Abstract
Background
A person‐centred approach in the context of health services delivery implies a biopsychosocial model focusing on all factors that influence the person's health and functioning. Those wishing to monitor change should consider this perspective when they develop and use guidelines to stimulate active consideration of the person's needs, preferences and participation in goal setting, intervention selection and the use of appropriate outcome measures.
Objective
To develop a position paper that promotes a person‐centred approach in guideline development and implementation.
Design, setting and participants
We used three narrative discussion formats to collect data for achieving consensus: a nominal group technique for the Allied Health Steering Group, an Internet discussion board and a workshop at the annual G‐I‐N conference. We analysed the data for relevant themes to draft recommendations.
Results
We built the position paper on the values of the biopsychosocial model. Four key themes for enhancing a person‐centred approach in clinical guidelines emerged: (i) use a joint definition of health‐related quality of life as an essential component of intervention goals, (ii) incorporate the International Classification of Functioning, Disability and Health (ICF) as a framework for considering all domains related to health, (iii) adopt a shared decision‐making method, and (iv) incorporate patient‐reported health outcome measures. The position statement includes 14 recommendations for guideline developers, implementers and users.
Conclusion
This position paper describes essential elements for incorporating a person‐centred approach in clinical guidelines. The consensus process provided information about barriers and facilitators that might help us develop strategies for implementing person‐centred care.
Keywords: guidelines; health‐related quality of life; International Classification of Functioning, Disability and Health; patient‐centred care; shared decision making
Background
Health service providers in clinical practice are encouraged to adhere to evidence‐based guidelines, which are considered important tools for quality improvement and health outcomes.1 Evidence‐based medicine is based on the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients,2 whereas evidence‐based practice is the translation of the evidence into health services. Best‐practice health services also need to take into account the contextual factors that affect the person's health condition. Contextual factors include internal personal factors and external environmental factors. Personal factors derive from the individual and include gender, age and education. Environmental factors make up the physical, social and attitudinal environment of a person; they include family support and the health service system.3 Contextual factors may affect a person's functioning and can be either a barrier to or a facilitator for the improvement of personal health outcomes within a health services system.
Historically, health‐care decision making has been based on recommendations from quantitative medical research and knowledge that focus on medical diagnosis, impairments and treatment. However, the understanding of health conditions and a person's functioning, disability and health has changed from a medical perspective focusing on the individual's physical aspects to a biopsychosocial perspective that recognizes the relationship between the individual and other related context.4 The biopsychosocial model posits that biological, psychological and environmental or social factors all influence the individual's functioning and health outcomes.5 From the biopsychosocial perspective, health‐care professionals should consider not only disease processes and the biomedical aspects of the person, but also the environmental and personal factors, the person's quality of life (QoL) and participation in all major life areas including making decisions and the choice of and control over his/her health and the use of health services. This implies a paradigm shift in the awareness of the roles of health professionals and persons with a health problem. Health professionals should understand their role as a health service provider, and persons with (or at risk for) health problems are service users. Needs and expectations differ between persons, and it takes time to change the paradigm from a paternalistic approach and perspective of a ‘patient’ who can be viewed as a passive recipient of the health service to a user perspective where there is choice and control. In this manuscript, we will use terms to reinforce this paradigm shift and use health rather than health care, health service provider rather than health‐care professional and service user rather than patient, except in circumstances where these words are used in definitions, quotes or specific references.
Person‐centred approach
The terms ‘person‐centred’ and ‘patient‐centred’ are often used interchangeably in health services. In this paper, we have adopted the term ‘person‐centred’ to better reflect the biopsychosocial model. In a person‐centred approach, a person (the service user) is valued as an active participant of the health service. Evidence‐based interventions should be adapted to meet individual needs and preferences where possible. This approach provides insight into factors related to a disease and facilitates interventions congruent with personal values, beliefs and environmental conditions of the health service user. The adoption of a person‐centred approach in a health services system can influence personal factors such as patient satisfaction, motivation, adherence to therapy and thus health outcomes.6, 7, 8, 9 Elements of person‐centred care include communication and relevant information, as well as shared decision making (SDM) and self‐management support.10 The Institute of Medicine includes patient‐centred care as one of the six essential aims for improving health care.11 Although person‐centred care is advocated in clinical practice, its implementation is constrained due to variation in definitions, perceived barriers to valid and reliable outcome measurements and the inherent difficulty with shifting traditional patterns of interaction.10, 12, 13, 14, 15
Clinical practice guidelines
Clinical practice guidelines are important tools for synthesizing evidence and translating research findings into practice. Their purpose is to assist health service providers and service users in health behaviour and decision making. Clinical practice guidelines should specifically aim at integrating the complex interplay of science with the provider's experience, reasoning and judgment, and the person's values and preferences in conjunction with consideration of both the context of the health service and the person's environment.16 Guidelines potentially support a person‐centred approach by guiding the health service provider in considering all relevant domains of the person's health, facilitating individualized and meaningful goal setting, recommending appropriate intervention strategies and using outcome measures that monitor change in the person's health and functioning.
Guidelines International Network
The Guidelines International Network (G‐I‐N) is a global network that supports evidence‐based health care and improvement of health outcomes by promoting the development, implementation and use of clinical practice guidelines internationally. Two of the aims of the Allied Health Community of the G‐I‐N are to promote person‐centred health services and to promote health‐related QoL activities – objectives for prevention, assessment, intervention and evaluation – in multidisciplinary clinical guidelines. The aims of our study are to identify some of the key themes necessary to make guidelines more person‐centred and to develop a position paper to promote these elements for a person‐centred approach in guideline development and implementation.
Method
Study design
We adopted a consensus method, using a mix of techniques to draft the position statement. The method consisted of three stages for identifying key themes linked to person‐centredness for the position statement: (i) a nominal group technique (NGT) used in the G‐I‐N Allied Health Steering Group (three rounds) combined with a focused literature search, (ii) an Internet discussion board for G‐I‐N members, and (iii) a workshop at the G‐I‐N 2011 annual conference.
The NGT involves a structured approach with discussion between the participants and prioritization of the themes.17, 18 The G‐I‐N Allied Health Steering Group participated in three nominal group rounds in teleconference, which lasted 1.5 h each. These sessions took place between December 2010 and June 2011. The G‐I‐N Allied Health Steering Group consisted of nine members from four countries. Table 1 provides an overview of the members' characteristics.
Table 1.
Characteristics of Allied Health Group members and participants of the Internet discussion board
| Variable | Members of the Allied Health Steering Group | Respondents on the Internet discussion board |
|---|---|---|
| Number of participants | 9 | 14 |
| Sex male/female | 1/8 | 7/7 |
| Health‐care background | ||
| Physical therapist | 5 | 1 |
| Nurse | 2 | 1 |
| Occupational therapist | 1 | |
| Health scientist | 1 | |
| Human movement scientist | 1 | |
| Psychiatrist | 1 | |
| Pharmacist | 1 | |
| General internist | 1 | |
| General practitioners | 2 | |
| Librarian | 1 | |
| Unknown | 5 | |
| Country | ||
| Netherlands | 4 | 5 |
| United Kingdom | 2 | 4 |
| Germany | 3 | |
| Belgium | 1 | |
| Canada | 2 | |
| Australia | 1 | 1 |
We used similar approaches for each of the three rounds. The modified NGT consisted of the following stages: introduction and explanation, silent generation of ideas, sharing of ideas, group discussion and ranking of ideas. The choice of the NGT directly involved the participants in both data collection and analysis, which helped ensure that their findings and interpretations accurately reflected their thoughts. A topic guide was used for semi‐structured discussions in the stages of sharing ideas and group discussions. In between the nominal group sessions, we explored the literature about the emerging themes to develop clarity and definitions and to see how we could fit these themes into clinical practice guidelines. We searched the PubMed, Cinahl, and EMBASE databases using combinations of the following keywords: biopsychosocial model; International Classification of Functioning, Disability and Health (ICF); shared decision making; health‐related QoL; outcome measures; clinical practice guidelines.
Before each succeeding session, PW and SD provided an overview of the results of the previous session together with a summary of the findings from the literature review. We used the refined themes as the basis for further questioning, discussion and consensus development with the broader G‐I‐N community. Given the international character of person‐centredness research, we initiated an Internet group discussion with pre‐defined questions about the identified themes. The proposed methodology facilitated joining the discussions in a rapid and convenient manner. The targeted participants were the 180 G‐I‐N members. We used a generic approach in inviting all G‐I‐N members by email to join the Internet discussion board. We asked the participants to respond whether they had specific knowledge about one of the themes. In addition, we invited 10 experts external to the G‐I‐N who were knowledgeable about the themes to contribute to the Internet discussion. These experts were researchers and health service providers with specific expertise in the ICF, QoL research, SDM methods or patient‐reported outcome measures. All participants were asked to state whether they endorsed the themes and to respond to the related questions. The participants were encouraged to add comments and suggestions in contributing to the discussion about any of the themes. The website was open for 2 months (July and August 2011).
We organized a workshop at the annual G‐I‐N conference in Seoul in August 2011. The 250 participants of the international conference could choose from seven parallel programmes at the proposed time of the workshop. The aim of the workshop was to reflect on the themes and to initiate further discussion. During the workshop, an overview of the aim and method was provided, followed by the information about the themes, definitions and the questions. The participants were asked to respond to questions identical to those for the online discussion board to encourage further discussion and consensus. The discussions at the workshop were audio‐recorded and transcribed.
The G‐I‐N Allied Health Steering Group used information from all stages of the development to finalize the position statement by providing recommendations for guideline developers, guideline implementers and health service providers. Figure 1 presents an overview of the study design.
Figure 1.
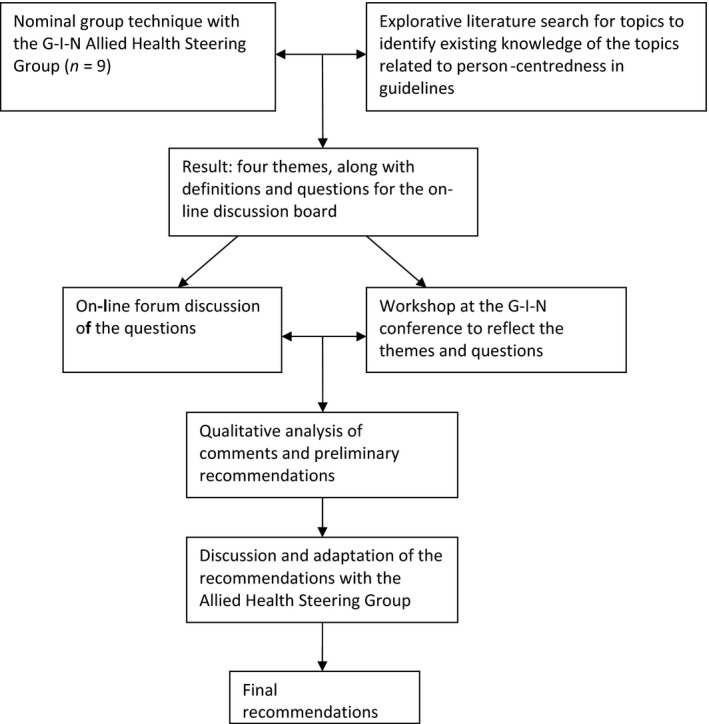
Overview of the study design.
Analysis
After the website closed, all comments from the discussion board were merged with the transcripts of the discussions from the workshop. We analysed the data to identify individual concepts of health professionals' perspectives. Similar arguments from different respondents were grouped, but individual remarks and disagreements were pointed out as well. One researcher (SD) selected key arguments and essential elements within each expert's reactions, and a second researcher (PW) validated all identified elements. The key arguments or topics raised for each theme were used to structure the results and to develop draft recommendations. The Allied Health Steering Group discussed and amended the draft recommendations.
Results
Nominal group sessions and the targeted literature search
The first nominal group session aimed at defining the scope of the position paper and topics for inclusion. This resulted in the biopsychosocial model for developing the position paper. The participants then shared ideas about how to integrate the biopsychosocial model into clinical guidelines and about which themes were relevant for incorporation in the position paper. The group of participants agreed on a shortlist of selected themes for further exploration in preparation for the second session. The selected themes were refined and grouped within themes during the second session. At the end of this session, we identified four themes to enhance a person‐centred approach in guidelines: (i) health‐related quality of life (HRQoL), (ii) ICF framework, (iii) SDM method, and (iv) HRQoL outcome measurement. In the third session, we discussed the selected themes and definitions and considered whether they are essential to enhancing the person‐centred approach in guideline development and implementation. This led to the selection of four key themes for further discussion via the Internet discussion board. The participants then shared ideas about the content of the Internet discussion board, for example what information should be included in addition to the definitions, what questions should be asked and who should be invited. This resulted in a structure for the Internet discussion board: provide a clear definition of each theme with background information and ask questions to initiate discussion for each of the key themes. Box 1 shows the definitions and questions for the discussion board.
Box 1. Themes and questions on the Internet discussion board.
| Theme | Definitions and questions |
|---|---|
| HRQoL | Definition: the person's perception of the impact of his disease and its intervention(s) in his daily life – physical, psychological, and social functioning and well‐being. |
| Question: Should the concept of HRQoL be used in all guidelines? | |
| ICF | Definition: the ICF as a good classification and framework for functioning, disability, and health‐related domains. These domains are classified by body, functions, and structures; activities and participation; and personal and external perspectives. |
|
Questions: Do guideline developers, guideline implementers, and service providers generally accept the ICF framework? Does the ICF provide a good framework for promoting quality of life in guidelines? |
|
| SDM | Definition: decision‐making jointly shared by patients and their health service providers is a move toward seeing patients as having a central role with the aim of strengthening and empowering them to express their values and preferences, to ask questions, and to participate actively in their own health. |
|
Questions: Do guideline developers, guideline implementers, and health service providers generally accept the SDM method? Should decision aids be recommended in guidelines? |
|
| Quality‐of‐life outcome measurement | Definition: Quality‐of‐life measures capture patients' perspectives of their diseases and interventions, their perceived need for health services, and their preferences for interventions and outcomes. Such measures are useful for goal setting and decision‐making for the individual patient. |
| Questions: Do patient‐reported outcome measures contribute to promoting quality of life in guidelines?Should guideline developers aim at including measures related to quality of life in all guidelines? |
HRQoL, health‐related quality of life; ICF, International Classification of Functioning, Disability and Health; SDM, shared decision making.
Key themes
The Allied Health Steering Group identified four themes that we considered essential to enhancing a person‐centred approach in guideline development and implementation. The themes were as follows:
Use a single definition of QoL as an essential component of guideline recommendations
Although QoL and HRQoL are often used interchangeably, they are in fact different constructs.19 ‘Quality of life’ has been defined as the capacity of an individual to achieve his/her life plans, or as the difference, at a particular point in time, between the hopes and expectations of an individual and his/her present situation.20 A generally accepted definition of HRQoL is the person's (patient's) subjective perception of the impact of his/her disease and its intervention(s) on his/her daily life – physical, psychological and social functioning and well‐being.21 In this paper, we use HRQoL because, by definition, it reflects the biopsychosocial model and a person‐centred care approach, and it seems to be the most appropriate in the context of health services.
Use a construct that covers all domains related to the person's health
The World Health Organization (WHO) has developed the ICF to provide unified, international and standardized language to describe and classify health and health‐related domains. This furnishes a common framework for health and health‐related outcome measurement.3, 22 The ICF incorporates three main domains of health and functioning: body functions and structures, activities and participation, and contextual factors (environmental and personal factors) and is aetiologically neutral. The ICF provides a framework for understanding health, disability and functioning, as well as a classification system for use in clinical practice and research.23, 24, 25, 26, 27 Figure 2 provides an overview of the domains of the ICF. The ICF creates a foundation for considering all aspects of the person's health condition during clinical assessment and for incorporation in guidelines; it is useful for diagnosis, goal setting, intervention selection and evaluation because it takes into account the contextual factors.3, 24, 28, 29, 30, 31, 32
Figure 2.
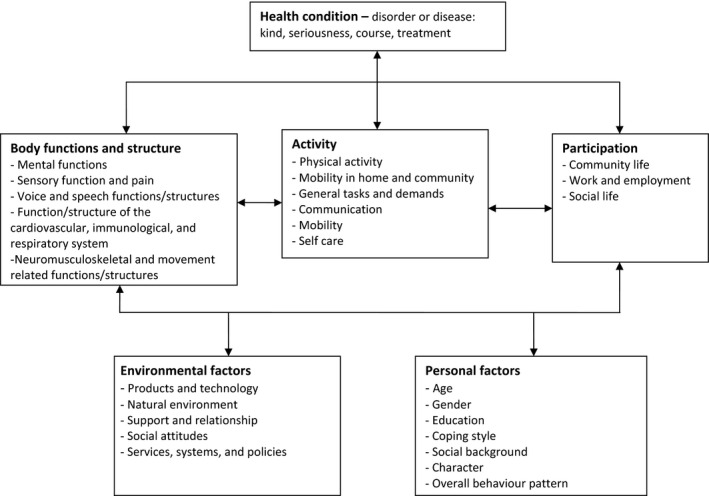
Domains of the International Classification of Functioning, Disability and Health.
Promote the use of a SDM method
Shared decision making promotes informed choices, ensuring that person–professional interaction is responsive to individual needs, values and priorities.33 It is a process in which the health service provider and the person with health problems as service user make a choice jointly;34 SDM is pivotal to person‐centred care.35 User involvement at each stage in the development of a clinical guideline is essential to facilitate the adoption of SDM methods within a guideline. Involving service users and representatives in developing a guideline will ensure that the views, experiences and interests of users are considered in the guideline. The guideline needs to promote SDM methods at the level of the health service consultation. In clinical practice, SDM promotes active participation in intervention decision making, self‐efficacy and self‐management.
Monitor health outcomes
For comprehensive assessment of the benefits of an intervention, it is essential to provide evidence of the impact of the health services on the person's health condition in all domains of health. Guidelines should therefore promote monitoring of health outcomes in clinical practice. The HRQoL measurement refers to aspects of the individual's physical, emotional and social well‐being,36 and it reflects all domains of health articulated in the biopsychosocial model. Most HRQoL measurements are based on patient‐reported outcome measures (PROMS), which are used in clinical practice to gain more insight into the way a person perceives his/her health and the impact of interventions on his/her QoL.37 Frequently used instruments of HRQoL measurement are generic (e.g. the Short Form (36) Health Survey) or disease specific (e.g. the Asthma Quality of Life Questionnaire). The benefits of measuring PROMS in clinical practice include facilitating communication about issues that are important to the patient as service user (which promotes SDM), evaluating the response to the intervention and enabling continuous assessment of quality of care.38, 39
Internet discussion board and workshop
We received 38 comments from 17 participants; 14 participants on the Internet discussion board and three participants in the workshop. There were comments on each theme within the proposed framework.
General comments
All participants confirmed the importance of a person‐centred approach, and some participants acknowledged that a person‐centred approach is currently not routinely integrated into guidelines and clinical practice.
The change from a medical perspective towards a more biopsychosocial model has not been achieved yet' and ‘Patient perspectives are needed in study designs, guideline development and implementation in clinical practice.
Health‐related quality of life
Most participants embraced the idea of including the concept of HRQoL in guidelines.
If we purport to use evidence‐based clinical practice and SDM, we must incorporate HRQoL as a central feature of guideline development. Engaging patients at the initial inception of the guideline and then at all following stages is critical.
Some participants suggested that improved QoL should be addressed as an ultimate goal in guidelines focusing on chronic diseases and health conditions with a high HRQoL impact.
The concept of HRQoL should be used in most guidelines, certainly for guidelines about chronic conditions and sometimes for non‐chronic conditions or problems too.
It is probably not relevant to include HRQoL in guidelines dealing with acute conditions when it can have but little long‐term effect.
Several participants emphasized the importance of HRQoL in guideline development and clinical practice in relation to goal setting for the intervention and the person's own responsibility for his/her health, whilst cultural and cost aspects should be taken into account.
The main goal is quality of life, but in clinical reasoning, more goals can be formulated to reach this main goal… this means that QoL measurement should be related to the common goal of both the patient and the provider.
Physicians themselves must adopt the patient's HRQoL as one of their major treatment aims and discuss HRQoL issues with the same priority as objective patient data.
When the concept of HRQoL is used in guideline development, one should also pay attention to the dimension of “culture”, “the spiritual level”, and “economic aspects”, depending on the topic or focus.
Other participants noted the need for further research for the usability and applicability of HRQoL measures, which is a prerequisite for incorporation in guidelines.
As guideline developers, we are also dependent on whether the concept of HRQoL is being used in the related healthcare and medical research – and of course whether it is being used by healthcare professionals themselves in daily practice. Building up evidence and developing guidelines is only possible on the basis of good research and implementation in daily practice.
International Classification of Functioning, Disability and Health
All respondents affirmed that the ICF framework provides guidance in clinical practice for considering all relevant dimensions of health, and it takes into account the facilitators for and barriers to recovery.
Personal and environmental factors are the most important ones in client‐centred care and shared decision‐making.
The ICF framework and coding system are generally not used in guidelines, except for some examples in the field of rehabilitation, occupational therapy and physical therapy. A few participants noted the dominance of disease‐related clinical outcomes and the complicated and time‐consuming coding system as reasons for the limited use of the ICF, although the framework is appropriate for considering all domains of health.
Most questions developed by guideline teams and researchers focus on the body functions and activity because these are deemed easier and more accurate measurement domains. This view is often echoed in clinical assessments and treatment plans. The ICF would be an excellent and appropriate framework, but it may require further “education” of peers to place it in its appropriate perspective.
Shared decision making
The participants perceived SDM positively as a way to incorporate personal values and intervention preferences because it will make persons with questions and needs active members in goal setting and empower them to take an interest and responsibility for their health.
Healthcare providers increasingly recognize the relevance of patient involvement in decision‐making and patient activation in care in general, especially when self‐management is required.
The participants noted increased recognition of the facilitating role guidelines might have in SDM by taking into account information about consequences of interventions, but also by considering whether decision aids and the development of patient versions (service users) were included in the guidelines.
Guidelines should move to a situation where there are patient versions that act as if they are decision support tools.
However, according to some participants, SDM is not widely implemented in clinical practice because health service providers lack skills and use their own perceptions and definitions about the involvement of patients as service users in medical decision making.
Providers do not always have the skills to activate patients in decision‐making.
Shared decision‐making is not suitable for all patients. Some of them will say, “Doctor, please tell me what to do… You know what's the best option for me.”
However, other participants state that there are barriers to the understanding of the SDM method in the guideline develop team.
I'm not sure that SDM has already been implemented in the minds of guideline developers', and ‘If it were accepted, then the concept of declaring reasonable options would be common.
Comparative information in meaningful and accessible format is a prerequisite for SDM, which is still a challenge.
Comparative, unbiased information is often not available, not even to the healthcare professional. So how can we expect doctors to be able to inform their patients correctly?
If decision aids are produced by commercial organizations (e.g. software companies) you need to be particularly careful about bias.
Outcome measures of health‐related quality‐of‐life
The participants highlighted the relevance of using HRQoL PROMS in addition to clinical measures to facilitate the dialogue between the person and professional about what is important to them and to the relevance and effectiveness of the intervention. Therefore, outcome measures that are specific and relevant to the targeted population must be incorporated into the guidelines.
Outcome measures can certainly contribute and should be included – but they should be linked to the key clinical questions and the key messages of the guideline.
The participants emphasized the importance of using evidence‐based instruments that are suitable for routine clinical practice in order to incorporate HRQoL outcome measurements into guidelines and to facilitate implementation in clinical practice. They also emphasized the principle that measurement results should be immediately available to the individual.
For many conditions, there is no good evidence whether one should use a disease‐specific instrument or a generic one and whether one of the available instruments is preferable in the given circumstances.
There needs to be an understanding of the tools and knowledge of how to interpret the result; for example, to know whether any change is meaningful.
Discussion
This position paper describes four themes that we perceived to be important for a person‐centred approach in guidelines. In guideline development, person‐centred care means promoting the active involvement of the person in taking an active role and responsibility for his/her own health, ensuring better consideration of the person's needs, preferences and context and evaluating relevant health outcomes. The ultimate aim of health services should be to increase or maintain the person's HRQoL. All domains within the ICF framework are potentially relevant and should be considered for incorporation in the guideline during development. This framework is also important for developing an understanding of the interactions between all domains of the individual's health in clinical practice. The use of the ICF and HRQoL measures will promote the use of SDM methods and provide opportunities to map scenarios for individualized person‐centred goals and realistic intervention strategies. The personal perspective is incorporated at various levels: by taking personal factors into account at the ICF level, by involving the service user at the SDM level and by considering the HRQoL PROMS for feedback from the individual about his/her perceived health and the effect of interventions.
The impact of a person‐centred approach
We argue that person‐centred care focuses sharply on participation of the person in clinical decision making by taking into account his/her perspective and by tailoring health services to the needs and preferences of the person. This approach has important implications for the outcome measures and the evaluation of the effectiveness of person‐centred interventions. The implication is that outcome measures should be related to the perceived effect on HRQoL.
Patient‐reported outcomes may also have benefits for improving problem detection, defining intervention goals, user–provider communication, SDM and assessing the effectiveness of the intervention.40, 41, 42, 43 This is especially relevant for managing chronic diseases (where evidence‐based health services require increasingly complicated and expensive interventions) and for the on‐going support for self‐management.44 Guideline developers must be aware of these benefits and should search for PROMS that are relevant to the targeted population.
Challenges for a person‐centred approach in clinical guidelines
The translation of evidence into clinical practice guidelines has been widely adopted in modern health services, although adherence to guidelines is extremely variable.45, 46, 47, 48 Evidence‐based medicine offers the best available evidence for the most effective intervention, mostly via randomized clinical trials. Clinical trials typically use strict inclusion criteria and outcome measures focused on specific diagnosis and the biomedical condition, and it frequently neglects relevant factors in decision making.49 Diverse barriers hinder translation of the results of clinical trials into clinical practice. These barriers include individual characteristics, interventions and health service providers, as well as environmental and practical issues, which are embedded in everyday ‘real life’ feasibility issues that prevent strict adherence to guidelines.50, 51, 52
A person‐centred focus has a holistic, biopsychosocial perspective: there is a sharp focus on participation in the diagnostic procedure, goal setting, intervention selection and prioritization of outcomes from both the provider and the user. Health service providers perceive tension between the need to respect personal preferences and the pressure to strictly apply guidelines. It is a challenge for health service providers to integrate both paradigms in clinical decision making2, 49 and to resolve what are still sometimes seen as competing issues. The participants pointed out the dominance of the medical model in curricula and research as a limitation of the biopsychosocial perspective. The relative unfamiliarity of the framework of the ICF in the results of this study and in the literature confirms this.53 Providing more information about the ICF framework might be a good approach for making the shift from the medical or social model to a solid application of the biopsychosocial model in a SDM approach.
Guidelines have yet to integrate evidence and tools that could enable the health service providers to consider personal values and preferences and to discuss alternative interventions.23 The use of HRQoL PROMS in clinical practice is limited.37, 54, 55 Our study participants recognize the benefits of these measures because they add a unique value and can inform person–professional decision making. The HRQoL PROMS provide information about how alternative interventions compare in terms of their benefits and risks for goal setting and about selecting the best intervention.42 Guideline developers should include outcome measures in such a way that they facilitate the translation of generalized, evidence‐based recommendations into individualized preference‐based decisions for specific groups of people. This means that HRQoL PROMS should be included in guidelines, in addition to clinical measures of biomedical status (e.g. laboratory, radiographic and physical examination). The participants noted guideline developers' difficulties in choosing the best measure (e.g. should it be based on the best evidence or the goal of including the outcome measure?) and barriers in clinical practice such as time constraints, interpreting results and the link to goal setting. These and other barriers such as costs, applicability to individuals, outcome measurement skills and possible lack of motivation for collecting and using PROMS must be considered.37, 54, 56, 57, 58, 59, 60 Training health professionals may be necessary to overcome such barriers, and this training should be part of the guideline implementation.
Involvement of service users is important not only in clinical practice, but also in guideline development. The AGREE Research Trust has developed the Appraisal of Guidelines for Research and Evaluation (AGREE II) instrument for guideline development, reporting and assessment. One of the quality criteria concerns patient involvement as service users in the development of the guidelines.61, 62 Recently, the G‐I‐N proposed a key set of components for guideline development that emphasizes the importance of including personal preferences of users in the rating of evidence and recommendations.63 Our participants have reported that SDM is not widely adopted in guideline development and clinical practice. Active involvement of patients as service users in the early stages of developing the guideline is important for addressing themes that are important to these users64 and leads to the identification of issues that may not have otherwise been considered.65, 66 Engaging service users is essential for recognizing the impact of the health condition or disease on functioning and QoL and also to get insight into the possible options and active participation in the intervention strategies. Guideline recommendations at the decision‐making level and decision aids for the service user can make clinical practice guidelines more sensitive to the person's preferences. Decision aids increase people's involvement and empowerment, improve knowledge and promote a realistic perception of outcomes. They also appear to have a positive effect on user–provider relationships.67, 68, 69
Limitations
This study has several limitations. First, there was little response to the Internet discussion board and at the conference. Whilst we invited all G‐I‐N members, many may not have considered themselves specific experts on the themes, but it may also reflect the G‐I‐N membership. The focus of many G‐I‐N members may be the content of clinical guidelines rather than joining a meta‐level discussion as we conducted in our study. Another reason for the low response could be the relatively short period (July and August) and the time of the year, which is the period when many G‐I‐N members in the northern hemisphere may have taken their vacation. The participants were mostly clinicians (e.g. physicians and allied health professionals), and their comments were on the individual level of interaction between person and clinician. The principles involved may be applicable to a person‐centred approach in public health as well.
Second, whilst we focused our literature search on key themes and definitions, it was not an exhaustive or systematic review. As a result, we may have missed relevant definitions and interpretations of key themes beyond the four identified themes for improving person‐centred care in guidelines. Despite this, the G‐I‐N Allied Health Steering Group considers it worthwhile to start the challenge to guideline developers, users and implementers to incorporate and consider these four most relevant themes identified in this study.
Recommendations
The G‐I‐N's Allied Health Community seeks to promote best practice by adopting a person‐centred approach in developing guidelines and their implementation. This requires an integrated approach that considers the complex interaction of the relation of the underlying disease with the functioning of the individual in his/her social context and the inclusion of individual values and preferences. Table 2 presents our final recommendations for guideline developers, guideline implementers and health service providers for enhancing a person‐centred care approach throughout guideline development, as well as during guideline implementation. The next steps for further research should be to analyse current guidelines for evidence of person‐centred care approaches and to explore variations in guideline recommendations regarding their integration.
Table 2.
Recommendations for guideline developers, guideline implementers and health service providers
| Guideline developers |
| Explicitly describe HRQoL in the guideline for exploring the needs and values of the patient as a service user, goal setting and outcome measures. |
| Use the ICF framework for the guideline to describe all relevant dimensions of the individual's functioning, health, and disability, and consider the interacting factors. |
| Define outcome measures that address the intervention's effectiveness in the relevant ICF domains. |
| Incorporate service users as active members in developing the guideline. |
| Include decision aids in guidelines, together with the evidence‐based information that underpins shared decision making. |
| Provide a service user version of the guideline or make information available in plain language and include information about the advantages and disadvantages of interventions and possible choices. |
| Guideline implementers |
| Present tailored information about the professional responsibility to share information with service users, to ask about their needs and values, to offer different intervention options if appropriate and to engage them in intervention and outcome measures. |
| Provide accurate support tools based on the ICF to describe health factors explicitly. |
| Use adequate linking rules to connect health problems to intervention goals and outcome measures for HRQoL, related to the ICF domains. |
| Health service providers |
| Recognize the individual's HRQoL in diagnosis, goal setting and intervention selection. |
| Consider all relevant dimensions of the individual's health functioning and disability and all interacting factors in line with the ICF framework. |
| Use service user reported health outcomes, based on quality‐of‐life measurements, for shared goal setting, intervention selection and user participation and evaluation. |
| Provide and share clear and evidence‐based information with the individual and others who are involved in their intervention decisions. |
| Tailor the information to the individual and include advantages and disadvantages of intervention options. |
HRQoL, health‐related quality of life; ICF, International Classification of Functioning, Disability and Health.
Conflicts of interest
There are no conflicts of interest for any of the authors.
Funding
The Dutch Council for Quality of Healthcare and the Royal Dutch Society for Physical Therapy supported the project financially (without restrictions on the scientific work; Grant Number 89‐89100‐98‐206).
Disclaimer
The Guidelines International Network (G‐I‐N) is an international not‐for‐profit association of organizations and individuals involved in the development and use of clinical practice guidelines. G‐I‐N is a Scottish Charity, recognized under Scottish Charity Number SC034047. More information on the Network and its activities is available on its website: www.g-i-n.net. This paper reflects the views of its authors, and the Guidelines International Network is not liable for any use that may be made of the information contained therein.
Disclosure
Philip van der Wees was Chair of the Guidelines International Network from 2010 to 2012.
Acknowledgements
We would like to thank all participants from the Internet board discussion and the workshop at the G‐I‐N conference for their contribution: C. Herrmann‐Lingen, M. Nijhuis‐van der Sanden, M. van den Berg, T. Howe, G. Ollenschläger, R. Harbour, J. Wilson, P. van Royen, T. van Achterberg, W. Göttgens, B. Shaw, G. Elwyn, M. Faber, S. Steinhausen (and three confidential contributors from the workshop at the conference). We especially would like to thank F. Macbeth of the G‐I‐N Board of Trustees for reviewing the final draft of this paper.
Appendix 1. Members of the G‐I‐N Allied Health Steering group
S. Bazin (SB), Chartered Society of Physiotherapy, London, UK. D. van Benthem (DvB), Dutch Association of Integrated Cancer Centres, Utrecht, The Netherlands. D. Dreesens (DD), Dutch Councis for Quality of Care, The Hague, The Netherlands. S. A. van Dulmen (SD), Radboud University Nijmegen Medical Centre, Scientific Institute for Quality of Healthcare, Nijmegen, The Netherlands. J. Gordon (JG), Royal College of Nursing, London, UK. S. Lukersmith (SL), Lukersmith & Assoc., Sydney, NSW, Australia. J. Muxlow (JM), School of Nursing, Dalhousie University Halifax, Nova Scotia, Canada. E. Santa Mina (ESM), Ryerson University Toronto, Toronto, ON, Canada. P. J. van der Wees (PW), Radboud University Nijmegen Medical Centre, Scientific Institute for Quality of Healthcare, Nijmegen, The Netherlands.
References
- 1. Grol R. Improving the quality of medical care: building bridges among professional pride, payer profit, and patient satisfaction. JAMA, 2001; 286: 2578–2585. [DOI] [PubMed] [Google Scholar]
- 2. Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. British Medical Journal, 1996; 312: 71–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization . Towards a Common Language for Functioning, Disability and Health – ICF. In: WHO/EIP/GPE/CAS. Geneva: WHO, 2002. [Google Scholar]
- 4. Kraus de Camargo O. Systems of care: transition from the bio‐psycho‐social perspective of the International Classification of Functioning, Disability and Health. Child: Care, Health and Development, 2011; 37: 792–799. [DOI] [PubMed] [Google Scholar]
- 5. Engel GL. The need for a new medical model: a challenge for biomedicine. Science, 1977; 196: 129–136. [DOI] [PubMed] [Google Scholar]
- 6. Henbest RJ, Stewart M. Patient‐centredness in the consultation. 2: does it really make a difference? Family Practice, 1990; 7: 28–33. [DOI] [PubMed] [Google Scholar]
- 7. Henbest RJ, Fehrsen GS. Patient‐centredness: is it applicable outside the West? Its measurement and effect on outcomes. Family Practice, 1992; 9: 311–317. [DOI] [PubMed] [Google Scholar]
- 8. Kinnersley P, Stott N, Peters TJ, Harvey I. The patient‐centredness of consultations and outcome in primary care. British Journal of General Practice, 1999; 49: 711–716. [PMC free article] [PubMed] [Google Scholar]
- 9. Stewart MA. Effective physician‐patient communication and health outcomes: a review. Canadian Medical Association Journal, 1995; 152: 1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 10. Robinson JH, Callister LC, Berry JA, Dearing KA. Patient‐centered care and adherence: definitions and applications to improve outcomes. Journal of the American Academy of Nurse Practitioners, 2008; 20: 600–607. [DOI] [PubMed] [Google Scholar]
- 11. IOM . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: Institute of Medicine, 2001. [Google Scholar]
- 12. Schunemann HJ, Fretheim A, Oxman AD. Improving the use of research evidence in guideline development: 10. Integrating values and consumer involvement. Health Research Policy and Systems / BioMed Central, 2006; 4: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Krahn M, Naglie G. The next step in guideline development: incorporating patient preferences. JAMA, 2008; 300: 436–438. [DOI] [PubMed] [Google Scholar]
- 14. Mead N, Bower P. Patient‐centredness: a conceptual framework and review of the empirical literature. Social Science & Medicine, 2000; 51: 1087–1110. [DOI] [PubMed] [Google Scholar]
- 15. Gillespie R, Florin D, Gillam S. How is patient‐centred care understood by the clinical, managerial and lay stakeholders responsible for promoting this agenda? Health Expectations, 2004; 7: 142–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. IOM . Clinical Practice Guidelines We Can Trust. Washington, D.C.: Institute of Medicine, 2011. [Google Scholar]
- 17. Potter M, Gordon S, Hamer P. The physiotherapy experience in private practice: the patients' perspective. The Australian Journal of Physiotherapy, 2003; 49: 195–202. [DOI] [PubMed] [Google Scholar]
- 18. Jones J, Hunter D. Consensus methods for medical and health services research. British Medical Journal, 1995; 311: 376–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Davis E, Waters E. Re: a structured review of studies on health‐related quality of life and economic evaluation in pediatric acute lymphoblastic leukemia. Journal of the National Cancer Institute, 2005; 97: 1786–1787. [DOI] [PubMed] [Google Scholar]
- 20. Bjornson KF, McLaughlin JF. The measurement of health‐related quality of life (HRQL) in children with cerebral palsy. European Journal of Neurology, 2001; 8: 183–193. [DOI] [PubMed] [Google Scholar]
- 21. EMEA . Reflection Paper on the Regulatory Guidance for the Use of Health Related Quality of Life (HRQL) Measures in the Evaluation of Medicinal Products. London: EMEA, 2005, accessed 10 April 2012. [Google Scholar]
- 22. Cieza A, Stucki G. The International Classification of Functioning Disability and Health: its development process and content validity. European Journal of Physical and Rehabilitation Medicine, 2008; 44: 303–313. [PubMed] [Google Scholar]
- 23. Boivin A, Legare F, Gagnon MP. Competing norms: Canadian rural family physicians' perceptions of clinical practice guidelines and shared decision‐making. Journal of Health Services Research & Policy, 2008; 13: 79–84. [DOI] [PubMed] [Google Scholar]
- 24. Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustun B, Stucki G. ICF linking rules: an update based on lessons learned. Journal of Rehabilitation Medicine, 2005; 37: 212–218. [DOI] [PubMed] [Google Scholar]
- 25. Stucki G, Kostanjsek N, Ustun B, Cieza A. ICF‐based classification and measurement of functioning. European Journal of Physical and Rehabilitation Medicine, 2008; 44: 315–328. [PubMed] [Google Scholar]
- 26. Fayed N, Cieza A, Bickenbach J. Illustrating child‐specific linking issues using the Child Health Questionnaire. American Journal of Physical Medicine & Rehabilitation, 2012; 91: S189–S198. [DOI] [PubMed] [Google Scholar]
- 27. Fayed N, Cieza A, Bickenbach JE. Linking health and health‐related information to the ICF: a systematic review of the literature from 2001 to 2008. Disability and Rehabilitation, 2011; 33: 1941–1951. [DOI] [PubMed] [Google Scholar]
- 28. Heerkens Y, Bougie T, Claus E. The use of the ICF in the process of supplying assistive products: discussion paper based on the experience using a general Dutch prescription guideline. Prosthetics and Orthotics International, 2011; 35: 310–317. [DOI] [PubMed] [Google Scholar]
- 29. Jorgensen U, Melchiorsen H, Gottlieb AG, Hallas V, Nielsen CV. Using the International Classification of Functioning, Disability and Health (ICF) to describe the functioning of traumatised refugees. Torture, 2010; 20: 57–75. [PubMed] [Google Scholar]
- 30. Leonardi M, Raggi A, Antozzi C et al Identification of international classification of functioning, disability and health relevant categories to describe functioning and disability of patients with myasthenia gravis. Disability and Rehabilitation, 2009; 31: 2041–2046. [DOI] [PubMed] [Google Scholar]
- 31. Leach E, Cornwell P, Fleming J, Haines T. Patient centered goal‐setting in a subacute rehabilitation setting. Disability and Rehabilitation, 2010; 32: 159–172. [DOI] [PubMed] [Google Scholar]
- 32. Schneidert M, Hurst R, Miller J, Ustun B. The role of environment in the International Classification of Functioning, Disability and Health (ICF). Disability and Rehabilitation, 2003; 25: 588–595. [DOI] [PubMed] [Google Scholar]
- 33. Boivin A, Currie K, Fervers B et al Patient and public involvement in clinical guidelines: international experiences and future perspectives. Quality & Safety in Health Care, 2010; 19: e22. [DOI] [PubMed] [Google Scholar]
- 34. Towle A, Godolphin W. Framework for teaching and learning informed shared decision making. British Medical Journal, 1999; 319: 766–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Weston WW. Informed and shared decision‐making: the crux of patient‐centered care. Canadian Medical Association Journal, 2001; 165: 438–439. [PMC free article] [PubMed] [Google Scholar]
- 36. Garratt A, Schmidt L, Mackintosh A, Fitzpatrick R. Quality of life measurement: bibliographic study of patient assessed health outcome measures. British Medical Journal, 2002; 324: 1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fung CH, Hays RD. Prospects and challenges in using patient‐reported outcomes in clinical practice. Quality of Life Research, 2008; 17: 1297–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Valderas JM, Alonso J. Patient reported outcome measures: a model‐based classification system for research and clinical practice. Quality of Life Research, 2008; 17: 1125–1135. [DOI] [PubMed] [Google Scholar]
- 39. Guyatt GH, Ferrans CE, Halyard MY et al Exploration of the value of health‐related quality‐of‐life information from clinical research and into clinical practice. Mayo Clinic Proceedings, 2007; 82: 1229–1239. [DOI] [PubMed] [Google Scholar]
- 40. Au HJ, Ringash J, Brundage M, Palmer M, Richardson H, Meyer RM. Added value of health‐related quality of life measurement in cancer clinical trials: the experience of the NCIC CTG. Expert Review of Pharmacoeconomics & Outcomes Research, 2010; 10: 119–128. [DOI] [PubMed] [Google Scholar]
- 41. McKenna SP. Measuring patient‐reported outcomes: moving beyond misplaced common sense to hard science. BMC Medicine, 2011; 9: 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Valderas JM, Kotzeva A, Espallargues M et al The impact of measuring patient‐reported outcomes in clinical practice: a systematic review of the literature. Quality of Life Research, 2008; 17: 179–193. [DOI] [PubMed] [Google Scholar]
- 43. Greenhalgh J, Long AF, Flynn R. The use of patient reported outcome measures in routine clinical practice: lack of impact or lack of theory? Social Science & Medicine, 2005; 60: 833–843. [DOI] [PubMed] [Google Scholar]
- 44. Wagner EH. Meeting the needs of chronically ill people. British Medical Journal, 2001; 323: 945–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bauer MS. A review of quantitative studies of adherence to mental health clinical practice guidelines. Harvard Review of Psychiatry, 2002; 10: 138–153. [DOI] [PubMed] [Google Scholar]
- 46. Carlsen B, Glenton C, Pope C. Thou shalt versus thou shalt not: a meta‐synthesis of GPs' attitudes to clinical practice guidelines. British Journal of General Practice, 2007; 57: 971–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Grimshaw JM, Thomas RE, MacLennan G et al Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technology Assessment, 2004; 8: iii–iv, 1–72. [DOI] [PubMed] [Google Scholar]
- 48. Stewart RE, Vroegop S, Kamps GB, van der Werf GT, Meyboom‐de Jong B. Factors influencing adherence to guidelines in general practice. International Journal of Technology Assessment in Health Care, 2003; 19: 546–554. [DOI] [PubMed] [Google Scholar]
- 49. Bensing J. Bridging the gap. The separate worlds of evidence‐based medicine and patient‐centered medicine. Patient Education and Counseling, 2000; 39: 17–25. [DOI] [PubMed] [Google Scholar]
- 50. Rothwell PM. External validity of randomised controlled trials: “to whom do the results of this trial apply?”. Lancet, 2005; 365: 82–93. [DOI] [PubMed] [Google Scholar]
- 51. Cranney M, Warren E, Barton S, Gardner K, Walley T. Why do GPs not implement evidence‐based guidelines? A descriptive study Family Practice, 2001; 18: 359–363. [DOI] [PubMed] [Google Scholar]
- 52. Lugtenberg M, Burgers JS, Clancy C, Westert GP, Schneider EC. Current guidelines have limited applicability to patients with comorbid conditions: a systematic analysis of evidence‐based guidelines. PLoS ONE, 2011; 6: e25987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Cerniauskaite M, Quintas R, Boldt C et al Systematic literature review on ICF from 2001 to 2009: its use, implementation and operationalisation. Disability and Rehabilitation, 2011; 33: 281–309. [DOI] [PubMed] [Google Scholar]
- 54. Lohr KN, Zebrack BJ. Using patient‐reported outcomes in clinical practice: challenges and opportunities. Quality of Life Research, 2009; 18: 99–107. [DOI] [PubMed] [Google Scholar]
- 55. Hahn EA, Cella D, Chassany O, Fairclough DL, Wong GY, Hays RD. Precision of health‐related quality‐of‐life data compared with other clinical measures. Mayo Clinic Proceedings, 2007; 82: 1244–1254. [DOI] [PubMed] [Google Scholar]
- 56. Bausewein C, Simon ST, Benalia H et al Implementing patient reported outcome measures (PROMS) in palliative care–users' cry for help. Health and Quality of Life Outcomes, 2011; 9: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Cano SJ, Hobart JC. The problem with health measurement. Patient Preference and Adherence, 2011; 5: 279–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Brundage M, Bass B, Jolie R, Foley K. A knowledge translation challenge: clinical use of quality of life data from cancer clinical trials. Quality of Life Research, 2011; 20: 979–985. [DOI] [PubMed] [Google Scholar]
- 59. Legare F, Ratte S, Stacey D et al Interventions for improving the adoption of shared decision making by healthcare professionals. The Cochrane Database of Systematic Reviews (Online), 2010; (5): CD006732. [DOI] [PubMed] [Google Scholar]
- 60. Gravel K, Legare F, Graham ID. Barriers and facilitators to implementing shared decision‐making in clinical practice: a systematic review of health professionals' perceptions. Implementation Science, 2006; 1: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Brouwers MC, Kho ME, Browman GP et al Development of the AGREE II, part 1: performance, usefulness and areas for improvement. Canadian Medical Association Journal, 2010; 182: 1045–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Collaboration A. Development and validation of an international appraisal instrument for assessing the quality of clinical practice guidelines: the AGREE project. Quality & Safety in Health Care, 2003; 12: 18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Qaseem A, Forland F, Macbeth F, Ollenschlager G, Phillips S, van der Wees P. Guidelines International Network: toward international standards for clinical practice guidelines. Annals of Internal Medicine, 2012; 156: 525–531. [DOI] [PubMed] [Google Scholar]
- 64. Tong A, Lopez‐Vargas P, Howell M et al Consumer involvement in topic and outcome selection in the development of clinical practice guidelines. Health Expectations, 2011; 15: 410–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Uphoff EP, Wennekes L, Punt CJ et al Development of generic quality indicators for patient‐centered cancer care by using a RAND modified Delphi method. Cancer Nursing, 2012; 35: 29–37. [DOI] [PubMed] [Google Scholar]
- 66. Yen L, Gillespie J, Rn YH et al Health professionals, patients and chronic illness policy: a qualitative study. Health Expectations, 2011; 14: 10–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Stacey D, Bennett CL, Barry MJ et al Decision aids for people facing health treatment or screening decisions. The Cochrane Database of Systematic Reviews (Online), 2011; (10): CD001431. [DOI] [PubMed] [Google Scholar]
- 68. van der Weijden T, Boivin A, Burgers J, Schunemann HJ, Elwyn G. Clinical practice guidelines and patient decision aids. An inevitable relationship. Journal of Clinical Epidemiology, 2012; 65: 584–589. [DOI] [PubMed] [Google Scholar]
- 69. Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical guidelines: potential benefits, limitations, and harms of clinical guidelines. British Medical Journal, 1999; 318: 527–530. [DOI] [PMC free article] [PubMed] [Google Scholar]


