Abstract
Background and objective
Implementing preventive health care for young children provides the best chance of improving health and changing a child's life course. In Australia, despite government support for preventive health care, uptake of preventive services for young children is low. Using Andersen's behavioural model of health‐care utilization, we aimed to understand how parents conceptualized their children's preventive health care and how this impacted on access to preventive health‐care services.
Design
Semi‐structured telephone interviews conducted between May and July 2011.
Setting and participants
Twenty‐eight parents of children aged 3–5 years from three diverse socio‐economic areas of Melbourne, Australia.
Results
Thematic analysis showed parents' access to child preventive health care was determined by birth order of their child, cultural health beliefs, personal health practices, relationship with the health provider and the costs associated with health services. Parents with more than one child placed their own experience ahead of professional expertise, and their younger children were less likely to complete routine preventive health checks. Concerns around developmental delays required validation through family, friends and childcare organizations before presentation to health services.
Conclusions
To improve child preventive health requires increased flexibility of services, strengthening of inter‐professional relationships and enhancement of parents' knowledge about the importance of preventive health in early childhood. Policies that encourage continuity of care and remove point of service costs will further reduce barriers to preventive care for young children. Recent reforms in Australia's primary health care and the expansion of child preventive health checks into general practice present a timely opportunity for this to occur.
Keywords: Andersen's theory, general practice, parents, preventive healthcare, qualitative research, young children
Introduction
It is increasingly recognized that the onset of chronic diseases, such as hypertension, cardiovascular disease, stroke and diabetes, is predestined by events in utero and early childhood.1, 2 Similarly, compelling associations link childhood emotional experience with an increased risk of adult mental and physical health.3 The pre‐school period is a critical transition point4 where high‐quality health interventions can reap benefits, which may extend across the life course.5 Accordingly, timely and appropriate delivery of preventive health services in early life, defined as activities to stop, interrupt or slow the likelihood of developing a disease and its progression,6 has assumed great priority on national health agendas and in health services delivery.
In Australia, where health care is both privately and publically funded, maternal child health nurses, paediatricians and general practice services intersect across the early years of life to provide relatively comprehensive immunization, developmental surveillance and screening services.7 Childhood immunization coverage is high (93 per cent of 2‐year‐olds), neonatal hearing screening programme participation is increasing, and exclusive breastfeeding to 6 months is widely promoted.8 A snapshot of children's development as they enter school shows that the majority (75%) are doing well.9 However, health risks for Australian children exist: currently, 22% of children are considered developmentally vulnerable and 4.9 per cent have special needs.9 Immunization coverage at 6 years is lower than that at 2 years,10 one‐fifth of pre‐schoolers are overweight or obese,11 and dental caries affects half of 6‐year‐olds.12 Additionally 11 per cent of 2‐year‐olds and 20 per cent of 5‐year‐olds suffer clinically significant behavioural problems.13 Moreover, different population groups within Australia experience widely varying levels of morbidity, with children living in remote or low socio‐economic areas and indigenous children the most disadvantaged.10
In response to these figures, and as a means of containing the costs of an ageing population with increasingly complex chronic diseases, the Australian government has set targets for child preventive health on healthy eating, body weight and physical activity, and, most recently, child mental health.14, 15 Responsibility for much of this developmental surveillance rests with maternal and child health nurses (MCHN), registered nurses and midwives with additional qualifications in child and community health, located within local council areas, with services free at the point of care. In the state of Victoria, where this study was conducted, parents are encouraged to make 10 key visits scheduled from birth to three and half years, the first seven of which are meant to occur before the child's first birthday.16 Uptake of services is excellent (90% of families complete the first four visits) but drops off to less than 60 per cent for the final visit.17 Evaluation of MCHN services has focussed on maternal rather than child health outcomes, including maternal emotional health,18 use of the Edinburgh Postnatal Depression Scale,19 maternal service engagement and rates of normal vaginal delivery.20
Internationally, health checks of young children by physicians have demonstrated increased detection of physical, developmental and behavioural problems.21, 22, 23, 24 In 2008, to improve monitoring of children's health, the government introduced the Healthy Kids Check (HKC) – a pre‐school health assessment aimed at 4‐year‐old children. HKCs are conducted in general practice, an appropriate setting given that four of five Australians visit a general practitioner (GP‐equivalent to a family physician) each year, and health promotion and prevention are key activities in the provision of patient care.25 Delivered by GPs, general practice nurses or Aboriginal health workers, a rebate can only be claimed once, and only when pre‐school vaccinations are completed.26 Although publically funded (a Medicare rebate is available to parents for this item of care), initial uptake of the HKC was much lower than anticipated and only 16 per cent of 4‐year‐olds completed a HKC in the first year, with wide variation between and within states.27 Reasons for this discrepancy are not well understood in the Australian context. Thus, the aim of this study was to explore parents' perceptions of preventive health care for children. Using Andersen's behavioural model, we explain how parents acquire knowledge of ‘normal’ child health and development, describe how they recognize and deal with possible developmental problems, explain their intentions to undertake preventive child health care and portray their experiences of accessing services. We begin by providing an overview of Andersen's theory and our methods before presenting our findings, discussion and key conclusions.
Theoretical framework
Andersen's behavioural model is a well‐established theoretical framework used to understand individuals' use of health services and equitable access to health care. In the model, need for care determines how much an individual with certain predisposing characteristics (age, sex and culture) uses health services according to their personal and community resources that enable access. Environmental factors (physical, economic and political components including the health‐care system), health behaviours (health promoting behaviours and use of services) and outcomes (consumer satisfaction and health status) influence access to health‐care services and were added to later phases of the model (Fig. 1).28
Figure 1.
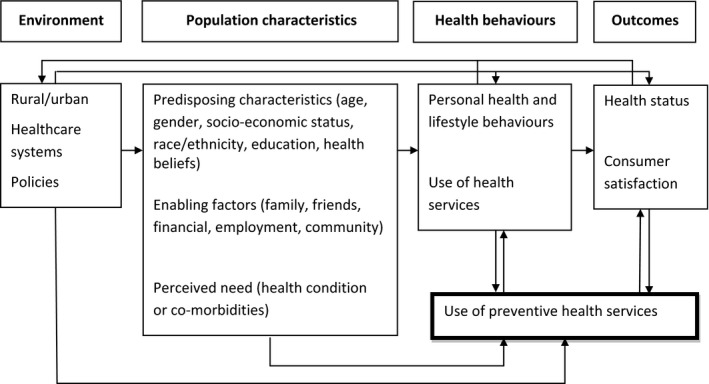
Andersen's Model of behavioural use of health services, and preventive health services.
For more than 30 years, Andersen's model has been empirically applied to multiple facets of medical care across diverse populations.29, 30, 31 Studies have shown that predisposing socio‐demographic factors such as gender, young age and ethnicity are barriers to accessing services32, 33, 34; specific health beliefs determined by culture, personal attitudes and values are powerful predictors for health service use35; educational achievements, increased household income and having health insurance enable access;36, 37, 38 and perceived need is a significant determinant for seeking care.37, 39 Other components of the model, health policy and health‐care safety‐net services,40 and health behaviours (previous use of services)33, 36 also impact on access to services.
For children's preventive health‐care, predisposing risk factors for non‐participation have been found to be young parental age,41 family structure (particularly single parent families)41, 42 and having older siblings.41 Language barriers may be the underlying reason for reduced use of services according to ethnicity43 or may indicate wider disparities in health behaviours and use of health services.44 Research shows the mixed effect of parental health beliefs on access to preventive child health‐care services. US data showed that mothers' beliefs about their child's health were not influential,45 but parents whose beliefs matched local guidelines for the timing of check‐ups were more likely to follow through with care.46 Families that lack personal resources (lower income, lower levels of education) have been found to be less likely to receive preventive services for their children.41 Outcomes for access were mixed with respect to need (increased in US study where the child was reported sick in the past year46; decreased in a Danish study with increasing number of hospitalizations41) and may reflect differing opportunities for preventive care in different health environments.
Qualitative studies have successfully applied Anderson's model to a diverse range of settings and health issues32, 47, 48, and quantitative studies have utilized Andersen's model to understand access to child health services including the use of emergency department for non‐urgent care,49 asthma care50 and preventive care.46 However, to the best of our knowledge, Anderson's model has not been qualitatively applied to child preventive health‐care services.
Method
Setting
Three socio‐economically diverse urban areas of Melbourne were chosen for the study: ‘Westgate’ (low socio‐economic), ‘Bayside’ (high socio‐economic) and ‘Dandenong’ [culturally and linguistically diverse (CALD)]. This third suburb was targeted to ensure the sample included the opinion of parents living in Australia for less than 10 years, as it was expected that their experience of accessing preventive health care could be quite different.51
Recruitment strategy
Parents were recruited from the community. The study was advertised in kindergartens, playgroups, community centres, maternal child health centres, libraries and supermarkets. Additional participants were recruited through snowballing. Potential participants were asked to contact the researchers and were selected if they had at least one child between the age of 3 and 5 years, lived in one of the three study areas, spoke English and had resided in Australia for more than 12 months. Recruitment was stopped when data saturation was achieved.52
Interviews
Data were collected between May and July 2011. Telephone interviews were conducted by the first two authors, following receipt of signed written consent. Interviews were tape‐recorded and lasted approximately 45 min. Respondents were offered an A$75 gift voucher to participate in the study. A semi‐structured interview guide, informed by Anderson's model, was used to question parents on their children's preventive health (Table 1).
Table 1.
Andersen's Behavioural Model of Health Services Use and development of questions for semi‐structured interview of parents
| Domains | Major concepts | Components | Examples of questions |
|---|---|---|---|
| Environment | Health care system | Personnel ‐ Medical and other | Do you have a regular doctor? |
| Organisational‐ health care systems in place |
What services are available to you in your community to help you monitor your child's health, growth and development? When considering visits to the doctor, how important is it for you to find a doctor who bulk‐bills? Have you ever received an invitation for your child to attend a health check? |
||
| Population characteristics | Predisposing characteristics | Demographic and social |
Could you tell me a little bit about you and your family? What language is spoken in the family home? |
| Health beliefs | I am interested to hear your views about your child's growth, development and behaviour – How do you monitor these aspects of your child's health? | ||
| Enabling resources | Personal and family |
Do you ever discuss issues about routine health care with your family or friends? Do you have any health insurance? |
|
| Perceived need |
Could you tell me about the health of your child in general over the last 12 months? Have you ever been concerned about your child's growth or development? What about eating and sleep? What about your child's emotional development and getting along with others? – What did you do? |
||
| Health behaviour | Personal health practices | Do you ever personally attend your doctor for a health check? | |
| Use of health services |
Has your child had a Healthy Kids Check or a pre‐school check? How about check‐ups with other health professionals? for example, dentist and optometrist Think back to the last time you had your child weighed/measured? Can you tell me about that? |
||
| Outcomes | Consumer satisfaction |
How satisfied are you with your maternal child health nurse services? What's your impression of the care you have received from doctors in the last few years? |
|
Data analysis
Data were analysed using thematic framework analysis comprising inductive and deductive techniques. The first two authors read, re‐listened and re‐read each transcript to familiarize themselves with the data and check for accuracy. They independently coded the data, then met to compare and discuss results and obtain consensus. As more codes were discovered, previously coded transcripts were checked to ensure that the codes still applied, in an iterative process to maintain quality within the data.53, 54 The third author was consulted to review the codes, resolve differences and oversee the linking of codes into categories. Data were finally imported into NVivo 8.55 Data were de‐identified to ensure participant anonymity. Approval was obtained from Monash University Human Research Ethics Committee.
Results
Twenty‐eight interviews were conducted. The mean age of participants was 40 years, and only one participant was male (Table 2). Ten participants were from CALD communities and had resided in Australia for less than 10 years (eight resided in the Dandenong region). Approximately half the sample could be classified as low‐ to middle‐income earners (based on receipt of family tax benefits and health insurance status). Eleven per cent of the sample had not completed secondary school, 64 per cent had an undergraduate degree, and 21% had a postgraduate qualification.
Table 2.
Characteristics of parents interviewed (n = 28)
| Number or range | |
|---|---|
| Age (years) | |
| Mean | 40 |
| Range | 30–47 |
| Gender | |
| Female | 27 |
| Male | 1 |
| Migrant less than 10 years | |
| UK | 4 |
| India/Ceylon | 2 |
| China | 1 |
| Vietnam | 1 |
| Hong Kong | 1 |
| Lebanon | 3 |
| Iraq | 2 |
| Marital status | |
| Married | 25 |
| Separated | 3 |
| Number of children | |
| 3–4 | 11 |
| 2 | 15 |
| 1 | 2 |
| Health Insurance | |
| Yes | 10 |
| No | 14 |
| Unknown | 4 |
| Family Tax Benefit Part Aa | |
| No | 10 |
| Yes | 16 |
| Unknown | 2 |
| Education level | |
| Not completed secondary school | 3 |
| Other qualification after secondary school | 7 |
| Undergraduate | 12 |
| Post graduate | 6 |
Recruited: 12 Playgroup Victoria newsletter; 4 kindergarten; 2 community centre; 1 supermarket community notice; 1 maternal child health centre; 8 snowball.
A government benefit payable for each child and adjusted according to number of children and taxable income.
Four themes were identified within Andersen's model: (i) the families' need, health belief systems and enabling resources (Population characteristics), (ii) health behaviour and parents' personal health practices, (iii) parents' satisfaction with the health service and continuity of care and (iv) financial barriers experienced by families when seeking preventive health care for their children.
Families' need, health belief systems and enabling resources
Perceived ‘need’ for preventive health services was primarily determined by birth order and the age of the child. In the early weeks of infancy, particularly for a first child, parents felt less confident managing feeding, growth and sleep behaviours and sought guidance from MCHN services. Contact with services diminished as the child got older. With subsequent children, parents were more confident, balancing the advice received from providers against knowledge gained from past experience. They frequently prioritized experience over expertise.
Especially being the second time now, I listen to the advice they give me about the feeding and things like that, but I think a lot of it is you have to just sort of decide what you're going to try yourself. (Belinda, 40 years, Bayside, 2 children)
Because she's my third I'm like, ‘Well, if she wants a dummy I'll do it’… It just seems it's not the pressure I think of your first one… it's not like I'm a bad mother, I'm doing it all wrong. (Rebecca, 38 years, Bayside, 3 children)
Parents were familiar with the schedule of visits proposed by MCHN services and the immunization requirements for young children. However, between 12 and 18 months of age (when primary vaccinations were completed), parents re‐evaluated the need for ongoing involvement with maternal and child health services. In our sample, one‐quarter (7/28) had not completed a visit at three and a half years. Some parents felt confident they could recognize developmental problems and others stated they were too busy managing their own or another child's health problems. CALD parents also said they preferred to use a doctor who spoke their first language.
Other cultural factors also influenced continuation with preventive services. Parents from overseas countries made positive comparisons favouring Australia's child health services. However, if advice conflicted with cultural expectations, satisfaction diminished and led to early discontinuation of services. Shada, (39 years, Dandenong, 4 children) for example, decided she would wean her children according to Lebanese practices and discontinued MCHN visits after 12 months:
I have had children for 15 years… In my country I start feeding my children at 3 months… But here they are told, no you can't do this, maybe after 6 months or 8 months…. I feel like I have experience, you know more than nurse.
Parents believed that a family history of developmental or health problems constituted a genetic risk and meant they became watchful of their children's health and development. There were frequent references to a personal or family history of vision problems such as ‘squint’ and ‘short sight’, height variations, speech delay, dental health and medical conditions such as asthma.
I suppose in terms of having reduced hearing through glue ear, both their dad and I have had it, so I suppose I was fairly conscious and they were both late talkers and with [my son] I was talking about it at his 18 month maternal health nurse check‐up. (Alison, 37 years, Westgate, 2 children)
Alongside family history, a culture of awareness for the timing of immunizations, maternal child health checks and kindergarten requisites was created through social relationships. This was an important personal resource that ‘enabled’ parents to acquire knowledge of services. Parents of young children sought relationships with other families with similarly aged children and consciously or instinctively checked their child's development against other children. Parents also expected childcare agencies to help them with monitoring, and in this data set, professionals who flagged potential problems to parents were MCHNs (3), kindergarten teachers (3), primary school teachers (3) and childcare workers (1).
I suppose because they're at childcare 3 days a week, seeing them there, and we go to playgroup, and we interact with other children's parents, so I can sort of gauge that they're doing okay. (Vanessa, 39 years, Bayside, 2 children)
They had a couple of hours once a week at occasional care and then a couple of hours at kinder so from that point of view their developmental levels were monitored from those sort of organisations. (Justine, 42 years, Bayside, 3 children)
Social influences played a significant role in uncovering a developmental delay. Parents consulted books and searched Websites and blogs to determine the likelihood of a problem, then corroborated their uncertainties with other significant individuals before taking the next step. However, parents were cognisant of being labelled ‘overanxious’.
I had a friend over, and I said, ‘Does she look a little bit cross‐eyed?’ And we were looking at her and it didn't seem all that noticeable again. And then the next day my husband and I were watching her, and she would look cross‐eyed from time to time, but then it would sort of correct itself. So I rang the maternal health nurse and got an appointment for her. (Jenny, 32 years, Westgate, 2 children)
Health behaviour and parents' personal health practices
This group of parents was already engaged with preventive health services and recognized the value of healthy lifestyles. Mothers (20/28) stated that they attended their GP for pap smears or blood tests, and two had undertaken personal health checks. All children had been vaccinated, and parents talked about exercise and healthy eating as their responsibilities. They talked of difficulties counteracting a busy lifestyle and moderating fast food, and friendships and peer groups were regarded as important for their child's social and emotional well‐being.
How parents sought health care for themselves influenced the choices they made on behalf of their children. Six of seven parents who used complementary and alternative medicine (CAM) administered it to their children, believing that the practice would ‘strengthen their immune system’. Some parents used vegetables or herbs familiar from their cultural background. One parent who regularly received acupuncture, chiropractic services and Chinese herbal medicines did not have a regular GP and had chosen to ‘homoeopathically vaccinate’ her children, terminating MCHN visits after 18 months:
The information I was getting from them was stuff that I could already see in my child and we're a tall family, so they were always at the top end of the percentile and …I guess for me, my belief was that they are just a set of figures. I believed that they were well and growing well. (Natalie, 39 years, Bayside, 2 children)
Parents' satisfaction with the health service and continuity of care
Satisfaction with health services affected the likelihood of continued engagement. Mixed results were obtained in relation to satisfaction with MCHN services. Many parents expressed high levels of satisfaction with the ‘light‐hearted’ environment and time allocated for appointments. Parents were comfortable asking for advice and described nurses as helpful, supportive and caring. Those who retained MCHN services through the preschool years alluded to the continuity of the relationship, the skill set of the nurse and how she handled the children, and the environmental ambience, including rooms geared for children and availability of promotional materials such as books and CDs.
Parents expected that in return for the efforts they made to attend routine health checks, the nurse would address their individual concerns and not just check developmental items. There was significant dissatisfaction when this expectation was not met.
I've always been very careful with my follow‐ups. The last one I did probably last year, his four year old follow‐up, and that was extremely basic. I was quite disappointed with it because I remember taking my daughter…she had to build blocks, she had to do this, she had to do that ‐ there was quite a few different steps that they ran through with her…[This time]she said ‘Did I have any concerns?’ and I said I'm just a bit worried about his pronunciation. She said ‘Oh no, that'll come with time’. And basically it was weigh him, measure him and out the door. (Virginia, 43 years, Westgate, 2 children)
The use of checklists was regarded as ‘superficial’ and ‘base level stuff’, and one parent articulated that a ‘good’ MCHN should ask ‘curious questions’ to probe responses made on a checklist more deeply. If parents felt that the check was basic, they did not feel there was anything to be gained by continuing to attend MCHN checks.
I've never ever felt that anything that they've asked wouldn't be obvious, would highlight anything anyway. I think that's another reason I probably don't go back very often. I don't sort of think anybody tries too much if you like. (Ella, 39 years, Bayside, 2 children)
Parents were also generally satisfied with their GP but pointed out significant differences between GP and MCHN child health services: practitioner availability of time and type of health care. Appointments with GPs were shorter and attendance usually involved a sick child with an acute health problem. Overall, parents lacked knowledge of preventive services offered by GPs, except for immunization services (50 per cent of participants). They could neither recall receiving routine preventive services for children nor asking the GP for advice or support with developmental issues.
I'm from that generation that kind of don't want to bother the doctor in some respects… He's literally on a needs must basis, when they're sick we go to the GP. I wouldn't even seek advice from my GP… I wouldn't go and say I'm really struggling with my children, I'm not sure if I can cope with them. (Rebecca, 38 years, Bayside, 3 children)
When prompted to consider specific aspects of preventive health care for children, parents recalled their GP had measured their child, but thought this was to calculate a drug dose not to monitor growth. Four parents said their child had received a health check from the GP with their immunization at 4 years. Two families were offered HKCs by GPs, but declined invitations as these clinics were not their regular point of care. Only one parent specifically requested a health check for her child, although her experience suggested the clinic doctor did not know about HKCs and included a blood test (not a routine part of the check).
As older siblings transitioned from the MCHN to the GP, parents looked for convenience with appointments and streamlined the family's health care.
Then if there were any other kinds of issues they would be able to deal with them on the spot rather than me having to be referred on …to see a doctor… You know, kill two birds with one stone I suppose. And if there had to be prescriptions done or anything like that then you could do it. (Angela, 47 years, Bayside, 3 children)
As a result, younger children were more likely to miss preventive care visits.
Immunisation, I've been struggling with that for the last 6 months… It's just a scheduling problem, remembering to do it.… just for the third child, I think it's just life with three kids and it's quite challenging. (Julia, 41 years, Westgate, 3 children)
And as attendances for acute health issues accumulated, a feeling of continuity of care with the GP developed, as the scheduled MCHN visits declined.
I'm familiar with the doctor, there's a relationship there and I honestly don't know who I'd see if I went down to the maternal child health centre tomorrow.
Financial barriers to preventive health services
Parents from all three socio‐economic areas cited cost and frequency of GP visits with small children, including the cost of medications, specialist visits, pathology services, allied and dental services, as potential barriers to health care, including preventive services. Whilst parents prioritized their children's health care, privately billed services were frequently beyond their reach, and resorting to public services meant children experienced delays accessing speech pathology, occupational therapy and psychological services.
Maternal and child health services are free at the point of service, whereas GP services are usually privately billed, with some of the costs rebated by the Australian Government insurance scheme, Medicare. Some practices offer direct billed (bulk‐billed) services, paid to the practitioner at a lower rate than the government scheduled fee, so that the patient does not incur out of pocket expenses. Amongst this group of parents, most (20/28) actively sought ‘bulk‐billed’ services for their children. All families from the Dandenong area (low socio‐economic, CALD community) were receiving health care that was direct billed. The four HKCs obtained appear to have been billed in this manner. Some parents prioritized continuity of care over cost, particularly for chronic health‐care issues.
Actually there are two [GPs] that I use, one does bulk billing for children, they tend to be a bit more inconsistent in terms of who the doctor is there, but that's okay for straight forward sort of illnesses…. And then there is another one… that I would probably categorise as the long‐term treatment one. So that's who I go to for [my daughter's] asthma… She's very good… very approachable… and has a nice calm manner about her. Yeah she's great. But you know she's also $65 a visit. (Justine, 42 years, Bayside, 3 children)
Dental services, which are generally privately billed and not rebated by Medicare, were a major source of financial anxiety to parents across each study area. One parent lamented that she could not afford to complete her daughter's orthodontic work and could not access treatment for her 4‐year‐old son's severe dental caries. In contrast, optometrists were well regarded for the fact that assessments were both comprehensive and ‘bulk billed’.
Discussion and recommendations
Through the application of Andersen's behavioural theory, our study clarifies parents' intentions to undertake health checks for their children and presents the social context through which parents recognize and act upon developmental concerns.
Parents in this data set were personally engaged in a range of preventive services and actively monitored their children's health with regards to diet, exercise, growth and social well‐being. All parents had immunized their children, and only one had not accessed maternal child health services. Child preventive health care was influenced by health beliefs and personal health practices. Considerable overlap between these two domains existed in relation to cultural background. These findings resonated with earlier studies which showed parental beliefs about: the use of complementary medicines,56 the timing of routine visits,46 and immunization,57 all affected preventive health‐care uptake for their children. Our study also revealed the significance parents assigned to family history when it came to anticipating problems.
Parents had good knowledge of the schedule of maternal and child health visits. Nevertheless, a quarter of our sample had ceased to visit the MCHN by the child's second year. Arguably the number of preventive visits – 16 in total – proved onerous for many families, especially where there was more than one child and siblings were older. As older siblings switched from the MCHN to the GP, parents sought to streamline health care, so that younger children were less likely to complete MCHN visits. These data correlate well with quantitative studies which have shown that having older siblings increases the risk of non‐adherence to the schedule of preventive child health examinations.41 Parent's beliefs in their own capabilities influenced this transition as did the need for expediency. The GP administered HKC goes some way towards increasing flexibility of preventive health‐care services to children, with practitioners ideally placed to tap into family history and cultural beliefs. Future developments could increase this service beyond the current single time point for its delivery.
Anomalies in children's health were initially picked up in home, kindergarten, school and childcare settings. Having an environment in which parents could compare their children's development was an important determinant of parents' help‐seeking. Parents expected agencies routinely involved with their children to help them monitor development and often discussed concerns with these professionals first. This hierarchy of information seeking serves as a reminder to health professionals to thoroughly evaluate parents' concerns when they are raised. A major goal of the Australian Government is to have a more effective early childhood development system with coordinated, interdisciplinary, flexible services that can refer to early intervention services.58 This could be augmented by ‘Medicare Locals’, primary health‐care organizations recently established in Australia to better respond to local health care needs and connect GPs and other health services.59 These organizations are ideally placed to foster liaisons between GPs and early childhood education and care, to integrate services and streamline referral processes.
Our study also highlighted the absence of routine preventive health services for children from general practice. Parents generally took their children to the doctors when they were sick, did not realize GPs had a stake in preventive health care for children and were reluctant to make appointments for non‐specific concerns. Developmental problems were not presented to the GP, and although parents were aware that GPs weighed children, they believed this was to calculate a drug dose and not to monitor growth; however, national guidelines suggest that GPs should measure BMI twice a year for their paediatric populations.60 Only one parent had specifically requested a HKC, despite them being available for the last 3 years, and few parents had even heard of them. The mismatch between government expectations for the delivery of preventive care and actual receipt was also a major finding with adult preventive care in general practice (where the focus of consultations was also acute care) and holds major implications for putting prevention into practice.61
Parents regarded continuity of care, both with MCHN and GP services, as important. Parents were unlikely to accept health checks from practices that were not the regular source of health care and considered that their child's cooperation was dependent upon familiarity with the practice and the practitioner. Adult patients who regularly attend one practice report greater provision of preventive care.62 Continuity of care may prove to be an important determinant of the quality of preventive health care for children in Australia, as it has overseas63, 64, 65, and policies that encourage continuity (e.g. increased insurance rebates for enrolment with a nominated provider) have previously been considered for other population groups.66
Parents expected health checks for their children to be delivered without incurring costs to them. Although some parents were paying part of the costs of acute GP care, most actively sought bulk‐billed services, which are usually available in metropolitan Melbourne. The situation could be quite different in rural and remote regions of Australia. Mazza et al.61 have shown that many Australian adult patients cannot afford the costs associated with GP preventive care consultations, and this is likely to be the case for child health checks. Whilst general practitioners are incentivized to provide bulk‐billed services to children ($5.90 additional rebate67), practitioners bemoan the widening gap between the costs of delivering good quality general practice services and poor indexation of the Medicare Benefits Schedule.68 A firm commitment to providing primary health care to children may need to revise such incentives. The costs of dental services for children and restricted access to allied health and other specialist services also need to be addressed if children are to achieve optimal health before commencing formal education.
Conclusion
In July 2011, at the completion of data collection, there was a change in government policy that targeted underprivileged children. Changes to rules surrounding Family Tax Benefits, meant that families with a child turning 4 years old, who received an income support payment, must complete a health check with the GP or MCHN to qualify for the benefit.69 This is likely to increase parent demand for health checks, and follow‐up research needs to be conducted to determine whether provision of HKCs has changed.
The strengths of this study include the theoretical underpinnings of the research and methodological rigour. We also strove to seek the opinion of parents from culturally diverse backgrounds (N = 10), typically a group more difficult to reach, and this was a community‐based sample with only one participant obtained from a (maternal and child) health service. We did not explore the views of parents in rural areas where parents may have had different experiences of child preventive health care. Participants who volunteered for this study did not include younger‐aged parents or families where both parents worked full time, and only one father took part. It is also likely that this group of parents were healthier than average and that they were more engaged with preventive health services. The comments made in this study would be typical of many parents, however, and may, in fact, represent the ‘tip of the iceberg’, as we could expect these groups to experience additional barriers. Future research could target the opinions of these groups of parents, could target more single parents and fathers and could be repeated across different areas of Australia.
Additional research could also address inter‐professional relationships at the community level to better understand how developmental concerns, which present to agencies outside of health care, can be expedited. This would build a more complete picture of child preventive health care and is an important step when child health is so dependent on parent–professional relationships. An evaluation of the outcomes of health checks for children would give substance to the drive for parents to attend professional childhood developmental assessments, but the introduction of the HKC is a positive first step towards increasing access through extension of services into general practice.
Conflict of interest
None.
Source of funding
This work was funded by the Shepherd Foundation, Malvern, Victoria, Australia. The funding body had no involvement in the conduct of the research.
Acknowledgements
Playgroup Victoria for help with recruitment of parents.
References
- 1. Barker DJP. The developmental origins of adult disease. Journal of the American College of Nutrition., 2004; 23: 588S–595S. [DOI] [PubMed] [Google Scholar]
- 2. Lau C, Rogers JM. Embryonic and fetal programming of physiological disorders in adulthood. Birth Defects Research Part C, Embryo Today: Reviews, 2004; 72: 300–312. [DOI] [PubMed] [Google Scholar]
- 3. Felitti VJ, Anda RF, Nordenberg D et al Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine., 1998; 14: 245–258. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization . Social Determinants of Health: The Solid Facts. Copenhagen, Denmark: WHO, 2003. [Google Scholar]
- 5. Belli PC, Bustreo F, Preker A. Investing in children's health: what are the economic benefits? Bulletin of the World Health Organization., 2005; 83: 777–784. [PMC free article] [PubMed] [Google Scholar]
- 6. Nutbeam D. Health Promotion Glossary. Geneva: World Health Organization, 1998. [Google Scholar]
- 7. Kuo AA, Inkelas M, Lotstein DS, Samson KM, Schor EL, Halfon N. Rethinking well‐child care in the United States: an international comparison. Pediatrics, 2006; 118: 1692–1702. [DOI] [PubMed] [Google Scholar]
- 8. Australian Institute of Health and Welfare (AIHW) . A Picture of Australia's Children. Canberra: AIHW, 2009. [Google Scholar]
- 9. Australian Government . A Snapshot of Early Childhood Development in Australia 2012 – AEDI National Report. Canberra: Australian Government, 2013. [Google Scholar]
- 10. AIHW . Headline Indicators for Children's Health, Development and Wellbeing. Canberra: AIHW, 2011. [Google Scholar]
- 11. Wake M, Hardy P, Canterford L, Sawyer M, Carlin JB. Overweight, obesity and girth of Australian preschoolers: prevalence and socio‐economic correlates. International Journal of Obesity, 2007; 31: 1044–1051. [DOI] [PubMed] [Google Scholar]
- 12. Chrisopoulos S, Harford JE. Oral Health and Dental Care in Australia: Key Facts and Figures 2012. Dental statistics and research series 60. Cat. no. DEN 224. Canberra: AIHW, 2013. [Google Scholar]
- 13. Robinson M, Oddy WH, Li J et al. Pre‐ and postnatal influences on preschool mental health: a large‐scale cohort study. Journal of Child Psychology and Psychiatry, 2008; 49: 1118–1128. [DOI] [PubMed] [Google Scholar]
- 14. Department of Health and Ageing . Building a 21st Century Primary Health Care System: Australia's First National Primary Health Care Strategy. Publications number: 6594. Canberra: Commonwealth of Australia, 2010. [Google Scholar]
- 15. Roxon N. Taking leadership‐ tackling Australia's health challenges. Medical Journal of Australia., 2007; 187: 493–495. [DOI] [PubMed] [Google Scholar]
- 16. Department of Education and Early Childhood Development . Your Maternal and Child Health Service Visits. Melbourne: State Government Victoria, 2006. [Google Scholar]
- 17. Moore T, Grove C. Best Practice Guidelines for Parental Involvement in Monitoring and Assessing Young Children. Victorian Government: Department of Education and Early Childhood Development, 2008. [Google Scholar]
- 18. Shepherd ML. Behind the scales: child and family health nurses taking care of women's emotional wellbeing. Contemporary Nurse, 2011; 37: 137–148. [DOI] [PubMed] [Google Scholar]
- 19. Rowe HJ, Fisher JR, Loh WM. The Edinburgh Postnatal Depression Scale detects but does not distinguish anxiety disorders from depression in mothers of infants. Archives of Women's Mental Health, 2008; 11: 103–108. [DOI] [PubMed] [Google Scholar]
- 20. Kemp L, Harris E, McMahon C et al Benefits of psychosocial intervention and continuity of care by child and family health nurses in the pre‐ and postnatal period: process evaluation. Journal of Advanced Nursing., 2012. doi: 10.1111/jan.12052 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 21. Hampshire AJ, Blair ME, Crown NS, Avery AJ, Brackenbury PB, Williams EI. Is pre‐school child health surveillance an effective means of detecting key physical abnormalities? British Journal of General Practice., 1999; 49: 630–633. [Google Scholar]
- 22. Magnusson M, Persson K, Sundelin C. The effectiveness of routine health examinations at 2, 6, 9 and 12 months of age: experiences based on data from a Swedish county. Child Care Health and Development, 2001; 27: 117–131. [DOI] [PubMed] [Google Scholar]
- 23. Tebruegge M, Nandini V, Ritchie J. Does routine child health surveillance contribute to the early detection of children with pervasive developmental disorders? An epidemiological study in Kent, U.K. BMC Pediatrics, 2004; 4: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Skovgaard AM, Houmann T, Christiansen E et al Can a general health surveillance between birth and 10 months identify children with mental disorder at 1 1/2 year? A case‐control study nested in cohort CCC 2000. European Child & Adolescent Psychiatry., 2008; 17: 290–298. [DOI] [PubMed] [Google Scholar]
- 25. Royal Australian College of General Practitioners . Standards for General Practices, 4th edn Melbourne, Australia: The Royal Australian College of General Practitioners, 2010. [Google Scholar]
- 26. Australian Government: Department of Health and Ageing (DoHA) . Medicare Benefits Schedule (MBS) Healthy Kids Check Fact Sheet. 2008.
- 27. Medicare Australia . Medicare Item Reports. Australian Government, 2011. [Google Scholar]
- 28. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of Health & Social Behavior., 1995; 36: 1–10. [PubMed] [Google Scholar]
- 29. Aday LA, Andersen RM. A framework for the study of access to medical care. Health Services Research., 1974; 9: 208–220. [PMC free article] [PubMed] [Google Scholar]
- 30. Hulka BS, Wheat JR. Patterns of utilization‐ the patient's perspective. Medical Care., 1985; 23: 438–460. [DOI] [PubMed] [Google Scholar]
- 31. Leigh WA, Lillie‐Blanton M, Martinez RM, Collins KS. Managed care in three states: experiences of low‐income African Americans and hispanics. Inquiry‐The Journal of Health Care Organization Provision and Financing, 1999; 36: 318–331. [PubMed] [Google Scholar]
- 32. Go VFL, Quan VM, Chung A, Zenilman J, Hanh VTM, Celentano D. Gender gaps, gender traps: sexual identity and vulnerability to sexually transmitted diseases among women in Vietnam. Social Science & Medicine., 2002; 55: 467–481. [DOI] [PubMed] [Google Scholar]
- 33. Honda K. Factors underlying variation in receipt of physician advice on diet and exercise: applications of the behavioral model of health care utilization. American Journal of Health Promotion, 2004; 18: 370–377. [DOI] [PubMed] [Google Scholar]
- 34. Lopez‐Cevallos DF, Chi C. Health care utilization in Ecuador: a multilevel analysis of socio‐economic determinants and inequality issues. Health Policy and Planning, 2010; 25: 209–218. [DOI] [PubMed] [Google Scholar]
- 35. Wu T. A culturally sensitive health care practice model ‐ Theory construction and its testing. American Journal of Chinese Medicine., 2004; 32: 467–485. [DOI] [PubMed] [Google Scholar]
- 36. Goh SN. Post acute care of the elderly in Singapore what factors influence use of services? Asia Pacific Journal of Social Work and Development, 2011; 21: 31–53. [Google Scholar]
- 37. Ndao‐Brumblay SK, Green CR. Predictors of complementary and alternative medicine use in chronic pain patients. Pain Medicine, 2010; 11: 16–24. [DOI] [PubMed] [Google Scholar]
- 38. Salinas JJ, Al Snih S, Markides K, Ray LA, Angel RJ. The rural‐urban divide: health services utilization among older Mexicans in Mexico. Journal of Rural Health, 2010; 26: 333–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hurwicz M‐L, Bercanovic E. Do elderly Medicare recipients contact physicians appropriately? Journal of Gerontology, 2002; 57B: S187–S194. [DOI] [PubMed] [Google Scholar]
- 40. Davidson PL, Andersen RM, Wyn R, Brown ER. A framework for evaluating safety‐net and other community‐level factors on access for low‐income populations. Inquiry‐The Journal of Health Care Organization Provision and Financing, 2004; 41: 21–38. [DOI] [PubMed] [Google Scholar]
- 41. Sondergaard G, Biering‐Sorensen S, Michelsen SI, Schnor O, Andersen AM. Non‐participation in preventive child health examinations at the general practitioner in Denmark: a register‐based study. Scandinavian Journal of Primary Health Care., 2008; 26: 5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gorman BK, Braverman J. Family structure differences in health care utilization among U.S. children. Social Science & Medicine., 2008; 67: 1766–1775. [DOI] [PubMed] [Google Scholar]
- 43. Cohen AL, Christakis DA. Primary language of parent is associated with disparities in pediatric preventive care. Journal of Pediatrics., 2006; 148: 254–258. [DOI] [PubMed] [Google Scholar]
- 44. Buescher PA, Horton SJ, Devaney BL et al Differences in use of health services between white and African American children enrolled in Medicaid in North Carolina. Maternal and Child Health Journal., 2003; 7: 45–52. [DOI] [PubMed] [Google Scholar]
- 45. Amen MM, Clarke VP. The influence of mothers' health beliefs on use of preventive child health care services and mothers' perception of children's health status. Issues in Comprehensive Pediatric Nursing, 2001; 24: 153–163. [DOI] [PubMed] [Google Scholar]
- 46. Hughes SC, Wingard DL. Parental beliefs and children's receipt of preventive care: another piece of the puzzle? Health Services Research., 2008; 43: 287–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lantican L. Health service utilization and perceptions of mental health care among Mexican American women in a U.S.‐Mexico border city: a pilot study. Hispanic Health Care International, 2006; 4: 79–88. [Google Scholar]
- 48. Andrasik MP, Rose R, Pereira D, Antoni M. Barriers to cervical cancer screening among low‐income HIV‐positive African American women. Journal of Health Care for the Poor and Underserved., 2008; 19: 912–925. [DOI] [PubMed] [Google Scholar]
- 49. Ben‐Isaac E, Schrager SM, Keefer M, Chen AY. National profile of nonemergent pediatric emergency department visits. Pediatrics, 2010; 125: 454–459. [DOI] [PubMed] [Google Scholar]
- 50. Wallace A, Scott J, Klinnert M, Anderson ME. Impoverished children with asthma: a pilot study of urban healthcare access. Journal for Specialists in Pediatric Nursing, 2004; 9: 50–58. [DOI] [PubMed] [Google Scholar]
- 51. Henderson S, Kendall E. Culturally and linguistically diverse peoples' knowledge of accessibility and utilisation of health services: exploring the need for improvement in health service delivery. Australian Journal of Primary Health, 2011; 17: 195–201. [DOI] [PubMed] [Google Scholar]
- 52. Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods, 2006; 18: 59–82. [Google Scholar]
- 53. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology, 2006; 3: 77–101. [Google Scholar]
- 54. Green J, Willis K, Hughes E et al Generating best evidence from qualitative research: the role of data analysis. Australian and New Zealand Journal of Public Health., 2007; 31: 545–550. [DOI] [PubMed] [Google Scholar]
- 55. NVivo qualitative data analysis software. QSR International Pty Ltd.Version 8; 2008.
- 56. Fong LK, Fong DP. Usage of complementary medicine among children. Australian family physician., 2002; 31: 388–391. [PubMed] [Google Scholar]
- 57. Lawrence GL, Hull BP, MacIntyre CR, McIntyre PB. Reasons for incomplete immunisation among Australian children. A national survey of parents. Australian family physician., 2004; 33: 568–571. [PubMed] [Google Scholar]
- 58. Council of Australian Governments . Investing in the Early Years—A National Early Childhood Development Strategy. Canberra: ACT, Department of Education Employment and Workplace relations, 2009. [Google Scholar]
- 59. Davies PK. Divisions of General Practice: will they transform, or die? Medical Journal of Australia., 2010; 193: 75–77. [DOI] [PubMed] [Google Scholar]
- 60. National Health and Medical Research Council . Clinical Practice Guidelines for the Management of Overweight and Obesity in Children and Adolescents. Commonwealth of Australia: Canberra, 2003. [Google Scholar]
- 61. Mazza D, Shand LK, Warren N, Keleher H, Browning CJ, Bruce EJ. General practice and preventive health care: a view through the eyes of community members. Medical Journal of Australia., 2011; 195: 180–183. [DOI] [PubMed] [Google Scholar]
- 62. Steven ID, Dickens E, Thomas SA, Browning C, Eckerman E. Preventive care and continuity of attendance. Is there a risk? Australian family physician., 1998; 27(Suppl 1): S44–S46. [PubMed] [Google Scholar]
- 63. Chung PJ, Lee TC, Morrison JL, Schuster MA. Preventive care for children in the United States: quality and barriers. Annual Review of Public Health, 2006; 27: 491–515. [DOI] [PubMed] [Google Scholar]
- 64. Flores AI, Bilker WB, Alessandrini EA. Effects of continuity of care in infancy on receipt of lead, anemia, and tuberculosis screening. Pediatrics, 2008; 121: E399–E406. [DOI] [PubMed] [Google Scholar]
- 65. DeVoe JE, Tillotson CJ, Wallace LS, Lesko SE, Pandhi N. Is health insurance enough? A usual source of care may be more important to ensure a child receives preventive health counseling. Maternal and Child Health Journal., 2012; 16: 306–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. National Health and Hospitals Reform Commission . A Healthier Future For All Australians‐Final Report. 2009. [DOI] [PubMed]
- 67. Department of Health and Ageing . Medicare Benefits Schedule Online. Australian Government, 2012.
- 68. Australian Medical Association . AMA Gaps Poster. 2011.
- 69. Australian Government Department of Human Services . Healthy Start for School Initiative. 2011.


