital staff to provide assistance that are outside of their control (e.g. the perception of a lack of time and too many competing activities) as the investigators had experienced these same frustrations in their previous clinical roles. It is also likely that previous research work conducted by the investigators with a range of theoretical models (such as the Health Belief Model24 and Person–Environment–Occupation model25) influenced how they conceptualized interconnections between emergent codes from the analysis.
Development of our risk taking framework permits further investigation of factors that may contribute to falls and inform interventions for their prevention. Where risk taking has led to a fall, it is now possible to classify the type of risk taking that took place and identify the factors that contributed to it. Similar work to the present study should also be conducted to determine perspectives of medical staff on the risk taking of older adults, and that of older adults from non‐English speaking backgrounds, both of whom were not included in the present study.
Acknowledgements
THa was supported by an Australian National Health and Medical Research Council Career Development Award.
THa is the director of Hospital Falls Prevention Solutions Pty Ltd. This company provides training in the ‘Safe Recovery’ patient education program which was mentioned in the present manuscript.
THa has received payment for expert witness testimony in the area of falls in hospitals.
THa has received payment for providing presentations at conferences in the area of falls in hospitals.
References
- 1. Lord SR, Ward JA, Williams P, Anstey K. An epidemiological study of falls in older community dwelling women: the Randwick falls and fractures study. Australian Journal of Public Health, 1993; 17: 240–245. [DOI] [PubMed] [Google Scholar]
- 2. Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. New England Journal of Medicine, 1997; 337: 1279–1284. [DOI] [PubMed] [Google Scholar]
- 3. Haines T, Bennell K, Osborne R, Hill K. Effectiveness of targeted falls prevention programme in subacute hospital setting: randomised controlled trial. BMJ, 2004; 328: 676–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Healey F, Monro A, Cockram A, Adams V, Heseltine D. Using targeted risk factor reduction to prevent falls in older in‐patients: a randomised controlled trial. Age and Ageing, 2004; 33: 390–395. [DOI] [PubMed] [Google Scholar]
- 5. Stenvall M, Olofsson B, Lundstrom M et al A multidisciplinary, multifactorial intervention program reduces postoperative falls and injuries after femoral neck fracture. Osteoporosis International, 2007; 18: 167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Haines TP, Russell T, Brauer SG et al Effectiveness of a video‐based exercise programme to reduce falls and improve health‐related quality of life among older adults discharged from hospital: a pilot randomized controlled trial. Clinical Rehabilitation, 2009; 23: 973–985. [DOI] [PubMed] [Google Scholar]
- 7. Hill AM, Hoffmann T, McPhail S et al Evaluation of the sustained effect of inpatient falls prevention education and predictors of falls after hospital discharge—follow‐up to a randomized controlled trial. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 2011; 66: 1001–1012. [DOI] [PubMed] [Google Scholar]
- 8. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age and Ageing, 2006; 35 (Suppl. 2): ii37–ii41. [DOI] [PubMed] [Google Scholar]
- 9. Hill A, Hill K, Brauer S et al Evaluation of the effect of patient education on rates of falls in older hospital patients: description of a randomised controlled trial. BMC Geriatrics, 2009; 9: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Furby L, Beyth‐Marom R. Risk taking in adolescence: a decision‐making perspective. Developmental Review, 1992; 12: 1–44. [Google Scholar]
- 11. Keeney R, Raiffa H. Decisions with Multiple Objectives: Preferences and Value Tradeoffs. New York: Wiley, 1976. [Google Scholar]
- 12. Friedman M, Savage LJ. The utility analysis of choices involving risk. The Journal of Political Economy, 1948; 56: 279–304. [Google Scholar]
- 13. Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica: Journal of the Econometric Society, 1979; 47: 263–291. [Google Scholar]
- 14. Byrnes JP, Miller DC, Schafer WD. Gender differences in risk taking: a meta‐analysis. Psychological Bulletin, 1999; 125: 367. [Google Scholar]
- 15. Haines TP, McPhail S. Threat appraisal for harm from falls: insights for development of education‐based intervention. Open Longevity Science, 2011; 5: 1. [Google Scholar]
- 16. Hill AM, McPhail S, Hoffmann T et al A randomized trial comparing digital video disc with written delivery of falls prevention education for older patients in hospital. Journal of the American Geriatrics Society, 2009; 57: 1458–1463. [DOI] [PubMed] [Google Scholar]
- 17. Zhang JG, Ishikawa‐Takata K, Yamazaki H, Ohta T. Is a type A behavior pattern associated with falling among the community‐dwelling elderly? Archives of Gerontology and Geriatrics, 2004; 38: 145–152. [DOI] [PubMed] [Google Scholar]
- 18. Kloseck M, Hobson S, Crilly R, Vandervoort A, Ward‐Griffin C. The influence of personality on falling and engagement in daily activities by community‐dwelling older adults. Physical & Occupational Therapy in Geriatrics, 2007; 26: 1–17. [Google Scholar]
- 19. Patton MQ. Qualitative Research & Evaluation Methods, 3rd edn. Thousand Oaks, CA, USA: Sage Publications, 2001. [Google Scholar]
- 20. Guba EG, Lincoln YS. Competing paradigms in qualitative research. Handbook of Qualitative Research, 1994; 2: 163–194. [Google Scholar]
- 21. Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ, 2000; 320: 114–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jones CI. Why Have Health Expenditures as a Share of GDP Risen So Much? Mass, USA: National Bureau of Economic Research Cambridge, 2002. [Google Scholar]
- 23. Haines TP, Hill AM, Hill KD et al Patient education to prevent falls among older hospital inpatients: a randomized controlled trial. Archives of Internal Medicine, 2011; 171: 516–524. [DOI] [PubMed] [Google Scholar]
- 24. Janz NK, Becker MH. The Health Belief Model: a decade later. Health Education Quarterly, 1984; 11: 1–47. [DOI] [PubMed] [Google Scholar]
- 25. Law M. The Person–Environment–Occupation model: a transactive approach to occupational performance. Canadian Journal of Occupational Therapy, 1996; 63: n1. [DOI] [PubMed] [Google Scholar]


