Abstract
Objectives
To assess patient preferences for different models of care defined by location of care, frequency of care and principal carer within community‐based health‐care services for older people.
Design
Discrete choice experiment administered within a face‐to‐face interview.
Setting
An intermediate care service in a large city within the United Kingdom.
Participants
The projected sample size was calculated to be 200; however, 77 patients were recruited to the study. The subjects had recently been discharged from hospital and were living at home and were receiving short‐term care by a publicly funded intermediate care service.
Interventions
Not applicable.
Main Outcome Measure
The degree of preference, measured using single utility score, for individual service characteristics presented within a series of potential care packages.
Results
Location of care was the dominant service characteristics with care at home being the strongly stated preference when compared with outpatient care (0.003), hospital care (<0.001) and nursing home care (<0.001) relative to home care, although this was less pronounced among less sick patients. Additionally, the respondents indicated a dislike for very frequent care contacts. No particular type of professional carer background was universally preferred but, unsurprisingly, there was evidence that sick patients showed a preference for nurse‐led care.
Conclusions
Patients have clear preferences for the location for their care and were able to state preferences between different care packages when their ideal service was not available. Service providers can use this information to assess which models of care are most preferred within resource constraints.
Keywords: allied health, assistants, community rehabilitation services, conjoint analysis, intermediate care, models of care, outcomes, patient preference, staff, support workers
In the developed world, the growing ageing population and increasing prevalence of chronic conditions have triggered a need to consider reorientation of health‐care systems from acute hospital‐based services to services which are provided in the community and focused on the management of long‐term conditions. Therefore, there is much interest in community‐based services for older people that assist transitions between care settings, avoid hospital use completely, and those which reduce hospital use by managing the interface or patient transition between hospital inpatient and community‐based care.
Intermediate care, a form of transition care in the United Kingdom (UK), is a government funded initiative that is free to all at the point of delivery. It is designed to prevent acute hospital admissions, facilitate early discharge and reduce admissions to long‐term care for older people. More recently, the focus has also been on greater streamlining of care for older people in the community. The model of intermediate care in the UK was directly shaped by government guidance outlined in the National Service Framework for Older People.1 This document defined intermediate care as a multifaceted service for those aged 65 or over covering transitions between hospital and home, including (but not limited to) supported discharge services, hospital avoidance services, residential rehabilitation and day hospitals. The Framework advised that these services were to be delivered by teams of doctors, allied health professionals/therapists (physiotherapists, occupational therapists, speech and language therapists, etc.), nurses and support workers/assistants. Following this guidance, the number and type of intermediate care services have grown in number and been configured in many different ways.2
A key driver for the implementation of intermediate care was to improve care pathways and experiences for older people.3 However, older peoples' preferences for care have not been examined in this context despite further government investment promoting consideration of patient preferences and placing the patient at the centre of service development.4
It is recognized that it has been hard to effect a change towards more patient‐centred care as traditional health‐care delivery has been largely defined and dominated by established professional groups.5 The delivery of patient‐centred care requires a workforce that is responsive to patient needs, rather than practitioners who are constrained by distinct role profiles. It is now well accepted that some forms of care can be delivered by more than one type of practitioner. This has been demonstrated in the UK, and elsewhere, where policies and programmes to address workforce shortages have resulted in the development of a range of new flexible models of workforce development and delivery.6, 7, 8
The workforce involved in caring for older people is undergoing substantial changes internationally. For instance, within community‐based older peoples' services, vertical and horizontal substitution is evident in role overlap between nurses, allied health practitioners and social care providers and through the delegation of a range of tasks to the rapidly growing support worker personnel.9, 10, 11 The potential to provide care in a range of different settings, including hospital, nursing homes, the patient's own home; and using a range of technologies, further impacts on the way that care is provided, and on the hierarchies and interactions between workers.9
A systematic review of the ‘Evidence for the effectiveness of intermediate care’3 found that the evidence supporting the development, structure and organization of specific intermediate care services is quite heterogeneous, and still lacking. Others have identified a need for more research regarding strategies to promote effective involvement of patients in decision making regarding their care.4, 5
Previous research has demonstrated large variations in the way that intermediate care services are provided.13 The majority of care is provided in the patient's own home; however, it can also be provided in community‐based facilities and dedicated hospital beds. The number and types of staffing vary greatly, as does the intensity of care provision. To date, there is no evidence of the ‘best’ way to deliver or organize intermediate care services. Nor is there any evidence on the preferences of service users on their desired configurations of care.
This study used a discrete choice experiment (DCE) approach (also known as conjoint analysis) to examine patient preferences. The DCE approach has been used widely in health services research to investigate a range of service issues.12 With this approach, preferences are determined by asking respondents to choose their preferred option between two different service configurations referred to as ‘pairwise choices’. This process is repeated with further pairs describing different service configurations. With sufficient data, it is possible to develop models that describe the impact of specific characteristics on patient preferences for different types of more complex service configurations. This regression model (or ‘utility function’) measures the relative importance of different service characteristics which allows trade‐off to be quantified on a single scale.
The aim of this study was to explore patient preferences for different configurations of care packages within an intermediate care service within a large city in the UK. For the purpose of this study, intermediate care is defined as non‐acute, time‐limited services that are designed to increase the independence of older people. This project was part of a broader programme of research that incorporated several studies to examine the impact of different workforce models on patient, staffing and service outcomes. The study reported here examined patient preferences for staffing and service intensity, whilst other components of the study looked at actual staffing models in relation to patient and staff outcomes.13, 14, 15
Methods
Study design
When developing the pairwise choices within a DCE, three design issues need to be considered. Firstly, the service characteristics of interest were identified. The three service characteristics identified for this study were based on a review of policy documents and research related to skills mix issues in intermediate care.15, 16 These were location of care, frequency of care, and principal caregiver. The degree of multidisciplinary working was also considered as another service characteristic that would be relevant to this research area; however, this was not added as we failed to develop a meaningful way of describing this characteristic within the confines of the DCE.
Secondly, levels are assigned to the characteristics so that they can be described in terms appropriate to the patient population and the policy question. The levels used in this study were ‘home’, ‘hospital’, ‘outpatients’ and ‘nursing home’, for location of care; ‘once per week’, ‘3 times per week’, ‘7 times per week’ and ‘15 times per week’, for frequency of care; and ‘support worker’, ‘nurse’, ‘therapist’ and ‘doctor’, for the principal carer. For the purpose of this study, the term ‘therapist’ refers to a physiotherapist, dietician, podiatrist, speech and language therapist, social worker or other manifestation of the term ‘therapist’ that the participant related to in terms of their caregiver.
Thirdly, different service configurations were identified in order to make a set of choices. This subset of service configurations were identified using an orthogonal array (Oa16.5.4.2) which identifies 16 service configurations.17 Pairings, or choice sets, were created using the minimal overlap approach identified in previous work.18 Giving answers to all sixteen choice sets was considered to be too taxing for some patients in the proposed sample, and so, the set of choices was split into two groups of 8 choices. An example of one choice set is shown in Table 1.
Table 1.
One possible choice of service configurationsa
| Type of care A | OR | Type of care B |
|---|---|---|
| Care own home, with | Care in hospital, with | |
| Contact once per week, and | Contact 15 times per week, and | |
| A support worker delivering most of your care | A doctor delivering most of your care |
Each card contains three components relating to place of care, frequency of care and the practitioner who provides the care. For each card shown, participants must pick whether the prefer type A or type B or ‘don't know’.
The interview schedule
The interview started with questions to elicit the patient characteristics, their use of services, their level of care needs as assessed by a therapist and measured on a 9‐point ordinal scale as a proxy for the severity of patient illness and to identify potential patient groups based on their level of service requirement,19 their degree of functioning as measured by the Therapy Outcome Measures Scale (TOMS)20 and their health‐related quality of life as measured by the EQ‐5D (formerly the Euro‐Qol).21
The TOMS is a therapist‐rated outcome measure used principally within rehabilitation.20 It contains four dimensions based on the World Health Organizations International Classification of Functioning22 describing care needs in relation to impairment, activity, social participation and well‐being. Each dimension is scored on an 11‐point scale (0–5, including half‐points). Lower scores indicate higher levels of impairment. The EQ‐5D is a simple, patient completed, generic quality‐of‐life measure with five domains, each described via a single question with three response categories. For this study, it serves as a summary measure of health‐related quality of life, ranging from 1 indicating full health to −0.6 indicating worst possible health.21
Prior to the choice sets, three questions asked the respondent how they rated the importance of the three dimensions of care on a four‐point response scale ranging from ‘very important’ to ‘not important’. Patients were then asked which type of therapist they would prefer from a choice of physiotherapist, dietician, podiatrist, speech and language therapist, social worker or other. From this information, the interviewer personalized the patient's preferred choice of therapist in the pairwise choices. This personalization of health‐care worker removed the possibility of the therapist being irrelevant to the respondent's care and thereby making the choice meaningless.
Following the discrete choice experiment, two further questions were asked to determine whether the experiment was fully understood by the respondents. Finally, the participant was asked ‘did they miss out any aspects of your care that you feel important? If yes, what are they?’ Furthermore, although participants were not formally invited to ask questions during the interview, the interviewer clarified any questions that did arise and this was recorded.
Two versions of the interview schedule were produced, each with eight separate choice sets. These two versions were randomly allocated to patients.
Participants and recruitment
Participants were current patients of an intermediate care service within a large city. The study received ethical approved from the local research ethics committee (ethics approval number 07/Q2305/45). The ethical considerations for this study were equity of participation, the risks of respondent burden and/or distress, maintaining participant confidentiality, and the consideration of the trade‐off of the risks versus the benefits to the participants. Due to the complexity of the study design and the questions, patients who were unable to communicate in English or had severe cognitive impairment were excluded from the study. Cognitive ability was assessed by the patient's ability to complete informed consent, and this was judged in advance by a professional member of staff who was familiar with the patient.
Sample size
A target of 200 patients was set. Sample size calculations based on anticipated effect sizes, or any other rules, have not been produced by previous applications of DCEs. A review of recent studies showed that sample sizes for interview‐based studies generally range from 50 to 300 respondents.23, 24, 25, 26, 27 Larger studies have been untaken, but these tend to be when postal questionnaires are the source of data and when more scenarios need to be evaluated.28 The sample size of 200 was therefore larger than some previous studies, but was thought necessary given likely missing data rates in the patient population and the need for subgroup analyses.
Data analysis
The data from the DCE were analysed using a random effects probit model within STATA, which estimates the impact of each attribute on the probability of ‘B’ being chosen. Probit regression is similar to logistic regression which is more widely used in multivariate analyses of probabilities. The key difference is that the two approaches relate to difference shaped distributions between 0 and 1. However, both share the general properties of the coefficients being non‐linearly related to the estimated probability with their signs and magnitudes reflecting the direction and relative size of any relationship. Consequently, the estimated coefficients indicate the importance of the different attributes on individual preferences. A positive sign on a coefficient indicates that as the level of the attribute increases so does the utility derived and vice versa. As a secondary analysis, differences in the preferences between patient subgroups were tested. The subgroups examined were service needs, health‐related quality of life (as measured by the EQ5D) and care needs (as measured by the TOMs).
Results
Only 77 interviews were undertaken, short of the target of 200 interviews. The principal reasons for this were a delay in research governance approval, a lack of patients being referred through to the study from some of the teams and a block on undertaking interviews within day care facilities over concerns that it would interfere with the smooth running of the services. However, all patients responded to at least one set of choices with only 31 of a total of 616 choices being coded as ‘don't know’, which includes any reason for a choice not being made.
The sociodemographic characteristics of the sample are described in Table 2. A large majority of the sample were over the age of 70, with a small majority over the age of 80, and 62% were female. The sample had generally poor health as measured by the EQ‐5D, with only four patients scoring over 0.8 (where one is full health and zero represents a health state considered by the general population to be equally preferable to being dead). Seven patients had negative scores, which represent health state considered by the general population to be worse than death.
Table 2.
Sociodemographic characteristics of the sample
| Characteristic | Type | Proportion (%) |
|---|---|---|
| Gender | Male | 37.7 |
| Age | <70 | 9.1 |
| 70–79 | 37.7 | |
| 80–89 | 48.0 | |
| 90+ | 5.2 | |
| EQ‐5D | <0 | 9.1 |
| 0–0.39 | 13.0 | |
| 0.4–0.69 | 54.5 | |
| 0.7–1 | 23.4 |
Current care requirements of the sample are described in Table 3. The most common level of care category suggested that the patients required a prevention and or maintenance programme (49%). Very few patients had very specific, complex care (levels of care 5–8). The majority of patients received their care at outpatient or day hospital visits. Only 42% of patients received care more than once per week through contacts with health professionals although 10% received more than 14 contacts per week. Therapists were the principal professional carer for around two‐thirds of the sample, with support workers being the principal carer for a quarter, and <10% of patients receiving the bulk of their care from either nurses or doctors.
Table 3.
Current care of the sample
| Characteristic | Type | Proportion (%) |
|---|---|---|
| Level of care | Client does not need any intervention | 6.5 |
| Client needs prevention/maintenance | 49.4 | |
| Client needs convalescence/respite | 1.3 | |
| Client needs slow stream rehabilitation | 1.3 | |
| Client needs regular rehabilitation | 28.6 | |
| Client needs intensive rehabilitation | 2.6 | |
| Client needs specific treatment for individual acute disability | 7.8 | |
| Client needs medical care and rehabilitation | 1.3 | |
| Client needs rehabilitation for complex disabling condition | 1.3 | |
| Place of care | At home | 23.4 |
| Outpatient visits/day hospital | 75.3 | |
| Nursing home | 1.3 | |
| Frequency of care | 0–1 contacts per week | 58.4 |
| 1.1–7 contacts per week | 24.7 | |
| 7.1–14 contacts per week | 6.5 | |
| >14 contacts per week | 10.4 | |
| Principal carer | Support worker | 23.4 |
| Nurse | 5.2 | |
| Therapist | 67.5 | |
| Doctor | 2.6 |
When asked to rate the importance of the different aspects of care that were used to derive the choice sets within the DCE (Table 4), it appears that location of care is the most important consideration. Frequency of care and type of carer appears less important, although still 80–90% of patients rated this as quite or very important.
Table 4.
Importance of different aspects of care
| Aspect of care | Very important | Quite important | Little importance | Not important |
|---|---|---|---|---|
| Location | 72.7 | 24.7 | 1.3 | 1.3 |
| Frequency | 58.4 | 31.2 | 7.8 | 2.6 |
| Type of carer | 58.4 | 20.8 | 18.2 | 2.6 |
Prior to the multivariate analysis of the choice data, which forms the central part of a DCE, we undertook a simple univariate analysis by identifying the proportion of times that a choice favoured an individual characteristic of a service regardless of the other characteristics. Figure 1 shows that for location of care, ‘home’ appears to be clearly favoured, with hospital and residential care preferred least.
Figure 1.
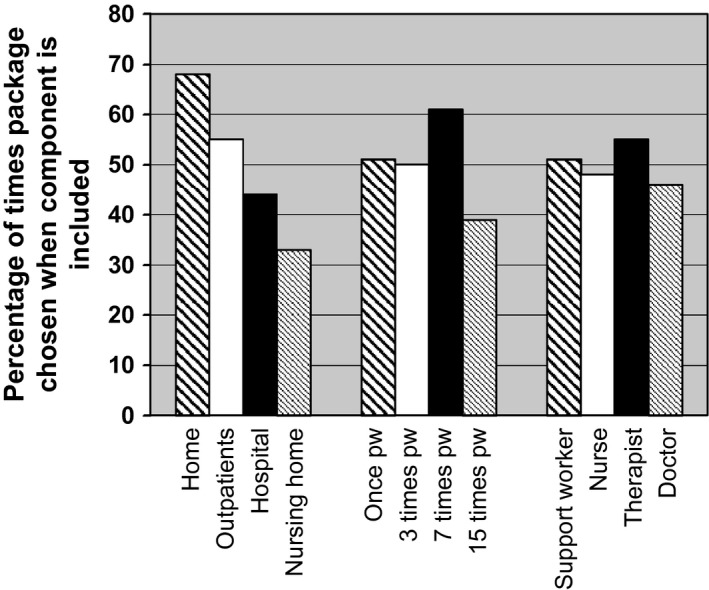
Impact of service component on patients’ choices.
The regression analysis shows a clearer picture (Table 5). For the full sample, home‐based care is the most preferred as all other locations (which are measured relative to home care) have negative and statistically significant coefficients. Hospital and residential care have the largest negative impact on patient preference and have P‐values <0.001. The most intensive form of therapy, with 15 contacts per week, is least preferred, and this is statistically significant. No other aspects of care have a statistically significant effect on preference. The subgroup analyses are generally supportive of these results, but with a few noticeable alterations.
Table 5.
Regression results of the pairwise comparisonsa
| All respondents | P‐value | EQ5D > 0.5 | P‐value | EQ5D < 0.5 | P‐value | Any TOMS < 3 | P‐value | All TOMS ≥ 3 | P‐value | LoC < 2 | P‐value | LoC > 1 | P‐value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Home | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – |
| Outpatients | −0.39 | 0.003 | −0.24 | 0.095 | −1.00 | 0.002 | −0.30 | 0.125 | −0.69 | <0.001 | −0.42 | 0.073 | −0.35 | 0.015 |
| Hospital | −0.77 | <0.001 | −0.64 | <0.001 | −1.18 | 0.002 | −0.32 | 0.143 | −1.27 | <0.001 | −1.02 | 0.038 | −0.48 | <0.001 |
| Nursing home | −0.95 | <0.001 | −0.80 | <0.001 | −1.72 | <0.001 | −0.73 | 0.000 | −1.35 | <0.001 | −1.01 | <0.001 | −0.91 | <0.001 |
| 1 contact pw | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – |
| 3 contacts pw | 0.02 | 0.869 | −0.1 | 0.927 | 0.14 | 0.674 | 0.01 | 0.942 | −0.06 | 0.730 | 0.09 | 0.765 | −0.06 | 0.578 |
| 7 contacts pw | 0.03 | 0.792 | −0.6 | 0.666 | 0.61 | 0.068 | 0.18 | 0.360 | −0.14 | 0.407 | 0.09 | 0.895 | −0.02 | 0.611 |
| 15 contacts pw | −0.28 | 0.018 | −0.34 | 0.009 | 0.02 | 0.938 | −0.16 | 0.367 | −0.48 | 0.005 | −0.14 | 0.015 | −0.42 | 0.365 |
| Support worker | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – | 0.00 | – |
| Nurse | 0.22 | 0.241 | 0.08 | 0.711 | 1.06 | 0.039 | 0.33 | 0.220 | 0.10 | 0.708 | 0.24 | 0.501 | 0.19 | 0.334 |
| Therapist | 0.27 | 0.295 | 0.20 | 0.498 | 0.65 | 0.293 | 0.43 | 0.234 | 0.02 | 0.955 | 0.51 | 0.958 | −0.02 | 0.140 |
| Doctor | 0.08 | 0.701 | −0.01 | 0.962 | 0.42 | 0.369 | 0.28 | 0.324 | −0.23 | 0.460 | 0.25 | 0.691 | −0.12 | 0.361 |
All parameters are relative to a baseline package of care at home, once per week and with the principal carer being a support worker, which by definition have a coefficient of zero and can have no P‐value. Negative coefficients suggest that the variable is less preferred than relevant component of the baseline package, and positive coefficients suggest that the variable is more preferred.
Using the estimated regression equations, we can calculate the mean utility of the sample for each combination of care characteristics. With four levels for each of the three care characteristics, 64 possible care packages can be defined. A selected set of care packages are listed in Table 6 in rank order.
Table 6.
Rankings of selected care packages
| Location | Frequencya (pw) | Principal carer | Linear predicted value (LPV)b | 95% confidence interval of LPV | Rankc |
|---|---|---|---|---|---|
| Home | 7 | Therapist | 0.30 | −0.27 to 0.88 | 1 |
| Home | 3 | Support worker | 0.02 | −0.22 to 0.27 | 11 |
| Outpatients | 7 | Therapist | −0.09 | −0.78 to 0.61 | 15 |
| Outpatients | 1 | Nurse | −0.17 | −0.63 to 0.29 | 20 |
| Home | 15 | Doctor | −0.20 | −0.71 to 0.31 | 21 |
| Outpatients | 15 | Doctor | −0.59 | −1.22 to 0.05 | 37 |
| Residential home | 1 | Therapist | −0.69 | −1.28 to −0.09 | 43 |
| Hospital | 15 | Nurse | −0.83 | −1.25 to −0.40 | 52 |
| Residential home | 15 | Support worker | −1.23 | −1.60 to −0.86 | 64 |
pw = Per week.
The linear predicted value is produced using the probit coefficients from the all respondent results in Table 5. Higher values represent more preferred scenarios. The upper and lower limits for this study are 0.3 and −1.23.
1 = best, 64 = worst.
At the end of the interview, patients were asked to assess their difficulty in answering the questions. 5% found the questions to be ‘very hard’, 22% ‘hard’ 26% ‘okay’, 29% ‘easy’ and 18% ‘very easy’. Likewise, when asked whether the descriptions of care seemed sensible, 18% thought them to be ‘very sensible’, 29% ‘moderately sensible’, 34% ‘okay’ 15% ‘not sensible’ and 4% thought they ‘made ‘no sense’.
Discussion
The DCE shows that whilst all aspects of care impact on the preferences of patients receiving intermediate care, location of care was the most important with care at home being most preferred, with residential home and hospital care least preferred. Given that the need to move care ‘closer to home’ is a key underpinning policy assumption that has driven the growth of intermediate care in the UK, this is an important finding.1 It is interesting to note that patients did not demonstrate an overwhelming desire to have frequent contacts, particularly among the healthier patients who appear to want contact with health professionals no more than once per week. There was strong evidence that intensive therapy (>15 contacts per week) was not a desirable option. The subgroup analysis suggests only small variations in preferences for services associated with health and care needs of the patient. This finding has important implications for the interdisciplinary provision of home‐based services to reduce the need for multiple providers to deliver different components of care. In other words, where there is the option for a single health‐care provider to address multiple health‐care needs, this is preferable to allowing several different service providers to enter the patient's home.
Perhaps, the greatest strength of the DCE approach is reflected in Table 6, which illustrates how preferences for care packages are not ‘all‐or‐nothing’. This shows that whilst there was a strong preference for care at home, respondents were willing to trade this off if other aspects of care were available at other locations. For example, daily outpatient therapy from a therapist was preferable to home care with twice daily contact with a doctor (rankings 15 and 21, respectively), although this difference was not statistically significant at the 5% level. From a service provider's perspective, this is important, as it shows that even with constraints on some aspects of the service, for example the staffing of home care, patient satisfaction could potentially be maintained by providing a different type of care in an alternative setting.
The results suggest that patients have no clear preferences for different types of staff. This reinforces the existing literature about patient preferences for different types of health‐care providers in community‐based rehabilitation. For example, in evaluations of the introduction of assistant practitioner roles, patients often have difficulty distinguishing between different staff types and generally express no specific preferences for specific staff as long as the practitioner is appropriately trained, supported and competent.11, 29
From a provider and service perspective, a wide range of skills are required to meet the disparate care needs of this patient group. Therefore, it makes sense that a smaller number of practitioners are trained to deliver the range of roles, rather than imposing a large, multidisciplinary team on an individual. This approach is consistent with the introduction of generic assistant practitioners and the blurring of role boundaries seen in some intermediate care settings.9
Study limitations
This is a heterogeneous client group, and thus, we are disappointed that we were only able to recruit 77 subjects particularly given that our estimated power calculation was for 200. However, even with this number, it remains one of the largest con joint analysis studies in this field.
One surprise was the lack of any clear pattern relating to the preferences for the professional group of the principal professional carer. Only in the subgroup of sick patients (EQ5D < 0.5) was there a statistically significant relationship with preference which in this group was to have nursing care. This possibly reflects the diverse mix of needs and preferences among the respondents, even when subgroups were examined. It may also reflect a genuine lack of understanding of the roles of different employed caregivers and as such the ability to discern between and hence have a preference for specific professions. For example, patients often struggle to identify the difference between qualified and support staff particularly as they age.30 This may be particularly difficult in this setting, given the frequent blurring of professional boundaries within the intermediate care workforce.
Other reasons for the lack of a clearer picture should also be considered. Firstly, the sample was heterogeneous in terms of disabilities and care needs, and as such, ‘unclear’ preferences for staff across the sample may be masking strong, yet conflicting, preferences among subgroups. This issue could also pertain to the groups that were not included in the study, specifically people who were excluded because the study was unable to address their communication requirements, whether cognitive or linguistic. By the nature of their exclusion, these subgroups are likely to have different requirements, and therefore preferences to meet their needs which this methodology was unable to capture.
Intermediate care, by nature, addresses the needs of heterogeneous patients, and to date, there are no commonly accepted ways of classifying patient subgroups within this patient population.2, 13 It is possible that patients with more discrete or more acute health problems may have clearer preferences for service and staffing types. It is equally plausible that in a service that is predominantly community based and designed to restore or optimize function, patients may want the least obtrusive model of care to aid their restoration and recovery, regardless of the type of role. Further research is required to ascertain the relationships between nature and acuity of illness and patient preferences for staffing and service types.
Secondly, a sizeable proportion of respondents found the questions to be hard (26%), or not sensible (20%). This, we interpreted as suggesting that the options were not appropriate for their particular situation. These problems can manifest themselves in two ways: missing data and arbitrary responses. Given the low rates of missing data, it is possible therefore that many responses were arbitrary. Whilst this does not bias the results, it does reduce our ability to identify ‘real’ preferences among the ‘noise’. It is difficult to see how this can be reduced within this patient population; interviews were undertaken to improve the quality of response, and the scenarios were kept simple. It is possible that we oversimplified scenarios such that they were no longer ‘sensible’; however, it is likely that greater complexity would have increased the number of patients considering the questions to be hard. We also limited the number of choice sets given to each respondent to reduce burden. However, this can introduce other problems as intraperson variability is increased and respondents have little opportunity to learn about the elicitation process and potentially generate more accurate responses. Whether more choices could be given to an elderly and frail population, however, is open to question from both research and ethical perspectives.
Finally, the lack of a clear picture with regard to some of the aspects of care may be due to the sample size. Whilst we had hoped to recruit 200 patients, only 77 were eventually included in the study. This has a direct effect on the power of the study to detect relationships within the data. This highlights a general limitation of discrete choice experiments that is rarely discussed; identifying what is an important difference in preferences and powering the study on identifying those differences is not straightforward. Greater participant numbers would provide more robust findings and subgroup analyses, but it is difficult to estimate what sample size would be sufficient to identify an important difference in preferences for any given power. However, even in the presence of many P‐values above conventional levels of significant, our conclusions identify the overwhelming importance of location of care to this patient group and represent an important starting point for defining patient‐focussed care packages for this group.
Whilst we highlight that the findings are useful when considering service provision, it is clear that the scenarios are simplifications. Consequently, service configurations will include aspects of care that were not considered here, but those patients may have strong views on. For example, within our broader programme of research, we have raised the importance of multidisciplinary working,15 yet we were unable to capture this within the DCE. Even with the simple design, we chose to explore in this study, some unlikely scenarios were generated through the DCE design process, for example doctors visiting patients 14 times per week. We could have mitigated this through a more restricted set of levels within ranges, but this would then have removed important care packages (such as support workers visiting 15 times per week). Clearly, there is a trade‐off between the comprehensiveness of care packages described and the plausibility of the packages that patients are asked to choose between. However, whilst some of the scenarios were unlikely, given that the vast majority of respondents considered the questions to be sensible, we feel that this did not unduly impact on the validity of our findings.
The study was undertaken within a single organization, and the majority of patients were referred from a single team (of a possible six). Clearly, this will not produce generalizable findings beyond the city or even that team. However, given the diversity of intermediate care provision, any study of this type that tries to generate generalizable findings will need to include other dimensions of care so that the full range of care models are described. As we discussed earlier, this will automatically produce more complex pairwise choices which will have the potential to make the interview too difficult for many respondents. More complex research designs may also produce a greater number of unlikely care packages, which may impact on the quality of responses.
This study shows that the DCE approach can be used to identify care packages that allow the quantification of patient preferences. However, fitting these data into a fuller evaluation of intermediate care services incorporating costs, patient outcomes and issues relating to workforce dynamics (e.g. team working) remain challenging.15
The key questions to answer in further research are the degree to which a more complex DCE is necessary that takes into consideration other aspects of the care packages offered, and the way in which the DCE results can be combined with cost and outcome data to identify the most cost‐effective service configuration that meets the diverse care needs seen across patient populations.
Conclusions
The DCE interview captured data on a wide range of patients, with varying health and care needs. Whilst some patients found the choice questions to be hard, all patients were able to answer some, and overall missing data rates were low. The results show that the most important aspect of care is the location, with home care the most preferred option. Some variations are seen among subgroups, with healthier patients preferring less intensive care or support. There is little evidence for one type of principal carer over another.
Funding
The work was funded by the United Kingdom National Institute for Health Research via its Service Delivery and Organisation research programme (grant 08/1519/95).
References
- 1. Department of Health . The National Service Framework for Older People. London: Department of Health, 2001. [Google Scholar]
- 2. Martin G, Peet S, Hewitt G, Parker H. Diversity in intermediate care. Health and Social Care in the Community, 2004; 12: 150–154. [DOI] [PubMed] [Google Scholar]
- 3. Audit Commission . Living Well in Later Life. A Review of Progress Against the National Service Framework for Older People. London: Commission for Healthcare Audit and Inspection, 2006. [Google Scholar]
- 4. Department of Health . HSC 2000/011: LAC 2000/10 Implementation of the Health Act Partnership Arrangements. London: Department of Health, 2000. [Google Scholar]
- 5. Larkin GV. Occupational Monopoly and Modern Medicine. London: Tavistock, 1983. [Google Scholar]
- 6. Department of Health . The NHS Plan. A Plan for Investment. A Plan for Reform. London: Department of Health, 2000. [Google Scholar]
- 7. Department of Health . Shifting the Balance of Power: the Next Steps. London: Department of Health, 2002. [Google Scholar]
- 8. Department of Health . Delivering the NHS Plan: Next Steps on Investment, Next Steps on Reform. London: Department of Health, 2002. [Google Scholar]
- 9. Nancarrow S. Dynamic role boundaries in intermediate care services. Journal of Interprofessional Care, 2004; 18: 141–151. [DOI] [PubMed] [Google Scholar]
- 10. Nancarrow S. The impact of intermediate care services on job satisfaction, skills and career development opportunities. Journal of Clinical Nursing, 2007; 16: 1222–1229. [DOI] [PubMed] [Google Scholar]
- 11. Moran AM, Nancarrow SA, Wiseman L et al Assisting role redesign: a qualitative evaluation of the implementation of a podiatry assistant role to a community health setting utilising a traineeship approach. Journal of Foot and Ankle Research, 2012; 5: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. British Medical Journal, 2000; 320: 1530–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nancarrow S, Moran A, Freeman J et al Looking inside the black box of community rehabilitation and intermediate care teams in the United Kingdom: an audit of service and staffing configuration. Quality in Primary Care, 2009; 17: 323–333. [PubMed] [Google Scholar]
- 14. Dixon S, Kaambwa B, Nancarrow S, Martin GP, Bryan S. The relationship between staff skill mix, costs and outcomes in intermediate care services. BMC Health Services Research, 2010; 10: 221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nancarrow S, Moran A, Enderby P et al The Relationship Between Workforce Flexibility and the Costs and Outcomes of Older Peoples Services. London: National Institute of Health Research, National Institute of Health Research SDaOP, 2010. [Google Scholar]
- 16. Nancarrow SA, Moran AM, Parker SG. Understanding service context: development of a service pro forma to describe and measure elderly peoples' community and intermediate care services. Health & Social Care in the Community, 2009; 17: 434–446. [DOI] [PubMed] [Google Scholar]
- 17. Sloane N. A library of orthogonal arrays. 2007, Available at: http://www2.research.att.com/∼njas/oadir, accessed 22 June 2007.
- 18. Street DJ, Burgess L, Louviere JJ. Quick and easy choice sets: constructing optimal and nearly optimal stated choice experiments. International Journal of Research in Marketing, 2005; 22: 459–470. [Google Scholar]
- 19. Enderby P, Stevenson J. What is intermediate care? looking at needs. Managing Community Care, 2000; 8: 35–40. [Google Scholar]
- 20. Enderby P, John A, Petherham B. Therapy Outcome Measures for Rehabilitation Professionals. 2nd edn. Enderby P, John A, Petherham B. (eds) Chichester: John Wiley and Sons Ltd; 2006. [Google Scholar]
- 21. Dolan P. Modelling valuations for EuroQol health states. Medical Care, 1997; 35: 1095–1108. [DOI] [PubMed] [Google Scholar]
- 22. World Health Organisation . International Classification of Functional Disability and Health. Geneva: World Health Organisation, 2001. [Google Scholar]
- 23. Johansson G, Stallberg B, Tornling G et al Asthma treatment preference study: a conjoint analysis of preferred drug treatments. Chest, 2004; 125: 916–923. [DOI] [PubMed] [Google Scholar]
- 24. Ratcliffe J. The use of conjoint analysis to elicit willingness‐to‐pay values. Proceed with caution? International Journal of Technology Assessment in Health Care, 2000; 16: 270–275. [DOI] [PubMed] [Google Scholar]
- 25. Ross MA, Avery AJ, Foss AJE. Views of older people on cataract surgery options: an assessment of preferences by conjoint analysis. Quality and Safety in Health Care, 2003; 12: 13–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bishop AJ, Marteau TM, Armstrong D et al Woman and health care professionals' preferences for Down's Syndrome screening tests: a conjoint analysis. British Journal of Obstetrics and Gynaecology, 2004; 111: 775–779. [DOI] [PubMed] [Google Scholar]
- 27. Sassi F, McDaid D, Ricciardi W. Conjoint analysis of preferences for cardiac risk assessment in primary care. International Journal of Technology Assessment in Health Care, 2005; 21: 211–218. [PubMed] [Google Scholar]
- 28. Bech M, Sorensen J, Lauridsen J. Eliciting women's preferences for a training program in breast self‐examination: a conjoint analysis ranking experiment. Value in Health, 2005; 8: 479. [DOI] [PubMed] [Google Scholar]
- 29. Nancarrow S, Mackey H. The introduction and evaluation of an occupational therapy assistant practitioner. Australian Occupational Therapy Journal, 2005; 52: 293–301. [Google Scholar]
- 30. Lange J. Nurses and assistive personnel: do patients know the difference? Journal of Nursing Administration, 2000; 30: 512–514. [DOI] [PubMed] [Google Scholar]


