Abstract
Context
Telecare and telehealth developments have recently attracted much attention in research and service development contexts, where their evaluation has predominantly concerned effectiveness and efficiency. Their social and ethical implications, in contrast, have received little scrutiny.
Objective
To develop an ethical framework for telecare systems based on analysis of observations of telecare‐in‐use and citizens’ panel deliberations.
Design
Ethnographic study (observation, work shadowing), interviews, older citizens’ panels and a participative conference.
Setting
Participants’ homes, workplaces and familiar community venues in England, Spain, the Netherlands and Norway 2008–2011.
Results
Older respondents expressed concerns that telecare might be used to replace face‐to‐face/hands‐on care to cut costs. Citizens’ panels strongly advocated ethical and social questions being considered in tandem with technical and policy developments. Older people are too often excluded from telecare system design, and installation is often wrongly seen as a one‐off event. Some systems enhance self‐care by increasing self‐awareness, while others shift agency away from the older person, introducing new forms of dependency.
Conclusions
Telecare has care limitations; it is not a solution, but a shift in networks of relations and responsibilities. Telecare cannot be meaningfully evaluated as an entity, but rather in the situated relations people and technologies create together. Characteristics of ethical telecare include on‐going user/carer engagement in decision making about systems: in‐home system evolution with feedback opportunities built into implementation. System design should be horizontal, ‘two‐way’/interactive rather than vertical or ‘one‐way’. An ethical framework for telecare has been developed from these conclusions (Table 1).
Keywords: ageing, citizens’ panels, ethical framework, technology, telecare
Introduction
In recent years, the development of remote care systems have attracted much attention in terms not only of market development, devices and capabilities, but also forms of clinical and service evaluation, shrinking budgets and demographic ageing.1, 2, 3, 4 Telecare1 systems for older people have largely developed in industry or service contexts where their evaluation has predominantly concerned effectiveness and efficiency, while their social and ethical implications have received little attention. Governmental and industry actors claim that telecare enables older people to play a more active role in managing their own ‘independence, health and well‐being’ and is therefore in tune with UK and European policy shifts towards increased emphasis on individual responsibility for health.5, 6 The recent £3.7 m English Department of Health trial evaluation of telehealth/telecare produced inconclusive results, indicating the scale of complexity in producing evidence about socio‐technical interventions.7, 8, 9, 10, 11, 12
‘Ageing‐in‐place’ underpins almost all government/local authority telecare programmes, an approach which involves staying ‘at home’ as long as possible. In this discourse, demographic ageing creates a ‘burden of care’ that then becomes manageable (only) through technological solutions. However, telecare has been described as inherently complex,13 and the largest group receiving home‐based services is arguably one of Europe's most vulnerable social groups, the oldest old, where ‘third age’ is seen to give way to ‘fourth age’.14, 15 Policy documents argue that telecare will help defuse an ‘age time bomb’:
Telecare has huge potential to support a diverse range of individuals to live at home. It can also give carers more personal freedom, meet potential shortfalls in the workforce and complement the work of clinicians and social care and housing providers to achieve outcomes that improve the health and well‐being of people using services.3
This vision of care, however, may oblige people to stay at home longer than is appropriate for them. While home telecare may have the potential to enhance independence, these developments should not be accepted uncritically, as how telecare technologies shape the domestic space and experience of home may impact quality of life in ways yet to be fully understood. Telecare systems may contribute to prolonging solitary life at ‘home’ when care in a collective setting may be better.
We argue that debate about the ethical and social consequences of these systems for individual users, carers, citizens and practitioners is as important as their structured evaluation in trials. The RCT model, essential in pharmaceutical and much biomedical research, cannot tell us all we need to know where the intervention is in a complex, dynamic context such as home care for older people. Clinical trials cannot deal well with the shifting variables in socio‐technical innovation practices, especially in the presence of significant policy push.16, 17, 18 In this study, we draw on a large, qualitative study in Spain, England, the Netherlands and Norway funded by the European Commission (EFORTT: Ethical Frameworks for Telecare Technologies for older people at home). We organize our findings in four parts: the limitations of telecare; telecare as a shift in networks of relations; telecare as a shift in responsibilities; and telecare as situated practice rather than fixed entity. These findings are then used to provide an ethical framework (Table 1) to be used as a basis by those designing, commissioning, prescribing and working with remote care technologies.
Table 1.
An ethical framework for telecare
| This is laid out as a series of questions to be openly considered and deliberated by users, carers, policy makers and professionals: this is not a checklist for ‘yes/no’ answers, but a framework for mature debate and aid to decision making |
| Design: Who is involved? |
| Who needs to be consulted, to participate in system design and to decide which needs are going to be met? Telecare should be designed, shaped and trialled through consultation with a broad range of actors. Many older people are ready and willing to participate in these processes: it is up to industry, government and providers to facilitate this activity, in collaboration with established networks of older people. Telecare that is produced without appropriate and meaningful consultation and engagement will not meet the needs of older people |
| Policy and practice: What problems can telecare help with? How do other problems fit in or not? |
| Although telecare can be very useful in an emergency situation and has other specific roles, it cannot function as a panacea for problems associated with ageing. There are needs that it cannot recognise or meet. When telecare is designed to enhance (or can be used for) social support, it seems very popular. More often it is used to monitor older people who remain rather passive: if they are more active in using the system for social contact this is seen as ‘misuse’. Telecare systems could be used to promote social relationships that are more horizontal and active rather than vertical and passive |
| Use and implementation: who is connected to the telecare system? |
| The installation of a telecare system opens up questions of privacy and confidentiality, highlighting complex issues about the ownership, use and control of personal information and sensor data. The availability of data raises questions about access to it. Information about an older person's activities in their home, or their feelings about their chronic illness, is powerful. The sharing of such information has the potential to change relationships of care: between parents and adult offspring and between paid carers and older people. Some developers recommend the use of telecare to monitor the capacities of older people living alone. It must be made clear to the older person at the point of installation that this might happen |
| Experience of use: how might a telecare device change an older person's home? |
| The aim of staying at home should be opened up to question, rather than assumed. Although many older people strongly desire to remain in their own homes as long as possible, this might not be so appealing if ‘home’ is under scrutiny and is the object of constant monitoring. Telecare systems run the risk of turning homes into ‘institutions’. Strong efforts should be made to minimise the disturbance to people's homes: designers, prescribers and installers must take seriously the objections of older people to such intrusions. Telecare devices can diminish people's sense of security despite their aims to do the opposite: they can make people feel vulnerable and scrutinised |
| Experience of use: who will be the active user of the telecare system: the older person/and others? |
| Becoming a user of telecare is to take on a new identity and accept a new network of connections in which older people have a particular (and quite limited) set of roles. There are notable differences in older peoples’ experiences of telecare systems where they can maintain physical control (e.g. activate alarms to request help) and those in which alarms are triggered environmentally. The latter lead to more ‘false alarms’, creating difficult work for tele‐operators and others involved in monitoring, and can create unnecessary concerns for older people and their families. Using telecare systems puts older people into new relations both with people they know, or have never met (but may come to know). These changes should be openly discussed with prospective users of telecare |
| Policy: is it worth the effort? |
| Telecare involves a lot of work for many different groups and creates new forms of labour, both for providers and so‐called users: it is not necessarily time or cost saving. In most cases, telecare cannot prevent negative incidents: it cannot stop people falling, becoming ill, or getting lost. Its two main functions are to triage assistance and/or enable support. Some telecare systems require a lot of effort from users, who need to log on daily or weekly to answer difficult questions and report on their health. Given that the telecare system is not usually going to prevent negative occurrences, is it really worth the installation and maintenance effort? Potential users and others need to balance the costs of the (material and emotional) labour involved against the benefits of being involved |
| Politics, choice and flexibility |
| Sometimes older people receive telecare as part of trials or pilot studies designed to test the acceptability and workability of particular systems. This is often a positive experience for older people, who enjoy being involved in a detailed analysis. Trial results are often positive due to the care and attention this stage of development attracts. Difficult decisions must then be made at the conclusion of such studies: it would be unethical to remove technologies from people who had come to rely on them, without an adequate substitute. Conversely, it is sometimes unclear to older people how they can have telecare removed from their homes. Older people must be able to change their minds about accepting telecare, which itself should be adaptable (open to supplementation/reduction). The prescription and installation of telecare is a complex process. Practical questions of cost to individuals and health services are paramount. In some countries, national policies put pressure on local authorities to commission telecare services, which may then be prescribed to individuals who may not benefit. Families may also pressurise individuals to accept systems they do not actually understand or want. There is a widespread presumption that telecare saves funds by reducing demand for collective living and reducing demand on other care services, but this assumption is simplistic and needs to be carefully scrutinised and analysed |
| Practice dynamics: what would happen if the older person's condition deteriorated? |
| Older people's lives can be subject to rapid change: often telecare is prescribed to very vulnerable people who are on the edge of being unable to manage on their own or who have serious chronic disease, with high support needs. Telecare is often installed as a ‘last ditch’ effort to help people stay ‘at home’. The systems themselves, however may be ‘static’, unable to change according to individuals’ needs. Some devices can be reprogrammed (e.g. bed sensors) but this requires ongoing analysis of how the current arrangements are benefiting the ‘users’. In some countries telecare is not well supported, so devices remain unused: either because older people/families do not understand how to use them, or because the device no longer meets the person's needs. Individuals – both professionals and others – need ongoing training about telecare systems so they can use them as effectively as possible |
Study design
Our study was underpinned by the concept of empirical ethics, that is, the argument that what is ‘good care’ is not only understood through the application of the four principles of medical ethics,19 or determined by clinical trial evaluations, but is understood through the studies of care in daily practice, in this case through observations of care settings. Hence, what constitutes good practice cannot be fully determined in advance, but emerges in and through the work of service users and practitioners.20, 21 This point contrasts with the approach often taken by telecare evaluators where there is a belief that both interventions and care practices can be sufficiently controlled to be measured, and where the merits of technology are often conflated with fiscal efficiency.22
The range of our research data is described in Table 2. EFORTT was not a comparative international study but an exploration of ethical issues arising from installation of different telecare systems in Spain, Norway, England and the Netherlands. In each country, an advisory group, drawn from older peoples’ groups, health, social care, academic and industry sectors, met every 6 months to guide the project. We followed telecare applications as closely and in as much detail as possible. This included observations of meetings where practitioners were attempting to make telecare systems work, or where managers were attempting to increase the visibility and uptake of telecare systems. It included extended observations at local telecare call/monitoring centres; telecare installation visits to older peoples’ homes; shadowing social workers or other professionals undertaking needs assessment and telecare referrals; telecare training events; and attendance at technology, medical and policy‐related conferences. We also conducted interviews with older people who had home telecare systems installed, technology developers and providers, and analysed the key policy documents.
Table 2.
Collection of data
| Spain: a study of home telecare services in Catalonia. Field notes from observations of and transcripts of interviews with Red Cross and other monitoring centre workers, home telecare managers and teleoperators, users and volunteers, and telecare designers. Group discussion transcripts with telecare users and health‐care and social care professionals. Documentary analysis |
| England: a study of the implementation of home telecare, initially funded under the Preventative Technology Grant, in one large local authority (system usually consisted a pendant alarm plus two other linked sensors, for example fall detector, gas detector, pill dispenser, bed monitor). Field notes from observations of and transcripts of recorded interviews with telecare system monitoring centre workers, installers and older telecare users. Group discussion transcripts with social workers, managers, occupational therapists, technology developers. Analysis of policy documents |
| The Netherlands: a study of telehealth projects. Field notes of observations and interview transcripts from the Health Buddy remote care device in oncology and the PAL4 home web camera system used alongside the Health Buddy. Documentary analysis |
| Norway: a study of web‐ and satellite‐based care systems. Field notes of observations and interview transcripts from the web‐based ‘SecurityNet’ and the use of GPS devices in dementia care. Interviews for SecurityNet included health‐care professionals, project managers, administrators in municipal health‐care services, designers and users; for the GPS system: informal and formal carers, relatives, designers, social care and health‐care authority workers. Documentary analysis |
In addition, we held 22 citizens’ panels: introductory and follow‐up meetings (Table 3). Panel members were older people and carers drawn from outside the observational/ethnographic study. Recruitment of older people (such as those who are receiving care services, both home‐based and institutional) to citizen panels was unsurprisingly challenging. The four research teams contacted voluntary/community organizations, older people's forums, senior citizen centres and carers’ support groups to identify a range of respondents. Unfortunately, in the 18 months between the introductory and follow‐up panels, some members’ health had declined and some had died; we then held extra meetings to maintain the range of respondents.
Table 3.
Citizens’ panels
| Country | Date | Participants | Composition |
|---|---|---|---|
| Introductory panels | |||
| England | 14 July 2008 | 8 | Older people |
| England | 11 August 2008 | 10 | Older people in independent assisted accommodation |
| England | 26 May 2009 | 8 | Informal carers |
| England | November 2009 | 6 | Older people/informal carers |
| England | December 2009 | 6 | Older people/informal carers |
| The Netherlands | 10 November 2008 | 8 | Older people |
| The Netherlands | 24 November 2008 | 5 | Informal carers |
| The Netherlands | 2 December 2008 | 7 | Informal carers |
| Norway | 8 September 2008 | 6 | Older people |
| Norway | 10 September 2008 | 8 | Carers |
| Norway | 29 October 2008 | 8 | Older people/carers |
| Spain | 19 July 2008 | 7 | Older people |
| Spain | 19 July 2008 | 4 | Carers |
| Follow‐up panels | |||
| England | 10 June 2010 | 15 | Older people in independent assisted accommodation |
| England | 10 June 2010 | 5 | Older people/informal carers |
| England | 18 June 2010 | 14 | Older people/informal carers |
| The Netherlands | 12 May 2010 | 7 | Older people/informal carers |
| The Netherlands | 17 May 2010 | 8 | Older people/informal carers |
| Norway | 16 June 2010 | 5 | Older people |
| Norway | 17 June 2010 | 3 | Carers |
| Spain | 26 July 2010 | 9 | Older people |
| Spain | 26 July 2010 | 9 | Carers |
In the introductory panels, members were first presented with the aims of the EFORTT project and some examples of telecare systems; they then reflected on the issues at stake for older people living at home. In the follow‐up panels, they provided comment on the preliminary findings of the observational work and suggestions for an ethical framework for telecare technologies. As in previous citizen panel work in this field,23, 24, 25 we conceptualized these panels as critical policy forums offering independent views on issues of significance to policy on ageing and to practice in health and social care for older people.
The event ‘Ageing with Technologies: a participative conference on care in Europe’, in Barcelona (see website), drew 118 participants from older peoples’ organizations, health‐care/social care practice, technology companies and service providers. Following a brief presentation from EFORTT, discussion groups considered project findings and draft points for the ethical framework. We digitally recorded all deliberations, interviews, citizens’ panels and group discussions with consent. All details that might lead to the identification of individuals were removed, and pseudonyms used for respondents’ names. The sequence of EFORTT research methods is shown in Fig. 1.
Figure 1.
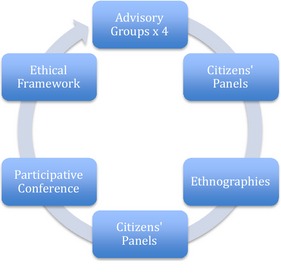
EFORTT research process.
Transcripts of field notes, interviews, conference discussions and citizens’ panels deliberations were analysed by each team alongside the relevant policy documents from each country, and recurring themes were identified. Extracts (from each form of data) were then selected and translated for distribution across the project, along with these preliminary analyses. A 2‐day ‘data clinic’ for all researchers was convened in Norway where the extracts were subjected to fresh readings; themes were debated and then analysis from the four studies brought together. The findings below are the result of this iterative and deliberative process. We have made selections from our empirical data to illustrate each finding (and underpin the recommendations embodied in Table 1), but inevitably, these selections can be only partial exemplars and many others could have been chosen. In addition, in‐depth analysis of country‐specific findings is published elsewhere.26, 27 In this way, Table 1 is derived from the iterative analysis, informed and refined by the citizens’ panels and participative conference, as illustrated in Fig. 1.
Large studies of telecare‐in‐use are still rare because of the ethical and practical difficulties in gaining access to accounts of the daily experience of ‘real’ older users. Our research achieved a measure of success here, but we acknowledge that this part of the study was limited to particular devices and contexts. The possibility of drawing conclusions across and between very different cultural, policy and technical contexts is limited, but our central argument against universal and benign images of telecare systems is supported by the data from all the four countries. The participative nature of the study exposed the design and analysis to frequent comment and challenge.
The theoretical background of the analysis is informed by science and technology studies (STS), in which it has been established through many detailed studies that technical systems both shape, and are shaped by, society. This socio‐technical approach means that as technologies are developed, so society is developed; in this case, therefore, telecare systems for older people may reflect the values of that society, a point we return to in the Discussion.28, 29
Principal findings and their ethical practice implications
Below, we detail the major findings that emerged from our study as a whole. Each of these is linked with questions and recommendations given in the ethical framework in Table 1. For each finding, we also give a fieldwork example, chosen from the data explored in our joint analysis.
Telecare has care limitations
There are many care tasks that telecare cannot do: see Table 1
Telecare does not perform care on its own, but becomes part of new forms of caring relations and activities. Contrary to many expectations, it creates additional work, introducing new tasks, skills and responsibilities. New actors are involved including installers, teleoperators, instructors, service providers and service workers, in addition to drawing on family carers, neighbours, friends and volunteers. Respondents were insistent that telecare should not be seen as a substitute for ‘human carers’:
We want to ensure that whatever the technology is, it isn't simply replacing the person who is currently giving the care. The huge danger is that if we go down that road to any great extent, it is so easy because of financial implications to reduce the personal input. It is so important not to replace that human contact.
(Citizens’ Panel Northshire, England)
Telecare is not a solution, but a shift in networks of relations
Telecare practice draws on a large socio‐technical system or network: see Table 1
Telecare does involve different forms of ‘human contact’; systems of alarms and sensors do not work effectively if the older person has no social network. In the English study of home sensors and alarms, for example, telecare monitoring centre staff stressed the continuing importance of immediate family or neighbourly ‘contacts’ when problems arose:
Telecare monitoring centre operator
You know a lot of the [people living with] Alzheimer's, things like that where their memory's going… I mean we've got gas detectors in and you go through and you're talking to them and you say ‘Can you smell any gas? Can you check your cooker for me?’ [They say] ‘I haven't got a gas cooker’ and they have, you know… So you just have to get someone [to go out]… I've always said telecare's only as good as the contacts we've got. If you can't get somebody to go and check on that, you know, you're really struggling, because the police don't want to know every few minutes [or] to be going. So the more contacts we can get with the telecare the better, because that's what we have to rely on you see.
Researcher So it's about the network –
Telecare monitoring centre operator it is
Researcher around that person?
Telecare monitoring centre operator Yes. Then we've got one or two… that have got nobody.
(Observation, English telecare monitoring centre)
The work of monitoring centre workers, predominantly women, involves unrecognized complexity and uncertainty and can be stressful. The current expansion of these call centres carries the risk of globalization of provision and dilution of care quality.30
This implies a shift in responsibilities
Tasks become redistributed in telecare systems: see Table 1
Using telecare systems involves a range of new activities for carers and older people. This became evident in the Norwegian study of wearable GPS tracking devices where researchers learned how relatives of older people living with dementia needed to take on new responsibilities, from charging the batteries in the device to making sure the ‘patient’ remembered to carry it. They also needed to take care of system payments and maintain contact with telecare agents and providers:
Technical aids come with an extra demand: that I as a next of kin will manage this; that I am able to sort it out and manage it, and follow it up and maintain it…..
(Norwegian carer for partner with dementia)
Sometimes, telecare shifts responsibility away from its traditional locations to other actors: for an older person living alone, the importance of neighbours rather than (necessarily) family members was stressed (neighbours can more easily check on older people and/or let care providers into the older person's house):
We only need them [family] if the user has not answered the control check for many days. Then we call the relatives to find out if the person is alright, but apart from that…neighbours who hold keys are more useful than relatives.
(Spanish personal home telecare coordinator)
Telecare projects an ideal ‘active user’: see Table 1
This ‘active user’ is the one who follows instructions/rules. In the Dutch Health Buddy monitoring system, patients must respond to a daily set of questions; if they fail to do so, a nurse will call them. The understanding of good care here is closely related to self‐management, which itself related to the ideas of independence and autonomy such as living alone and moving freely. Hence, good care is seen as being responsible and if possible, playing a part in preventing conditions, such as chronic obstructive pulmonary disease, from deteriorating.
Mr. V has a connection with the COPD nurse via a webcam and a Health Buddy for monitoring his symptoms.
Mr. V Well, I typed in a few times that I was out of breath. And then they phone me up, because I could be in the red [the nurses get a red alert, demanding their action]. This means you are in the danger zone. And then, they call at once, really. And they say: ‘Yes, you need to see the doctor’. But I am not the type to run to the doctor. And then they call the next day and they say: ‘Mr. V, what did the doctor say?’ And then I say: ‘No, I did not go.’ ‘Yes, but you should learn to listen’, because you know, when we [COPD patients] get inflammation, then it is for us, of course, really fatal. Because every inflammation we get, is at the expense of your lungs. The alveolus [part of the lungs] are destroyed.
Researcher And this cannot be repaired?
Mr V No, that's what I am saying. When you have COPD, you keep it like it is or it gets worse. See, you have diseases that get better, but this, cannot; it will never get better. That's just it.
Researcher So that is why they push you like this?
Mr V Yes, yes. And then they say: ‘Yes Mr. V, you should learn to listen’.
(Observation, Dutch telehealth user's home)
However, as with other monitoring devices, the Health Buddy user learns that if abnormal readings are transmitted, a call will be triggered, so responsibility passes, in this case, to a professional. The projected ideal of active user is also in some ways a passive one. She/he is active in certain ways and compliant in others.
Telecare may lead to decreased privacy for older people or may be intrusive: see Table 1
Good care sustains privacy, and while telecare may enhance privacy if it enables reduction in home visits, in some situations privacy may be threatened, for instance, by movement sensors in the home or devices using GPS tracking. Complex negotiation between the alternatives of perceived loss of privacy and possible increased liberty by the users and carers is called for. Some clients using telecare for health monitoring feel that it can be intrusive as it frequently confronts them with their condition, for example where they are required to answer a set of questions about their illness on a daily basis.
The project manager says: ‘There weren't many refusers, but those who were there, handed their Health Buddy back in the first week they had it. They either found the use too strenuous [they were too ill], or too confronting, meaning that they did not want to think about questions of death & dying, possible symptoms or the impact of the disease on their lives’.
(Dutch field notes, telecare project group meeting)
Telecare sometimes offers ‘peace of mind’: see Table 1
Good telecare practice was widely described as reassuring. This is particularly noticeable in the use of alarm pendants: even if the pendant is never or hardly actually activated, it can provide reassurance for the older person and her/his family and friends.
I consider telecare as a complement. In case of an emergency, it is a complement, because if something happens to me, the first thing I do is to call my daughter or son. And if I press that button, their telephone number appears immediately.
(Group discussion with telecare users, Spain)
However, there is a risk of false reassurance, as in the case of the Dutch respondent who had monitored her weight and blood pressure twice a day via her telecare device, but was then very upset when she suffered a heart attack.
Telecare cannot be meaningfully evaluated as an entity, but rather in the situated relations people and technologies create together
Older people living at home often use telecare in unorthodox and unpredicted ways: see Table 1
In each country, we found examples of older people refusing to wear their pendants (or being selective about when and where they put them on) or to use monitors and asking to have systems taken away. Inability to comprehend the system may result in non‐use. We observed in the English study a client who left her falls monitor, designed to be worn around the waist, carefully on the shelf in order not to activate it. And in Spain:
….and so I keep repeating. Its not enough to keep explaining…. When the woman found the other man who had died in bed in the morning, he was cold. What he should have done was press the button to activate the means of help, surely. Instead he went out into the street and called the neighbour.
(Group interview with Spanish telecare workers)
Some older people used telecare to meet needs for which the service was not designed. Often, these are social needs: some clients ‘over‐used’ telecare to get social contact with monitoring centre operators. Such over‐use or ‘misuse’ was considered problematic by social care managers observed in the English study, who suggested at a telecare project meeting that such people should have the system removed from their homes. In Spain, the issue of ‘non‐compliance’ was regarded as a risk for the providers:
We always tell them to use it and they say, ‘Yes, yes, I will wear it, from tomorrow’. And then later, they do what they want.
(Group interview with telecare workers and volunteers)
Some informal/family carers ‘customize’ devices to suit the particular needs of the individual or setting: see Table 1
Carers looking after older people also tinkered with the technologies to adapt them for their particular situation. One Norwegian carer described using matchsticks and tape to ensure that her husband (who has dementia) did not accidentally set off his alarm.
It is a challenge to get him to take it with him. I found a small pouch for a mobile phone with a key‐ring. He still remembers to lock the door. It was a routine I knew he still had. And he takes the GPS with him 80% of the time. But then the pouch was too thin I found. Because when he had it in his pocket he pressed the button by accident, so it switched itself off. So I bought a new pouch with a key ring. And then I made this homemade solution of placing match sticks and tape in a frame around the ‘off’ button so that the button is sheltered.
(Norwegian carer)
Some health‐care and social care workers also find it necessary to modify systems to enhance workability. Such ‘tinkering’ to make them work more efficiently, more affordable or improve workflow stemmed from interaction with and involvement of older people. In Norway, as its pilot period was completed and the web‐based support system SecurityNet was established as a service by the municipality, a small (local) company was given responsibility for the development/maintenance of the system:
In the beginning we had a good deal of contact with the elderly participants. It was then we got the feedback that the video picture was too small. And there was too many buttons. So we did quite a bit of development‐work. (…) I have met all of them.
(Norwegian ICT developer)
Systems can fail: see Table 1
Although telecare can enhance older people's freedom to move around, system failure can create dangers.
We had this very serious incident recently. It was late autumn and quite cold. And he [her husband] walked into the nearby forest. And in this area the GPS is very unspecific. In the forest there are tracks only. I searched for him several times and became very anxious. And then the battery stopped working! In the end I got hold of him on the telephone. But he was unable to tell me where he was. And he was very scared. I called him later and then he thought he knew where he was. 1½ hours later he got home. Then he had been away for 7 ½ hours without food or drink. He was soaked and panicked and his shoes were full of water.
(Norwegian carer)
Discussion
Telecare does not offer a ‘technological fix’ to replace either existing health‐care services or informal care networks: it is not a simple solution to care crises, personnel crises or budget crises in ageing societies. The policy aim, that telecare will be effective for people living alone and lacking social networks, does not appear to be based on empirical evidence, which tends to show the opposite. Telecare either sustains/develops a network that is already in place or needs to mobilize and install a new network if there is no existing one. Telecare rests upon and is dependent upon networks, including volunteers and family carers. Existing or new care networks can be supported by meaningful consultation with potential ‘users’ starting from the goals, values and life history of the older person.31
There are clear limits to what telecare systems can do – they cannot, for instance, help people to the toilet or clean the house. Telecare is not ‘effective’ in itself; to say it is ‘good’ does not identify a property of particular technical devices, but how they become integrated in networks of users and technologies.
Through telecare, responsibilities in care networks are shifted and delegated in new ways. More responsibility may be shifted onto the individual user/older person, who is now given the task of caring for and looking after her/himself. Such systems may make users aware and conscious of themselves in new ways and teach them to examine and evaluate themselves, their bodies and themselves as persons, in ways they previously did not. But other forms of home telecare, which are more ‘passive’ or monitoring based, shift agency away from the older person, where decisions can be taken based on sensor/movement data about which the client may not be aware. As our colleagues in Spain have elaborated, independence and dependence are very finely balanced.32 Further, independence may be enhanced in cases of dementia such as being enabled to walk freely, but this often creates new responsibilities for carers who may find monitoring or tracking devices liberate them from the need for constant vigilance, while other tasks are introduced. Through home telecare, the redistribution of tasks also implies new meanings for privacy and confidentiality, both in the collection of data about personal movement, but also in the sense that one's home is ‘opened’ to a range of others who may call, check or visit.
This study demonstrates the meaninglessness of talking about care technologies themselves in terms of good/bad, effective/ineffective, outside of their context of use. It shows that telecare is not neutral and that the good/bad debate is a reduction in the complexity of the phenomenon. We show that poor telecare design results in wrong assumptions about the role and identity of the ‘user’ and that older peoples’ customization of devices is both legitimate and often necessary to make devices ‘work’ in context. We show the importance of recognizing the limits to telecare, revealed through practice in the face of rather over‐optimistic policy.
We believe our work highlights the value of the empirical ethics approach and the growing contribution of science and technology studies to the field of health technology assessment. What we claim to add to the STS literature is in moving beyond analysis in our engagement with normative questions, as a way to intervene in telecare development (i.e. with the ethical framework in Table 1).27, 33, 34
An ethic of telecare emerges from this approach. The research data about the creative use and non‐use of telecare raise questions about what ‘proper use’ is thought to be in each context. It shows that telecare should not be understood as a universal solution, but a situated one. We argue that people's creativity in customizing systems and adaptability using them is essential to the ‘ethical’ practice of telecare and that these should be respected and accommodated, rather than seen as a problem to be eliminated. In this way, telecare systems (in design and implementation) might enhance independence and avoid becoming totalizing and coercive.
Funding
Funding was provided under the EU FP7 Science in Society Programme, Project No. 217787.
Competing interests
None.
Ethical approval
Ethical approval was granted for the English study by Northshire Council research ethics committee on 29 May 2008, and all participants provided written informed consent. Approvals in Spain, the Netherlands and Norway were obtained in accordance with respective local and national requirements. All transcripts have been anonymized.
Acknowledgements
We wish to thank all the members of the older citizens’ panels in England, Spain, Norway and the Netherlands. We are grateful to the older people who allowed us to visit them in their homes; to the telecare providers and workers; and to social workers, managers and commissioners in all the four countries who gave us their time for observations and interviews. We also wish to thank the EFORTT project officer Josephine Baxter for her invaluable contribution to the project process and the other EFORTT investigators: Christine Milligan, Elham Kashefi (England); Daniel Lopez, Blanca Callen, Tomas Sanchez‐Criado (Spain); Hilde Thygesen (Norway) and Dick Willems (the Netherlands). We are also grateful to Louis Neven who as a visiting PhD student accompanied the English team on two citizen panels.
Note
Telecare is defined by the English Department of Health as ‘…aimed at vulnerable people who need the support of Social Care or Health Services to keep living on their own. For example those with physical disabilities, the frail and elderly or those suffering from dementia or epilepsy’. Telehealth is defined as ‘…aimed at helping people manage their long‐term health conditions in their own home (e.g. diabetes, heart failure and/or chronic obstructive pulmonary disease)’. There is much confusion (and conflation) about telecare and telehealth and the relationship between them. While telecare usually refers to social care such as safety and security systems, and telehealth to systems aimed at home management of particular medical conditions such as COPD, this distinction is largely a UK one, and we found ‘telecare’ to be often used for both in our partner countries. The distinction is also largely artificial in that, for example, older people assessed as having care needs may also develop medical conditions, and younger people with chronic conditions may also have care needs. Our working definition of telecare is the provision of health and social care at a distance using new technologies.
References
- 1. Audit Commission . Implementing Telecare. London: Audit Commission, 2004. [Google Scholar]
- 2. Department of Health . Building Telecare in England. London: Department of Health, 2005. [Google Scholar]
- 3. Walker K. Britain's Age Timebomb. http://www.dailymail.co.uk/news/article-2009269/Cost-1-4m-extra-pensioners-means-NHS-stay-free.html#ixzz1jzbunyj2. Daily Mail, 29 June 2011 (accessed 29 March 2013).
- 4. Office of the Deputy Prime Minister/Department of Health . Preventative Technology Grant 2006/07 – 2007/08, Local Authority Circular, LAC (2006) 5.
- 5. 3millionlives . Improving access to telehealth and telecare. http://3millionlives.co.uk/ (accessed 29 March 2013).
- 6. Tunstall/WSD Knowledge Bank , http://www.tunstallwsd.co.uk/ (accessed 29 March 2013).
- 7. Department of Health . Whole Systems Demonstrators: an overview of telecare and telehealth, http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_100946 (accessed 29 March 2013).
- 8. McCartney M. Show us the evidence for telehealth. British Medical Journal, 2012; 344: e469. [DOI] [PubMed] [Google Scholar]
- 9. Sharvill N. Daily contact with a nurse may be more important that high tech telecare. British Medical Journal, 2012; 344: e875. [DOI] [PubMed] [Google Scholar]
- 10. Praities N. Telemedicine unlikely to be cost effective admit researchers, http://www.pulsetoday.co.uk/newsarticle-content/-/article_display_list/13585495/telemedicine-unlikely-to-be-cost-effective-admit-researchers-leading-dh-pilot (accessed 29 March 2013).
- 11. Steventon A, Bardsley M, Billings J et al Effect of telehealth on use of secondary care and mortality: findings from the whole system demonstrator cluster randomised trial. British Medical Journal, 2012; 344: e3874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Goodwin N. Jumping the Gun in the telehealth steeplechase. http://www.kingsfund.org.uk/blog/2012/07/jumping-gun-telehealth-steeplechase (accessed 29 March 2013).
- 13. Barlow J, Bayer S, Curry R. Implementing complex innovations in fluid multi‐stakeholder environments: experiences of telecare. Technovation, 2006; 26: 396–496. [Google Scholar]
- 14. Laslett P. A Fresh Map of Life: The Emergence of the Third Age. London: Weidenfield and Nicholson, 1989. [Google Scholar]
- 15. OECD . Long‐Term Care for Older People: The OECD Health Project. Paris: OECD Publishing, 2005. [Google Scholar]
- 16. May C, Mort M, Williams T, Mair F, Gask L. Health technology assessment in its local contexts: studies of telehealthcare. Social Science and Medicine, 2003; 57: 697–710. [DOI] [PubMed] [Google Scholar]
- 17. Pols J. Care at a Distance: On the Closeness of Technology, Amsterdam: Amsterdam University Press, 2012. [Google Scholar]
- 18. Greenhalgh T. Whole Systems Demonstrator: Policy, politics and publications ethics, Rapid Responses to Steventon et al 2012, http://www.bmj.com/content/344/bmj.33874/rr/591291 (accessed 3 Jan 2013).
- 19. Beauchamp T, Childress J. Principles of Biomedical Ethics, 5th edn New York: Oxford University Press, 2001. [Google Scholar]
- 20. Borry P, Schtormans P, Dierikx K. Empirical ethics: a challenge to bioethics medicine. Health Care and Philosophy, 2004; 7: 1–3. [Google Scholar]
- 21. Mol A. The Logic of Care. New York: Routledge, 2008. [Google Scholar]
- 22. Eccles A. Ethical Considerations Around the Implementation of Telecare technologies. Journal of Technology in Human Services, 2010; 28: 44–59. [Google Scholar]
- 23. Mort M, Finch T. Generating Principles for Telehealthcare: a Citizens’ Panel Perspective. Journal of Telemedicine and Telecare, 2005; 11: 1. [DOI] [PubMed] [Google Scholar]
- 24. King G, Heaney DJ, Boddy D, O'Donnell CA, Clark JS, Mair FS. Exploring public perspectives on e‐health: findings from two citizen juries. Health Expectations, 2011; 14: 351–360. doi:10.1111/j.1369‐7625.2010.00637.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kashefi E, Mort M. Grounded citizens’ juries: a tool for health activism? Health Expectations, 2004; 7: 290–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mort M, Roberts C, Callen B. Ageing with telecare: care or coercion in austerity? Sociology of Health and Illness, 2013; 35: 799–812. [DOI] [PubMed] [Google Scholar]
- 27. Roberts C, Mort M, Milligan C. Calling for Care: ‘Disembodied’ Work, Teleoperators and Older People Living at Home. Sociology, 2012; 46: 490–506. [Google Scholar]
- 28. Brown N, Webster A. New Medical Technologies and Society: Reordering Life. Cambridge: Polity Press, 2004. [Google Scholar]
- 29. Mackenzie D, Wajcman J (eds). The Social Shaping of Technology, 2nd edn Buckingham: Open University Press, 1999. [Google Scholar]
- 30.Ethical Frameworks for Telecare Technologies for older people at home, Final Report of EC FP7 Science in Society project no 217797, 2011, 25. downloadable from www.lancs.ac.uk/efortt/ (accessed 1 Aug 2012).
- 31. Bailey C, Sheehan C. Technology, older persons’ perspectives and the anthropological ethnographic lens. ALTER, European Journal of Disability Research, 2009; 3: 179–197. [Google Scholar]
- 32. Sánchez Criado T. Las lógicas del telecuidado: La fabricación de la ‘autonomía conectada’ en la teleasistencia para personas mayores. PhD thesis, Department. of Social Anthropology, Universidad Autónoma de Madrid, 2012.
- 33. Willems D. Varieties of goodness in high‐tech home care In: Mol A, Moser I, Pols J. (eds) Care in Practice. On Tinkering in Clinics, Homes and Farms. Bielefeld: Transcript verlag, 2010: 257–276. [Google Scholar]
- 34. Willems D, Pols J. Goodness! The empirical turn in health care ethics. Medische Antropologie/ Medical Anthropology, 2010; 22: 161–170. [Google Scholar]


