Abstract
Context
Eliciting patients' views of type 2 diabetes self‐management provides insights on how policy and services might better support the needs of this population.
Objective
To synthesize black and ethnic minority patients' views on the barriers and facilitators influencing the self‐management of type 2 diabetes.
Search strategy
A systematic search of international literature published in nine electronic databases was undertaken in 2008. Search strategies used both MeSH and free‐text terms. Two relevant journals were also hand searched.
Inclusion criteria
Any primary empirical study published in the English language since 1986 that reported black and ethnic minority patients' views on type 2 diabetes self‐management.
Data extraction and synthesis
Data were extracted and study quality was formally assessed. Data were analysed using thematic synthesis.
Main results
Fifty‐seven studies were included, of qualitative (n = 54), mixed‐method (n = 2) or quantitative (n = 1) design. Studies were from North America (n = 41), Europe (n = 14) and Australia (n = 2), including 1735 participants in total. Three analytical themes emerged: ‘Importance of identity’; ‘Being understood by others’ and ‘Making sense of condition’, all linked conceptually under the overarching theme ‘Sense of self’. The quality of the studies varied.
Discussion and conclusions
The findings provide insight into what black and minority ethnic people regard as the barriers to, and facilitators of self‐management, as opposed to what health professionals, policy makers and trial researchers may have assumed. Recognition of the views of people with diabetes is essential for the design and delivery of patient‐centred care and policies.
Keywords: ethnicity, minority, qualitative, self‐management, systematic review, type 2 diabetes
Introduction
Worldwide the prevalence of type 2 diabetes mellitus (T2D) is increasing1 and it is now the fifth most common cause of death.2 In 2009 2.3 million people in the UK had T2D,3 while globally it is estimated that 171 million people live with the condition and this is expected to increase to 366 million by 2030.4 T2D is associated with a range of acute and long‐term complications, including heart and circulatory disorders, renal failure and sight loss.5
Black and minority ethnic (BME) groups are at higher risk of developing T2D,6 and diabetes outcomes tend to be worse among people from some BME and socially deprived groups.7, 8 One factor contributing to poorer outcomes is an inadequate match of health and social care to the needs of these patient groups; thus designing more appropriate policy and interventions may impact on health inequalities.9 To do this, patients' views of T2D and the factors that influence their ability to manage the condition, need to be better understood.
By maintaining good glycaemic control the chance of complications of T2D can be reduced and quality of life improved.10 Self‐management is central to diabetes, as it is for many long‐term conditions,11 and has been defined as the behaviours that the patient employs in implementing the treatment regimen within their lifestyle routine.12 Diabetes self‐management requires the patient to make multiple decisions each day regarding diet, activity, glucose monitoring and medicine adherence to prevent hypo‐ and hyper‐glycaemia.13 Decisions and actions are based on their knowledge, beliefs, attitudes, resources and support systems.14
The patient empowerment approach to self‐management education interventions was first proposed in the 1990s.15 It aims to support patients in identifying and achieving their own goals; indeed empowering patients to self‐manage has been seen as the cornerstone of T2D management.16 This suggests that there is merit in health‐care systems recognizing those groups most at risk, such as BME communities, and tailoring appropriate programmes to support self‐management.17 Western health systems including the UK18 have advocated patient‐centred care as a key component of health policies for over a decade.19 Appropriate patient‐centred treatment programmes can only be tailored when patients' views on self‐management are known and understood.
To our knowledge there are currently only two reviews that have explored culturally relevant issues relating to diabetes self‐management and they focused on only one or two BME groups, living in a single country.20, 21 In addition, reviews have evaluated diabetes self‐management interventions delivered to BME groups.22, 23, 24, 25, 26 To our knowledge there are no existing systematic reviews that have synthesized research across countries for BME patients' views on multiple T2D self‐management behaviours. This review aimed to answer the question, ‘What are BME patients' views relating to self‐management of T2D?’
Methods
Design
A systematic review and interpretative data synthesis of primary empirical studies reporting patients' views.
This review is one of a linked pair of systematic reviews undertaken in line with the Evidence for Policy and Practice Information (EPPI) Centre's innovative ‘mixed‐methods framework’27 in which data from intervention studies (usually trials) are reported alongside data from ‘views studies’.28 The interventions review is currently under review. The EPPI centre's framework enables multiple research questions to be answered because many research designs can be included and multiple syntheses can be undertaken.
The EPPI approach was well suited to this systematic review because it provides clear guidance on synthesizing evidence from ‘views’ studies that place people's own voices at the centre of analysis. ‘Views’ studies are usually but not always qualitative. For the purposes of this review ‘views’ studies were identified as studies of any design that presented views as data, considering these insights as valuable in themselves, as opposed to presenting these as a strategy for generating variables that would go on to be tested in a model.29
As with traditional systematic review methods, the EPPI process incorporates transparent steps to reduce the impact of bias and error that may be present in primary studies as well as in the process of reviewing. These procedural points are detailed in the remainder of the methods section.
Search strategy
A single literature search was undertaken for the two linked reviews. When screening the titles and abstracts of retrieved papers, papers were categorized as being potentially relevant for inclusion in either the ‘views’ or ‘interventions’ reviews.
The first step was to identify synonyms for the review's three key components (BME groups, T2D, self‐management), using British and North American terms and spellings. The search used both ‘controlled vocabulary’ (standardized indexed search terms) and ‘free‐text terms’. In total the search included 159 terms in OVID databases. These search terms have been made available as supporting information for the online edition.
Eight bibliographical databases (MEDLINE, CINAHL, EMBASE, HMIC, AMED, PsycINFO, CSA, Web of Science) and one specialist register (Cochrane Library) were searched to April 2008. Some of the smaller databases did not employ controlled vocabulary, and even in databases that did, these were not standardized. Consequently, a search strategy was initially devised in MEDLINE and then adapted to other databases. Free‐text terms were used consistently throughout.
To test search sensitivity, two key journals (Diabetes Care and Ethnicity and Health) were hand searched from 2000 to 2008. This process did not produce any studies not already identified.
Inclusion and exclusion criteria
The entry criteria were adapted from previously defined study selection criteria:30 populations, interventions, outcomes and study designs. As this review aimed to explore patients' perspectives and not the effects of intervention studies, ‘Interventions’ was replaced with ‘Health issue.’
Population
Adults with a diagnosis of T2D.
Study samples of whom at least 50% were BME or when studies reported separate findings for BME subsamples.
BME was defined as ‘individuals with a cultural heritage distinct from the majority population’.31
Health issue
Patients' perspectives on T2D self‐management.
Study design
Any.
Outcomes
Any outcome related to T2D self‐management.
Exclusion criteria
Studies not published in English.
Studies of indigenous ethnic groups.
Given the focus of the review, the historical and policy contexts were considered to be influential, so we applied a publication start date of 1986, the date of Lorig's influential paper on self‐management in long‐term conditions.32
Procedure and materials
A screening tool was developed to review the search results. Initially screening was based on title and abstract, conducted by one author (RM) with a second author (CJ or PK) checking the decisions on a 10% sample for reliability. When the inclusion criteria appeared to have been met, the full paper was obtained and read for potential inclusion by RM.
Data extraction and quality assessment
The next step involved selecting a tool which enabled consistent and accurate data extraction and quality assessment of the included research papers thereby minimizing bias in the interpretation of findings.33 A key consideration when selecting a critical appraisal tool was that it accommodated both of the linked pair of systematic reviews, one of which focused on data from intervention studies (usually trials) while the other, reported here, focused primarily on qualitative data from ‘views studies’.
There is no one ‘gold standard’ critical appraisal tool. A systematic review on the content of critical appraisal tools was consulted.34 Katrak et al. retrieved 121 tools, 16 of which enabled an assessment of studies of both a quantitative and qualitative design and these tools were reviewed for our purpose. The template developed by Long and Godfrey35 was selected which served both data extraction and quality assessment.
Long and Godfrey's template was slightly adapted for the purposes of this systematic review. The EPPI Centre's review guidelines for data extraction and quality assessment of intervention studies36 were also adopted. This amalgamation of the two existing checklists plus the review questions specific to this study formed the basis of the critical appraisal tool developed here. This has been made available as supporting information for the online edition.
Data were extracted by one author (RM) and then checked by a second author (PK or CJ).
Evidence synthesis
It was anticipated that the ‘views’ data would be highly heterogeneous. In order to organize a large and potentially varied data set, key findings from the primary studies were organized according to the following three questions:
What is the meaning of ‘self‐management’ to BME patients with T2D?
What helps and what prevents their self‐management?
What ideas do BME patients themselves identify for what could promote self‐management?
The findings of the studies were integrated using thematic synthesis and in so doing, key themes were identified to answer the overall review question ‘What are BME patients' views relating to self‐management of T2D?’ The process of thematic synthesis followed four sequential stages:37
Line‐by‐line coding of the key findings of the primary studies was undertaken by RM, and this produced a bank of codes.
The data set was organized by RM, according to the three review questions (above). This facilitated the development of ‘descriptive themes’, which remained proximate to the findings of the primary studies.
Generation of interpretative ‘analytical themes’ enabled additional understanding of the concept by ‘going beyond’ the primary studies and producing more abstract constructs.38 To obtain analytical themes, all the study authors considered the descriptive themes in the context of how they answered the review question. Barriers and facilitators to self‐management were obtained from patients' views, and the implications of the findings for supporting the development of T2D self‐management interventions were considered. Through this process, more conceptual themes emerged that reflected patients' perspectives on their T2D self‐management.
The relationship between the analytical themes was also carefully considered by all of the study authors until an emergent over‐arching theme was identified, which addressed the systematic review question.
Results
Description of studies
The search identified 15 725 articles (see Fig. 1), of which 84 met the inclusion criteria after screening by title and abstract and were retrieved and read in full. Final screening resulted in 57 included studies,35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95 involving a total of 1723 patients.
Figure 1.
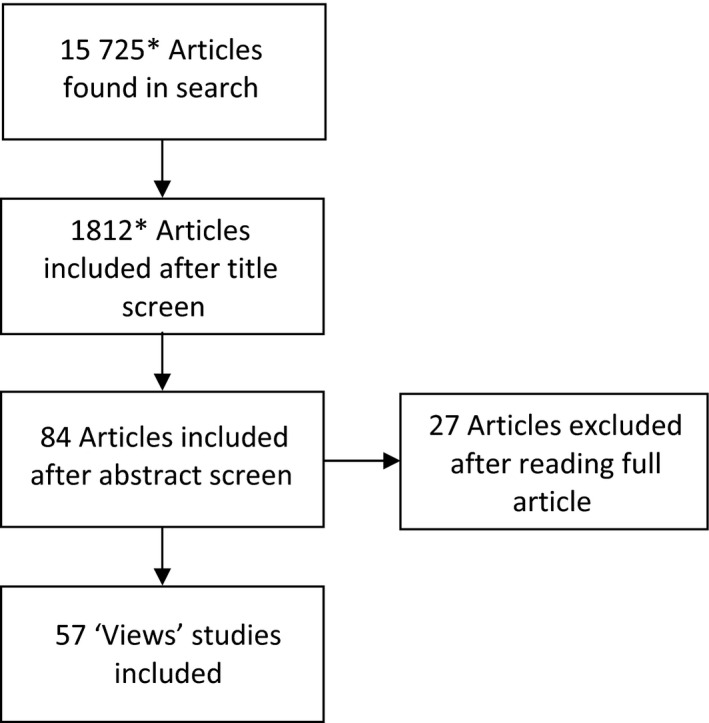
A flow chart of study selection. *These numbers relate to a broad search strategy that was used to identify studies for this ‘views’ review and the linked ‘interventions’ review.
One study had used a quantitative design,60 two were of a mixed‐method design83, 88 and the remaining 54 were qualitative studies. Thirty‐eight studies were undertaken in the US36, 37, 38, 39, 40, 43, 44, 46, 47, 48, 49, 51, 52, 55, 56, 58, 59, 61, 62, 63, 64, 65, 66, 68, 74, 76, 77, 78, 79, 81, 82, 83, 85, 89, 90, 92 and a further three in Canada.60, 80, 84 Fourteen studies were from Northern Europe (11 in the UK41, 42, 50, 57, 71, 72, 73, 75, 86, 87, 88 and three in Scandinavia53, 54, 91). The remaining two studies were from Australia.69, 70 Because the literature was dominated by North American research, it is unsurprising that most of the BME groups were of African39, 42, 44, 51, 52, 59, 74, 77, 78, 79, 83, 86, 88, 89, 92 or Latino origin.36, 37, 38, 40, 45, 47, 58, 62, 63, 64, 65, 66, 68, 82, 90 The next largest numbers of studies included South Asian41, 50, 53, 54, 57, 71, 72, 73, 75, 84, 87 and East Asian48, 49, 60, 67, 76 populations. One study included Italian immigrants;83 the remaining five studies included patients from more than one BME group.55, 61, 69, 70, 85 Nine of the 57 studies included only women,36, 37, 43, 44, 46, 50, 69, 70, 83 while one study included only men.74
The studies addressed a broad and diverse set of issues relating to T2D self‐management, including general lived experience;36, 43, 58, 67, 74, 75, 89, 91, 92 lifestyle;50, 52, 54, 55, 73, 81, 83, 86 beliefs about diabetes;42, 45, 48, 56, 57, 64, 69, 76 perceptions of health professionals';41, 53, 69, 70, 79 general self‐management;39, 44, 62, 65, 90 diabetes education;38, 40, 82, 84 alternative treatments;66, 77, 85 explanatory models of T2D;37, 49, 68 insulin therapy;60, 63 family roles;46, 80 depressed mood;47, 80 culture;56, 88 health‐care goals;64 health service use;75 medicines;74 symptoms;81 social support;72 fatalism;54 problem‐solving;62 and empowerment.90 Three studies56, 69, 80 investigated more than one of these issues.
Quality assessment
Methodological quality was assessed according to accepted standards by appraising individual components of each study's: design; procedure; conduct; and analysis. Table 1 summarizes the application of the quality assessment criteria to each study; 26 criteria apply to qualitative (and mixed‐method) studies, while only 24 criteria apply to the quantitative studies. Seven studies38, 50, 58, 64, 69, 75, 86 scored poorly, meeting less than half the criteria. Four of these studies38, 50, 64, 86 were published over ten years ago, when research quality criteria were less standardized. Since the findings of the seven lower‐quality studies did not differ from the higher‐quality majority, all studies were retained in the review.
Table 1.
Number of studies scoring a ‘yes’ on quality assessment criteria by study design
| All (N) | % | Qualitative (n = 54) | Mixed (n = 2) | Quantitative (n = 1) | |
|---|---|---|---|---|---|
| Clear aims | 57 | 100 | 54 | 2 | 1 |
| Clear articulation of rationale | 57 | 100 | 54 | 2 | 1 |
| Clear description of setting | 54 | 95 | 51 | 2 | 1 |
| Explicit theoretical framework | 16 | 28 | 16 | 0 | 0 |
| Clear description of self‐management behaviour | 48 | 84 | 46 | 1 | 1 |
| Stated measure of self‐management | 8 | 14 | 5 | 2 | 1 |
| Clear description of recruitment procedure | 49 | 86 | 46 | 2 | 1 |
| Clear description of sampling procedure | 56 | 98 | 53 | 2 | 1 |
| States inclusion and exclusion criteria | 50 | 88 | 47 | 2 | 1 |
| State participation rates | 16 | 28 | 16 | 0 | 0 |
| Target sample achieved | 14 | 25 | 14 | 0 | 0 |
| Clear description of sample | 51 | 89 | 48 | 2 | 1 |
| Appropriate sampling | 48 | 84 | 45 | 2 | 1 |
| Provision of recruitment data | 22 | 39 | 19 | 2 | 1 |
| Provision of attrition data | 15 | 26 | 13 | 1 | 1 |
| Clear description of data collection | 57 | 100 | 54 | 2 | 1 |
| Information collected with sufficient detail and depth | 50/56 | 89 | 49 | 1 | ‐ |
| Clear description of data analysis | 37 | 65 | 35 | 2 | 1 |
| Reliability and validity of data analysis methods reported | 42 | 74 | 40 | 1 | 1 |
| Evidence of reflexivity | 7/56 | 13 | 55 | 1 | ‐ |
| Explicit mention of health literacy | 2 | 4 | 2 | 0 | 0 |
| Interprets findings in context of other studies/theory | 51 | 89 | 48 | 2 | 1 |
| Evidence of consumer involvement | 13 | 23 | 10 | 2 | 1 |
| State implications | 51 | 89 | 48 | 2 | 1 |
| Strengths and limitations stated | 45 | 79 | 42 | 2 | 1 |
| Conclusion justified | 55 | 96 | 52 | 2 | 1 |
| Total (of possible 1486) | 1021 | 962 | 39 | 20 | |
| % of maximum possible score | 69 | 68 | 75 | 83 |
Self‐management views
The synthesis identified three analytical themes, 10 descriptive themes with nine subthemes, and an over‐arching theme (see Fig. 2); these will now be discussed in turn. Differences that emerged across gender or ethnicity are identified in the findings.
Figure 2.
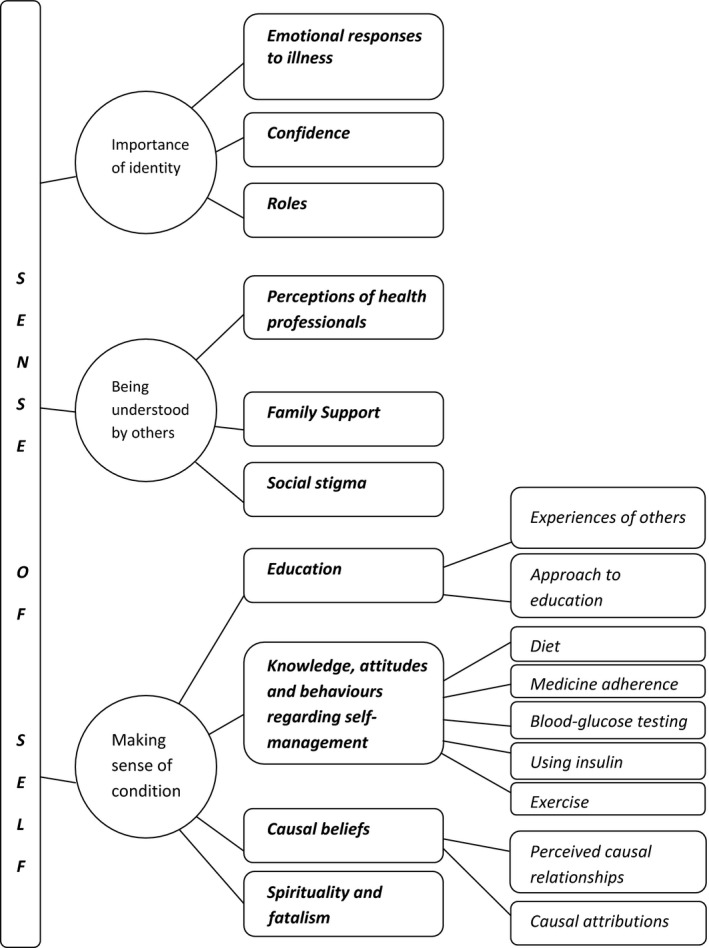
Identified descriptive and analytical themes.
Analytical Theme 1: Importance of identity
Self‐management was largely influenced by how the patients identified themselves. A patient's identity was evidenced in their: emotional outlook, particularly in response to the diagnosis and living with T2D; confidence levels; and roles.
Descriptive Theme 1a: Emotional responses to illness
Patients recalled their emotional responses to their diagnosis of diabetes as overwhelmingly negative including: depression;43, 45, 58, 59, 90 denial;38, 42, 43, 51, 56, 59, 70, 74 anxiety;69, 72, 83, 87 resignation;37, 45, 51, 73, 74, 81, 87, 89 and pessimism.36, 37, 43, 49, 51, 59, 72, 73, 91 Patients described how diabetes was an ‘assault’ on their identity.
Emotional responses to self‐management were also mentioned. Patients reported frustration59, 73, 77, 90 and anger43, 59, 74, 90 with the complexity of self‐management. Fear of diabetes and its complications43, 44, 58, 67, 68, 72, 74, 81, 87, 91 added to the difficulties associated with initiating and maintaining good self‐management.
A commonly adopted strategy to facilitate self‐management was improving emotional well‐being. Some people actively sought opportunities to be involved in activities that made them happier and healthier.49, 63, 66, 67, 85, 89, 92 Others either accepted39, 44, 59, 65, 74 or avoided focusing on44, 51, 57, 63, 69, 91 their diabetes so as to improve their emotional well‐being. By accepting their diabetes, patients were better able to receive support from others49, 69, 81, 82, 84, 89 as well as help themselves self‐manage.43, 44, 59, 65, 81, 82, 89, 91
Descriptive Theme 1b: Confidence
Those who accepted their diabetes, demonstrated an empowered perspective to self‐management and were able to embrace their new, evolving identity. They emphasized the personal experience of living with diabetes, maintaining that knowledge of their own bodies could not be surpassed in managing the condition.36, 37, 39, 40, 42, 44, 49, 59, 64, 70, 74, 91
For those who experienced a disoriented identity or rejected their new identity, developing diabetes resulted in a loss of confidence in their ability to implement behavioural changes required for self‐management.36, 37, 40, 45, 51, 69, 77 Furthermore, some expressed the view that diabetes was a ‘betrayal’ by their own body.36, 70, 78, 92
Descriptive Theme 1c: Roles
Gender roles were commonly discussed.36, 38, 41, 44, 45, 46, 47, 52, 55, 56, 63, 69, 73, 74, 75, 76, 77, 80, 83, 84, 87, 91, 92 Men focused on how diabetes affected them physically,47, 63, 73, 74, 77, 91, 92 while women expressed general concerns about having poorer health.36, 47, 91, 92 Gender was influential with respect to perceived support, with men tending to report significant family support41, 47, 56, 63, 74, 92 and women tending to feel unsupported.47, 56, 73, 83, 91
Cultural norms were more evident in women's discourses.73, 76, 84, 87 For many women, the role of caregiver affected self‐management.36, 38, 41, 44, 45, 46, 52, 63, 69, 73, 75, 77, 80, 83, 84 For some, their family, social and work roles facilitated self‐management because they believed it was important to maintain health, so as to retain identity, independence and a sense of normality. For some women, such caregiver roles were a barrier, requiring time and energy that made it physically and emotionally difficult for them to self‐manage their T2D.
Health goals were commonly described in functional rather than biomedical terms, that is, being able to continue with aspects of their daily routine.61, 63, 65, 78, 91 Similarly, symptoms were defined in terms of impact on social, familial and working roles.44, 52, 58, 65, 67, 73, 74, 78 Diabetes served to motivate some people to maintain their pre‐diagnosis roles in order to preserve their identity within their social, religious and familial groups.36, 39, 43, 46, 50, 91 By the same token, patients reported unease with being dependent on others.44, 49, 56, 71, 72, 74, 78, 81, 91
Analytical Theme 2: Being understood by others
Patients' views emphasized a need for their condition to be understood by others in their family and local community. Patients also actively sought health professionals who understood their cultural background.
Descriptive Theme 2a: Perceptions of health professionals
Patients frequently reported seeking guidance from health professionals.36, 39, 41, 43, 44, 45, 47, 53, 59, 70, 79, 92 There was respect for the physician's professional status,69, 84, 87 which, for some, meant they never criticized health professionals.41, 53, 92 Others even withheld information about their own ‘poor’ self‐management practices.41, 69, 70, 76, 81, 92
Patients were mindful of the health professional's lack of time.53, 57, 84 Some patients were critical of the quality and amount of information they received,69, 70 while others accepted that health professionals were busy.43, 89, 90 Patients showed high regard for health professionals who offered patient‐centred care36, 39, 42, 92 and communicated in a meaningful way.36, 53, 79, 82
Failing to consistently follow health professionals' recommendations because of the challenges of managing daily life within a complex regimen41, 78, 89, 90, 92 and the constraints imposed by comorbidities was not uncommon.39, 41, 47, 54, 58, 73, 87, 89 Professional advice was also not always followed when patients disagreed with the recommendations36, 39, 54, 60, 69, 70, 90 or viewed health professionals as untrustworthy.40, 42, 51, 53, 69, 77
Patients' perceptions of their health professional were shaped by the cultural and linguistic appropriateness of the health‐care exchange; in circumstances when the consultation was perceived to be inappropriate patients referred to health professionals' inability to relate to them.39, 43, 53, 54, 77, 81, 84, 92 For example, patients were critical of health professionals' dietary recommendations that were perceived as expecting the patient to reject culturally traditional foods.42, 53, 54, 81, 91
The linguistic inappropriateness of the exchange with the health professional was mentioned by patients who understood none or little of the host country language.47, 87 Those who spoke positively of consultations tended to share a common language and culture with their health professional as this made communication easier, more direct and culturally sensitive.36, 50, 72, 76, 81, 84 The inadequacy of working through interpreters as compared with direct communication with bilingual staff also emerged.53, 54, 56, 60, 72, 84
Descriptive Theme 2b: Family support
This was a commonly reported descriptive theme to emerge. Interestingly, all statements of family support being ‘valued’ came from North American studies of African‐Americans or Latinos.38, 44, 46, 68, 77, 83, 89, 90, 92 Only two studies reported patients resisting family support by concealing their condition, motivated in part to protect family members from worry.48, 69 It was noted that disclosure of the condition elicited emotional68, 69, 87, 90 and practical support from the family, particularly with diet.43, 46, 50, 52, 55, 68, 89
Some patients reported that families lacked understanding of the need for dietary modifications.36, 53, 75, 87, 90, 91 Many patients reported that feeling supported by their family depended on the family understanding their condition.38, 39, 40, 44, 45, 47, 90
Although identified less frequently, some views suggested a lack of familial support, which was largely due to poor understanding of the condition.38, 44, 82, 91 There was a perceived lack of empathy from some families who did not change their expectations of the individual's home responsibilities after diagnosis of diabetes.83, 84
Descriptive Theme 2c: Social stigma
Several studies identified social stigma as a concern,36, 44, 60, 67, 73, 84, 89 which at times prevented patients from disclosing their diagnosis, leading to an impaired ability to self‐manage. Elsewhere, however, patients talked about diabetes as a common condition and as such they felt comfortable telling people they had it68, 74 with information sharing occurring naturally.
Analytical Theme 3: Making sense of own condition
Despite showing a high regard for education, the majority of views demonstrated a lack of knowledge about, and negative attitudes towards, making lifestyle changes to manage their diabetes. Patients evidenced inaccurate health beliefs, either as a result of misunderstanding the underlying causes and consequences of diabetes or by over‐emphasizing cultural health beliefs. Traditional beliefs regarding spirituality and fatalism further impacted on patients' understanding of diabetes.
Descriptive Theme 3a: Education
Two subthemes emerged within this descriptive theme.
Experiences of others
The experiences of others, including family members, with diabetes were seen as a valued, informal source of education and information.36, 37, 39, 42, 43, 49, 55, 59, 67, 77, 82, 87, 89 The experiences of others also influenced patients' health‐care goals. However, social comparison had negative consequences for some because it led them to believe that poor outcomes of diabetes were inevitable.36, 37, 45, 51, 58, 59, 73, 74, 81, 87, 89 For some, however, exposure to others' poor health facilitated acceptance of their diagnosis73 and a realization of possible outcomes; as such, it was a motivator to self‐manage well.39, 42, 47, 59 Several studies reported the value attached to having good role models because they inspired hope for a normal life and provided the opportunity for interaction with someone who was successful at self‐management and understood the challenges of the condition.39, 81, 90
Approach to education
Some patients sought a non‐didactic approach to education,43, 61, 66, 70, 77, 82, 88, 89, 90 and this tended to be reported in American studies. Meanwhile, other patients sought a more didactic approach to education36, 39, 41, 51, 53, 57, 61, 67, 70, 72, 75, 82, 84, 87, 90, 92 where formal learning techniques were employed, and these tended to be in studies with South Asian samples.
Patients talked favourably of education classes.43, 45, 68, 81, 89 Group education was positively received due to its supportive55, 69, 73, 81, 87, 89 and motivational85 atmosphere. Some sought the inclusion of family members, partly for their support but also so they too could learn how to manage diabetes.38, 53, 81, 82, 90
Patients sought practical education centred on diet,43, 52, 55, 80, 81, 82, 88, 89, 90 and culturally appropriate education focused on physical activity.55, 72, 73, 90 The use of health‐care jargon was identified as an educational barrier54, 57, 70 as were patients' own literacy limitations.49, 82, 88, 90, 91
Descriptive Theme 3b: Knowledge, attitudes and behaviours regarding self‐management
Studies reported a broad range of knowledge, attitudes and behaviours regarding diabetes self‐management. More studies reported negative attitudes and behaviours and a lack of knowledge than did those identifying good knowledge, and positive attitudes and behaviours about diabetes. Patients' knowledge and attitudes towards specific self‐management behaviours are now presented in the five following subthemes; ordered according to frequency of occurrence in the primary studies, with the most common presented first.
Diet
Patients spoke of the importance of diet for self‐management.49, 55, 68, 81, 83, 90, 91 However, there was considerable evidence of limited knowledge about what constituted a healthy diet for a person with diabetes.36, 52, 54, 68, 78, 81, 82, 84, 90, 91 Unsurprisingly, a lack of education was a barrier to achieving and maintaining a healthy diet.36, 74, 78, 80, 87, 91
Identified cultural barriers included a craving for traditional foods recognized as problematic for those with diabetes.36, 43, 67, 81, 89, 91 Perceptions of healthy food practices were culturally influenced38, 47, 49, 56, 57, 63, 67, 68, 71, 77, 87, 90 leading some to integrate professional dietary advice into their own cultural perception of a healthy diet.56, 68
There were negative perceptions of the diet recommended to them, including its taste38, 41, 52, 63, 81, 91 and expense.43, 52, 63, 81 Patients reported concerns about protecting the eating experience of the family,36, 41, 42, 48, 52, 56, 63 at times subordinating their own dietary needs for the sake of the family.36, 41, 44, 49, 54, 63, 75, 81 Some patients reported difficulty in adhering to an appropriate diet during special family occasions.43, 52, 57, 59, 67, 75, 87, 88
Medicine adherence
The importance of taking medication as prescribed was recognized.49, 61, 63, 68, 71, 78, 87, 89, 91 However, there was inconsistent motivation to take medicines,40, 44, 64, 69 and some would reduce their medicine intake when they felt well.49, 71, 74, 76
Traditional cultural beliefs about medicine featured strongly. Some BME samples distrusted Western medicines42, 49 due to side‐effects60, 71, 76, 81, 84; long‐term health implications71, 76, 89 and its relative recency when compared with traditional therapies such as Chinese medicine.63 Traditional remedies were referred to frequently by patients across different BME groups37, 38, 42, 49, 60, 66, 67, 68, 69, 71, 76, 77, 81, 84, 85, 88, 89, 90 and were used to varying degrees.
Blood glucose testing
Some patients reported that testing their blood glucose daily helped them evaluate the success of self‐management49, 57, 67, 78 and that they knew what to do when blood glucose was too high or low91 although they did not always have the time or energy to respond.44, 57, 65 The relationship between blood glucose and long‐term health outcomes was not always recognized.82, 84, 90
Hypoglycaemia was clearly and fearfully described.43, 49, 63, 68, 74 It may be to avoid this outcome that some patients reported maintaining a higher than recommended level of blood glucose.41, 49, 74, 81 In contrast, descriptions of hyperglycaemia were rare and unclear.68, 84
Using insulin
Negative perceptions of using insulin were evident, especially among East Asian participants.49, 60, 67, 76 There was also a stigma concerning insulin use, with people believing that regular use led to addiction,71 dependency44, 60 or a need for higher doses.79 The most frequent barrier to insulin use was the dislike of injections.44, 60, 68, 73, 76, 83
There was also considerable apprehension around insulin use in terms of illness progression. A need for insulin was understood to signify severity of the condition42, 44, 60, 67, 75, 76 and was thought to be related to more severe complications.44, 68, 76, 81
There were two main sets of views favouring insulin. First, that it helped control symptoms, avoid complications and prolonged quality of life;47 and second, that it was faster acting than oral medicines.73
Exercise
The importance of exercise was less frequently identified in comparison with other self‐management behaviours. Socio‐economic factors were identified as barriers, including prohibitive health club costs,38, 90 fear of walking in high crime neighbourhoods49, 50, 63, 81 and the difficulty of incorporating activities into busy lives with long working hours.38, 49, 73 Cultural barriers included a lack of culturally relevant information81, 90 or culturally sensitive facilities73, 88 for physical activity. Physical barriers also included the cold climate of the host country,38, 49, 74, 80, 91 comorbidities and pain.38, 49, 63, 73, 80, 81
Descriptive Theme 3c: Causal beliefs
There were two sub‐themes within this descriptive theme.
Perceived causal relationships
Many views identified causal relationships between symptoms and complications that were incorrect according to a biomedical framework.
Symptoms of high blood glucose were correctly identified by patients in five studies, in which it was suggested that symptoms could be interpreted and used to adjust lifestyle68, 78 with the aim of avoiding deterioration of the condition.49, 63, 67, 78 Other patients, however, considered the symptoms of poor self‐management to be inevitable37, 58, 77, 83 and so delayed seeking medical help.39, 77, 89
The causal relationships between prolonged periods of high blood glucose and complications of the condition were correctly identified by patients in two studies only45, 49 with a further two identifying a goal to prevent complications through good self‐management.59, 61 Complications were not always understood well.81, 84 As with symptoms, some patients believed that complications were inevitable.36, 37, 49, 59, 67, 72
Causal attributions
Some patients ascribed their T2D to a range of lifestyle factors including diet42, 58, 64, 67, 74, exercise and weight gain.67, 68 Others considered the cause of diabetes to be genetic.36, 37, 51, 58, 64, 67, 68, 73, 74, 87
Interestingly, Latino samples tended to attribute diabetes onset to an emotional life event such as a family bereavment.36, 47, 56, 58, 64, 68, 75, 82 Anger,58, 68 general sadness and stress were also identified as causes.42, 45, 49, 67, 76 Some patients made a link with the distress of the migration experience42, 47 or the move to a new environment.42, 49, 50, 56, 67, 73, 75
Other causal beliefs included eating too many sweets37, 75, 77 and taking medicines prescribed for other conditions.74 Spiritual factors51, 73, 87 were also cited. Participants in two studies stated that they did not know the cause.58, 67
Descriptive Theme 3d: Spirituality and fatalism
Spirituality and fatalism were seen to both support and hinder coping. Spiritual beliefs had an important role in providing emotional support.42, 43, 45, 69, 83, 87 Prayer was considered to reduce stress.66, 83, 85, 89 Spiritual beliefs could hinder coping as well as help. For example, there were cases of religiosity where patients did not show sickness, undertake self‐management or accept treatment.44, 51 There were also examples of religious considerations prevailing over dietary ones.50, 91
Others expressed views that while their faith had direct influence on the outcome of their condition it did not absolve them from taking responsibility for self‐management.42, 50, 66, 83, 84 In this way, positive fatalistic attitudes helped them accept their condition, and this was associated with improvements in mental health.52 Negative fatalistic attitudes included patients believing that their actions would not change their future.36, 37, 43, 49, 51, 59, 72, 73, 91
Over‐arching Theme: ‘Sense of self’
The three analytical themes (‘importance of identity’, ‘being understood by others’, ‘making sense of own condition’) were closely inter‐related. An individual's perception of their condition was in part influenced by their self‐identity before and after diagnosis. Furthermore, it was important to patients that others understood their (perception of their) condition. As such the over‐arching theme was identified as ‘sense of self’, reflecting the belief that inherent to successful self‐management is the interplay between personal resources and the environment.
Discussion
The systematic review aimed to further understanding of BME views on the barriers and facilitators influencing self‐management of type 2 diabetes. Data were included from 57 primary studies across a variety of self‐management behaviours, populations and settings. While it is accepted that this is a large data set, the method of thematic synthesis was employed rigorously at each of its five stages. This ensured that depth in the analysis was not compromised. The review identified three analytical themes (‘importance of identity’, ‘being understood by others’, ‘making sense of own condition’) and an over‐arching theme ‘sense of self’.
As discussed earlier, other reviews have explored culturally relevant issues relating to diabetes self‐management, but they only focused on one or two BME groups living in a single country.20, 21 To our knowledge, this is the first systematic review to synthesize views about type 2 diabetes self‐management across a variety of BME populations in a variety of settings. Moreover, this is the first review on this topic to have synthesized studies, using qualitative research traditions.
Due to the large amount of published primary research, this secondary data analysis was timely. The synthesis drew together data from BME populations in similar Western settings to examine commonalities and differences. This allowed theoretical generalization, which had not been possible from the individual qualitative studies.
In interpreting the findings of the review, it is necessary to recognize four potential limitations. First, the research was included from several countries, and the contextual variation might influence the validity of a synthesis. For example, the issue of language difficulties as a barrier to self‐management is very different for first‐generation immigrants than for sixth‐ or seventh‐generation African‐Americans in the USA. It would be useful to know whether English‐speaking and non‐English‐speaking BME patients experience the same or different barriers. A future review could address this question.
A second potential source of bias was the exclusion of studies of indigenous populations. The rationale was that while indigenous groups may belong to minority ethnic groups, they are not immigrants. It was thought that indigenous and immigrant BME groups are likely to experience different barriers and facilitators to diabetes self‐management. This issue warrants an evidence base and is one that a future review might address.
Thirdly, it is possible that the broad literature search (of 240 terms, resulting in 15 275 retrieved titles) lacked specificity. This increased the chance of missing a relevant article during the selection process. The trade‐off between sensitivity and specificity in searching for qualitative research has been debated,93, 94 and the conclusion appears to be that there is no fail‐safe method.
Finally, the review was limited to studies published from 1986 to 2008, hence relevant studies published outside these dates have been excluded. Nevertheless, we consider that this comprehensive review offers new evidence.
The BME patients' views about diabetes self‐management were captured within three analytical themes. First, how patients identified themselves was of great importance to successful self‐management. Second, being understood by others facilitated self‐management; patients wanted family members to understand their condition and health professionals to understand their culture. Third, patients' own limited understanding of diabetes was a barrier to self‐management. These three analytical themes highlighted the complex nature of self‐management.
These findings were consistent with previous research. Wilson et al.21 synthesized quantitative and qualitative evidence relating to self‐management and access to health services for South Asian and Black African‐Caribbean people with diabetes in the UK. They also found barriers at the patient, provider and service levels. Patients lacked knowledge of self‐management, which was attributed to language and communication difficulties and a lack of culturally sensitive services.
A key issue in this review not identified in the study by Wilson et al.21 was how living with the condition influenced identity and ‘sense of self’. That said, the importance of this theme does resonate with wider views on long‐term conditions. For example, long‐term conditions have been conceptualized in terms of biographical disruption.98 This poses the interesting question to what extent the findings of this review are specific to T2D (or to an immigrant, socially and educationally disadvantaged population with T2D) and how much they are generally true of patients living with any long‐term condition? The resonance of the over‐arching theme ‘sense of self’ suggests that how patients learn to manage a long‐term condition is not necessarily consistent with traditional Western assumptions of how this may be achieved, for example, through formal education classes. Rather the findings suggest that learning is acquired through living with diabetes and experiencing and overcoming situations. This supports the notion of patient‐centred experiential learning and the provision of interactive health education interventions.
Two previous systematic reviews synthesized accounts of the experience of diabetes in predominantly non‐BME patients, using the meta‐ethnographic method.96, 97 A key finding from both reviews was that effective self‐management was learnt through experience and experimentation with behaviours over time. As you would expect there is some overlap between these findings and those reported in this systematic review. However, there are also interesting and important differences. For example, previous reviews reported that a majority of patients preferred to take a dynamic position that allowed them to control their own condition and which was not reliant on health professionals. In contrast, many patients in this review sought didactic health education. This systematic review was also novel in its finding of the importance that patients place on maintaining culturally normative social, familial or work roles. An interesting similarity between this review and those of Paterson et al.100 and Campbell et al.99 is the need identified by all patients for receiving support and understanding from others, particularly family and health professionals. However, the emphasis on family was far greater in the studies included in this review.
The high prevalence of T2D in patients' communities came across in the theme ‘making sense of own condition’ where patients talked about learning through information sharing with friends and family. However, the dependence on family and friends for information was noted by patients as risky because of its limits and potential for being incorrect.101 However, there may be advantages to collecting information from various sources and choosing between them, in engendering patient independence.102 A potential implication for health‐care interventions would be to harness naturally occurring peer support groups among high prevalence populations, encouraging upward social comparisons.103 Social comparison principles refer to how individuals compare themselves with others to evaluate their feelings and abilities, particularly when they are distressed.104 Such upward comparisons can initiate self‐improvement behaviours, while downward comparisons may be used to enhance self‐esteem.103
An intervention that utilizes existing social support networks would have the same potential advantages as those noted in peer support groups in general: providing condition‐specific information105 and opportunities for social comparison and emotional support;100, 101 reducing subjective uncertainty103 and being sympathetic to the individual's cultural and social needs.104 Additional advantages would be practical in enabling patients who know each other to overcome the barriers of transport and language limitations. Moreover, even after the intervention had ended, individuals would continue to support one another.
The review findings suggest that the identified themes were not addressed sufficiently in the development of health‐care policy and the delivery of health services. Identifying patients' views from the primary empirical studies has been valuable, not only for understanding the uptake of available interventions, but also for the potential to inform the development of interventions that have more appropriate and acceptable content and delivery to minority groups.
Supporting information
Data S1 Critical appraisal form (views).
Data S2 Type 2 diabetes & BME & self‐management.
Acknowledgements
The project was fully sponsored by a studentship from the University of Leeds, School of Healthcare.
References
- 1. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Research and Clinical Practice, 2009; 87: 4–14. [DOI] [PubMed] [Google Scholar]
- 2. Roglic G, Unwin N, Bennett PH et al The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care, 2005; 28: 2130–2135. [DOI] [PubMed] [Google Scholar]
- 3. Diabetes UK . ‘Postcode lottery’ for care in England revealed. http://www.diabetes.org.uk/About_us/News_Landing_Page/Postcode-lottery-for-care-in-England-revealed/ (Accessed 12 December 2010).
- 4. World Health Organisation Commission on the Social Determinants of Health . Achieving health equity: From root causes to fair outcomes http://www.who.int/social_determinants/resources/interim_statement/en/index.html. (Accessed 14 Febuary 2008).
- 5. Davies MJ, Heller S, Skinner TC et al Effectiveness of the diabetes education and self‐management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. British Medical Journal, 2010; 336: 491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Riste L, Khan F, Cruickshank K. High prevalence of Type 2 Diabetes in all ethnic groups, including Europeans in a British inner city: relative poverty, history, inactivity or 21st century Europe. Diabetes Care, 2001; 24: 1377–1383. [DOI] [PubMed] [Google Scholar]
- 7. Forouhi NG, Merrick D, Goyder E et al Diabetes prevalence in England, 2001—estimates from an epidemiological model. Diabetic Medicine, 2006; 23: 189–197. [DOI] [PubMed] [Google Scholar]
- 8. Imkampe AK, Gulliford MC. Increasing socio‐economic inequality in type 2 diabetes prevalence—Repeated cross‐sectional surveys in England 1994–2006. European Journal of Public Health, 2010; 20: 1–7. [DOI] [PubMed] [Google Scholar]
- 9. Abate N, Chandalia M. The impact of ethnicity on type 2 diabetes. Journal of Diabetes and Its Complications, 2003; 17: 39–58. [DOI] [PubMed] [Google Scholar]
- 10. Watkins PJ, Amiel SA, Howell SL, Turner E. Diabetes and its Management. London: Blackwell, 2003. [Google Scholar]
- 11. Kennedy A, Gask L, Rogers A. Training professionals to engage with and promote self‐management. Health Education Research, 2005; 20: 567–578. [DOI] [PubMed] [Google Scholar]
- 12. Lorig KR, Holman HR. Self‐management education: context, definition, and outcomes and mechanisms. Behavioural Science, 2000; 26: 1–17. [DOI] [PubMed] [Google Scholar]
- 13. Clement S. Diabetes self‐management education. Diabetes Care, 1995; 18: 1204–1214. [DOI] [PubMed] [Google Scholar]
- 14. Sakraida TJ, Robinson MV. Health literacy self‐management by patients with type 2 diabetes and stage 3 chronic kidney disease. Western Journal of Nursing Research, 2009; 31: 627–647. [DOI] [PubMed] [Google Scholar]
- 15. Funnell MM, Brown TL, Childs BP et al The national standards for diabetes self‐management education. Diabetes Care, 2008; 31: 97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Snoek FJ, Skinner TC. Psychology in Diabetes Care. Chichester, UK: Wiley, 2000. [Google Scholar]
- 17. Hawthorne K. Effect of culturally appropriate health education on glycaemic control and knowledge of diabetes in British Pakistani women with type 2 diabetes mellitus. Health Education Research, 2001; 16: 373–381. [DOI] [PubMed] [Google Scholar]
- 18. Department of Health . Equity and excellence: liberating the NHS. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_117353 (Accessed 4 April 2012).
- 19. McClimans LM, Dunn M, Slowther AM. Health policy, patient‐centred care and clinical ethics. Journal of Evaluation in Clinical Practice, 2011; 17: 913–919. [DOI] [PubMed] [Google Scholar]
- 20. Caban A, Walker EA. A systematic review of research on culturally relevant issues for Hispanics with diabetes. Diabetes Educator, 2006; 32: 584–595. [DOI] [PubMed] [Google Scholar]
- 21. Wilson C, Alam R, Latif S, Knighting K, Williamson S, Beaver K. Patient access to healthcare services and optimisation of self‐management for ethnic minority populations living with diabetes: a systematic review. Health and Social Care in the Community, 2012; 20: 1–19. [DOI] [PubMed] [Google Scholar]
- 22. Hawthorne K, Robles Y, Cannings‐John R, Edwards AGK. Culturally appropriate health education for Type 2 diabetes in ethnic minority groups: a systematic and narrative review of randomized controlled trials. Diabetic Medicine, 2010; 27: 613–623. [DOI] [PubMed] [Google Scholar]
- 23. Khunti K, Camosso‐Stefinovic J, Carey M, Davies MJ, Stone MA. Educational interventions for migrant South Asians with type 2 diabetes: a systematic review. Diabetic Medicine, 2008; 25: 985–992. [DOI] [PubMed] [Google Scholar]
- 24. Sarkisian CA, Brown AF, Norris KC, Wintz RL, Managione CM. A systematic review of diabetes self‐care interventions for older, African American or Latino adults. Diabetes Educator, 2003; 29: 467–479. [DOI] [PubMed] [Google Scholar]
- 25. Saxena S, Misra T, Car J, Netuveli G, Smith R, Majeed A. Systematic review of primary health care interventions to improve diabetes outcomes in minority ethnic groups. Journal of Ambulatory Care Management, 2007; 30: 218–230. [DOI] [PubMed] [Google Scholar]
- 26. Whittemore R. Culturally competent interventions for Hispanic adults with type 2 diabetes: A systematic review. Journal of Transcultural Nursing 2007; 18: 157–166. [DOI] [PubMed] [Google Scholar]
- 27. Harden A, Thomas J. Methodological issues in combining diverse study types in systematic reviews. International Journal of Social Research Methodology, 2005; 8: 257–271. [Google Scholar]
- 28. Oliver S, Harden A, Rees R et al An emerging framework for including different types of evidence in systematic reviews for public policy. Evaluation, 2005; 11: 428–446. [Google Scholar]
- 29. Thomas J, Sutcliffe K, Harden A et al Children and Healthy Eating: A Systematic Review of Barriers and Facilitators. London: EPPI‐Centre, Social Science Research Unit, Institute of Education, University of London, 2003. [Google Scholar]
- 30. Khan KS, Kunz R, Kleijnen J, Antes G. Systematic Reviews to Support Evidence‐Based Medicine: How to Review and Apply Findings of Healthcare Research. London: Royal Society of Medicine, 2003. [Google Scholar]
- 31. Manthorpe J, Hettiaratchy P. Ethnic minority elders in the UK. International Review of Psychiatry, 1993; 5: 171–178. [Google Scholar]
- 32. Lorig K, Feigenbaum P, Regan C, Ung E, Chastain RL, Holman HR. A comparison of lay‐taught and professional‐taught arthritis self management courses. Journal of Rheumatology, 1986; 13: 763–767. [PubMed] [Google Scholar]
- 33. Canberra. National Health and Medical Research Council: How to Use the Evidence: Assessment and Application of Scientific Evidence, 2000. Available at: http://www.nhmrc.gov.au _files_nhmrc/file/publications/synopses/cp69.pdf, accessed 10 February 2009.
- 34. Katrak P, Bialocerkowski AE, Massy‐Westropp N, Kumar S, Grimmer KA. A systematic review of the content of critical appraisal tools. BMC Medical Research Methodology, 2004; 16: 4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Long AF, Godfrey M. An evaluation tool to assess the quality of qualitative research studies. International Journal of Social Research Methodology Theory and Practice, 2004; 7: 181–196. [Google Scholar]
- 36. Peersman G, Oliver S, Oakley A. EPPI‐Centre Review Guidelines: Data Collections for the EPIC Database. London: EPPI‐Centre, Social Science Research Unit, Institute of Education, University of London, 1997. [Google Scholar]
- 37. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology, 2006; 3: 77–101. [Google Scholar]
- 38. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. Medical Research Methodology, 2008; 8: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Adams CR. Lessons learned from urban Latinas with type 2 diabetes mellitus. Journal of Transcultural Nursing, 2003; 14: 255–265. [DOI] [PubMed] [Google Scholar]
- 40. Aloozer F. Secondary analysis of perceptions and meanings of type 2 diabetes among Mexican American women. The Diabetes Educator, 2000; 26: 785–795. [DOI] [PubMed] [Google Scholar]
- 41. Anderson RM, Goddard CE, Garcia R, Guzman JR, Vazquez F. Using focus groups to identify diabetes care and education issues for Latinos with diabetes. The Diabetes Educator, 1998; 24: 618–625. [DOI] [PubMed] [Google Scholar]
- 42. Anderson‐Loftin W, Moneyham L. Long‐term disease management needs of southern African Americans with diabetes. The Diabetes Educator, 2000; 26: 821–832. [DOI] [PubMed] [Google Scholar]
- 43. Benavides‐Vaello S, Garcia AA, Brown SA, Winchell M. Using focus groups to plan and evaluate diabetes self‐management interventions for Mexican Americans. The Diabetes Educator, 2004; 30: 238–256. [DOI] [PubMed] [Google Scholar]
- 44. Bissell P, May CR, Noyce PR. From compliance to concordance: barriers to accomplishing a re‐framed model of health care interactions. Social Science and Medicine, 2004; 58: 851–862. [DOI] [PubMed] [Google Scholar]
- 45. Brown K, Avis M, Hubbard M. Health beliefs of African–Caribbean people with type 2 diabetes: a qualitative study. British Journal of General Practice, 2007; 57: 461–469. [PMC free article] [PubMed] [Google Scholar]
- 46. Burns D, Skelly AH. African American women with type 2 diabetes: meeting the daily challenges of self care. Journal of Multicultural Nursing & Health, 2005; 11: 6–10. [Google Scholar]
- 47. Cagle CS, Appel S, Skelly AH, Carter‐Edwards L. Mid‐life African‐American women with type 2 diabetes: influence on work and the multicaregiver role. Ethnicity and Disease, 2002; 12: 555–566. [PubMed] [Google Scholar]
- 48. Carbone ET, Rosal MC, Torres MI, Goins KV, Bermudez OI. Diabetes self‐management: perspectives of Latino patients and their health care providers. Patient Education and Counseling, 2007; 66: 202–210. [DOI] [PubMed] [Google Scholar]
- 49. Carter‐Edwards L, Skelly AH, Cagle CS, Appel SJ. “They care but don't understand”: family support of African American women with type 2 diabetes. The Diabetes Educator, 2004; 30: 493–501. [DOI] [PubMed] [Google Scholar]
- 50. Cherrington A, Ayala G, Sleath B, Corbie‐Smith G. Examining knowledge, attitudes, and beliefs about depression among Latino adults with type 2 diabetes. The Diabetes Educator, 2006; 32: 603–613. [DOI] [PubMed] [Google Scholar]
- 51. Chelsa CA, Chun KM. Accommodating type 2 diabetes in the Chinese American family. Qualitative Health Research, 2005; 15: 240–255. [DOI] [PubMed] [Google Scholar]
- 52. Culhane‐Pera KA, Her C, Her B. “We are out of balance here”: a Hmong cultural model of diabetes. Journal of Immigrant and Minority Health, 2007; 9: 179–190. [DOI] [PubMed] [Google Scholar]
- 53. Duthie‐Nurse G. An anthropological study into the views on diet and disease of a sample of Hindu Gujarati‐speaking women with type 2 diabetes. Practical Diabetes International, 1998; 15: 109–111. [Google Scholar]
- 54. Egede LE, Bonadonna RJ. Diabetes self‐management in African Americans: an exploration of the role of fatalism. The Diabetes Educator, 2003; 29: 105–115. [DOI] [PubMed] [Google Scholar]
- 55. El‐Kebbi IM, Bacha GA, Musey VC, Gallina DL, Dunbar V, Phillips LS. Diabetes in urban African Americans. V. Use of discussion groups to identify barriers to dietary therapy among low‐income individuals with non‐insulin‐dependent diabetes mellitus. Diabetes Educator, 1996; 22: 488–492. [DOI] [PubMed] [Google Scholar]
- 56. Fagerli RA, Lien ME, Wandel M. Health worker style and trustworthiness as perceived by Pakistani–born persons with type 2 diabetes in Oslo, Norway. Health, 2007; 11: 109–129. [DOI] [PubMed] [Google Scholar]
- 57. Fagerli RA, Lien ME, Wandel M. Experience of dietary advice among Pakistani‐born persons with type 2 diabetes in Oslo. Appetite, 2005; 45: 295–304. [DOI] [PubMed] [Google Scholar]
- 58. Feathers JT, Kieffer EC, Palmisano G et al The development, implementation, and process evaluation of the REACH Detroit Partnership's Diabetes Lifestyle Intervention. The Diabetes Educator, 2007; 33: 509–520. [DOI] [PubMed] [Google Scholar]
- 59. Hadwiger S. Acculturation and diabetes in a new Hispanic community. Hispanic Health Care International, 2005; 3: 133–142. [Google Scholar]
- 60. Hawthorne K, Tomlinson S. Pakistani moslems with type 2 diabetes mellitus: effect of sex, literacy skills, known diabetic complications and place of care on diabetic knowledge, reported self‐monitoring management and glycaemic control. Diabetic Medicine, 1999; 16: 591–597. [DOI] [PubMed] [Google Scholar]
- 61. Heuer L, Lausch C. Living with diabetes: perceptions of Hispanic migrant farmworkers. Journal of Community Health Nursing, 2006; 23: 49–64. [DOI] [PubMed] [Google Scholar]
- 62. Hill‐Briggs F, Cooper DC, Loman K, Brancati FL, Cooper LA. A qualitative study of problem solving and diabetes control in type 2 diabetes self‐management. The Diabetes Educator, 2003; 29: 1018–1028. [DOI] [PubMed] [Google Scholar]
- 63. Ho EY, James J. Cultural barriers to initiating insulin therapy in Chinese people with type 2 diabetes living in Canada. Canadian Journal of Diabetes, 2006; 30: 390–396. [Google Scholar]
- 64. Huang ES, Gorawara‐Bhat R, Chin MH. Self‐reported goals of older patients with type 2 Diabetes Mellitus. Journal of the American Geriatrics Society, 2005; 53: 306–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hunt LM, Pugh J, Miguel V. How patients adapt diabetes self‐care recommendations in everyday life. The Journal of Family Practice, 1998; 46: 207–215. [PubMed] [Google Scholar]
- 66. Hunt LM, Valenzuela MA, Pugh JA. NIDDM patients' fears and hopes about insulin therapy: the basis of patient reluctance. Diabetes Care, 1997; 20: 292–298. [DOI] [PubMed] [Google Scholar]
- 67. Hunt LM, Valenzuela MA, Pugh JA. Porque me tocoa a mi? Mexican American diabetes patients' causal stories and their relationship to treatment behaviours. Social Science and Medicine, 1998; 46: 959–969. [DOI] [PubMed] [Google Scholar]
- 68. Hunt LM, Arar NH, Larme AC, Rankin SH, Anderson RM. Contrasting patient and practitioner perspectives in type 2 diabetes management. Western Journal of Nursing Research, 1998; 20: 656–682. [DOI] [PubMed] [Google Scholar]
- 69. Hunt LM, Arar NH, Akana LL. Herbs, prayer, and insulin use of medical and alternative treatments by a group of Mexican American Diabetes Patients. Journal of Family Practice, 2000; 49: 216–223. [PubMed] [Google Scholar]
- 70. Jayne RL, Rankin SH. Application of Leventhal's self‐regulation model to Chinese immigrants with type 2 diabetes. Journal of Nursing Scholarship, 2001; 33: 53–59. [DOI] [PubMed] [Google Scholar]
- 71. Jezewski MA, Poss J. Mexican Americans' explanatory model of type 2 diabetes. Western Journal of Nursing Research, 2002; 24: 840–858. [DOI] [PubMed] [Google Scholar]
- 72. Kokanovic R, Manderson L. Social support and self‐management of type 2 diabetes among immigrant Australian women. Chronic Illness, 2006; 2: 291–301. [DOI] [PubMed] [Google Scholar]
- 73. Kokanovic R, Manderson L. Exploring doctor‐patient communication in immigrant Australians with type 2 diabetes. Journal of General Internal Medicine, 2007; 22: 459–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lawton J, Ahmad N, Hallowell N, Hanna L, Douglas M. Perceptions and experiences of taking oral hypoglycaemic agents among people of Pakistani and Indian origin: a qualitative study. British Medical Journal, 2005; 330: 1247–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. Diabetes service provision: a qualitative study of the experiences and views of Pakistani and Indian patients with type 2 diabetes. Diabetic Medicine, 2006; 23: 1003–1007. [DOI] [PubMed] [Google Scholar]
- 76. Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. “I can't do any serious exercise”: barriers to physical activity amongst people of Pakistani and Indian origin with type 2 Diabetes. Health Education Research, 2006; 21: 43–54. [DOI] [PubMed] [Google Scholar]
- 77. Liburd LC, Namageyo‐Funa A, Jack L, Gregg E. Views from within and beyond: illness narratives of African‐American men with type 2 diabetes. Diabetes Spectrum, 2004; 17: 219–224. [Google Scholar]
- 78. Macaden L, Clarke CL. Risk perception among older South Asian people in the UK with type 2 diabetes. International Journal of Older People Nursing, 2006; 1: 177–181. [DOI] [PubMed] [Google Scholar]
- 79. Mull DS, Nguyen N. Vietnamese diabetic patients and their physicians: what ethnography can teach us. Western Journal of Medicine, 2001; 175: 307–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Parry KK, Mobley T, Allen O. Use of folk treatments for diabetic plantar ulcers among African Americans with Type II diabetes. International Journal of Rehabilitation and Health, 1996; 2: 265–275. [Google Scholar]
- 81. Phinney A, Wallhagen M. Recognizing and understanding the symptoms of type 2 diabetes. Canadian Journal of Nursing Research, 2003; 35: 108–124. [PubMed] [Google Scholar]
- 82. Polzer RL. African Americans and diabetes: spiritual role of the health care provider in self‐management. Research in Nursing and Health, 2007; 30: 164–174. [DOI] [PubMed] [Google Scholar]
- 83. Ponzo MG, Gucciardi E, Weiland M, Masi R, Lee R, Grace SL. Gender, ethnocultural, and psychosocial barriers to diabetes self‐management in Italian women and men with type 2 diabetes. Behavioral Medicine, 2006; 31: 153–160. [DOI] [PubMed] [Google Scholar]
- 84. Quatromoni PA, Milbauer M, Bosner BM, Carballaeira NP, Brunt M, Chipkin SR. Use of focus groups to explore nutrition practices and health beliefs of urban Caribbean Latinos with diabetes. Diabetes Care, 1994; 17: 869–873. [DOI] [PubMed] [Google Scholar]
- 85. Rosal MC, Goins KV, Carbone ET, Cortes DE. Views and Preferences of Low‐Literate Hispanics Regarding Diabetes Education: Results of Formative Research. Health Education Behaviour, 2004; 31: 388–405. [DOI] [PubMed] [Google Scholar]
- 86. Samuel‐Hodge CD, Headen SW, Skelly AH et al Influences on day‐to‐day self‐management of type 2 diabetes among African‐American women: spirituality, the multi‐caregiver role, and other social context factors. Diabetes Care, 2000; 23: 928–933. [DOI] [PubMed] [Google Scholar]
- 87. Sanghera R. Deterrents to participation in diabetes education: perspectives of elderly Indo‐Canadians. Canadian Journal of Diabetes Care, 2000; 24: 19–26. [Google Scholar]
- 88. Schoenberg NE, Stoller EP, Kart CS, Perzynski A, Chapleski EE. Complementary and alternative medicine use among a multiethnic sample of older adults with diabetes. Journal of Alternative and Complementary Medicine, 2004; 10: 1061–1066. [DOI] [PubMed] [Google Scholar]
- 89. Scott PA. Culture, food, diet and diabetes: the West Indian perspective. Practical Diabetes lnternational, 1997; 14: 209–211. [Google Scholar]
- 90. Stone M, Pound E, Pancholia A, Farooqi A, Khunti K. Empowering patients with diabetes: a qualitative primary care study focusing on South Asians in Leicester, UK. Family Practice, 2005; 22: 647–652. [DOI] [PubMed] [Google Scholar]
- 91. Stone MA, Patel N, Drake L, Gayle C. Making education in diabetes culturally appropriate for patients. Practice Nursing, 2006; 17: 621–625. [Google Scholar]
- 92. Utz SW, Steeves RH, Wenzel J et al “Working hard with it”: self‐management of type 2 diabetes by rural African Americans. Family & Community Health, 2006; 29: 195–205. [DOI] [PubMed] [Google Scholar]
- 93. Vincent D, Clark L, Zimmer LM, Sanchez J. Using focus groups to develop a culturally competent diabetes self‐management program for Mexican Americans. The Diabetes Educator, 2006; 32: 89–97. [DOI] [PubMed] [Google Scholar]
- 94. Wallin AM, Lofvander M, Ahlstrom G. Diabetes: a cross‐cultural interview study of immigrants from Somalia. Journal of Clinical Nursing, 2007; 16: 305–314. [DOI] [PubMed] [Google Scholar]
- 95. Wenzel J, Utz SW, Steeves R, Hinton I, Jones RA. “Plenty of sickness”: descriptions by African Americans living in rural areas with type 2 diabetes. Diabetes Educator, 2005; 31: 98–107. [DOI] [PubMed] [Google Scholar]
- 96. Harden A, Peersman G, Oliver S, Oakley A. Identifying primary research on electronic databases to inform decision‐making in health promotion: the case of sexual health promotion. Health Education Journal, 1999; 58: 290–301. [Google Scholar]
- 97. Flemming K, Briggs M. Electronic searching to locate qualitative research: evaluation of three strategies. Journal of Advanced Nursing, 2007; 57: 95–100. [DOI] [PubMed] [Google Scholar]
- 98. Bury M. Chronic illness as biographical disruption. Sociology of Health and Illness. 1982; 4: 167−182. [DOI] [PubMed] [Google Scholar]
- 99. Campbell R, Pound P, Pope C et al Evaluating meta‐ethnography: a synthesis of qualitative research on lay experiences of diabetes and diabetes care. Social Science and Medicine, 2003; 56: 671–684. [DOI] [PubMed] [Google Scholar]
- 100. Paterson B, Thorn S, Dewis M. Adapting to and managing diabetes. Journal of Nursing Scholarship, 1998; 30: 57–62. [DOI] [PubMed] [Google Scholar]
- 101. Tillotson L, Smith S. Locus of control, social support, and adherence to the diabetes regimen. Diabetes Educator, 1996; 22: 133–138. [DOI] [PubMed] [Google Scholar]
- 102. Conrad P. The experience of illness: recent and new directions. Research in Social Health, 1987; 6: 1–31. [Google Scholar]
- 103. Tyler T, Blader S. Identity and cooperative behavior in groups. Group Processes and Intergroup Relations, 2001; 4: 207–226. [Google Scholar]
- 104. Winkelman WJ, Choo CW. Provider‐sponsored virtual communities for chronic patients: improving health outcomes through organizational patient‐centred knowledge management. Health Expectations, 2003; 6: 352–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Helgeson V, Gottlieb B. Support groups In: Cohen S, Underwood L, Gottlieb BH. (eds) Social Support Measurement and Intervention: A Guide for Health and Social Scientists. New York: Oxford University Press, 2000: 221–245. [Google Scholar]
- 106. Hogg M, Terry D. Social identity and self‐categorization processes in organizational contexts. Academy of Management Review, 2000; 25: 121–140. [Google Scholar]
- 107. White M, Dorman S. Receiving social support online: implications for health education. Health Education Research, 2001; 16: 693–707. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1 Critical appraisal form (views).
Data S2 Type 2 diabetes & BME & self‐management.


