Abstract
Background
Our breast cancer clinic promotes patient use of decision and communication aids (DAs/CAs) through two mechanisms: coaching and prompting. From January through September 2010, we provided services to 462 of 1106 new visitors (42%). Of those 462 visitors, 267 (58%) received coaching. For the remainder (195 or 42%), the best we could do was prompt them to self‐administer the DA and CAs.
Objective
We wanted to learn whether patients prompted to use DAs/CAs did so.
Methods
We surveyed prompted patients after their visits. We asked how much of each DA they reviewed, whether they listed questions, made notes and audio‐recorded their consultations. We tallied frequencies and explored associations using logistic regression.
Results
Of the 195 prompted patients, 82 responded to surveys (42%). Nearly all (66/73 or 90%) reported reviewing some or all of the booklets and 52/73 (71%) reported viewing some or all of the DVDs. While 63/78 (81%) responded that they wrote a question list, only 14/61 (23%) said they showed it to their doctor. Two‐thirds (51/77 or 66%) said someone took notes, but only 16/79 (20%) reported making audio recordings.
Discussion
More patients reported following prompts to use DAs than CAs. Few reported showing question lists to physicians or recording their visits. Our exploratory analyses surfaced associations between using CAs and race/ethnicity or education that merit further investigation.
Conclusion
Prompting patients assures better use of decision than communication aids. Clinicians may need to take a more active role to ensure patients receive adequate notes and recordings.
Keywords: breast cancer, communication aids, decision aids, prompting
Introduction
In response to patient information and communication needs, our university‐based breast cancer clinic launched a Decision Services unit to assist patients in using decision and communication aids. Decision aids are materials that present information about treatments and outcomes. Communication aids include question lists, audio recordings and notes.
In prior randomized controlled trials, decision and communication aids were associated with educational and psychological benefits such as increased question‐asking, knowledge and information recall.1, 2, 3, 4 Our implementation studies corroborate these research findings in our patient population. For example, we have found that decision aids improve our patients' knowledge of key breast cancer facts.5 Regarding question lists, previously other researchers found that prompting cancer patients to review suggested questions increased the number of questions patients ask during consultations by 6, from 6 on average to around 12.6, 7, 8, 9 Our question coaching goes further and is associated with identification of on average 15 questions that might otherwise have been forgotten or overlooked.10 Our evaluations also reflect prior research findings that cancer patients listen to audio recordings of their oncology visits and include other people in these reviews.10, 11, 12, 13
The Decision Services unit promotes the use of decision and communication aids through two mechanisms: coaching and prompting. For a maximum 30% of new patients visiting our surgeons and oncologists each year, we have the capacity to provide coaches who facilitate review of relevant decision aids and then personally assist with the use of communication aids for the visit. Specifically, the coaches call patients to encourage review of decision aids sent by clinic schedulers; help patients develop a list of questions; send the list of questions to doctors prior to the visit; and then accompany the patient to take notes and audio record the appointment. Our coaching programme is described in more detail elsewhere.13, 14, 15, 16
Because of resource limitations, we cannot provide coaching to all patients. Therefore, we prompt the remainder of patients to self‐administer decision and communication aids. We were curious as to whether patients who were prompted to self‐administer the decision and communication aids, actually did so.
The question of how many patients self‐administers decision and communication aids is not fully addressed in the existing literature. While patients involved in randomized control trials reported valuing decision and communication aids,1, 2, 3, 4, 5, 6, 7, 8, 9, 10 we found only limited research reporting on the success of implementations where patients were prompted to self‐administer these interventions. For example, one short‐term implementation found that 44% of patients used question prompt sheets during their consultations.17 As for audio recording, we found no studies addressing the question of how many patients audio‐recorded their visits. In 2002, Tattersall and Butow18, 19 strongly recommended providing consultation audio tapes to patients with cancer. In 2008, Pitkethly4 reviewed 16 studies and concluded that providing recordings of consultations is beneficial to most adults with cancer, as did Stephens and van der Muelen.20 But in all of these studies, the practice of providing the recording was initiated by the researcher or medical provider.
Because of these gaps in the literature, we formulated our own study to ask how many of our prompted patients were able to self‐administer decision and communication aids. Specifically, we asked, how many prompted patients:
Reviewed the decision aid(s) they received?
Wrote down a list of questions?
Successfully recorded their appointments?
Brought someone along to take notes at the appointment and how did they use those notes?
We also asked how the patients who self‐administered communication aids actually used their question lists and recordings, and whether there were any demographic subsets more likely to follow the prompts and make use of the decision and communication aids.
Methods
Study design and timing
This is a case series based on a review of programme records, including 4‐week follow‐up survey responses obtained between January and September 2010. We obtained ethics approval from the UCSF Committee on Human Research to abstract and de‐identify our programme records for research analysis and reporting purposes.
Setting and population
The UCSF Breast Care Center (BCC) is a high‐volume clinic providing multidisciplinary care in an NCI‐designated Comprehensive Cancer Center at the University of California, San Francisco. The study sample was drawn from the population of new patients treated for breast cancer at the BCC. In 2010, the BCC served a total of 554 new patients, 70% of whom were White, 18% were Asian, 6% Hispanic and 6% African American.
Intervention
Our programme distributes five decision aids coproduced by the Informed Medical Decisions Foundation and Health Dialog. The aids are designed to assist patients with breast cancer making treatment decisions at five different crossroads:
DCIS (stage 0) treatment options
Early stage surgical options (stage 1 or 2)
Early stage adjuvant chemotherapy and hormone therapy options (stage 1 or 2)
Reconstruction options (any stage)
Newly diagnosed metastatic (stage 4) options.
We distribute these decision aids through multiple mechanisms. The underlying trigger consists of a patient contacting a clinic scheduler to make an appointment to discuss treatment options with a surgeon or oncologist. Clinic schedulers then requisition appropriate decision aids for patients based primarily on the type of specialist they are seeing and their stage of disease. Patients seeing surgeons who are stage 0 are sent the DCIS programme, those who are stage 1 or 2 are sent the early stage surgical options programme and those seeing a plastic surgeon the reconstruction programme. We also routinely send the reconstruction programme with the DCIS or early stage surgical option programmes, as we want all patients who may find themselves considering mastectomy to be aware of reconstruction options. There are two decision aids for patients seeing oncologists, one for patients seeking post‐surgical treatment therapies and are stage 1 or 2, and one for individuals who have recently been diagnosed with metastatic (stage 4) breast cancer. Patients seeing both surgeons and oncologists may have received three or four programmes over their course of treatment.
The Decision Services team fulfils the requisition, by mailing a package that includes a decision aid in the form of a digital video disc (DVD) and accompanying booklet, along with a cover letter. The cover letter prompts patients to review the decision aid. The cover letter also prompts patients to make a list of questions as they review the decision aid, bring the list of questions to their appointment, bring a friend to take notes and borrow a recorder if necessary from the Cancer Resource Centre in our hospital lobby.
There are three scenarios in which patients might end up self‐administering decision and communication aids. Some visitors may have been sent a decision aid but were never offered coaching. Another set of visitors declined coaching but accepted one or more decision aids. The third set of visitors accepted coaching but did not receive it because they had not been picked up from our waiting list.
Visitors placed on the coaching waiting list are prioritized by need (we assess interest, English language proficiency, cognitive deficits, emotional distress and whether the visitor will be alone) but ultimately the number of coaches available in any 1 week is constrained by the coaches' overall schedule. Each coach is expected to coach one visitor each week, and while coaches will provide additional sessions as their other duties allow, our capacity during the study period averaged 10 sessions per week.
Study sample and data collection procedures
We formed the case series that comprises our study sample by identifying the patients who had received only the prompted intervention described previously (Fig. 1). At 4 weeks post‐intervention, we contacted patients with a survey. We invited patients with email addresses to take the survey online by sending an email message with a weblink. If after 2 weeks a patient had not yet completed the survey, author SV called the patient and administered the survey over the telephone. If there was no answer, she sent a reminder email. Two weeks after the second attempt at contact, SV again contacted non‐responders by telephone, and if unavailable emailed a final request to complete the survey.
Figure 1.
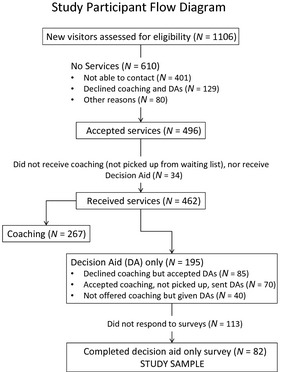
Study Participant Flow Diagram. DA denotes Decision Aid.
For patients without email addresses, we mailed them the survey by US Postal Service with a stamped, return envelope. We contacted non‐responders as described earlier for the email survey group, except that we followed up by mail and telephone.
Outcomes, measures, instruments and analysis plan
Our programme evaluation included the following items aimed at patients who had received prompting but not coaching from Decision Services.
Study question 1: How many patients reviewed the decision aids they received?
Our survey asked patients to check off which of the five decision aids they had received. For each title, we asked how much of the DVD (all, some or none) they watched, and how much of the booklet (all, some or none) they reviewed.
Study question 2: How many patients wrote down a list of questions and how did they use the list?
We asked each patient ‘did you write down a list of questions to take with you to your appointment?’ If yes, we asked whether they referred to the list during the appointment and if they showed the list to their doctor.
Study question 3: How many patients successfully recorded their appointments and how did they use the recording?
We asked patients ‘did you bring an audio‐recording device to your appointment?’ If yes, we asked if they successfully recorded the appointment, if they listened to the recording since the appointment and whether anyone else listened to the recording.
Study question 4: How many patients brought someone along to take notes at the appointment and how did they use those notes?
We asked patients ‘did someone take notes during the appointment?’ If yes, we asked who took the notes (patient, spouse, friend or other), if they reviewed the notes since the appointment and if they shared the notes with anyone else.
Study question 5: Were any demographic subsets more likely to follow the prompts and make use of the aids?
On the surveys we asked patients to provide information about their demographics, specifically their breast cancer stage, age, educational level, marital status, employment status, ethnicity and race.
To learn whether any of the demographic variables were predictors of patient adoption of communication aids, we conducted stepwise linear regression for all the demographics for each of the three dichotomous variables: list, recorder and notes. For the other study questions, we calculated and tabulated descriptive statistics.
Results
Sample characteristics
Between January and September of 2010, we identified 195 patients who had received the intervention prompting them to self‐administer decision and communication aids and invited them to participate in our follow‐up survey. A total of 82 (42%) responded to our surveys (Fig. 1). The average age of our respondents was 57 years old. Of the 82 respondents, the majority (71%) were White (58/82) and most (82%) were non‐Hispanic (67/82). The majority (67%) were married or in a committed relationship (55/82). The majority (60%) completed college or had advanced graduate degrees (49/82), although most (51%) were not working (42/82). The majority (55%) were diagnosed with Stage 1 or 2 breast cancer (45/82).
Demographically, our survey respondents are not significantly different from the overall 2010 BCC population (Fisher exact chi square for race = 0.99 and for Hispanic = 1.0); those who did not respond to the survey (Fisher's exact chi square for race = 0.468 and for Hispanic = 0.170); or those who received coaching during the same time period (Fisher's exact chi square for race = 0.236 and for Hispanic = 0.374). Table 1.
Table 1.
Distribution of categorical demographic variables
| Variables | Study participants | Study non‐respondents | Coaching participants | BCC Clinic 2010 | ||||
|---|---|---|---|---|---|---|---|---|
| n | Percentage | n | Percentage | n | Percentage | n | Percentage | |
| Race | ||||||||
| White | 58 | 71% | 69 | 61% | 111 | 69% | 417 | 75% |
| Asian | 12 | 15% | 9 | 8% | 15 | 9% | 101 | 18% |
| African American | 1 | 1% | 3 | 3% | 8 | 5% | 33 | 6% |
| Other | 2 | 2% | 4 | 4% | 15 | 9% | 3 | 1% |
| Missing | 9 | 11% | 28 | 25% | 13 | 8% | 0 | 0% |
| Total | 82 | 100% | 113 | 100% | 162 | 100% | 554 | 100% |
| Hispanic | ||||||||
| Non‐Hispanic | 67 | 82% | 69 | 61% | 141 | 87% | 523 | 94% |
| Hispanic | 8 | 10% | 3 | 3% | 10 | 6% | 31 | 6% |
| Missing | 7 | 9% | 41 | 36% | 11 | 7% | 0 | 0% |
| Total | 82 | 100% | 113 | 100% | 162 | 100% | 554 | 100% |
| Age | ||||||||
| Mean age | 82 | 57 years | 113 | 54 years | 162 | 55 years | 434 | 56 years |
| Breast Cancer Stage | ||||||||
| Stage 0 (DCIS) | 20 | 24% | – | – | – | – | 80 | 18% |
| Stage 1 | 26 | 32% | – | – | – | – | 160 | 37% |
| Stage 2 | 19 | 23% | – | – | – | – | 128 | 29% |
| Stage 3 | 5 | 6% | – | – | – | – | 43 | 10% |
| Stage 4 (metastatic) | 4 | 5% | – | – | – | – | 22 | 5% |
| Unknown | 3 | 4% | – | – | – | – | 1 | 0% |
| Missing | 5 | 6% | – | – | – | – | 0 | 0% |
| Total | 82 | 100% | – | – | – | – | 434 | 100% |
| Education | ||||||||
| Some high school | 2 | 2% | – | – | – | – | – | – |
| High school grad | 7 | 9% | – | – | – | – | – | – |
| Some college | 15 | 18% | – | – | – | – | – | – |
| College grad | 22 | 27% | – | – | – | – | – | – |
| Some grad school | 2 | 2% | – | – | – | – | – | – |
| Master's | 14 | 17% | – | – | – | – | – | – |
| Doctorate | 5 | 6% | – | – | – | – | – | – |
| More than college grad | 6 | 7% | – | – | – | – | – | – |
| Missing | 9 | 11% | – | – | – | – | – | – |
| Total | 82 | 100% | – | – | – | – | – | – |
| Less than college grad | 24 | 29% | – | – | – | – | – | – |
| College grad and beyond | 49 | 60% | – | – | – | – | – | – |
| Missing | 9 | 11% | – | – | – | – | – | – |
| Total | 82 | 100% | – | – | – | – | – | – |
| Marital status | ||||||||
| Married | 49 | 60% | – | – | – | – | – | – |
| In a committed relationship | 6 | 7% | – | – | – | – | – | – |
| Single | 6 | 7% | – | – | – | – | – | – |
| Divorced/separated | 11 | 13% | – | – | – | – | – | – |
| Widowed | 6 | 7% | – | – | – | – | – | – |
| Missing | 4 | 5% | – | – | – | – | – | – |
| Total | 82 | 100% | – | – | – | – | – | – |
| Employment status | ||||||||
| Working full time | 18 | 22% | – | – | – | – | – | – |
| Working part time | 15 | 18% | – | – | – | – | – | – |
| Not working | 42 | 51% | – | – | – | – | – | – |
| Missing | 7 | 9% | – | – | – | – | – | – |
| Total | 82 | 100% | – | – | – | – | – | – |
Survey administration
To rule out differences in survey administration (33 email, 31 telephone and 18 paper/pencil), we conducted chi square analysis (using Fisher's exact testing) on the responses to all the survey questions. Only one question (whether they had viewed the booklet) demonstrated a statistically significant difference (Fisher's exact = 0.026). This difference is attributable to the fact that 7/29 respondents surveyed by telephone said they viewed ‘none’ of the booklet, while 0/17 mail and 0/27 email respondents said they viewed ‘none’.
How many patients reviewed the decision aids they received?
Almost all (90%) of those who responded to the question reported reviewing ‘Some’ (19/73) or ‘All’ (47/73) of the booklets and 71% reported viewing ‘Some’ (8/73) or ‘All’ (44/73) of the DVDs (Table 2). Forty‐five respondents received more than one decision aid, but for consistency of comparisons, we only included patient responses to the first decision aid they received. Nine of the 82 respondents (11%) did not answer the viewership section of the questionnaire for the first decision aid they received.
Table 2.
Viewership of decision aids
| n | Percentage | Some + All | Percentage | |
|---|---|---|---|---|
| View booklets | ||||
| None | 7 | 9% | ||
| Some | 19 | 23% | (19 + 47 = 66) 66/73 | 90% |
| All | 47 | 67% | ||
| Missing | 9 | 11% | ||
| Total | 82 | 100% | 66/82 | 80% |
| View videos | ||||
| None | 21 | 26% | ||
| Some | 8 | 10% | (8 + 44 = 52) 52/73 | 71% |
| All | 44 | 54% | ||
| Missing | 9 | 11% | ||
| Total | 82 | 100% | 52/82 | 63% |
Using chi square analysis to compare the titles of the programmes as a proxy for specialty (we sent three programmes to surgeons and two to oncologists), we found no statistically significant differences in the use of decision aids.
How many patients wrote down a list of questions and how did they use the list?
Of 78 respondents, 63 (81%) reported that they wrote down a list of questions. When asked if they had referred to the list of questions during their appointment, 56 (90%) of those listing questions replied yes; however, only 14 (23%) said they showed the list to their doctor (Table 3).
Table 3.
Usage of communication aids
| n | Yes | No | Missing | Total responses possible | Yes as % responses | Yes as % Total possible | |
|---|---|---|---|---|---|---|---|
| Question lists | |||||||
| Created question list | 78 | 63 | 15 | 4 | 82 | 81 | 77 |
| Referred to question list | 62 | 56 | 6 | 16 | 78 | 90 | 72 |
| Showed QL to MD | 61 | 14 | 47 | 17 | 78 | 23 | 18 |
| Recordings | |||||||
| Brought recorder to appt | 79 | 16 | 63 | 3 | 82 | 20 | 20 |
| Used recorder | 16 | 15 | 1 | 63 | 79 | 94 | 19 |
| Listened to later | 15 | 8 | 7 | 64 | 79 | 53 | 10 |
| Shared with someone | 15 | 6 | 9 | 64 | 79 | 40 | 8 |
| Appointment notes | |||||||
| Took notes | 77 | 51 | 26 | 5 | 82 | 66 | 62 |
| Reviewed notes later | 48 | 37 | 11 | 29 | 77 | 77 | 48 |
| Shared notes with someone | 46 | 28 | 18 | 31 | 77 | 61 | 36 |
Nearly all (96%) patients reported having All (55/72) or Most (14/72) of their questions answered by their provider at the appointment. Using chi square analysis to compare the titles of the programmes as a proxy for specialty, respondents seeing surgeons were more likely to respond to the question ‘did you get all your questions answered’ and generally responded more favourably than those seeing oncologists. Surgeons: 4/54 missing, 42/54 All, 6/54 Most and 2/54 None. Oncologists: 6/28 missing, 13/28 All, 8/28 Most and 1/28 Some.
How many patients successfully recorded their appointments and how did they use the recording?
Sixteen of 79 respondents (20%) reported having brought a recorder to their appointments. Of those 16 patients, all but one reported successfully recording the appointment. Eight of 15 (53%) who made recordings reported having listened to the recording after the appointment. Six of 15 (40%) reported sharing the recording with someone else (Table 3).
How many patients brought someone along to take notes at the appointment and how did they use those notes?
Fifty‐one of 77 patients (66%) said they took notes or had family and friends do so. Twenty (39%) patients said their spouses took notes at the appointment; 18 (35%) said friends or someone else took notes; and 13 (25%) took notes themselves. Thirty‐seven of the respondents (73%) reviewed the notes after the appointment, and 28 (55%) shared the notes with someone else (Table 3).
Were any demographic subsets more likely to follow the prompts and make use of the aids?
We conducted stepwise linear regression for all the demographics (race, Hispanic, education, marital status, employment status, breast cancer stage and age) for each of the three dichotomous variables: question list, recorder and notes.
Question lists
The likelihood for patients to make a list of questions increased by a factor of 1.46 for each unit increase in education (Table 1 for educational levels). Specifically, the odds ratio for making a list of questions was 1.46 [95% CI 0.99–2.16, P = 0.058].
Most who made a list indicated they had referred to the list during the appointment (56/62). In the context of such low variability, demographics were not a predictor of who would refer to the list.
Non‐White, less educated participants were more likely to report showing their question list to their doctors than White participants with more education. Specifically, the odds ratio for showing a list was 4.9 [95% CI: 1.2–21.3, P‐value <0.01] for non‐White race or Hispanic ethnicity compared with non‐Hispanic whites; and 3.7 [95% CI 0.9–15.5, P = 0.05] for education less than a college degree compared with college degree or higher.
Consultation recordings
While there was a greater likelihood for Hispanic patients to bring a recorder (38%) as compared to non‐Hispanics (17%), the small number of Hispanic participants (8) makes this finding non‐significant (P = 0.70). Overall, there were too few observations to determine whether demographics predicted how the recordings were used, although there were trends towards Hispanic and married participants being more likely than average to share the recordings with someone.
Consultation notes
Demographics did not predict whether or not anyone took notes at their appointments or shared the notes later, but increasing education [odds ratio = 1.8 (95% CI: 0.9–3.4, P = 0.060)] and increasing stage [odds ratio = 5.9 (95% CI: 1.3–27.4, P = 0.022)] were associated with increased probability that respondents had reviewed the notes since their appointment.
Decision aids
We conducted regression analysis on how much patients reviewed each decision aid component (DVD or booklet) starting by including all the demographic variables, then removing one at a time (highest P‐value). None of the demographic variables predicted how much of the DVD or booklet respondents reviewed.
Discussion and conclusion
Discussion
Survey administration
All respondents to the email and paper/pencil surveys indicated they had reviewed ‘all’ or ‘some’ of the booklets. Seven of the 31 telephone respondents stated they had not reviewed the booklets, although one had watched ‘all’ of the DVD. The fact that these respondents had not viewed the decision aids may be why they had not completed the survey when invited earlier. This response bias is what motivated us to contact non‐respondents by phone to learn whether visitors who do not respond actually do follow the prompts to use decision and communication aids.
How many patients reviewed the decision aids they received?
Most patients (Table 2) followed the prompts to review the decision aids they received. This makes sense to us because 95% of households in the United States have a DVD player.21 It is also logical that reviewing the booklets have a higher uptake as most people might review the booklet to help them decide whether they wanted to view the companion DVD.
How many patients wrote down a list of questions and how did they use the list?
The uptake on the suggestion to ‘write down your questions’ is also not surprising. In addition to our prompting, more and more resources are making similar suggestions. A popular website available to help patients create their questions is the Agency for Healthcare Research and Quality's ‘Questions are the Answer’ (http://www.ahrq.gov/questions/). Books such as ‘Dr. Susan Love's Breast Book’ suggest questions you should ask your doctor at the end of each chapter22 and two of the decision aids we send include suggested questions for your doctor. Additionally, patients with breast cancer manage families and offices, they make lists on a regular basis (shopping, to‐do, etc.), and so making a list of their questions is a reasonable thing to do.
What surprised us was how few patients (23% of those listing questions) actually showed their list of questions to their physicians. There are possible demographic associations that may explain this (see Were any demographic subsets more likely to follow the prompts and make use of the aids?) or it may be as simple as no one specifically prompted them to show the list to their doctor. In our experience, doctors appreciate knowing the full list of questions in advance or at the start of a visit as this allows them to plan the discussion better. While some physicians are concerned that this might slow down a consultation, a majority of studies that measured the impact of interventions such as prompt sheets on consultation length found no change in the length of appointments.3, 23
Our results are distinct from those of a prior study; Dimoska17 reported that while 91% of the patients seeing radiation oncologists, surgeons and palliative care clinicians accepted a standardized question prompt list, 88.5% reported reading it, but only 44% reported using it during the consultation. We found 90% reported using their question list during the consultation even if only 23% showed it to their doctor. We believe this discrepancy may be explained by the extent to which patients feel their list of questions is personalized. Indeed, in most of the other published research3, 6, 7, 23, 24, 25 on question prompting, the intervention consists of a standardized list of relevant questions that patients personalize by circling those they wish to ask. Patients in our study may have been more likely to use their lists because they were personally generated and therefore perhaps more personally relevant than the standardized lists in the Dimoska study. While prompt sheets do leave patients space to add in additional questions, perhaps question prompting interventions should begin with patients listing their personally unique questions first. Patients may need to be prompted to share their lists with the doctor at the start of the visit, in addition to just making a list of questions and using it during the visit.
Our results demonstrate a ceiling effect towards patients having gotten all their questions answered. While it appears most are getting their questions answered, it may not be sufficient to measure the proportion of questions answered but rather investigate the quantity and range of topics that were asked and answered. Studies have demonstrated coaching increases the number of questions asked from a median of 8.5 to a median of 13.1 Over the last three programme years our records indicate an increase from a mean of 9 to a mean of 23 after coaching. These additional questions might not have been made explicit without coaching and therefore gone unanswered. Future studies should investigate the range of topics asked and answered during consultations.
How many patients successfully recorded their appointments and how did they use the recording?
The prompt with the smallest uptake was the suggestion to make a recording. Less than 20% of respondents reported they had successfully recorded their appointments. We found this result surprising since so much research4, 11, 12, 20, 26 has found audio recordings to be effective in promoting patient recall of complex consultations. In addition to the prompts in our communications with patients, there are signs on our clinic exam room walls suggesting that patients are welcome to borrow a recorder. In other settings, students increasingly record their lectures, and the introduction of the smart phone has made recording interactions as easy as pushing a button or downloading an app. While our patients are older than typical college students, many carry smart phones, and digital recorders are relatively inexpensive, easy to use and small enough to easily transport. We can only speculate on what barriers prevented patients from attempting to make recordings, leading us to the conclusion there is need for further research into the barriers to routine implementation of such an effective communication aid.
While more than half our respondents (8/15 or 53%) indicated they had listened to the recordings later it was such a small sample that we did an analysis of our programme data over the past three programme years. Patients who received coaching and responded to our follow‐up surveys (338/857, 38% response rate) routinely listened to the recordings (175/300 or 58%) and 84% (253/300) said they would recommend recording to others. These numbers are consistent with a recent implementation study promoting consultation recordings in oncology that found 69% of their participants listened to at least a portion of the recording within a week of the consult.27
How many patients brought someone along to take notes at the appointment and how did they use those notes?
Two‐thirds of patients (51/77 or 66%) said that they took notes or had family and friends do so for them. This left over a third who did not have notes; most of whom (21/26) left with neither notes nor recordings. Given the complexity and amount of information to absorb in breast cancer consultations, we are concerned about this gap. We are also concerned about the quality of notes taken by family members or friends. We see an analogy with the practice of having family members or friends serve as language interpreters. This was common in the past but has fallen out of favour for ethical and safety reasons.
Instead of patients depending on their own ability to bring a note taker or take notes themselves, providing a summary of the consultation could be an effective strategy to help patients remember facts from their consultations. Research is mixed on the impact of providing patients with a summary of their consultation and relatively scarce. In van der Meulen's20 systematic review, summaries were not found to contribute as much to patient recall as recordings or a physician endorsing a question prompt sheet; whereas Pitkethly et al.4 endorsed equally providing recordings or summaries of consultations. Further research is needed to clarify whether the quality of consultation summaries has an impact on patient recall of information.
Were any demographic subsets more likely to follow the prompts and make use of the aids?
Our exploratory analyses surfaced associations between using communication aids and race/ethnicity or education that merit further investigation. Our sample size was small but further analysis is warranted to validate our preliminary findings that there is a trend for increased education to be positively related to patients making a list of questions. In addition, while most patients reported not showing their question lists, those that did show their questions to their medical providers were more likely to be non‐White and less educated than the other respondents. In other words, higher education is associated with making a list, but those who showed their lists to the providers were generally less educated and non‐White.
We speculate that non‐White, less educated patients felt the doctor might understand their questions better if the doctor looked at their lists rather than depend on their ability to verbally communicate their questions. Following that logic, our better educated patients may have felt more confident in their ability to communicate directly with their doctors.
Whether or not respondents reviewed their notes after their appointment was also associated with increased education and an increased stage of cancer. The ingrained study skills that go with increased education probably contribute to this population spending more time reviewing their notes. An increased stage of disease is an indication of disease progression associated with poorer outcomes. The need for reflection on the diagnosis, impact on quality of life of treatment options could lead to a need to review the information the physician had provided. Further research on these associations is warranted.
Study quality
The strengths of this study include that it is the only one we are aware of that measures the impact of prompting patients to self‐administer Decision and Communication Aids as part of routine clinical care. Limitations to our study include the fact that this is a small sample of specialty care patients and the results may not generalize beyond our practice. Other limitations include the possibility of a social acceptability bias towards answering positively that respondents looked at some of the programme we sent them. Our low‐response rate might be because it is uncomfortable for patients to admit they have not used our decision and communication aids, motivating them not to return the survey. It was specifically this response bias that motivated us to contact individuals by telephone who had not yet responded to earlier invitations to complete the survey. As telephone respondents were willing to tell us they had not used the decision aids when that was the case, we do not believe social desirability bias is a concern.
Because this was a retrospective study, we have discovered shortcomings in our data tracking mechanisms. While we can identify the total number of individuals who entered the study pool, we did not have a mechanism in place to identify how each respondent arrived into the pool of visitors who had to self‐administer decision and communication aids, limiting our ability to make comparisons between those who refused coaching vs. those we were not able to serve.
Conclusion
Research demonstrates decision aids are valuable tools to improve patient knowledge of key breast cancer facts. Communication aids are associated with patients asking questions and remembering the information provided by physicians. Prompting patients alone was associated with good use of decision aids, but did not assure effective use of communication aids. We have identified two areas where prompting patients by itself is insufficient: Patients did not on their own share their lists with their providers, nor did they make recordings of their consultations. Anecdotally physicians suggest patients will sometimes wait until a doctor literally has his/her hand on the door and is ready to leave to ask the most important question.28, 29 Patients need to be coached to share their questions at the beginning of consultations rather than leaving it up to the medical provider to elicit all their questions.
In specialty settings that make decision aids available and prompt patients to use communication aids, it is reasonable to expect that patients will make good use of decision aids and that they will write down and bring their questions. Prompting alone will probably not get patients to show their lists to their providers at beginning of consultations or make notes and recordings of their own consultations. Providers might request to ‘take a look’ at patient question lists. Clinicians might also consider routinely making recordings of consultations to give to their patients or providing patients with a copy of their dictated notes.
People with cancer may simply be too overwhelmed to manage decision and communication aids without assistance. For these aids to be used most effectively, it may be necessary to do a better job of identifying which patients need coaches to assist connecting them with decision aids, listing their questions and making notes and recordings.13, 14, 15, 16 We are also seeking to expand the pool of available coaches by reducing labour costs by training students who gain experience and academic credit in exchange for providing free assistance with decision and communication aids.10 Additional studies are needed to identify barriers and facilitators to the routine use of audio recordings and consultation summaries in oncology settings.
Sources of funding
The Informed Medical Decisions Foundation develops the breast cancer decision aids and provides funding for Decision Services' core operations and data collection. The UCSF Breast Care Center funds our field operations. We are also sustained by gifts and donations from individuals and organizations including the Safeway Foundation and Wells Fargo. The Informed Medical Decisions Foundation (grant 0015) provided funding for this study. Authors JB, and SV drew partial salary support from a demonstration project grant provided by the Informed Medical Decisions Foundation. The Foundation is a non‐profit corporation that co‐develops the breast cancer decision aids described in this report, and supplies them at no charge to the Decision Services unit of the UCSF Breast Care Center as part of the Foundation's research agenda. The decision aids are co‐developed and distributed commercially by Health Dialog, a subsidiary of Bupa Health Assurance Limited, a global provider of health services based in the United Kingdom. The funding sources had no involvement in any aspect of this study.
Acknowledgements
The authors would like to thank the patients who took the time to reply to our surveys and answer our calls while making critical decisions at a difficult time. We also wish to acknowledge Gail Sorrough and her team at the Fishbon Memorial Library at the University of California, San Francisco, for their ongoing assistance with research; and to Ann Griffin at the UCSF Cancer Registry for ongoing assistance with patient population statistics. Also, the entire faculty and staff of the Breast Care Center cooperates and collaborates with the integration of decision support into the clinic, and several faculty members support the salaries of Decision Services program associates. Many employees of the Breast Care Center, including the premedical program associates who staff Decision Services, assist with data collection. The internship program is grateful to Meredith Buxton, who administers the overall premedical internship program, and Amy Boebel, a donor, for endowing the leadership development component of the internship program.
References
- 1. Brown R, Butow PN, Boyer MJ, Tattersall MH. Promoting patient participation in the cancer consultation: evaluation of a prompt sheet and coaching in question‐asking. British Journal of Cancer, 1999; 80: 242–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. O'Connor AM, Stacey D, Entwistle V et al Decision aids for people facing health treatment or screening decisions. Cochrane Database Systematic Review, 2003; 2: CD001431. [DOI] [PubMed] [Google Scholar]
- 3. Kinnersley P, Edwards A, Hood K et al Interventions before consultations for helping patients address their information needs. Cochrane Database Systematic Review, 2007; 3: CD004565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pitkethly M, Macgillivray S, Ryan R. Recordings or summaries of consultations for people with cancer. Cochrane Database Systematic Review, 2008; 3: CD001539. [DOI] [PubMed] [Google Scholar]
- 5. Belkora JK, Volz S, Teng AE, Moore DH, Loth MK, Sepucha KR. Impact of decision aids in a sustained implementation at a breast care center. Patient Education and Counseling, 2012; 86: 195–204. [DOI] [PubMed] [Google Scholar]
- 6. Butow PN, Dunn SM, Tattersall MH, Jones QJ. Patient participation in the cancer consultation: evaluation of a question prompt sheet. Annals of Oncology, 1994; 5: 199–204. [DOI] [PubMed] [Google Scholar]
- 7. Brown RF, Butow PN, Dunn SM, Tattersall MH. Promoting patient participation and shortening cancer consultations: a randomised trial. British Journal of Cancer, 2001; 85: 1273–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bruera E, Sweeney C, Willey J, Rosales M. Breast cancer patient perception of the helpfulness of a prompt sheet versus a general information sheet during outpatient consultation: a randomized, controlled trial. Journal of Pain and Symptom Management, 2003; 25: 412–419. [DOI] [PubMed] [Google Scholar]
- 9. Butow P, Devine R, Boyer M et al Cancer consultation preparation package: changing patients but not physicians is not enough. Journal of Clinical Oncology, 2004; 22: 4401–4419. [DOI] [PubMed] [Google Scholar]
- 10. Belkora J, Volz S, Loth MK et al Five years of integrating decision and communication aids into routine breast cancer care: an implementation report. 6th International Shared Decision Making Conference. Maastricht, Netherlands; 2011. [Google Scholar]
- 11. Bruera E, Pituskin E, Calder K, Neumann CM, Hanson J. The addition of an audiocassette recording of a consultation to written recommendations for patients with advanced cancer: a randomized, controlled trial. Cancer, 1999; 86: 2420–2425. [PubMed] [Google Scholar]
- 12. Ong LM, Visser MR, Lammes FB, van Der Velden J, Kuenen BC, de Haes JC. Effect of providing cancer patients with the audiotaped initial consultation on satisfaction, recall, and quality of life: a randomized, double‐blind study. Journal of Clinical Oncology, 2000; 18: 3052–3060. [DOI] [PubMed] [Google Scholar]
- 13. Belkora JK, Loth MK, Volz S, Rugo HS. Implementing decision and communication aids to facilitate patient‐centered care in breast cancer: a case study. Patient Education and Counseling, 2009; 77: 360–368. [DOI] [PubMed] [Google Scholar]
- 14. Belkora J, Katapodi M, Moore D, Franklin L, Hopper K, Esserman L. Evaluation of a visit preparation intervention implemented in two rural, underserved counties of Northern California. Patient Education and Counseling, 2006; 64: 350–359. [DOI] [PubMed] [Google Scholar]
- 15. Belkora J, Edlow B, Aviv C, Sepucha K, Esserman L. Training community resource center and clinic personnel to prompt patients in listing questions for doctors: follow‐up interviews about barriers and facilitators to the implementation of consultation planning. Implementation Science, 2008; 3: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Belkora JK, Loth MK, Chen DF, Chen JY, Volz S, Esserman LJ. Monitoring the implementation of Consultation Planning, Recording, and Summarizing in a breast care center. Patient Education and Counseling, 2008; 73: 536–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dimoska A, Butow PN, Lynch J et al Implementing patient question‐prompt lists into routine cancer care. Patient Education and Counseling, 2012; 86: 252–258. [DOI] [PubMed] [Google Scholar]
- 18. Tattersall MH. Consultation audio‐tapes: an information aid, and a quality assurance and research tool. Supportive Care in Cancer, 2002; 10: 217–221. [DOI] [PubMed] [Google Scholar]
- 19. Tattersall MH, Butow PN. Consultation audio tapes: an underused cancer patient information aid and clinical research tool. The Lancet Oncology, 2002; 3: 431–437. [DOI] [PubMed] [Google Scholar]
- 20. van der Meulen N, Jansen J, van Dulmen S, Bensing J, van Weert J. Interventions to improve recall of medical information in cancer patients: a systematic review of the literature. Psycho‐Oncology, 2008; 17: 857–868. [DOI] [PubMed] [Google Scholar]
- 21. Gruenwedel E. Blue‐ray Household Penetration Tops 17%. Home Media Magazine: Questex.com; 2010.
- 22. Love SM, Lindsey K. Dr Susan Love's breast book, 5th edn Cambridge: Da Capo Press, 2010. [Google Scholar]
- 23. Dimoska A, Tattersall MH, Butow PN, Shepherd H, Kinnersley P. Can a “prompt list” empower cancer patients to ask relevant questions? Cancer, 2008; 113: 225–237. [DOI] [PubMed] [Google Scholar]
- 24. Brown RF, Shuk E, Butow P, Edgerson S, Tattersall MH, Ostroff JS. Identifying patient information needs about cancer clinical trials using a Question Prompt List. Patient Education and Counseling, 2011; 84: 69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Clayton J, Butow P, Tattersall M et al Asking questions can help: development and preliminary evaluation of a question prompt list for palliative care patients. British Journal of Cancer, 2003; 89: 2069–2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stephens MR, Gaskell AL, Gent C et al Prospective randomised clinical trial of providing patients with audiotape recordings of their oesophagogastric cancer consultations. Patient Education and Counseling, 2008; 72: 218–222. [DOI] [PubMed] [Google Scholar]
- 27. Hack TF, Ruether JD, Weir LM, Grenier D, Degner LF. Promoting consultation recording practice in oncology: identification of critical implementation factors and determination of patient benefit. Psycho‐Oncology, 2012; 22: 1273–1282. [DOI] [PubMed] [Google Scholar]
- 28. Bahrych S. Taking the time to answer patient questions. KevinMD.com; 2011.
- 29. Krueger J. The patient will see you now. Journal of Participatory Medicine, 2011; 3: e53. [Google Scholar]


