Abstract
Background
Shunts, the main treatment for hydrocephalus, are problematic because they frequently malfunction. Detecting shunt malfunction is challenging because symptoms are similar to those of common childhood illnesses, particularly viral infections. Parents are responsible for identifying shunt malfunction and responding accordingly. Understanding parents' experiences has the potential to improve parent–professional collaboration and the management of the child's condition.
Aim
To explore parents' experiences of living with a child with hydrocephalus and their decisions when they suspect shunt malfunction.
Design and methods
A cross‐sectional interview‐based survey using qualitative methods was undertaken. Twenty‐five parents participated in the interviews. Framework approach underpinned data analysis.
Findings
Three concepts, ‘uncertainty’, ‘developing expertise’, and ‘a normal life’, were identified. These concepts were dynamic in nature as parents learned through experience, adapted to changes in their child's health status and made decisions about their needs. Uncertainty because of the unpredictability and life‐threatening nature of shunt malfunction dominated parents' accounts. Through experience, parents learned to differentiate between symptoms that suggested a shunt problem and those of other childhood illnesses, but perceived their expertise was not always valued by health professionals or used to inform clinical decisions. Decisions about where or when to seek advice related to prior experiences of health‐care services and minimizing disruption for the whole family.
Conclusion
Parents can recognize illness symptoms suggestive of shunt malfunction and want to collaborate with health professionals about the management of their child's condition. Collaboration with parents requires health professionals to listen to parents' concerns and value their experiences.
Keywords: children, collaboration, hydrocephalus, parents' experiences, shunts
Background
Hydrocephalus is a long‐term condition, normally identified in early childhood, where there is excessive fluid in the ventricular system within the brain. Increased cerebrospinal fluid levels cause ventricular enlargement resulting in compression and destruction of adjacent structures which affects brain growth and development. Seventy percent of children with hydrocephalus are managed by the insertion of a ventricular shunt, which diverts excessive fluid from the ventricles to another body compartment, commonly the peritoneum.1, 2 Shunts are prone to malfunctioning; failure rates are in the region of 40–50% within the first year of placement.3, 4 Prompt identification and treatment of shunt malfunction is necessary to avoid permanent neurological impairments or death.5, 6, 7, 8
Parents are responsible for recognizing the symptoms of potential shunt malfunction in their child, which are unpredictable, variable and similar to those of common childhood illnesses, particularly viral infections.5, 7, 9, 10 Parents need to make a judgment about whether these non‐specific symptoms require attendance at a hospital for a diagnostic scan of shunt malfunction or watchful waiting at home. Assessing a child for possible shunt malfunction requires health professionals to listen to, and value parents' concerns.7, 10 However, health professionals often perceive parents' assessment of their child's condition to be inaccurate contributing to avoidable hospital admissions.8, 10 Understanding parents' experiences of living with a child with hydrocephalus is essential in understanding their decisions about where and when to seek health‐care advice for suspected shunt malfunction.
Study aims
To understand parents' experiences and perceptions of living with a child with shunted hydrocephalus. The specific objectives were to:
Investigate how parents learn about shunt management and associated complications;
Explore parents' decision making about seeking specialist treatment when their child has symptoms associated with shunt malfunction.
Participant recruitment
A purposeful sampling strategy using predetermined inclusion criteria ensured a range of conditions associated with hydrocephalus were included. The common causes of hydrocephalus are congenital anatomical brain defects, intraventricular haemorrhage associated with premature births and complications of meningitis.1, 11 Parents were recruited from a regional children's neurosciences ward within a United Kingdom National Health Service acute hospital trust and the local branch of a national support group for individuals with spina bifida and hydrocephalus [Spina Bifida Hydrocephalus Information Networking Equality (SHINE)]. In qualitative research, it is not possible, nor desirable, to predict precise sample sizes at the start of a study. This is not problematic because data collection and preliminary analysis occur simultaneously guiding the final sample size. Data saturation, where no new issues emerged during the interviews, was achieved at 12 interviews. A further three interviews were undertaken because these parents had been recruited and subsequent analysis confirmed data saturation had been achieved.
Study design and methods
A cross‐sectional interview‐based survey employing qualitative methods was undertaken in order to explore the breadth and depth of parents' experiences. Data were collected between September 2006 and September 2007. Semi‐structured interviews using a topic guide ensured the interview remained focused on meeting the study objectives (Table 1). Interviews were undertaken per household, sometimes involving one parent sometimes both parents, in response to real‐world contexts and recognizing parents shared responsibility for decisions about their child's care.
Table 1.
Interview topic guide
| Guiding questions |
|---|
| Building up the depth of questions |
|
Describing experiences
Would you describe your family? How did you find out your child had hydrocephalus? What were you told about hydrocephalus when your child was first diagnosed? What were you told about the treatment of your child's hydrocephalus? Can you explain how shunts were explained to you? Were you given an opportunity to discuss shunts with anyone else? What do you remember as being helpful when you were getting all this information? What do you remember as being unhelpful when you were getting this information? |
|
Knowledge of hydrocephalus
Before your child was diagnosed with hydrocephalus, had you heard of the condition? Can you explain why your child has hydrocephalus? Would you describe what you know about the treatments for hydrocephalus? How did you explain your child's hydrocephalus to family or friends? What have you told/will you tell your child about hydrocephalus? |
|
Making decisions about illness symptoms
Will you describe when your child was last ill? (What sort of symptoms did your child have?) Did you worry that the illness may be related to the shunt? (Why was that? What did you do? What advice were you given? How did you feel?) If your child is ill, how do you know if it is a problem with the shunt or not? (What particular symptoms are you looking for?) Can you remember an occasion when your child was ill and you thought it was a shunt problem, but it wasn't? (What did you do? What happened? How did you feel?) |
|
Feelings about impact of hydrocephalus for the child and family
Will you describe how you felt at the time your child was diagnosed with hydrocephalus? How do you feel hydrocephalus has affected, if at all, aspects of your child's life? How do you feel your child's hydrocephalus has affected the rest of the family? What worries, if any, do you have about your child having a shunt? How do you feel about your child having a shunt? Have you heard of any occasions when other parents thought everything was OK, but their child had a problem with the shunt? (Can you think of any reasons this happen?) Thinking about everyday life, do you make any extra considerations because your child has a shunt? (If so in what ways?) Do you have any thoughts or worries about your child caring for themselves in the future? |
|
Concluding questions
Suppose a group of health‐care staff were trying to decide the best way to support parents who have a child with a shunt, what would you recommend? Do you have anything you wish to add? |
The framework approach underpinned data analysis.12 Although the approach enabled data to be explored systematically, the analytical processes were iterative and involved forward and backward movement across the stages of data management, descriptive accounts and explanatory accounts. Application of the framework approach and transparency of the data analysis in relation to this study have been published elsewhere.13 The unit of analysis was the interview, either with couples or with one parent depending on whether both parents participated. The qualitative software program NVivo® version 2 (QSR International, Doncaster, Victoria, Australia) was used to assist data management.
A range of strategies enhanced the validity and reliability of the findings. Following the interviews, a focus group consisting of four participants, two parents who had participated in the interviews and two SHINE advisors, was undertaken to ascertain whether the findings provided a recognizable and authentic account of living with a child with hydrocephalus. Other techniques included seeking out similarities and differences across participants’ accounts prior to developing final themes and using rich extracts of parents' accounts enabling judgments to be made credibility of themes and concepts.14, 15
Local research ethics committee and site‐specific approval from the local research and development department were obtained (LREC reference AB/44233/1C/442 + 33/60145/1). Consent was obtained prior to the commencement of the interview. There was potential that the nature of some of the questions could cause distress; systems were in place to refer parents to the senior ward sister, SHINE advisor or consultant neurologist if required.
A limitation of the study was that participants did not reflect the diverse minority‐ethnic communities within UK society. The personal experiences of JS (principle researcher) had the potential to influence the study findings. However, the rigorous application of the framework approach, and debating and agreeing final themes and concepts between all authors ensured findings were an accurate representation of parents' accounts.
Findings
Twenty‐five parents participated in the study, comprising of ten couples (all male/female) and five mothers. Parent and child characteristics are presented in Table 2. Three overarching concepts emerged from the analysis of parents' accounts of their experiences and were labelled; ‘uncertainty’, ‘developing expertise’ and ‘a normal life’. These concepts and associated themes are presented in Table 3, and are described below using data extracts to illustrate each theme.
Table 2.
Participant characteristics
| Parents' characteristics | Total (n = 25) |
|---|---|
| Gender male: female | 10:15 |
| Age (years) | Mean 38.3: range 21–52 |
| 21–30 | 2 |
| 31–40 | 12 |
| 41–50 | 9 |
| Above 50 | 2 |
| Highest qualification | |
| A levels or above | 13 |
| GCSE | 10 |
| None | 2 |
| Socio‐economic classificationa | |
| 1 | 0 |
| 2–4 | 13 |
| 5–7 | 6 |
| 8 | 6 |
| Ethic group: White British | 25 |
| Number of children | Mean 2: range 1–5 |
| 1 | 6 |
| 2 | 7 |
| 3 or above | 2 |
| Child characteristics | Total (n = 15) |
|---|---|
| Gender male: female | 8:7 |
| Age (years) | Mean 6.7: range 2–13 |
| Under 5 | 7 |
| 6–10 | 5 |
| 11–15 | 3 |
| Age at diagnosis | |
| Prenatal | 5 |
| Neonate (<1 month) | 7 |
| 1–4 months | 3 |
| Reason for hydrocephalus | |
| Intraventricular haemorrhage | 7 |
| Spina bifida | 5 |
| Aqueduct stenosis | 2 |
| Post meningitis | 1 |
| Associated conditionsb | |
| Epilepsy | 5 |
| Cerebral palsy | 2 |
| Hearing impairments | 2 |
| Other | 2 |
| None | 5 |
| Shunt revisions | Mean 1.7: range 0–4 |
| 0 | 3 |
| 1 | 4 |
| 2 | 3 |
| 3 + | 5 |
| Type of school/nursery | |
| Mainstream | 9 |
| Mainstream + support | 5 |
| Special school | 1 |
UK National Statistics Socio‐economic Classification.
One child had both cerebral palsy and epilepsy.
Table 3.
Core concepts and themes
| Core concepts | Themes |
|---|---|
| Uncertainty | Reactions to child's diagnosis |
| Concerns about the shunt | |
| Receptiveness of professionals to interacting with the family | |
| The child's future | |
| Developing expertise | Making sense of hydrocephalus |
| Differentiating between childhood illness and shunt malfunction | |
| Understanding support organizations | |
| A normal life | Barriers and facilitators to normal family life |
| Balancing normality with watchfulness | |
| Valuing normal life |
Uncertainty
Uncertainty was a constant part of daily life and dominated parents' accounts of living with a child with hydrocephalus. The concept labelled uncertainty was underpinned by four themes: reactions to child's diagnosis, concerns about the shunt, receptiveness of professionals to interacting with the family, and the child's future (Table 3).
Reactions to child's diagnosis
The most common reaction to receiving their child's diagnosis was shock and the fear of brain damage; these reactions were heightened by parents' uncertainty about their ability to cope with living with a child with a long‐term condition, and the impact on family life. The following extracts illustrate parents' emotions and uncertainties at the time of diagnosis:
Well I remember feeling, like to me I felt the whole world had collapsed. It was quite scary really wasn't it, because we didn't know how it was going to affect him. We were thinking that we wouldn't be able to do things that other families would be able to do. Family 12 mum, child 4 years
‘I did worry how I would cope’. Family 11 dad, child 5 years
‘I found that he had spina bifida…and they just kept monitoring (for hydrocephalus) until he was born and they would just have to see how severe it was… so I'm really in a state, I wasn't really sure because you know they kept saying, the doctors, that he might have brain damage’. Family 1 mum, child 3 years
Concerns about the shunt
A dominant feature of daily life related to the uncertain, unpredictable and life‐threatening nature of shunt complications. Consequently, being able to recognize shunt malfunction was a significant feature of parents' accounts, and a source of stress and anxiety. Additional concerns about the shunt included possible revisions as their child grew, risks associated with surgery and whether the shunt would be permanent throughout adulthood. Ways of coping with shunt malfunction included being constantly vigilant for illness symptoms that might indicate a problem with the shunt, seeking advice from health‐care professionals and trying not to dwell on potential shunt malfunction. The following extracts summarize parents' feelings and concerns about shunts:
‘To me it is stressful because it is twenty‐four hours a day, you know in another couple of hours things could change and we could be over in (city). It's stressful and you know it could all go wrong again …at the end of the day he could die from a blocked shunt’. Family 2 mum, child 8 years
‘You are thinking is he going to be alright when he comes out (of surgery) or is he going to come out or whatever. You really are thinking is he going to be coming back. You just totally don't know’. Family 12 dad, child aged 4 years
Receptiveness of professionals to interacting with the family
Parents wanted to develop effective relationships with health professionals, teachers and SHINE advisors. parents' perceived some professionals were unwilling to engage in in‐depth discussions about their child's needs and restricted the information shared with parents. Parents were unsure about the best way to engage with health professionals and contribute to care decisions. Parents described having to be an advocate for their child, for example, emphasizing changes, in their child, which are likely to indicate a problem with the shunt or suggesting ways their child's learning needs could be better met. The following extracts summarize parents' accounts of interactions with professionals:
‘In clinic, we were saying well how does it (scan) compare to the last scans. He (the doctor) didn't really want to talk about it’. Family 15 mum (dad interrupts)
‘No he didn't seem interested… we want to know about (child's) hydrocephalus, so to do that we need to have a look at scans … I am sure if someone explained it we could really understand and get some knowledge. It's not as though we're stupid’. Family 15 dad, child 5 years
‘I think the label ‘uncertainty’ is really appropriate and really sums up what it is like. But it is not just about doctors’ and teachers’ experience or I suppose knowledge is it. I remember having a lot of uncertainty when (child) went up to seniors, he was used to the school in the village and teachers and children know him and are tolerant of him. I was concerned about the response he would get in a large school and would the teachers understand his needs when they have so many other children. But they have been marvellous and it's not just about their knowledge but how they respond to having a child like (child) in the school’. Family 8 dad, child 11 years
‘I know there is something wrong. She (doctor) said we will see how he goes. I said “look he needs to be looked at”. I said I have been patient, I know what you see is not what the books tell you but please do something. So they said they would scan him… he is under pressure it's blocked. And I said I know that, I have been saying this all day’. Family 14 mum, child 12 years
Concerns about their child's future
Uncertainties about their child's future included: ability to live independently; developing friendships and forming relationships; managing their own health needs; and participating in every day social activities. Although parents described a range of uncertainties about their child's long‐term future, these concerns appeared to be heightened for parents whose children had complex needs. Mobility and continence related issues were identified as the main barriers to social integration and added to parents' concerns about their child's transition to adulthood. Parents reported trying to balance supporting their child to become independent with being overprotective. Views about their child's future are summarized in the following extracts:
‘The elimination side of things but she is going to have a rough time with other children as she gets older. I think, we anticipate that she will have difficulties…. I imagine she will face obstacles with other children like bullying’. Family 5 mum, child 6 years
‘(Partner) is a bit scared when he first starts going out with his mates …if somebody bangs his head, …you can't not let him go out can you, he will be old enough to do what he wants’. Family 12 dad, child 4 years
‘What is going to happen in the future? He will probably always be going to have to live with us and what is going to happen to him’. Family 8 mum, child 11 years
Developing expertise
Parents are responsible for recognizing and responding to changes in their child that might indicate a problem with the shunt. Developing the expertise to manage their child's condition was associated with three themes; ‘making sense of hydrocephalus’, ‘differentiating bet‐ween childhood illnesses and shunt malfunction’ and ‘understanding support organizations’ (Table 3).
Making sense of hydrocephalus
The emotions experienced on first learning of their child's diagnosis made it difficult for parents' to comprehend information about their child's condition. For parents who had never heard of the condition, grappling with the ‘label’ of hydrocephalus compounded their bewilderment. The quality of information provision was variable. Sometimes information provision met parents' needs, delivered clearly and in a way that demonstrated empathy. In contrast, the amount of information provided was described as overwhelming with overuse of complex medical terminology. Planned educational events hosted by SHINE, where there were opportunities to meet other parents, were described as invaluable. Examples of trying to making sense of hydrocephalus are summarized below:
‘When the word “hydrocephalus” was said to us, it was like a Greek Island. You know, well what is it? What does it mean? And I said why, what's happened?’ Family 3 mum, child 5 years
‘I mean he (GP) worded things so superbly he said she, the water drains into the head, it flows into the head but it is not coming away. You know he gave us a lot of confidence it was all explained quite simply and it does stay with you, those first few explanations do actually stay with you’. Family 7 mum, child 10 years
‘We have found out a lot ourselves on the internet, if we haven't fully understood something from the health‐care professions, then we have been able to look this up further. But I can imagine that if people didn't have access to the internet, or those capabilities, I could see them not getting the information’. Family 11 dad, child 5 years
‘The only thing that we get is from SHINE. If not part of it, you are left to go on your own little merry way’. Family 12 mum, child 4 years
Differentiating between childhood illness and shunt malfunction
The ability to recognize shunt malfunction developed through gaining knowledge about hydrocephalus and its treatment, and experiencing illness episodes in their child including those which were shunt related. The majority of the children had required at least one revision of the shunt, with three or more revisions not uncommon. Consequently, some parents developed considerable expertise in recognizing changes in their child that might suggest shunt malfunction. Parents described a range of situations, where they were able to differentiate between general childhood illnesses and shunt malfunction. However, parents found it difficult to express exactly how they knew illness symptoms were shunt related. Explanations included just knowing the subtle differences between general illnesses and shunt problems and recognizing changes in their child's usual habits and behaviours that were likely to be indicative of a shunt problem and instinct, summarized in the following extracts:
Instinct. ‘Because of her colour, there is just something about her eyes or she will start to use maybe the wrong word, or a bit sluggish in the morning and it just rings bells really…Once she had this flu bug that has been going round…the high temperature, blinding headache and felt sick. Which for her is normal shunt problems, but I just know there are subtle differences’. Family 7 mum, child 10 years
‘Although we had always had problem with food and vomiting, this was different. (Child) had headache, he was crying but it was different to his normal cry, his vomiting was not after feeds as usual, but in the morning and before feeds. He just wasn't right. You think how will you know, but it's your child and you know it is different, a different type of headache’. Family 2 mum, child 8 years
Understanding support organizations
A range of factors influenced parents' decisions in relation to where to seek advice including the degree of certainty that their child's symptoms were suggestive of shunt malfunction or more likely to be general health concerns; previous experiences; health professionals’ familiarity with the child and family; the experience and knowledge health professionals had in relation to children with hydrocephalus; practical issues such as anxieties about driving a sick child to a city a considerable distance away. Although having direct access to the regional children's neurosciences ward was valued by parents and described as an essential safety net, parents living in rural areas were more likely to consult their general practitioner as the first point of contact, summarized in the following extracts:
‘My GP's good, the doctors and the doctors are very good and see her straight away, and if I am struggling and I think it is her shunt, I usually go straight round there’. Family 9 mum, child 2 years
‘We spend quite a lot of the time waiting in (local hospital) for someone to make a decision, which we can do that at home really. We know that if we go to out of hour's service, we will be admitted. So we tend to wait a bit longer in cases where we are unsure. If we were absolutely definite, we go straight to (regional centre)’. Family 12 dad, child 4 years
Although parents could identify the services and support available when their child had acute illness symptoms, identifying services relating to other aspects of their child's needs was variable. Parents of children with complex needs found it difficult to navigate their way round services that might help them meet their child's health and educational needs. Parents highlighted a key worker with detailed understanding of the needs of children with hydrocephalus would be invaluable. The following extracts are examples of the perceived gaps in service provision:
‘There has been no one who has taken ownership of his hydrocephalus or who has been able to answer questions about his longer term issues’. Family 15 dad, child 5 years
‘With the number of consultant appointments and all her educational appointments… a nurse specialist that could pull that care together, I mean (child) has eight consultants who do not work alongside each other’. Family 11 mum, child 5 years
A normal life
Parents described the challenges of striving for and maintaining a normal life whilst being mindful of the chance that a shunt can malfunction at any time. Normal life was associated with two–three themes; barriers and facilitators to normal family life, balancing normality with watchfulness and valuing normal life (Table 3).
Barriers and facilitators to normal family life
Parents' lifestyle choices were often influenced by the needs of their child with hydrocephalus. Undertaking family activities was disrupted because of the frequency of acute hospital admissions; the number and timing of out‐patient appointments; having to be available to respond to health‐related issues while the child was at school; providing care for their child during school hours; lack of social opportunities for themselves and their child, illustrated in the following accounts:
‘We can't do anything, can't plan. Like tomorrow, I mean they're off school, and like today, we have a hospital appointment, we'll do something but we can't plan, so it affects family life. I couldn't work full time. Part‐time is not by choice because of all (child) appointments and obviously if they ring you up from school, I have to come out of work’. Family 4 mum, child 10 years
‘I got a phone call when I was at work, from a teacher at school saying that she had felt a lump on the back of her head but she hasn't banged it and if it is just the shunt and I said well that it's always there. So I had to drive home from work to feel it and confirm to them that is just how the shunt should be even though we had told them previously and shown them where it was in the past so they are on edge about it’. Family 11 Dad, Child aged 5 years
Balancing normality with watchfulness
The life‐threatening nature of shunt malfunction and responsibility for identifying the cause of illness symptoms was, at times, overwhelming. The unpredictable nature of shunt malfunction was described as disruptive and had the potential to dominate family life. Parents were constantly vigilant in relation to detecting shunt malfunction but tried to balance being watchful with continuing usual family activities. Parents described being over cautious when responding to illness symptoms because of a fear of not detecting shunt malfunction. Although parents' expressed guilt about the number of times they accessed health services, others perceived it was acceptable to access health services as a precaution because of the uncertain nature of shunt‐related illness symptoms, illustrated in the following extracts:
‘You have to be a lot more cautious and think a lot more about things, about what you are doing and where you go …. it is a big deal but it's not that big… it is just the way it is’. Family 11 dad (mum interrupts)
‘So I think you are right (partner), we try very hard to let her experience life as any other four‐ or five‐year old. I don't think we minimalize it, I think we respond appropriately but we try not to let it limit (child's) life or ours, or our lives’. Family 11 mum, child 5 years
‘Sometimes you feel like judge, jury and doctor and everything don't you’. Family 12 mum, child 4 years
‘Whenever (child) is ill, we would always think is it the shunt. It's always the first thing, which really it should be, the first thing you think of is, is it the shunt’. Family 11 dad, child 5 years
‘We will take him to the (regional centre) and it won't turn out to be anything serious, I'm fine with that. It's better than the thought of missing it’. Family 15 dad, child 5 years
Valuing normal life
parents' perceived that living with a child with hydrocephalus had similar challenges to bringing up a child without hydrocephalus. Parents described the importance of recognizing their child as an individual with unique strengths and skills, and integrating their child's needs into everyday family life. Parents made considerable efforts to engage in usual family activities such as seeking information about local hospitals before embarking on holidays. Parents identified difficulties in obtaining travel insurance for their child with hydrocephalus. Some parents described taking holidays abroad without travel insurance. For some mothers meeting their child's needs was not compatible with full‐time employment. The following extracts highlight parents' views about parenting a child with hydrocephalus:
‘You know people think hydrocephalus, might think is all bad news. But it's not, there's a lot of reward, for example, a child who has so much against them doing so well’. Family 2 dad, child 8 years
‘See your child as a child first and foremost and look at all the positive things, and be aware that the shunt may or may not have problems, but try and not let it take over your life. It will always be there in the back of your mind, but look on the positive’. Family 2 mum, child 8 years
‘Worrying continually, but you do about all of your children… you worry that they will get in with the wrong crowd and not make good of themselves. But I do worry extra about (child)’. Family 7 mum, child 10 years
Conceptual framework
The conceptual framework presented in Fig. 1 brings together the core concepts and the way parents assimilated and integrated their experiences and knowledge as they gained the expertise to manage their child's condition. A significant feature of living with a child with hydrocephalus was the constant uncertainty associated with the unpredictable nature of shunt malfunction. Consequently, the concepts of ‘uncertainty’, ‘developing expertise’ and ‘a normal life’ were underpinned by the ever‐present shunt‐related concerns. Although shunt‐related concerns dominated parents' accounts, parents tried balancing the vigilance needed to identify signs of shunt malfunction with living a ‘normal’ family life. This was achieved by ‘learning through experience’, ‘adapting to changes in the child’ and ‘making decisions’, and will be explored in the discussion.
Figure 1.
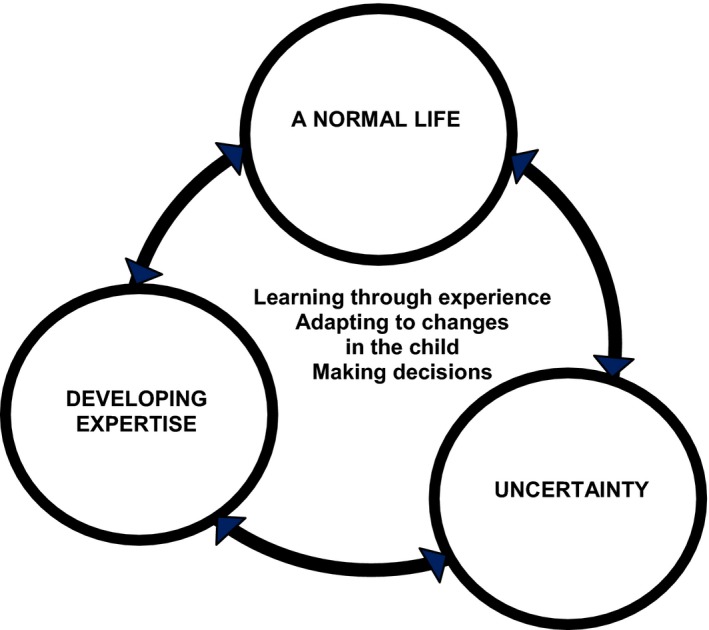
Conceptual framework: dynamic model of living with a child with hydrocephalus.
Discussion
A diagnosis of a long‐term condition is associated with many uncertainties which relate to the diagnosis and its meaning, treatment choices and their effectiveness, long‐term consequences of the condition and future life choices.16, 17 These uncertainties mirrored parents' accounts of living with a child with hydrocephalus. Uncertainty has been identified as a significant psychological stressor for the individual with a long‐term condition and their family.18 A range of theories have attempted to explain the relationship between uncertainty and illness.19 Uncertainty causes a shift in usual functioning which can be reconciled through the process of recognizing, appraising and managing the cause of the uncertainty.20 However, resolving uncertainty is dependent on an individuals’ confidence and their perception of the level of control they have in a given situation.21 Reducing uncertainty involves using strategies to gain control and develop confidence in managing the situation.22 parents' accounts of living with a child with hydrocephalus suggest that through experience, they developed confidence in their ability to recognize and respond to possible shunt malfunction. As parents' confidence increased they wanted greater involvement in care decisions when seeking advice from health professionals. However, parents described not feeling in control of their child's condition because of the unpredictable nature of shunt malfunction. This lack of control may explain why uncertainties about their child's shunt dominated parents' accounts of living with a child with hydrocephalus. In addition, the life‐threatening nature of shunt malfunction resulted in parents deferring decisions about the shunt to health professionals.
Evidence suggests parents perceive that developing the expertise to manage their child's long‐term condition will optimize the child's heath and development, and minimize the physical, psychological and social impact of the condition for the child.23, 24, 25, 26 The process of developing this expertise has been described as blending knowledge and skill acquisition with experiential knowledge in to adapt to changes in the child's condition.26, 27, 28 For parents living with a child with hydrocephalus, a significant part of managing their child's condition was associated with recognizing shunt malfunction and responding accordingly. Through integrating their knowledge and experiences of their child's condition, parents developed considerable competence and expertise in relation to differentiating between general childhood illnesses and shunt malfunction. This included developing the skills to recognize and respond to subtle changes in their child. For some parents, the integration of knowledge and experience when differentiating between general illnesses and shunt malfunction became intuitive. These findings are similar to a longitudinal study that explored how mothers living with a child with a long‐term condition developed the necessary expertise to meet their child's needs and became empowered when consulting with health‐care professionals.29 If necessary the mothers’ challenged health professionals’ assessments and decisions.
The anticipated benefits of empowering patients to self‐manage their care are improved health outcomes because patients are more likely to respond and act on illness symptoms, more effective use of medicines and treatments, greater understanding of the implications of professional advice and better ability to cope with the condition.30 Yet, service users report dissatisfaction in the level they are involved in care delivery and care decisions.31, 32 The concept of shared decision making, where the patient is actively involved in the evaluation of possible treatment options and shares decisions about the care package that best meets their needs, is based on a range of treatment options being available.30 In the context of hydrocephalus when the child's shunt malfunctions, the only reasonable course of action is surgical revision of the shunt. Parents acknowledged there were no alternative treatment choices following a definitive diagnosis of shunt malfunction. Nevertheless, they still wanted to collaborate with health professionals when establishing the diagnosis. However, parents also wanted health professionals to recognize their knowledge, skills and experience with regard to managing their child's condition. parents' accounts suggested that health professionals’ willingness to collaborate about their child's diagnosis and care was variable.
The concept of ‘normalization’ is widely described in the literature relating to long‐term conditions and is associated with the ability to cope and adjust to the child's condition.33, 34, 35 The process of normalization can be hindered because of ongoing disruptions to family life as a result of providing direct care and accompanying the child for treatments and clinic appointments.33, 36 However, over time, the majority of parents living with a child with a long‐term condition embed their child's needs into the routines of daily life.37, 38 Parents who participated in the study did not identify with the term ‘normalization’, suggesting all families were unique. However, parents' accounts revealed they constantly balanced the vigilance needed to identify signs of shunt malfunction with living a ‘normal’ family life. For some parents, the unpredictability and life‐threatening nature of shunt malfunction and the frequency of hospital admissions dominated family life.
Conclusion
This study investigated parents' experiences of living with a child with a shunt. The conceptual framework reflects the way parents assimilate their day‐to‐day experiences and knowledge as they develop the expertise to manage their child's condition. Parents develop considerable expertise in recognizing and responding to illness symptoms in their child. For some parents, this included differentiating between illness symptoms that were indicative of common childhood illness and those that were more likely to be due to a problem with the shunt. Although parents were satisfied with the services they received such as having direct access to the children's neurological ward, promptness in organizing diagnostic investigations and surgery if the shunt required revising, at times, parents felt their concerns were not listened to and their experiences not valued. parents' judgements about their child's symptoms and decisions when managing shunt problems were at times influenced by meeting the needs of all the family members. Parents were constantly balancing the vigilance needed to identify signs of shunt malfunction with living a ‘normal’ family life. Health professionals' judgements about parents' management of their child's hydrocephalus need to take into consideration this social context to collaborate effectively with parents.
Author contributions
Joanna Smith: study design, data collection and analysis, developing the paper; Professor Francine Cheater: study design, developing the paper; Dr Hilary Bekker: Study design, developing the paper.
Acknowledgements
We wish to thank Dr John Livingston (Consultant Neurologist), Sharon Peacock (Neurosciences Nurse Specialist), Julie Cooper (Senior Sister Children's Neurosciences) and Bernadette Baldwin (Northern Regional Advisor for Association for Spina Bifida and Hydrocephalus) for their enthusiasm, support and advice about the study.
References
- 1. Fernell E, Hagberg G. Infantile hydrocephalus: declining prevalence in pre‐term infants. Acta Paediatrica, 1998; 87: 392–396. [DOI] [PubMed] [Google Scholar]
- 2. Kennedy CR, Ayers S, Campbell MJ, Elbourne D, Hope P, Johnson A. Randomized, controlled trial of acetazolamide and furosemide in post‐hemorrhagic ventricular dilation in infancy: follow up at 1 year. Pediatrics, 2001; 108: 597–607. [DOI] [PubMed] [Google Scholar]
- 3. Piatt JH, Carlson CV. A search for determinants of cerebrospinal fluid shunt survival: retrospective analysis of a 14‐year institutional experience. Pediatric Neurosurgery, 1993; 19: 233–242. [DOI] [PubMed] [Google Scholar]
- 4. Drake JM, Kestle JRW, Milner R et al Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery, 1998; 43: 294–305. [DOI] [PubMed] [Google Scholar]
- 5. Kirkpatrick M, Engleman H, Minns RA. Symptoms and signs of progressive hydrocephalus. Archives of Diseases in Childhood, 1989; 64: 124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rekate HL. Shunt revisions: complications and their prevention. Pediatric Neurosurgery, 1991; 17: 155–162. [DOI] [PubMed] [Google Scholar]
- 7. Watkins L, Hayward R, Andar U, Harkness W. The diagnosis of blocked cerebrospinal fluid shunts: a prospective study of referral to a paediatric neurosurgical unit. Child's Nervous System, 1994; 10: 87–90. [DOI] [PubMed] [Google Scholar]
- 8. Iskandar BJ, Tubbs S, Mapstone TB, Grabb PA, Bartolucci AA, Oakes WJ. Death in shunted hydrocephalic children in the 1990's. Pediatric Neurosurgery, 1998; 28: 173–176. [DOI] [PubMed] [Google Scholar]
- 9. Garton HJL, Kestle JRW, Drake JM. Predicting shunt failure on the basis of clinical symptoms and signs in children. Journal of Neurosurgery, 2001; 94: 202–210. [DOI] [PubMed] [Google Scholar]
- 10. Barnes NP, Jones SJ, Hayward RD, Harkness WJ, Thompson D. Ventriculoperitoneal shunt blockage: what are the best predictive clinical indicators? Archives of Diseases in Childhood, 2002; 87: 198–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mori K, Shimada J, Kurisaka M, Sato K, Watanabe K. Classification of hydrocephalus and outcome of treatment. Brain and Development, 1995; 17: 338–348. [DOI] [PubMed] [Google Scholar]
- 12. Spencer L, Ritchie J, O'Conner W. Analysis, principles and processes In Ritchie J, Lewis J. (eds) Qualitative Research Practice. London: Sage Publications, 2003: 199–262. [Google Scholar]
- 13. Smith J, Firth J. Qualitative data analysis: application of the framework approach. Nurse Researcher, 2011; 18: 52–62. [DOI] [PubMed] [Google Scholar]
- 14. Tuckett G. Part 11. Rigour in qualitative research: complexities and solutions. Nurse Researcher, 2005; 13: 29–42. [DOI] [PubMed] [Google Scholar]
- 15. Slevin E. Enhancing the truthfulness, consistency, and transferability of a qualitative study: using a manifold of two approaches. Nurse Researcher, 2002; 7: 79–197. [Google Scholar]
- 16. Penrod J. Advancing uncertainty: untangling and discerning related concepts. International Journal of Qualitative Methods, 2002; 1: 54–58. [Google Scholar]
- 17. Shaha M, Cox C, Talman K, Kelly D. Uncertainty in breast, prostate and colorectal cancer: implications for supportive care. Journal of Nursing Scholarship, 2008; 40: 60–67. [DOI] [PubMed] [Google Scholar]
- 18. Mishel MH. Uncertainty in acute illness. Annual Review of Nursing Research, 1997; 15: 57–80. [PubMed] [Google Scholar]
- 19. Wright LJ, Afari N, Zautra A. The illness uncertainty concept: a review. Current Pain and Headache Reports, 2009; 13: 113–138. [DOI] [PubMed] [Google Scholar]
- 20. Mishel MH. Reconceptualization of the uncertainty in illness theory. Image: Journal of Nursing Scholarship, 1990; 22: 256–262. [DOI] [PubMed] [Google Scholar]
- 21. Penrod J. Living with uncertainty: concept advancement. Journal of Advanced Nursing, 2007; 57: 238–245. [DOI] [PubMed] [Google Scholar]
- 22. Penrod J. Refinement of the concept of uncertainty. Journal of Advanced Nursing, 2001; 1: 238–245. [DOI] [PubMed] [Google Scholar]
- 23. Swallow VM, Jacoby A. Mothers' evolving relationships with doctors and nurses during the chronic illness trajectory. Journal of Advanced Nursing, 2001; 36: 755–764. [DOI] [PubMed] [Google Scholar]
- 24. Dickinson AR, Smythe E, Spence D. Within the web: the family‐practitioner relationship in the context of chronic childhood illness. Journal of Child Health Care, 2006; 10: 309–325. [DOI] [PubMed] [Google Scholar]
- 25. Sullivan‐Bolyai S, Rosenberg R, Bayard M. Fathers' reflections on parenting young children with type 1 diabetes. MCN. The American Journal of Maternal and Child Nursing, 2006; 31: 24–31. [DOI] [PubMed] [Google Scholar]
- 26. Cashin GH, Small SP, Solberg SM. The lived experiences of fathers who have children with asthma; a phenomenological study. Journal of Pediatric Nursing, 2008; 23: 372–397. [DOI] [PubMed] [Google Scholar]
- 27. Balling K, McCubbin M. Hospitalized children with chronic illness: parental care giving needs and valuing parental experience. Journal of Pediatric Nursing, 2001; 16: 315–326. [DOI] [PubMed] [Google Scholar]
- 28. Kirk S, Glendinning C, Callery P. Parent or nurse? The experience of being a parent of technology‐dependent child. Journal of Advanced Nursing, 2005; 51: 456–464. [DOI] [PubMed] [Google Scholar]
- 29. Gibson C. Facilitating reflection in mothers of chronically ill children. Journal of Clinical Nursing, 1999; 8: 305–312. [DOI] [PubMed] [Google Scholar]
- 30. Coulter A, Parsons S, Askham J. Where are the patients in decision‐making about their own care. Copenhagen: WHO, 2008. [Google Scholar]
- 31. Grol R, Wensing M, Mainz J et al Patient's in Europe evaluate general practice care: an international comparison. British Journal of General Practice, 2000; 50: 882–887. [PMC free article] [PubMed] [Google Scholar]
- 32. Richards N, Coulter A. Is the NHS becoming more‐patient centred? Oxford: Picker Institute, 2007. [Google Scholar]
- 33. Smith J, Cheater F, Bekker H. parents' experiences of living with a child with a long‐term condition: a rapid structured review of the literature. Health Expectations, 2013. doi: 10.1111/hex.12040 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Knafl K, Gilliss CL. Families and chronic illness: a synthesis of current research. Journal of Family Nursing, 2002; 8: 178–198. [Google Scholar]
- 35. Coffey JS. Parenting a child with chronic illness: a metasynthesis. Pediatric Nursing, 2006; 32: 51–59. [PubMed] [Google Scholar]
- 36. Hentinen M, Kyngäs H. Factors associated with the adaptation of parents with a chronically ill child. Journal of Clinical Nursing, 1998; 7: 316–324. [DOI] [PubMed] [Google Scholar]
- 37. Knafl K, Zoeller L. Childhood chronic illness: a comparison of mothers' and fathers' experiences. Journal of Family Nursing, 2000; 6: 287–302. [Google Scholar]
- 38. Wennick A, Hallström I. Families' lived experience one year after a child was diagnosed with type 1 diabetes. Journal of Advanced Nursing, 2007; 60: 299–307. [DOI] [PubMed] [Google Scholar]


