Abstract
Background
Shunts, the main treatment for hydrocephalus, are problematic as they frequently malfunction. Identifying shunt malfunction requires parents to recognize its symptoms and health professionals to integrate parents' information about the child's symptoms within the clinical assessment to reach a diagnosis.
Aim
To investigate parent–professional shared decision making during the diagnosis of suspected shunt malfunction in acute hospital admissions.
Design and methods
A mixed method study involving audio recordings of admission consultations, a shared decision making questionnaire and interviews 1‐week post‐consultation, was undertaken. Twenty‐eight family members and fourteen health professionals participated. The interactions were analysed using conversational analysis, framework approach for the interview data and descriptive statistics for questionnaire responses.
Findings
Both parents and professionals focussed on establishing a diagnosis and ruling out shunt malfunction when a child with hydrocephalus was ill. Participants' perceived effective collaboration as central to this task: parents wanted to contribute to the process of diagnosis by providing information about the likely cause of symptoms. Professionals were satisfied with the level of involvement by parents, although parent satisfaction was more variable. The challenge for professionals was to integrate parents' expertise of their child's presenting symptoms within clinical decision making processes.
Conclusion
In this context, both parents' and professionals' perceived their interactions to be about problem‐solving, rather than making decisions about treatments. Although the shared decision‐making model can help patients to make better decisions between treatment options, it is unclear how best to support collaboration between professionals and parents to ensure a good problem‐solving process.
Keywords: collaboration, health professionals, hydrocephalus, long‐term conditions, parents, shared decision making
Background
Current health policy within western societies endorses a model of service and care delivery based on patient‐centeredness emphasizing the need for health professionals to actively engage with and involve service users in decision making processes.1 In the child health setting, this encompasses involving parents, and children where appropriate, in decisions that affect their child's health care.2 Shared decision making is the process whereby patients and health professionals take an active role in decisions concerning the patient's health.3 This broad conceptualization of shared decision making can be applied to a range of decision making activities such as patients' contribution to the nature of their problem4 and the patient's involvement in decisions about care delivery and treatment monitoring.5 A shared decision‐making model of care has particular relevance for parents living with a child with a long‐term condition because the day‐to‐day management of care becomes primarily the responsibility of the family. Professionals rely on parents to provide health‐care interventions for their children and to recognize changes in the child's condition. Yet, research exploring parents' experiences of living with a child with a long‐term condition suggests that parent–professional collaboration is variable despite parents' expectations of involvement in care decisions.6 Parent–professional communication appears to be primarily focussed on information giving, gaining consent for treatment and establishing good rapport rather than encouraging active contribution towards care decisions.7, 8
Shunts, the main treatment for hydrocephalus, are problematic as they frequently malfunction,9, 10 which can have life threatening consequences.11, 12 Detecting shunt malfunction is challenging because symptoms are variable and may be similar to those of common childhood illnesses, particularly viral infections.11, 13, 14 Identifying shunt malfunction therefore requires effective parent–professional collaboration: recognition and appropriate response by parents to the symptoms of shunt malfunction and the integration of parents' information about the child's symptoms by professionals within clinical decision making and diagnosis. Parents of children with hydrocephalus develop considerable expertise in recognizing and responding to illness symptoms in their child but perceive that this expertise is not always valued by professionals.15 A detailed examination of the interactions between parents and health professionals may identify approaches that support or hinder parents' contribution to their child's care when they seek health‐care advice in the context of suspected shunt malfunction. Although there is a growing body of research focussing on interactions in health‐care settings and particularly studies using conversation analysis as the primary method,16, 17, 18, 19 the idiosyncratic nature of the clinical problem which is the focus of this article has received little attention.
Study aims
To investigate parent–professional shared decision making during the diagnosis of suspected shunt malfunction in acute hospital admissions. Specific objectives:
Identify parents' and professionals' contribution to the diagnosis of shunt malfunction;
Explore parents' and professionals' perceptions and experiences of shared decision making within this clinical context.
Participant recruitment
Participants were recruited from a regional children's neurosciences ward within a United Kingdom National Health Service acute hospital trust. The sampling criteria were broad and included any parent of a child admitted to the children's neurosciences ward because they were concerned about their child's shunt and the health professionals involved in the child's initial assessment. Although typically not responsible for diagnostic decisions, nurses were included because in this clinical context self‐referral to the ward resulted in senior nurses making immediate clinical judgements about the severity of the child's clinical condition and initiating initial management strategies.
Study design and methods
A mixed method design, primarily based on qualitative approaches, was adopted to explore the breadth and depth of parent–professional interactions and experiences when a child is admitted to hospital with suspected shunt malfunction. Detailed descriptions of the methods, data collection strategies and data analysis are available online. Data were collected between September 2008 and September 2009. A range of data were collected and included:
Twenty‐one audio‐recorded interactions between parents and health professionals during the assessment of a child admitted to hospital because of possible shunt malfunction. Combinations were parent (mother or father or both, and child where appropriate) and nurse or doctor; each admission varied depending on which health professionals consented to participate and whether junior staff consulted with senior colleagues when uncertain about the child's diagnosis;
Thirty‐one follow‐up interviews undertaken 1‐week following the child's discharge from hospital. An interview topic guide was used to explore parents' and professionals' perceptions of involving parents in care decisions when a child is admitted to hospital because of possible shunt malfunction. Some health professionals participated in more than one interview;
Forty‐four questionnaires consisting of 10 statements relating to decision making tasks. Statements were developed from the OPTION (observed patient involvement)20 and COMRADE (combined outcome measure for risk communication and treatment decision making effectiveness)21 tools. Statements were scored on a 5‐point agree–disagree continuum scale. Parents completed separate questionnaires to evaluate nurses and doctors, and some health professionals completed more than one questionnaire. The questionnaires enabled parents' and professionals' evaluation of the extent to which professionals involve parents in care decisions to be compared.
Local research ethics committee and site‐specific approval from the research and development department were obtained (LREC reference 08/H1313/18). Consent was obtained from participants prior to both recording of the interactions and undertaking interviews. Health professionals received information about the study in advance of and during the data collection period. The acute nature of the child's admission to hospital did not allow parents the usual period of 24 h to decide whether to participate. In an emergency situation, the senior nurse on duty made a clinical judgement on whether to provide parents with information about the study. Parents were allowed sufficient time to read the study information before the senior nurse ascertained if they wished to participate.
Data analysis
A range of analytical approaches were undertaken. First, the principles of conversation analysis (CA) were applied to the interactional data. CA is a well‐established socio‐linguistic method for analysing conversation. The patterns, structures and practices of talk‐in‐interaction were explored through the application of the analytical processes associated with CA (turn‐taking, turn design, social actions and sequence organization).22 The CA notations used are presented in Table 1. Essential to the validity of the interactional data was the verification of the analysis by an experienced CA researcher (JC). Second, the framework approach, based on thematic analysis, underpinned the analysis of data obtained from the individual interviews.23 Third, data obtained from the questionnaires were quantitative in nature, and analysis of the extrapolated data consisted of descriptive statistics, primarily percentages and frequencies.
Table 1.
Transcription notation system for CA
| Relative timing of utterances | |
| (0.5) | Numbers in brackets indicate timings in whole and tenths of a second |
| (.) | A full stop in brackets indicates a micro pause of less than two tenths of a second |
| = | No discernible interval between turns |
| [] | Square brackets are used to denote overlapping speech |
| Characteristics of speech delivery | |
| . | Full stops are used to indicate a falling intonation |
| here | Underline is used to indicate an emphasis of words relative to surrounding talk |
| ↑ or ↓ | Indicates speech spoken with a high or low pitch relative to surrounding talk |
| °here° | Degree signs indicate speech that is quiet or soft relative to surrounding talk |
| >this< | Talk speeded up or compressed relative to surrounding talk |
| <this> | Talk slower or elongated relative to surrounding talk |
| .hhh | Indicates an in breath (number of h's indicate length) |
| hhh. | Indicates an out breath (number of h's indicate length) |
Findings
Forty‐two participants participated in the study and included 28 family members (13 mothers, 6 fathers, 9 children) and 14 health professionals (2 senior nurses, 2 junior nurses, 4 senior doctors, 6 junior doctors). One mother and one junior doctor did not participate in the interview. A summary of participant and child characteristics is presented in Table 2.
Table 2.
Participant characteristics
| Parents characteristics | (n = 13)a |
|---|---|
| Gender | |
| Male: Female | 1:12 |
| Age (years) | Mean 38.5: range 21–56 |
| 21–30 | 3 |
| 31–40 | 6 |
| Above 40 | 4 |
| Highest qualification | |
| A levels or above | 4 |
| GCSE | 4 |
| None | 5 |
| Socio‐economic classification | |
| 2 | 3 |
| 5–7 | 4 |
| 8 | 6 |
| Ethic group | (n = 14)a |
| White British: Asian | 13:1 |
| Child characteristics | (n = 14)b |
|---|---|
| Gender | |
| Male: Female | 9: 5 |
| Age (years) | Mean 8.6: range 1–15 |
| Under 5 | 5 |
| 6–10 | 2 |
| 11–15 | 7 |
| Shunt revisions | Mean 2: range 0–12 |
| 0 | 4 |
| 1 | 3 |
| 2 | 3 |
| 3+ | 4 |
| Health professional characteristics | (n = 14) |
|---|---|
| Gender | |
| Male:Female | 6:7 |
| Age (years) | Mean 33.6: range 27–56 |
| 21–30 | 5 |
| 31–40 | 8 |
| Above 50 | 1 |
| Years since qualified | Mean 8.8: range 3–17 |
| Less than 5 | 5 |
| 6–10 | 6 |
| Above 10 | 3 |
| Role and grade | |
| Senior nurses | |
| Band 7 | 1 |
| Band 6 | 1 |
| Junior nurses | |
| Band 5 | 2 |
| Senior doctors | |
| Specialist registrars | 4 |
| Junior doctors | |
| Specialist trainee (year 2) | 2 |
| Specialist trainee (year 3) | 4 |
| Ethnic group | |
| White (British and Irish) | 10 |
| Asian (Indian and Pakistani) | 4 |
One parent participated in the interaction but not the interview, data missing but ethnic group was obtained from medical notes.
Characteristics for all 14 children obtained from medical notes (children participated in the interactions).
The findings are presented in two sections. First an overview from each of the data collection methods is reported. Second, findings from the interactional and interview data are drawn together to present a cohesive account of patient–professional collaboration in the context of diagnosing shunt malfunction in children and to enhance the credibility of the findings.24
Overview of the findings
Parent–professional interactions
Topic sequences within doctor–patient consultations are well established and relate to greetings, the presenting complaint, examination, making a diagnosis, treatment planning and closings sequences.25 These well‐established sequences were not always evident in the interactions; for example, a possible reason for the child's presenting symptom was not always offered. Interactions involving nurses and senior doctors had a greater emphasis on exploring the presenting complaint and care planning compared to those of junior doctors. Two themes were evident across the interactions that related to the study focus and were explored in depth; ‘establishing a cause for illness symptoms’ and ‘involving parents in care planning’. Twenty‐three cases of interest were identified relating to establishing the likely cause of the child's illness symptoms. Four types of turn designs were identified: health professionals invited parents to offer a possible cause for the child's illness symptoms; parents initiated the offer of a possible cause for the child's illness symptoms; and parents either accepted or rejected health professionals' judgements about the likely cause of the child's illness symptoms. Parents were more likely to offer a possible cause for the child's illness symptoms if invited to do so by health professionals (Table 3).
Table 3.
Establishing a cause for illness symptoms (n = 23)
| Turn design | Parent invited to offer a diagnosis | Parent initiated the offer of a diagnosis | Parent accepted professional judgements | Parent rejected professional judgements |
|---|---|---|---|---|
| Frequency | 30% (n = 7) | 18% (n = 4) | 26% (n = 6) | 26% (n = 6) |
| Example | Doctor: so what are you your thoughts as to what's going on | Mum: he could have chicken pox he has spots on his legs | Doctor: he looks like he has a virus, we'll do a scan just in case | Doctor: does anyone have coughs, colds tummy bugs |
| Mum: well I don't really know but the shunts is a concern | Doctor: it's worth taking a look | Mum: ok yes I think he's virally | Mum: if I thought she had a virus I wouldn't have brought her in |
Eleven cases of interest were identified in relation to involving parents when planning care and treatments. Analysing the cases of interest identified two types of turn designs: parents either accepted or rejected care plans. Parents were more likely to accept than reject care plans offered by health professionals (Table 4).
Table 4.
Involving parents when planning care (n = 11)
| Turn design | Accepted care plans | Rejected care plans |
|---|---|---|
| Frequency | 82% (n = 9) | 18% (n = 2) |
| Example | Doctor: the concern is the shunt isn't inside the tummy but I don't think it's that, we'll keep him overnight, if he's still headachy in the morning then we'll repeat his scan | Doctor: we'll have to do a CT scan |
| Mum: that's fine | Mum: with it hurting at the back I thought about the cyst changing at the back of his head, would he need an MRI to see that |
Interview data
Six themes emerged from the analysis of interview data: ‘eliciting and valuing parents’ concerns’; ‘incorporating parents’ knowledge with the clinical assessment’; ‘establishing a cause of illness symptoms’, ‘involving parents in care planning’; ‘barriers and levers to effective parent–professional collaboration’.
Questionnaire data
Data from the questionnaires are summarized in Table 5. Overall parents and professionals were satisfied with the level of parental involvement in their child's care. Across all questions, 55% of the scores for both groups related to ‘strongly agree’ or ‘agree’ responses. Health professionals did not score ‘strongly disagree’ in response to any of the statements and ‘disagree’ for only one statement relating to ‘ascertaining the level parents wanted to participate in care decisions’. In contrast, parents used the full range of response categories with ‘strong disagreement’ or ‘disagreement’ indicated in 9 of the 10 statements.
Table 5.
Participants' perceptions of decision making tasks (questionnaire data)
| Summary of statements (questionnaire data; n = 26 parent responsesa, n = 18 professional responsesb) | Score (%) | S/A | A | N | D | S/D |
|---|---|---|---|---|---|---|
| Listening/being listened to | Parent | 65 | 23 | 12 | 0 | 0 |
| HP | 44 | 40 | 6 | 0 | 0 | |
| Causes for the child's symptoms suggested | Parent | 35 | 27 | 23 | 11 | 4 |
| HP | 61 | 39 | 0 | 0 | 0 | |
| Parents views included in the assessment | Parent | 54 | 31 | 4 | 11 | 0 |
| HP | 61 | 33 | 6 | 0 | 0 | |
| Treatment options discussed | Parent | 35 | 35 | 15 | 15 | 0 |
| HP | 50 | 39 | 11 | 0 | 0 | |
| Advantages/disadvantages of treatment discussed | Parent | 42 | 15 | 12 | 31 | 0 |
| HP | 45 | 33 | 22 | 0 | 0 | |
| Parents understanding of treatment options ascertained | Parent | 50 | 27 | 4 | 19 | 0 |
| HP | 50 | 22 | 28 | 0 | 0 | |
| Parents had opportunity to ask questions | Parent | 73 | 19 | 0 | 8 | 0 |
| HP | 83 | 17 | 0 | 0 | 0 | |
| Ascertain level parents wanted to be involved in care decisions | Parent | 27 | 46 | 23 | 9 | 0 |
| HP | 33 | 44 | 17 | 6 | 0 | |
| Decisions about care were made with parents | Parent | 65 | 15 | 8 | 8 | 4 |
| HP | 50 | 39 | 11 | 0 | 0 | |
| Satisfaction with the level of involvement in care | Parent | 61 | 23 | 8 | 0 | 8 |
| HP | 61 | 39 | 0 | 0 | 0 |
SA, strongly agree; A, agree; N, neither agree or disagree; D, disagree; SD, strongly disagree; HP, health professional.
Parents completed two questionnaires – rating both doctors and nurses.
Some health professional completed more than one questionnaire.
Integration of findings from the interactional and interview data
The themes from the interactional data and interview data were brought together to form two core concepts that characterized participants' experiences and perceptions about parental involvement when diagnosing shunt malfunction. The first concept related to the challenges when establishing a diagnosis of shunt malfunction in children. The second concept related to parents' and professionals' perceptions of collaboration, and the practices of health professionals that enabled or hindered effective collaboration. The concepts and associated themes are presented in Table 6.
Table 6.
Concepts and themes
| Concepts | Themes |
|---|---|
| Establishing a diagnosis of shunt malfunction | Eliciting and valuing parents' concerns |
| Incorporating parents' knowledge with the clinical assessment | |
| Establishing a cause for illness symptoms | |
| Collaboration: perceptions and practices | Involving parents in care planning |
| Barriers and levers to effective parent‐professional collaboration | |
| Perceptions of parent‐professional collaboration |
Establishing a diagnosis of shunt malfunction
For both parents and professionals, a significant feature of managing hydrocephalus in children was establishing whether or not illness symptoms were evidence of shunt malfunction. Professionals recognized the role of parents' knowledge of their child and the need to take account of their concerns in the assessment processes. However, there were variations in parents' experiences of having their views valued, illustrated in the following interview extracts:
One nurse said you know your daughter best and how she is in herself. So they do listen to you. Well they did to me and my concerns. I mentioned it (the shunt) and they said they'd get it checked straight away and they did.
Admission 10, mum
I am not sure if they (doctors and nurses) believed me at first, I kept saying this was not usual. Although they listened they didn't really seem to believe me.
Admission 1, mum
Conversation analysis of the interactions provided evidence of both a bilateral and unilateral style of communication between parents and professionals. ‘Bilateral’ collaboration occurs as a process of negotiation, whereas in a ‘unilateral’ approach, health professionals operate, in the main, independent of their interactions with the patient26. First, the ‘bilateral’ example is presented where there is evidence of effective communication with the parent to elicit information about the child's symptoms and collaboration to diagnose the problem (Table 7).
Table 7.
Eliciting and valuing parents' concerns – the ‘bilateral’ example
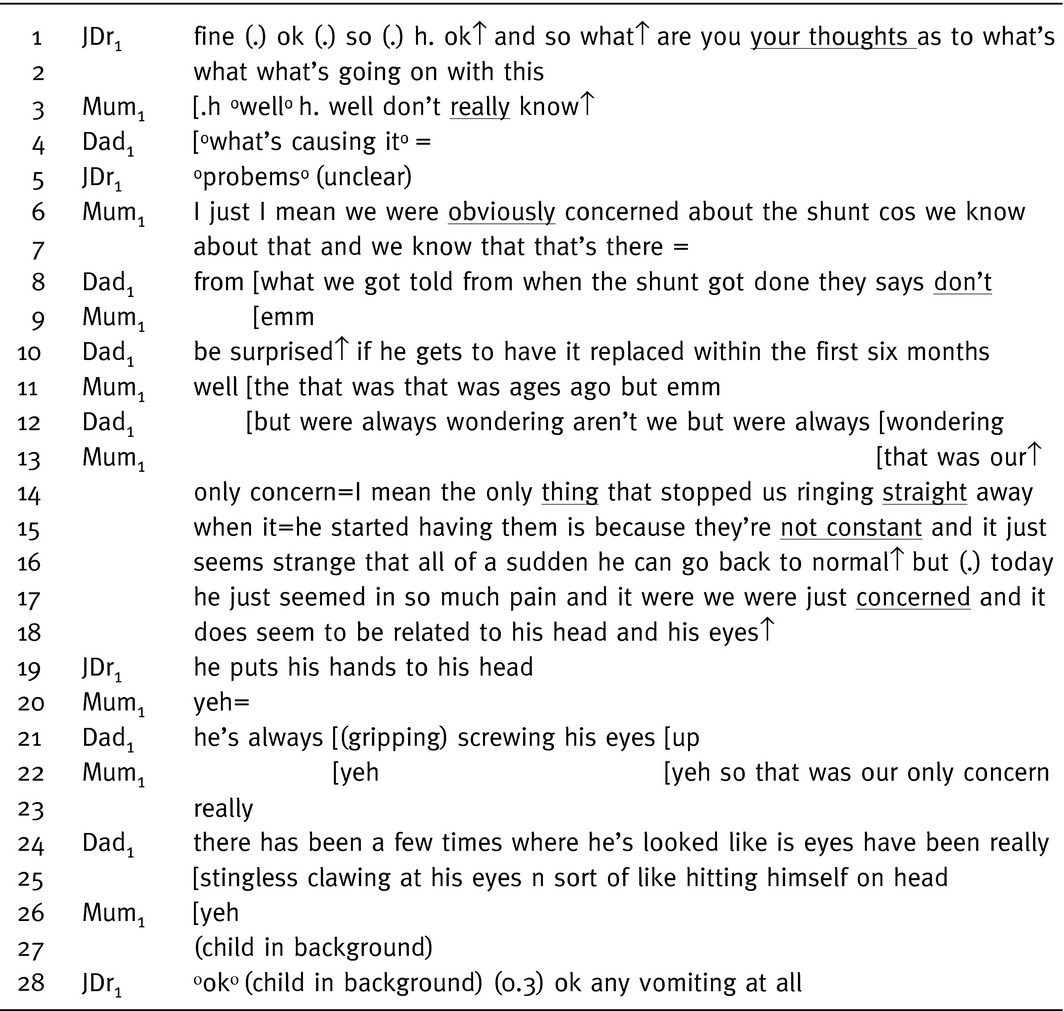
The sequence begins with the doctor inviting parents (‘you’ corrected to ‘your’) to offer a reason for their child's illness symptoms (lines 1–4, Table 7). Although the doctor's turn in line 5 is unclear, it is followed immediately by the mother taking a turn where she offers a possible reason for her concerns (line 6); ‘obviously concerned about the shunt’, with an emphasis on ‘obviously’. The sequence progresses in lines 6–18 as a dialogue between the parents which builds on and clarifies the information initially provided. During this exchange, there is no interruption from the doctor. His next turn (line 19) is essentially a clarification and acts as a continuation prompt, evident in lines 20–26 where parents continue the narrative relating to their concerns. The sequence concludes with a receipt of parents' accounts by the doctor (line 28).
The second example (Table 8) illustrates a more ‘unilateral’ style of communication. Although the purpose of the doctor's turns in the openings of the interactions presented in Tables 7 and 8 are aimed at soliciting the parents' perceptions about the likely cause of their child's presenting symptoms, the turn designs have contrasting sequential consequences. In the first sequence presented (Table 7), the second action in the opening turn (line 1, Table 7) is designed as an open invitation to parents to offer a reason for their child's illness symptoms. In contrast, the second action in the turn in line 1, Table 8, an assessment is made of the mother's likely concerns prior to seeking the mother's view (line 2). The turn design is shaped to produce a ‘preferred’ response'27; the mother could have agreed with the doctor's assessment but she offers a related but alternative ‘dispreferred’ response (line 3).
Table 8.
Eliciting and valuing parents' concerns‐ the ‘unilateral’ example
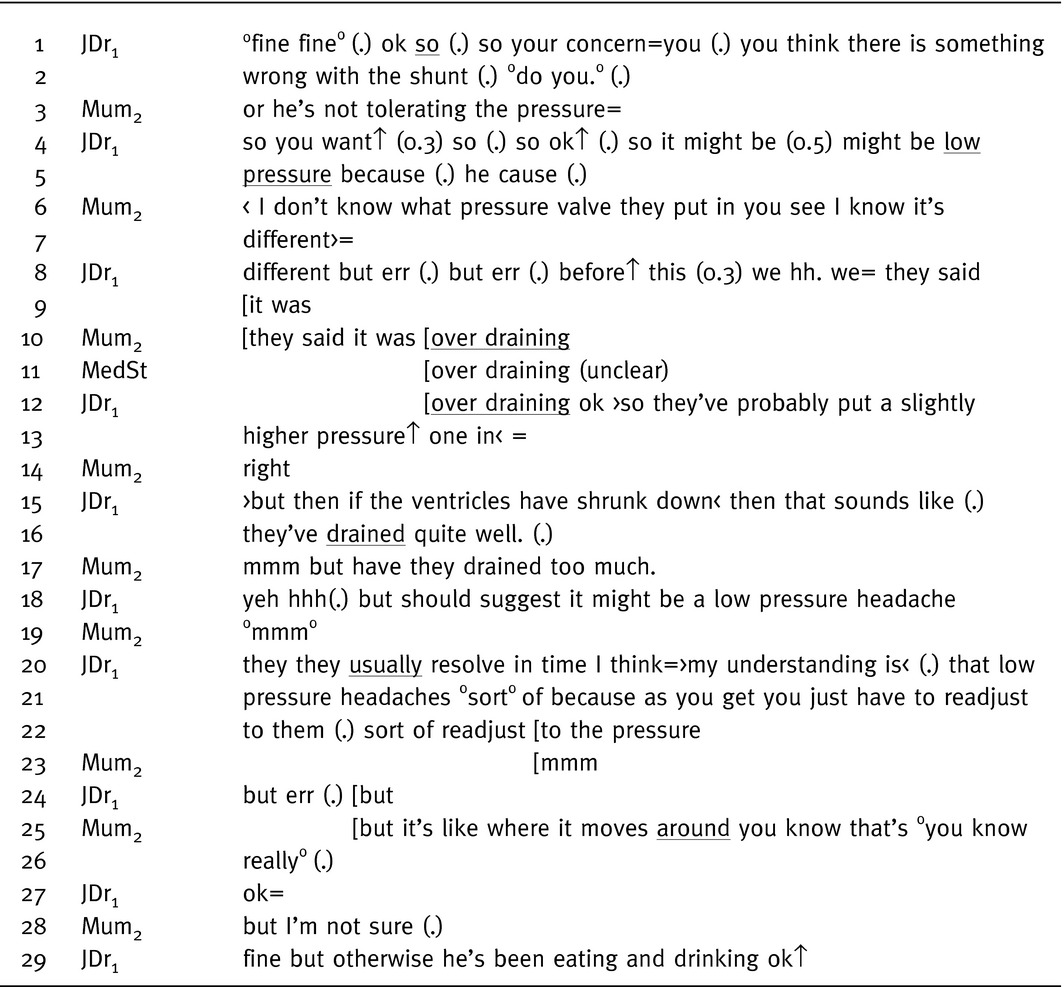
The doctor's offer in relation to the reason for the mother seeking medical advice and the mother's response appears problematic; he corrects his offer from ‘your concern’ to ‘you think’, there is a pause before completing his turn and falling intonation at the end of the turn (line 2) suggesting he does not necessarily concur. Following the mother's offer of an alternative explanation for her concerns (line 3), the sequences progresses (lines 4–25) with an expansion of the initial invitation (line 1); the mother offering reasons for the child's illness symptoms and the doctor responding. Explanation‐response sequences in medical encounters have been described in depth.28, 29 Typically, doctors may leave elements of patients' explanations unacknowledged as they focus on the tasks of the medical consultation. However, as in this extract in Table 8, doctors may also disregard patients' explanations and insert their own explanatory responses, which can lead to conflicts between the viewpoints of the doctor and patient.29
Doctors' responses when soliciting patients' (or parents) presenting concerns are crucial in establishing or rejecting the legitimacy of the presented problem.30 The doctor ‘receipts’ the mother's concern with ‘ok’, this acknowledges, but does not address her prior turn (line 27), indicating a rejection, or at least a down‐grading, of the legitimacy of problem she presents. The sequence concludes with a receipt of the mother's account by the doctor (indicated by ‘fine’ in line 29), and the turn continues without pause to a new sequence and topic proffer in the form of an invitation. During the follow‐up interview, the doctor recognized the mother as having considerable experience in relation to identifying the signs of shunt malfunction in her child; the child had undergone a considerable number of shunt‐related operations. However, the mother perceived that her views during the encounter were not valued.
Parents know the child far better than you and know when their children aren't well. Mum is probably as experienced as anyone in terms of shunt problems and the symptoms that (child's name) shows. Shunts are very difficult so we are obliged to treat everything seriously, especially if parents have concerns. His symptoms aren't always the text book symptoms.
Admission 2, junior doctor1
They don't seem to take on board what you're saying.
Admission 2, mum
Establishing a diagnosis of shunt malfunction based on clinical symptoms is difficult; uncertainties related to differentiating between symptoms that might be shunt related and those of common childhood illnesses, particularly viral infections. The relationship between participants' initial impressions and the admission outcome, in terms of the symptoms being shunt related, were variable. The examples below relate to the same admission (the child's shunt was revised):
This is not how he usually is and I just knew this wasn't him. He wasn't right he started holding and shaking his head. His behaviour is out of character that it had to be his shunt. I just though what else could it be.
Admission 1, mum
Children at that age pull their ears with an ear infection, so I didn't entirely dismiss the shunt but it did go down on my list of possibilities because clearly he has signs of an ear infection with frank pus, and it was a nasty ear infection. So I thought the ear infection was causing all the problems.
Admission 1, junior doctor1
These were new symptoms, shaking his head, and they were not like usual when (child's name) gets a cold or earache and could be due to the shunt.
Admission 1, senior nurse1
Collaboration: perceptions and practices
Parents' and professionals' struggled with the concept of shared decision making in relation to treatment decisions in this clinical context because following a diagnosis of shunt malfunction surgery to revise the shunt is the only realistic option. For some professionals, working with parents was primarily about ensuring they understood the child's care requirements to obtain consent for treatments. In contrast, professionals also described the value parents added to care decisions and the need to build effective and lasting relationships with the child and family.
I think the value a parent contributes is really quite high and not recognised as such. Where we fall down is actually not to do with lack of that belief but time constraint, when you're on call you're focusing on a set of specific questions of what to assess. I think parents sometimes want to talk about their concerns and anxieties, we don't address that a lot of the time and it can set off a chain reaction for the whole future because a shunt is for life. If set off to a bad start, it can run the whole experience bad over a long term.
Admission 5, senior doctor1
I think they should be involved to some degree and you need to listen to them and explain and usually they are on the same page as you anyway.
Admission 12, junior nurse1
They informed us of everything that had gone on, emm I don't know how to answer that (involvement in care decisions) because they do obviously go through everything with you on each procedure, so you are involved all the time. There's only one decision to be made really and obviously we just want him to be right and want his shunt working. I would not like to think we would have the final decision, but I would also like to think that everything has been discussed.
Admission 13, mum
Vitally important to involve parents. It's about working in partnership with parents' rather than their contribution to decisions. Clinicians obviously deal with children with different problems, so have a better understanding of the problem as a whole, although parents might know their child better. It's essential that clinicians do lead the management, involving parents it's more of a case of making parents understand the condition, or the cause of the symptoms. Working in paediatrics, one of the tenants must be including parents, but the emphasis is on good communication, decision making is more about listening and education.
Admission 1, junior doctor1
Professionals' perceptions of the factors that created barriers to communicating effectively with parents were more likely to relate to time constraints due to workload pressures and environment restrictions such as a lack of privacy when interacting with parents. In contrast, parents' perceived that effective communication with professionals was hindered by not being listened to, being excluded when professionals grouped together to discuss their child's care (for example, during ward rounds) were not kept informed of care plans and received conflicting information.
I needed to know what was happening so I could let family know back at home. I was just having to guess because nobody told me anything.
Admission 7, dad
There is so much conflicting information really. They don't seem to take on board what your saying, that's my feeling. No they really have their own agenda and that's what we are on now their agenda.
Admission 2, mum
Although parents were unlikely to reject care plans offered by professionals, the design and properties of the parent–professional interactions when accepting or rejecting care were different (Tables 9 and 10). In the sequence presented in Table 9, the senior doctor offers his views in lines 3–6 of the child's assessment. An initial plan of care is offered (line 15) which is immediately accepted by the child in line 18. Once accepted, the doctor moves on to providing more details in relation to establishing the cause of the child's illness symptoms (lines 24, 27, 30, 32). Although a diagnosis is not established, both the child and mother orient themselves to accepting the plan of care, evident by immediately responding to the doctor's turns, with ‘ok’, ‘yep’ and ‘that's fine’ (for example, lines 29, 31, 33). These features are typical in medical encounters when there is acceptance of treatment decisions.31
Table 9.
Agreeing a plan of care
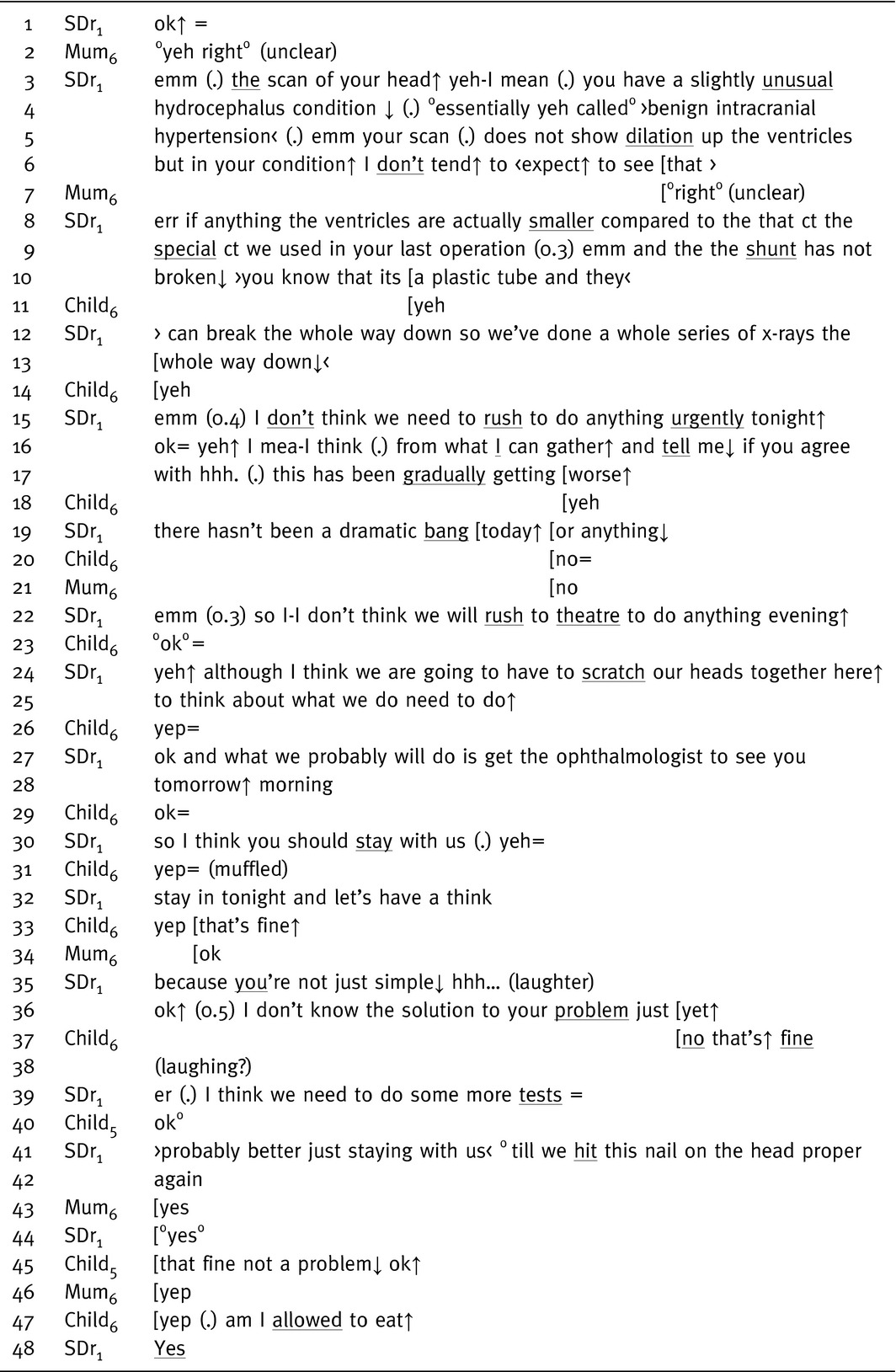
Table 10.
Rejecting a plan of care
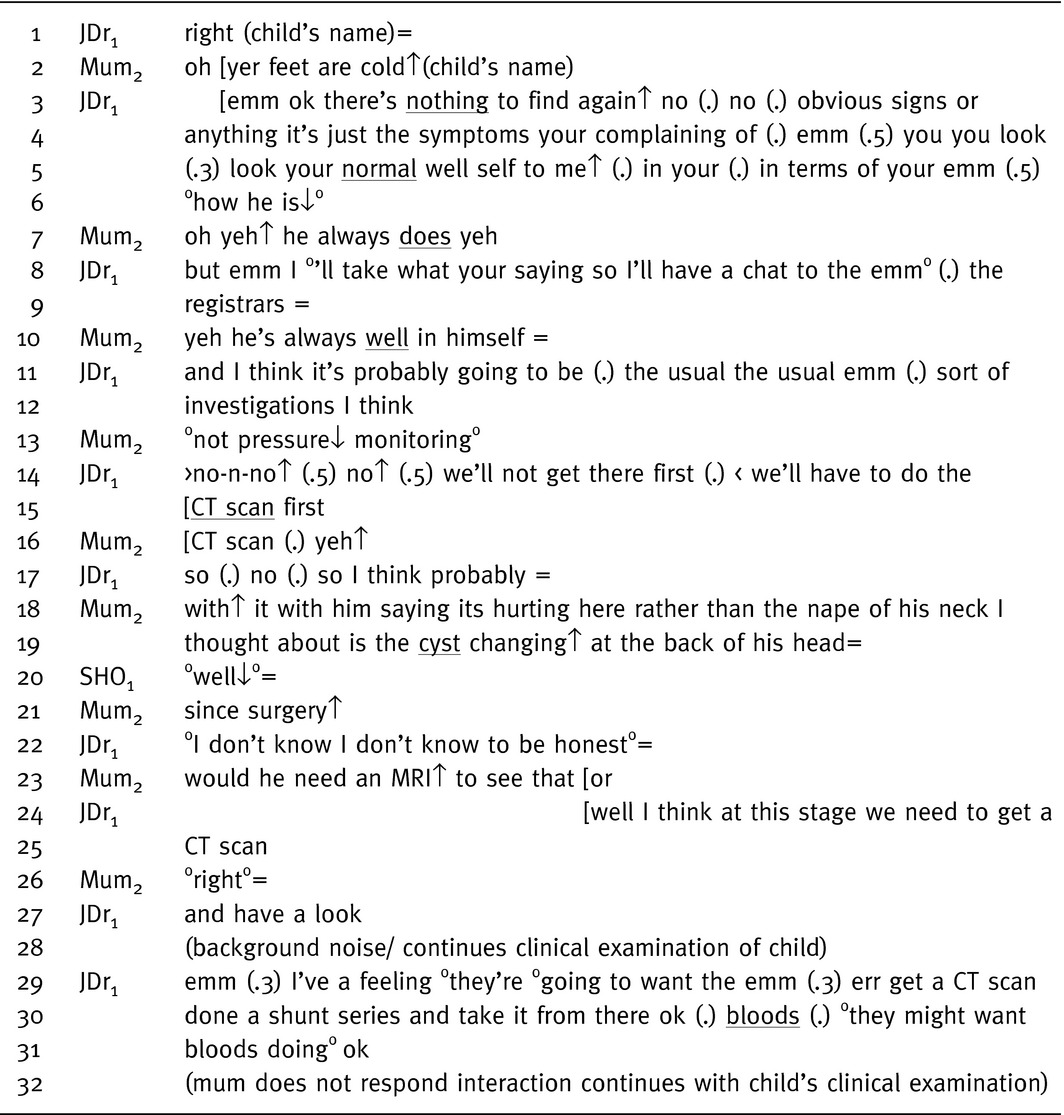
When rejecting care plans, interactions with parents become problematic, the sequence presented in Table 10 demonstrates active resistance to the care plan offered. The doctor's turns are punctuated with pauses, changes in pitch and hitches when delivering a possible diagnosis (lines 3–5) and when suggesting a plan of action (for example, lines 11–12). In contrast, the mother's turns are even in tone, measured and controlled (lines 18 and 23). The doctor's plan of investigations is not accepted by the mother, this ‘dispreferred’ response appears to result in the subsequent sequences being problematic (lines 3–6, and 14). The mother's responses are quiet and she emphasizes, evident by a fall in intonation, that she would resist ‘pressure monitoring’ (line 13). The mother builds a case for the investigations which she believes are appropriate in lines 18, 19 and 23. The doctor resists the mother's suggestions and moves to close the sequence, ‘well at this stage we'll need to get a CT’ in line 24. This turn is delivered at an even pace without the pauses and changes in intonation evident in his prior turns. The mother in her pre‐closing turn ‘receipts’ that she understands this sequence is closing with a quiet ‘right’ in line 26. The quiet responses coupled with the no response (line 28) suggest the mother does not necessarily concur with the care plan. Doctors are orientated towards patients accepting treatment offers; resistance places the doctor in the position of having to encourage the patient to accept the treatment or offer an alternative.31 In contrast, patients, as in the example presented in Table 10, do not necessarily conform to the doctors' preference for agreement, challenge prepositions and maintain contrary preferences.32
The descriptions of parent–professional interaction presented in Tables 9 and 10 differ in the way that care plans are presented and negotiated. In the first interaction, a definitive course of treatment is not offered, but alternatives are provided for further consideration in relation to establishing a cause of the illness symptoms. Deciding the cause of the child's illness symptoms is framed in a way that any decisions will be based on agreement between the child and the doctor evident by the use of ‘we’ and ‘our’ (‘we are going to have to scratch our heads together’, line 24, ‘think about what we need to do’, line 25, ‘let's have a think’, line 32).26 In contrast, decisions about the type of investigations that will be undertaken in the second interaction (Table 10) are presented as information giving and the discussion is centred on medically controlled options consistent with a unilateral approach to parent–professional collaboration.26
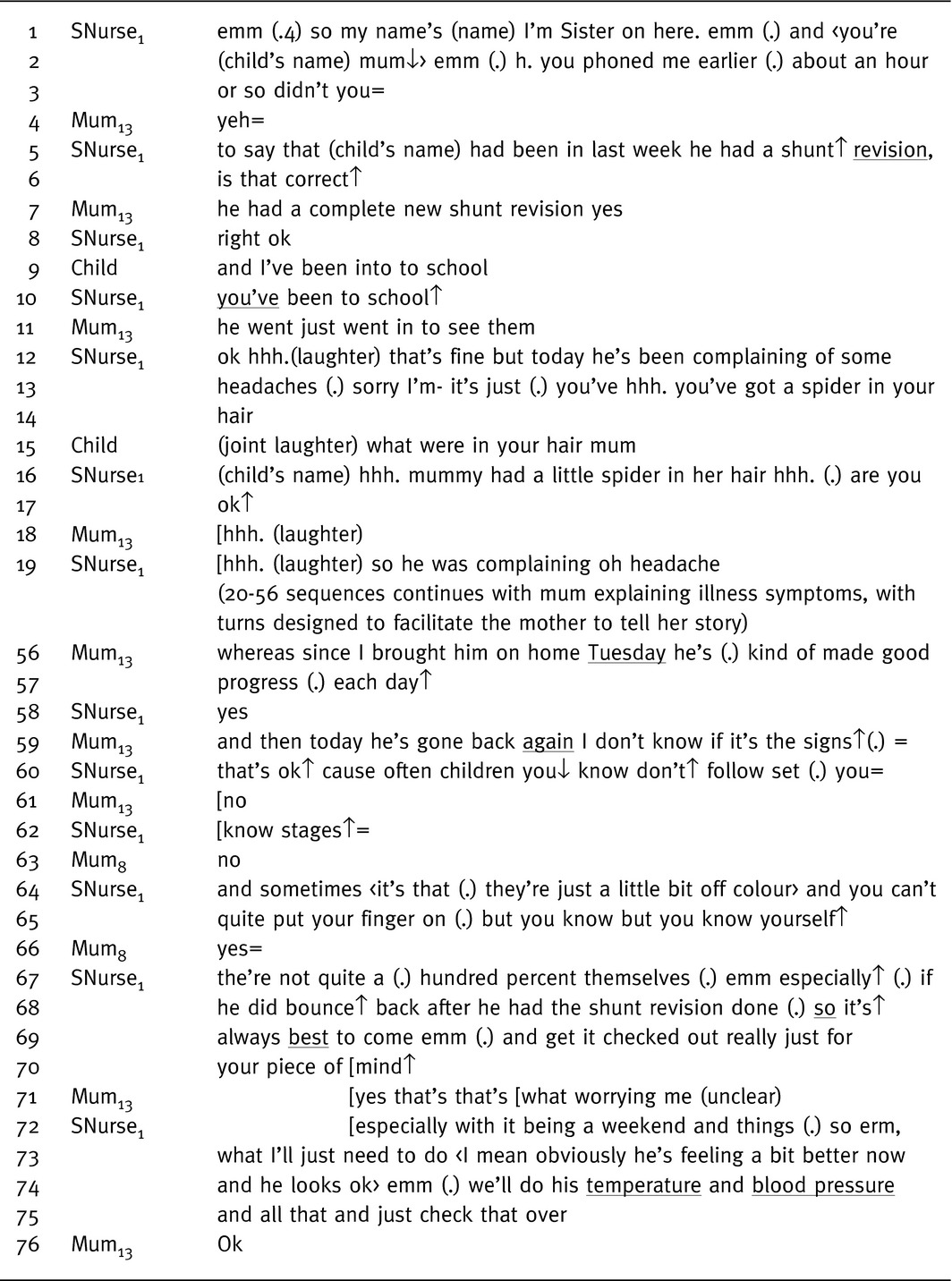
A range of factors that facilitate or hinder effective parent–professional engagement were identified. Parents' and professionals' identified listening, information sharing, valuing parents' experiences, establishing rapport and continuity with the professionals providing care for the child as ways of effectively engaging with parents. Establishing rapport has been recognized as one way of engaging effectively with parents33, 34 and was evident during the conversation analysis of the interactions. In the sequence presented in Table 11, rapport building is evident from the beginning of the senior nurse–parent interaction (lines 1–8) when the child's recent hospital admission is summarized. The nurse enabled the mother's ‘telling of her storey’ which is evident by her acknowledging the mother's talk with minimal utterances, such as the ‘yes’ in line 58. In her pre‐closing sequence, the nurse offers support for the mother's decision to bring the child back to the ward ‘it's↑ always best to come emm (.) and get it checked out’ (line 69), ‘for your piece of mind’ (line 70). The mother's narrative is primarily presented in her own terms, and the nurse's responses display understanding, empathy and agreement with the mother's account.33, 34 Listening to patients' stories is one of the ways professionals can attend to patients' concerns and understand their illness.
Table 11.
Effective parent‐professional collaboration: rapport buildings
Discussion
The key message from the findings of this study is that for both parents and health professionals establishing a diagnosis of shunt malfunction required working collaboratively but the position in the care pathway where optimal collaboration could occur differed. Shared decision making is more likely to occur during the treatment planning stage of consultations because patients and professions are orientated towards treatment plans having joint responsibility.25, 31 Typically, patients accept professionals' judgements when responding to the delivery of the diagnosis and with minimal utterances and actively respond to treatment decisions.31 Parents in this study contributed to diagnostic sequences, and although their contributions were more likely to be in response to an explicit invitation from health professionals, parents also offered possible causes for their child's illness symptoms. Previous studies of the negotiation of treatment decisions between doctors and parents related to new health problems31; differences in the findings reported here may reflect the different care context, such as the acute nature of the child's admission to hospital, and parents' vast experience of their child's condition.
Despite shared decision making being the dominant model of patient–professional engagement,5 it is poorly defined and has not been widely adopted by health professionals.35, 36, 37 For children with long‐term conditions and their families, there appear to be difficulties in operationalizing a model of shared decision making, which assumes that a range of treatment choices exist in relation to the care under discussion. This scenario is potentially problematic as many interactions between patients and professionals require involvement around problem‐solving and illness management rather than deciding between a range of options. The shared decision making model can help patients make better decisions between treatment options,38, 39 but is less helpful in urgent care setting.40 When a child presents with potential shunt malfunction, the priority of care is to establish a diagnosis rather than offering a definitive treatment plan. In this clinical context, there was evidence that parents' knowledge of their child and previous experiences of shunt malfunction were used alongside the clinical assessment when health professionals made a judgement about the child's illness symptoms.
The quality of interactions between patients and health professionals can influence the effectiveness of information exchange, the development of patient–professional relationships, rapport building and the way care is negotiated at each stage of the care pathway.41 The process of including parents was not always transparent; health professionals' perceived that they included and valued parents' contribution to care decisions, while parents did not always perceive that their contributions were valued. Collaboration in this clinical context is not about shared decision making in relation to treatments but about the value health professionals' place on parents' experiences, and the way these experiences are incorporated into clinical decision making. Collaboration, in the context of making health‐care decisions, has been defined as ‘a process of engagement in which health professionals and patients work together to understand clinical issues and determine the best course of action’.36 As collaborators in their child's care parents expected to be included at each stage of the care pathway; health professionals' perceived involvement to occur primarily at the information gathering and treatment planning stages. Further research is required to understanding the nature of ‘expert parents’ in terms of the attributes that constitute becoming an expert and the ways health professionals engage with and incorporate parents expertise into care decisions when working with children with long‐term conditions. Exploring the reasons for differences between the perceptions of parents and professionals in relation to collaborative practice may facilitate better parent–professional engagement and collaboration.
Central to effective patient–professional collaboration and a good problem‐solving process is the rapport and trust that patients develop with health professionals. Investing in eliciting patients' perspectives such as identifying their concerns, exploring the impact of illness symptoms on patients lives and involving patients in decisions can enhance patient–professional partnerships.42 Findings from the study presented suggest that although good practice was evident, collaborating with parents, particularly when parents had considerable expertise in managing their child's long‐term condition, was challenging. Practical training to help health professionals develop and use a range of communications strategies, rather than basing interactions on subjective judgments43, could be a means of improving parent–professional collaboration. Furthermore, the development of a measure and evaluating collaborative practice could assist in measuring the effectiveness of interventions aimed at improving parent–professionals collaboration.
Conclusion
The shared decision making paradigm, where parents and health professionals exchange treatment preferences to reach an agreement on a plan of care, is not a helpful one to guide interactions in this clinical context where the diagnosis of the health problem has not yet been established. Further, in this context, once a diagnosis has been made, there is only one course of action. When a child presents with potential shunt malfunction, the priority is to reach an accurate diagnosis rather than planning treatments. Parents' satisfaction when seeking health‐care advice for suspected shunt malfunction was linked to the way professionals' engaged and involved them in decisions about the likely cause of illness symptoms, a model of collaboration is more appropriate. Parents developed considerable expertise in recognizing the symptoms of shunt malfunction in their child and were able to distinguish between shunt‐related illness symptoms and those associated with common childhood illnesses. Parents want to contribute towards decisions about their child's care, but this input does not appear to be a priority for health professionals. Yet, professionals vary in their effectiveness to integrate parents' expertise with their clinical assessment and involve explicitly parents in the diagnosis prior to planning the child's care.
Author contributions
Dr Joanna Smith contributed to study design, data collection and analysis, and wrote the manuscript. Professor Francine Cheater contributed to study design and wrote the manuscript. Dr Hilary Bekker contributed to study design, development of questionnaires and wrote the manuscript. Dr John Chatwin contributed to study design, application of conversation analysis and wrote the manuscript.
Supporting information
Appendix S1. Shared decisions about a child's care on presentation of suspected shunt malfunction.
Acknowledgements
We wish to thank Dr John Livingston (Consultant Neurologist), Sharon Peacock (Neurosciences Nurse Specialist), Julie Cooper (Senior Sister Children's Neurosciences) and Bernadette Baldwin (Northern Regional Advisor for Association for Spina Bifida and Hydrocephalus) for their enthusiasm, support and advice about the study.
References
- 1. International Alliance of Patients' Organizations . Patient‐Centre Healthcare Review, 2nd edn London: International Alliance of Patients' Organizations, 2007. [Google Scholar]
- 2. Department for Education of Skills/Department of Health . National Service Framework for Children; Every Child Matters. London: DfES/DH, 2004. [Google Scholar]
- 3. Howie JGR, Heaney D, Maxell M. Quality, core values and general practice consultation: issues of definition, measurement and delivery. Family Practice, 2004; 21: 458–468. [DOI] [PubMed] [Google Scholar]
- 4. Bugge C, Entwistle VA, Watt IS. Information that is not exchanged during consulations: significance for decision‐making. Social Scinece and Medicine, 2006; 63: 2313–2320. [DOI] [PubMed] [Google Scholar]
- 5. Entwistle V. Patient involvement in decision‐making: the importance of a broad conceptualization In: Edwards A, Elwyn G. (eds) Shared Decision‐Making in Healthcare, 2nd edn Oxford: Oxford University Press, 2009: 17–22. [Google Scholar]
- 6. Smith J, Cheater F, Bekker H. Parents' experiences of living with a child with a long‐term condition: a rapid structured review of the literature. Health Expectations, 2013. doi: 10.1111/hex.12040 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Espezel HJE, Canam CJ. Parent‐nurse interactions: care of hospitalised children. Journal of Advanced Nursing, 2003; 44: 34–41. [DOI] [PubMed] [Google Scholar]
- 8. Payot A, Gendron S, Lefebvre F, Doucet H. Deciding to resuscitate extremely premature babies: how do parents and neonatologists engage in the decision? Social Science and Medicine, 2007; 64: 1487–1500. [DOI] [PubMed] [Google Scholar]
- 9. Piatt JH, Carlson CV. A search for determinants of cerebrospinal fluid shunt survival: retrospective analysis of a 14‐year institutional experience. Pediatric Neurosurgery, 1993; 19: 233–242. [DOI] [PubMed] [Google Scholar]
- 10. Drake JM, Kestle JRW, Milner R et al Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery, 1998; 43: 294–305. [DOI] [PubMed] [Google Scholar]
- 11. Watkins L, Hayward R, Andar U, Harkness W. The diagnosis of blocked cerebrospinal fluid shunts: a prospective study of referral to a paediatric neurosurgical unit. Child's Nervous System, 1994; 10: 87–90. [DOI] [PubMed] [Google Scholar]
- 12. Iskandar BJ, Tubbs S, Mapstone TB, Grabb PA, Bartolucci AA, Oakes WJ. Death in shunted hydrocephalic children in the 1990's. Pediatric Neurosurgery, 1998; 28: 173–176. [DOI] [PubMed] [Google Scholar]
- 13. Garton HJL, Kestle JRW, Drake JM. Predicting shunt failure on the basis of clinical symptoms and signs in children. Journal of Neurosurgery, 2001; 94: 202–210. [DOI] [PubMed] [Google Scholar]
- 14. Barnes NP, Jones SJ, Hayward RD, Harkness WJ, Thompson D. Ventriculoperitoneal shunt blockage: what are the best predictive clinical indicators? Archives of Diseases in Childhood, 2002; 87: 198–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Smith J Parents' management of their child's hydrocephalus and shunt. PhD thesis, Leeds: University of Leeds, 2010. [Google Scholar]
- 16. Collins S, Britten N, Ruusuvuori J, Thompson A. Understanding the process of patient participation In: Collins S, Britten N, Ruusuvuori J, Thompson A. (eds) Patient Participation in Healthcare Consultations: Qualitative Perspectives, Maidenhead: Open University Press, 2007: 3–21. [Google Scholar]
- 17. Chatwin J. Activity transitions in the homoeopathic therapeutic encounter. The Sociological Review, 2009; 57: 163–185. [Google Scholar]
- 18. Collins S. Explanations in consultations: the combined effectiveness of doctors and nurses communication with patients. Medical Education, 2005; 39: 785–796. [DOI] [PubMed] [Google Scholar]
- 19. Entwistle VA, Watt IS, Gilhooly K, Bugge C, Haites N, Walker A. Assessing patients' participation and quality of decision making: insights from a study of routine practice in diverse settings. Patient Education and Counselling, 2004; 55: 105–113. [DOI] [PubMed] [Google Scholar]
- 20. Elwyn G, Hutchings H, Edwards A et al The OPTIONS scale: measuring the extent that clinicians involve patients in decision‐making tasks. Health Expectations, 2005; 8: 34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Edwards A, Elwyn G, Hood K et al The development of COMRADE‐ a patient‐based outcome measure to evaluate the effectiveness of risk communication in consultations. Patient Education and Counselling, 2003; 50: 311–322. [DOI] [PubMed] [Google Scholar]
- 22. Drew P, Chatwin J, Collins S. Conversation analysis: a method for research into interactions between patients and health‐care professionals. Health Expectations, 2001; 4: 58–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Spencer L, Ritchie J, O'Conner W. Analysis, principles and processes In: Ritchie J, Lewis J. (eds) Qualitative Research Practice. London: Sage Publications, 2003: 199–218. [Google Scholar]
- 24. Tobin GA, Begley CM. Methodological rigour within a qualitative framework. Journal of Advanced Nursing, 2004; 48: 388–396. [DOI] [PubMed] [Google Scholar]
- 25. Robinson J. An interactional structure of medical activities during acute visits and its implications for patient participation. Health Communication, 2003; 15: 27–59. [DOI] [PubMed] [Google Scholar]
- 26. Collins S, Drew P, Watt I, Entwistle V. ‘Unilateral’ and ‘bilateral’ practitioner approaches in decision‐making about treatment. Social Science and Medicine, 2005; 61: 2611–2627. [DOI] [PubMed] [Google Scholar]
- 27. Schegloff EA. Sequence Organisation in Interaction: A Primer in Conversation Analysis. Cambridge, New York: Cambridge University Press, 2007. [Google Scholar]
- 28. Gill VT. Doing attributions in medical interaction: patients' explanations for illness and doctors' responses. Social Psychology Quarterly, 1998; 61: 342–360. [Google Scholar]
- 29. Gill VT, Maynard DW. Explaining illness: patients' proposals and physicians responses In: Heritage J, Maynard DW. (eds) Communication in Medical Care: Interactions between Primary Care Physicians and Patients. Cambridge: University Press, 2006: 115–150. [Google Scholar]
- 30. Robinson J. Soliciting parents' presenting concerns In: Heritage J, Maynard DW. (eds) Communication in Medical Care: Interactions between Primary Care Physicians and Patients. Cambridge: Cambridge University Press, 2006: 22–47. [Google Scholar]
- 31. Stivers T. Treatment decisions: negotiations between doctors and patients in acute care encounters In: Heritage J, Maynard DW. (eds) Communication in Medical Care: Interactions between Primary Care Physicians and Patients. Cambridge: Cambridge University Press, 2006: 279–312. [Google Scholar]
- 32. Boyd E, Heritage J. Taking the patient's medical history: questioning during comprehensive history taking In: Heritage J, Maynard DW. (eds) Communication in Medical Care: Interactions between Primary Care Physicians and Patients. Cambridge: Cambridge University Press, 2006: 151–184. [Google Scholar]
- 33. Chatwin J, Watt I, Collins S, Field R. A feeling of equality: some interactional features that build rapport and mutuality in a clinical encounter In: Collins S, Britten N, Ruusuvuori J, Thompson A. (eds) Patient Participation in Healthcare Consultations: Qualitative Perspectives. Maidenhead: Open University Press, 2007: 83–103. [Google Scholar]
- 34. Ruusuvuori J. Managing affect: integration of empathy and problem‐solving in health care encounters. Discourse Studies, 2007; 9: 597–622. [Google Scholar]
- 35. Gravel K, Légaré F, Graham I. Barriers and facilitators to implementing shared decision‐making in clinical practice: a systematic review of the literature. Implementation Science, 2006; 1: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. O'Grady L, Jadad A. Shifting from shared to collaborative decision‐making: a change in thinking and doing. Journal of Participatory Medicine, 2010; 8: e13. [Google Scholar]
- 37. Légaré F, Turcotte S, Stacey D, Ratté S, Kryworuchko J, Graham ID. Patients' perceptions of sharing in decisions: a systematic review of interventions to enhance shared decision making in routine clinical practice. Patient, 2012; 5: 1–19. [DOI] [PubMed] [Google Scholar]
- 38. Entwistle V, Prior M, Skea ZC, Francis JJ. Involvement in treatment decision‐making: its meaning to people with diabetes and implications for conceptualisation. Social Science & Medicine, 2008; 66: 362–375. [DOI] [PubMed] [Google Scholar]
- 39. Lown BA, Hanson JL, Clark WD. Mutual influence in shared decision making: a collaborative study of patients and physicians. Health Expectations, 2009; 12: 160–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Frank C, Fridlund B, Baigi A, Asp M. Patient participation in the emergency department: an evaluation using a specific instrument to meagre patient‐participation (PPED). Journal of Advanced Nursing, 2010; 67: 728–735. [DOI] [PubMed] [Google Scholar]
- 41. Gordon C, Ellis‐Hill C, Ashburn A. The use of conversational analysis: nurse‐patient interaction in communication disability after stroke. Journal of Advanced Nursing, 2009; 65: 544–553. [DOI] [PubMed] [Google Scholar]
- 42. Frakel RM, Stein T. Getting the most out of the clinical encounter: the four habits model. The Permanente Journal, 1999; 3: 79–88. [PubMed] [Google Scholar]
- 43. Ranmal R, Prictor M, Scott JT. Interventions for improving communication with children and adolescents about their cancer. Cochrane Database of Systematic Reviews, 2008; 4: CD002969. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Shared decisions about a child's care on presentation of suspected shunt malfunction.


