Abstract
Background
Stigma and judgemental assumptions by health workers have been identified as key barriers to accessing health care for people living with co‐occurring mental health and substance use issues (dual diagnosis).
Objective
To evaluate the effectiveness of consumer‐led training by people with dual diagnosis in improving the knowledge, understanding and role adequacy of community health staff to work with this consumer group.
Methods
A controlled before‐and‐after study design with four waves of quantitative data collection was used. Qualitative data were collected to explore participants' views about training. Participants were staff from two community health services from Victoria, Australia. Recruitment occurred across various work areas: reception, oral health, allied health, counselling and health promotion. At baseline, all participants attended a 4‐h clinician‐led training session. The intervention consisted of a 3‐h consumer‐led training session, developed and delivered by seven individuals living with dual diagnosis. Outcome measures included understanding of dual diagnosis, participants' feelings of role adequacy and role legitimacy, personal views, and training outcomes and relevance.
Results
Consumer‐led training was associated with a significant increase in understanding. The combination of clinician‐led and consumer‐led training was associated with a positive change in role adequacy.
Conclusions
Consumer‐led training is a promising approach to enhance primary health‐care workers' understanding of the issues faced by dual‐diagnosis consumers, with such positive effects persisting over time. Used alongside other organizational capacity building strategies, consumer‐led training has the potential to help address stigma and judgemental attitudes by health workers and improve access to services for this consumer group.
Keywords: alcohol and drug, community health, consumer‐led, consumers, dual diagnosis, health communication, mental health, primary health care, stigma, substance use, training, workforce development
Introduction
People with alcohol and other drug (AOD) use issues also commonly experience co‐occurring mental health issues.1, 2 The co‐occurrence of drug and mental health concerns (dual diagnosis) has been consistently confirmed. Recent Australian data suggest that, overall, recent users of illicit drugs (past 12 months) were more likely to have been diagnosed or treated for a mental illness than those who had not used during the last 12 months. This association was evident for a range of individual substances: cannabis, ecstasy, meth/amphetamines and cocaine.3 Recent data from the Illicit Drug Reporting System (IDRS), Australia's national illicit drug monitoring system, found that 63% of Victorian participants who self‐reported illicit drug use also self‐reported mental health problems. Furthermore, of those with self‐identified co‐occurring illicit drug use and mental health problems, 90% reported having sought assistance from mental health services.4 This high prevalence of dual diagnosis is a concern and highlights the importance of having a competent workforce that is aware of the complex issues faced by individuals with dual diagnosis.
Dual diagnosis is typically associated with a range of poorer health and well‐being outcomes. Compared to those with a single disorder (e.g. depression), people living with dual diagnosis are more likely to experience physical health problems, suicidal thoughts or behaviour, social isolation, homelessness and high volumes of service utilization.5, 6, 7, 8 Not surprisingly, concerns that people living with dual diagnosis are regularly falling through the ‘cracks’ have been regularly raised by mental, AOD and other health service providers over the past decade.9, 10, 11, 12 A range of barriers to access treatment and follow‐up have been identified by both consumers and service providers.10, 13 Examples of such barriers include the stigma associated with living with co‐occurring illicit drug use and mental health problems; challenges associated with responding to complex and concurrent vulnerabilities; a lack of holistic or comprehensive services; a lack of appropriate services; poor service user knowledge of available services; inadequate referral processes and pathways; overly restrictive intake requirements; and service providers' judgemental assumptions regarding people living with dual diagnosis.9, 10, 14, 15, 16
Consumers, health practitioners and policymakers all stress the need for further education of primary health‐care workers (including reception staff) regarding dual diagnosis, to increase understanding and reduce stigma, judgemental attitudes and assumptions associated with dual diagnosis.9, 10, 12, 15, 16, 17 Indeed, improving the way people with dual diagnosis are perceived by health‐care workers is seen as necessary to enhance service responses in favour of this consumer group, as well as this consumer groups' experiences of such services. Consumer involvement in training and education is therefore viewed as instrumental in achieving these outcomes.13, 15
Consumers have been increasingly involved in the training of students, primary health‐care workers and their organizations in fields such as mental health and nursing.18, 19, 20, 21, 22, 23 Consumers may take on a variety of roles, including as ‘consultants’ in the development of materials and as trainers or teachers.21, 22, 24 However, there is a paucity of published examples of consumers having a high level of autonomy and ownership over the development and delivery of training packages. In 1995, Cook et al.25 demonstrated that the post‐training attitudes of American mental health professionals were significantly more positive when trained by a consumer than by a non‐consumer. Again in the USA, a consumer‐led intervention was shown to effectively improve mental health provider competencies in domains such as delivery of care, teamwork and in the delivery of holistic responses to mental health problems.26 In the Australian context, Meehan and Glover27 demonstrated that consumer‐led training enhanced mental health providers' knowledge of consumer‐focussed, recovery‐based ‘good’ practice.
To our knowledge, no study to date has examined the outcomes of consumer‐led training specifically for dual diagnosis or when delivered to a diverse audience of primary health‐care professionals and administrative staff. In addition to providing allied health, counselling, oral health and health promotion services, many Victorian community health services also offer AOD treatment services.13 As such, they are currently targeted by National and State initiatives to enhance their dual‐diagnosis capability and linkages with mental health services.13 Enhancing the health‐care workforce's understanding of, and capacity to respond to, the needs of people living with dual diagnosis is of concern for both practice and policy.
The aim of the current study was therefore to evaluate whether consumer‐led training would be effective in improving the knowledge, understanding and confidence of community health staff to work with people living with co‐occurring mental health and substance use issues, a dual diagnosis. Additionally, how the outcomes of consumer‐led training differ from those of more traditional training, that is, training delivered by ‘expert’ dual‐diagnosis clinicians, was also investigated.
Method
Study design
A controlled before‐and‐after study design was used, with two sites and four waves of data collection. The approach taken is summarized in Fig. 1.
Figure 1.
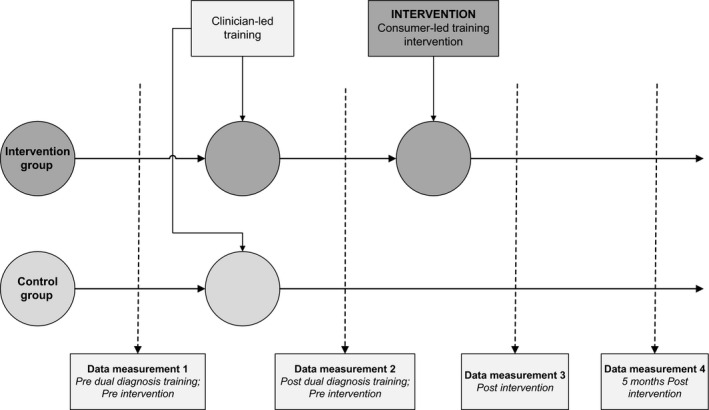
The study used a controlled before‐and‐after design with two sites and four waves of quantitative data collection.
Two independent community health services from the Metropolitan Region of Melbourne, Victoria, Australia, were involved. One acted as the intervention site and the other as the control site. Both organizations are similar in size, with 125 staff members at the intervention site and 115 at the control site. Both deliver a range of oral health, allied health, counselling, family and children services, and health promotion projects and programmes. However, key differences between sites are noteworthy. Firstly, the intervention site offers AOD counselling services, while the control site does not. The latter, however, coordinates the regional Needle and Syringe Program. Consequently, we can reasonably assume that consumers at each organization would differ, as would their expectations and experiences at each site. Secondly, at the commencement of the project, the intervention site had already benefited from 3 years of funding to build the capacity of its AOD team to work with consumers with dual diagnosis. To optimize comparability between sites and also minimize the effect of service mix and service user make up and experiences on the study results, a clinician‐led training session regarding dual diagnosis was provided to both study sites prior to the consumer‐led training at the intervention site.
At each site, staff were recruited to participate in the study prior to commencing the clinician‐led training session. Recruitment involved raising awareness of the training via email to all staff; with those unable to attend the clinician‐led training being excluded from participating. Staff members from all areas of both organizations were encouraged to attend.
Training and intervention
A 3.5‐h, clinician‐led training session was delivered by a senior dual‐diagnosis clinician at both the intervention and control sites. Topics covered in this session included defining dual diagnosis; prevalence of dual diagnosis in health‐care settings and the general population; barriers to treatment; the local health‐care service system; relevant dual‐diagnosis policy; dual diagnosis and marginalization; and attitudes and values regarding dual diagnosis that influence practice. The session was delivered using a mix of content delivery, case scenarios and individual reflection.
The intervention consisted of a 3‐h, consumer‐led training session, entirely developed and delivered by a group of individuals living with co‐occurring mental health and substance use issues. Over a 2‐month period, eight people living with dual diagnosis worked together with two facilitators from the Association of Participating Service Users, a consumer‐based organization dedicated to increasing the participation of people currently or previously using illicit drugs in health systems and policy, to develop their own training package. A total of seven consumers living with dual diagnosis were involved in delivering the session. Their session involved the provision of evidence‐based information on substance use, addiction and its impact on brain function, denial, relapse and compliance rates. They used role play and personal stories to illustrate barriers to health care and ways in which services can be improved, and provided an opportunity for session attendees to ask questions. The consumer‐led training was delivered to the intervention site only, 2 months after the clinician‐led training.
Measures
The Work Practice Questionnaire (WPQ) has been shown to be a reliable tool for assessing the impact of AOD‐related training and development.28 In the current study, the WPQ was refined so it could be used to assess the impact of dual‐diagnosis‐focussed training. As in the original form of the WPQ, the questionnaire applied in the current study contained eight domains. Together, the domains encompassed a total of 22 subthemes. Each subtheme represented a total of three to nine statements, which participants rated their level of agreement or disagreement to using a seven‐point Likert scale. Higher scores represented higher levels of agreement. The six subthemes considered in this paper as study variables are understanding, role adequacy, role legitimacy, personal views, training outcomes and training relevance (Table 1). Examples of subthemes excluded here for future analysis include opportunity for input, team cohesion, system influence and monitoring and review.
Table 1.
Subthemes from the modified Work Practice Questionnaire utilized for data collection, which were used as variables for this study
| Domaina | Subthemes | Example of underlying statements |
|---|---|---|
| Dual diagnosis | Understanding of dual diagnosis, mental health and alcohol and other drug (AOD) | How would you rate your understanding of dual‐diagnosis? Mental health? AOD? |
| Individual | Role adequacy | I am confident in my ability to respond to dual‐diagnosis‐related issues |
| I have the necessary knowledge to work with people with dual‐diagnosis‐related issues | ||
| Role legitimacy | I have a legitimate role to play in responding to alcohol‐ and other drug‐related issues | |
| I am clear about my responsibilities in responding to alcohol‐ and other drug‐related issues | ||
| Personal views and understanding | I think it would be difficult to live with dual diagnosis | |
| I generally think people living with dual diagnosis bring their difficulties on themselves | ||
| Training | Training outcomes | This training programme has enabled me to respond to dual‐diagnosis‐related issues with greater confidence |
| I gained skills and knowledge from this training programme that enabled me to work more effectively with people with dual‐diagnosis‐related issues | ||
| Training relevance | I changed the way I worked as a result of this training and development | |
| I changed the way I thought about people living with dual‐diagnosis‐, mental‐health‐ and AOD‐related issues as a result of this training and development | ||
| Personal and organizational demographics | Age, gender, current position, length of work in organization, length of work in sector, principal areas of work, time spent responding to dual‐diagnosis‐related issues | |
| Education and previous training | Education completed, previous training and development in dual diagnosis, mental health and/or AOD |
Domains excluded from data analysis were team, workplace and organizational.
Data were collected on four occasions: at baseline (before any training), after the clinician‐led training, after the consumer‐led training and 5 months following the consumer‐led training. Four 1‐h focus groups were also conducted to further explore participants' perspectives on the training sessions delivered. Three focus groups were held at the intervention site (including one exclusively with management) and one at the control site. Questions focused on staff experience of the training delivered, knowledge gained, usefulness of the training, and changes in confidence and work practices.
Data analysis
Data were screened for accuracy of entry and missing values from cases (i.e. participants). Mean substitution was applied to address the issue of missing values. Data were analysed using Statistical Package for Social Sciences (spss) 18 for Windows (spss Inc., Chicago, IL, USA). Bonferroni adjustments were made to the alpha (α) levels in all relevant analyses performed to control for Type 1 error.
Due to insufficient numbers, surveys completed at the control site at the 5‐month follow‐up (time four) were excluded from data analysis. Consequently, four waves of data were analysed for the intervention site, whereas only three waves were analysed for the control site. Only data from participants who completed four waves of data collection at the intervention site and three waves of data collection at the control site were retained for analyses.
An overall score was computed for each study variable (understanding, role adequacy, role legitimacy, personal views, training outcomes and training relevance) by adding up the ratings given to all statements under a particular subtheme. One‐way repeated measures anova was conducted to compare mean scores of understanding, role adequacy, role legitimacy and personal views over time at each study site. Mean scores of training outcomes and training relevance, as measured after the clinician‐led training and the consumer‐led training, were compared within each study site using paired samples t‐tests. Independent samples t‐tests were conducted to compare the mean scores of all six study variable between the two sites. Pearson's product‐moment correlation coefficients (r) were calculated to explore the association among study variables.
Focus groups were audio‐recorded and subsequently transcribed. Thematic analysis was undertaken using the transcripts to gain an in‐depth understanding of staff's perceptions and experiences of the training.29 For the purposes of this article, quotes have been used to further illustrate and explore the quantitative findings.
Results
Study participants
In total, 41 participants completed at least three waves of survey: 27 at the intervention site and 18 at the control site. Due to participant fatigue, only 31 participants completed the fourth wave of data collection at the 5‐month follow‐up: 23 at the intervention site and 8 at the control site (Table 2). Attrition at time four was therefore much greater at the control site (75.8%) than at the intervention site (45.5%). A total of 23 staff members participated in the focus groups: 8 from the control site and 15 from the intervention site.
Table 2.
Participation in data collection and percentage of attrition for each site, per quantity of surveys completed
| Participation in data collection | |||
|---|---|---|---|
| Completed initial survey | Completed 3 surveys (% attrition) | Completed 4 surveys (% attrition) | |
| Intervention site | 38 | 27 (28.9) | 23a (39.5) |
| Control site | 33 | 18a (45.5) | 8 (75.8) |
| Total | 71 | 45 (36.6) | 31 (56.3) |
Participants used in data analysis.
Characteristics of survey participants are detailed in Table 3. At both sites, the majority of participants were female and aged between 35 and 54 years. Nearly three‐quarters of respondents classified themselves as ‘team members’. At both sites, the highest level of educational attainment for approximately half of respondents was a bachelor's degree or a graduate certificate/diploma.
Table 3.
Characteristics of staff who completed three waves of data collection at the control site and four waves at the intervention site (N = 41)
| Characteristics | Intervention (n = 23) | Control (n = 18) | ||
|---|---|---|---|---|
| n | % | n | % | |
| Age in years | ||||
| ≤34 | 3 | 13.0 | 2 | 11.1 |
| 35–54 | 18 | 78.3 | 13 | 72.2 |
| ≥55 | 2 | 8.7 | 3 | 16.7 |
| Gender | ||||
| Male | 0 | 0 | 2 | 11.1 |
| Female | 23 | 100 | 16 | 88.9 |
| Current position in organization | ||||
| Manager or team leader | 6 | 26.1 | 6 | 33.3 |
| Team member or staff member | 17 | 73.9 | 12 | 66.7 |
| Approximate percentage of time spent responding to dual‐diagnosis‐related issues | ||||
| 0% | 6 | 26.1 | 5 | 27.8 |
| 1–20% | 11 | 47.8 | 12 | 66.7 |
| 21% or more | 6 | 26.1 | 1 | 5.6 |
| Principal areas of worka | ||||
| Non‐care (no contact with clients) | 12 | 53.2 | 5 | 27.8 |
| Care (direct contact with clients) | 11 | 47.8 | 13 | 72.2 |
| Highest level of education completed | ||||
| Basic (secondary to diploma) | 7 | 30.4 | 3 | 16.7 |
| Standard (bachelor and graduate certificate/diploma) | 12 | 52.2 | 9 | 50.0 |
| Postgraduate (master's and doctorate) | 4 | 17.4 | 5 | 27.8 |
| Previously completed training/development with a primary focus on dual diagnosis, mental health or alcohol/drugs | ||||
| Yes | 11 | 47.8 | 4 | 22.2 |
| No | 12 | 52.2 | 14 | 77.8 |
Where staff members endorsed both areas of work, they were only assigned to the ‘care’ category (9 at intervention site, 8 at control site).
Comparability of study sites
Analyses were carried out to examine the comparability of participants across sites. Attributes such as age distribution, highest level of educational attainment, position type (management vs. non‐management) and type of work (care vs. non‐care) did not differ significantly between sites. At the intervention site, more participants had previously attended AOD, mental health‐ or dual‐diagnosis‐related training and development (47.8%, compared to 22.2% at the control site) and reported spending more of their work time responding to dual diagnosis (26.1%, compared to 5.6%). Although t‐tests did not find between‐site differences for these two variables, we believe them to be a meaningful reflection of the differences between each organization.
Correlations among demographic and study variables
No significant correlations were found among demographic and study variables (understanding, role adequacy, role legitimacy and personal views) at baseline. Regardless of study site, age and position type were not found to be correlated to any of the study variables. The proportion of time spent responding to dual‐diagnosis issues was significantly positively associated with understanding (r = 0.59, P < 0.001), role adequacy (r = 0.74, P < 0.001), role legitimacy (r = 0.68, P < 0.001) and personal views (r = 0.31, P < 0.05) at baseline. Having attended previous training and development regarding dual diagnosis was also significantly positively associated with understanding (r = 0.58, P < 0.001), role adequacy (r = 0.71, P < 0.001), role legitimacy (r = 0.66, P < 0.001) and personal views (r = 0.50, P < 0.001) at baseline. Being in a role involving direct contact with people living with dual diagnosis was significantly positively associated with greater scores of understanding (r = 0.36, P < 0.05), role adequacy (r = 0.52, P < 0.001) and role legitimacy (r = 0.37, P < 0.05) at baseline, but not with personal views (r = 0.29, P = 0.07). Educational attainment was only significantly positively correlated with role legitimacy (r = 0.36, P < 0.05) and personal views (r = 0.38, P < 0.05) at baseline.
Correlations among study variables
Using data from both sites, understanding was significantly positively correlated with role adequacy (r = 0.76, P < 0.001), role legitimacy (r = 0.52, P < 0.001), training outcomes (r = 0.49, P < 0.001) and training relevance (r = 0.46, P < 0.001). Role adequacy was significantly positively correlated with role legitimacy (r = 0.66, P < 0.001), training outcomes (r = 0.54, P < 0.001) and training relevance (r = 0.58, P < 0.001). Role legitimacy was significantly positively correlated with personal views (r = 0.41, P < 0.001) and training relevance (r = 0.43, P < 0.001). Personal views were not associated with training outcomes (r = 0.15, P = 0.18) nor with training relevance (r = 0.14, P = 0.23). Finally, training outcomes and training relevance were significantly positively correlated (r = 0.77, P < 0.001). Table 4 contains a summary of these findings.
Table 4.
Person product‐moment correlations (r) among study variables, both sites combined (N = 41)
| Understanding | Role adequacy | Role legitimacy | Personal views | Training outcomes | Training relevance | |
|---|---|---|---|---|---|---|
| Understanding | – | 0.76a | 0.52a | 0.35a | 0.49a | 0.46a |
| Role adequacy | – | – | 0.66a | 0.38a, b | 0.54a | 0.58a, c |
| Role legitimacy | – | – | – | 0.41a, b | 0.27 | 0.43a |
| Personal views | – | – | – | – | 0.15 | 0.14 |
| Training outcomes | – | – | – | – | – | 0.77a |
| Training relevance | – | – | – | – | – | – |
Correlation significant at P ≤ 0.01.
Correlation significant at the intervention site only (n = 23).
Correlation significant at the control site only (n = 18).
Interestingly, understanding and personal views were significantly positively correlated (r = 0.35, P < 0.001), as were role adequacy and personal views (r = 0.37, P < 0.001). But, when correlations were calculated for each site, these associations only remained significant at the intervention site.
Understanding
Mean understanding scores were compared over time (Fig. 2). As expected given the difference in service mix between the two sites, along with the previous capacity building activity undertaken at the intervention site, a significant difference was observed in understanding levels between the intervention and the control sites at baseline (P < 0.05). Following the clinician‐led training, an increase in understanding was observed at the control site. Subsequent to this change, the mean difference in understanding scores between study sites became non‐significant (P = 0.18). Following the consumer‐led training, understanding scores increased by 15% at the intervention site (P < 0.01), thus resulting in a significant difference between sites (P < 0.01). Understanding remained at an increased level at the intervention site, even 5 months following the consumer‐led training.
Figure 2.
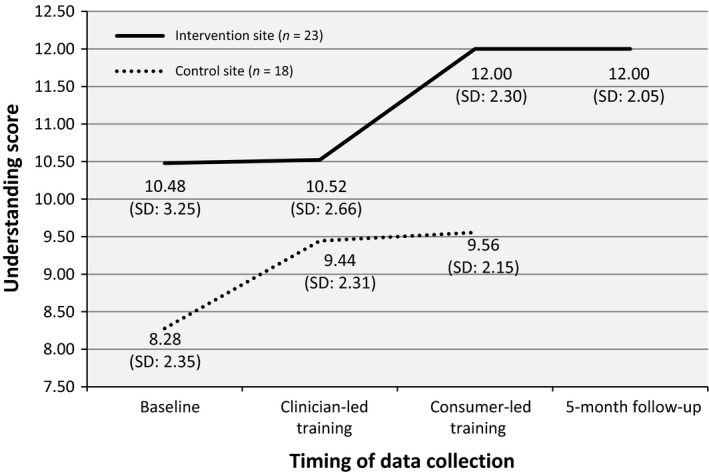
Based on one‐way repeated measures anova, the variation in mean understanding score was significant (P < 0.01) between clinician‐led training and consumer‐led training at the intervention site. There was a non‐significant trend (P = 0.07) towards increased understanding at the control site following the clinician‐led training.
Role adequacy
Similar to understanding, the mean scores for role adequacy were significantly different between sites at baseline (P < 0.05). This difference across sites remained significant following both types of training. At the control site, no difference in role adequacy was found across the three data collection points (Fig. 3). The slight but non‐significant increase at time three might be attributable to organizational activity after the clinician‐led training, such as the recruitment of a new Needle and Syringe Program coordinator (personal communication from the collaborating general manager of the control site). At the intervention site, both training sessions were associated with a non‐significant, incremental rise in role adequacy. However, the cumulative effect of the two training sessions (i.e. clinician‐led and consumer‐led) was associated with significantly higher role adequacy scores after the consumer‐led training, compared to baseline (P < 0.05).
Figure 3.
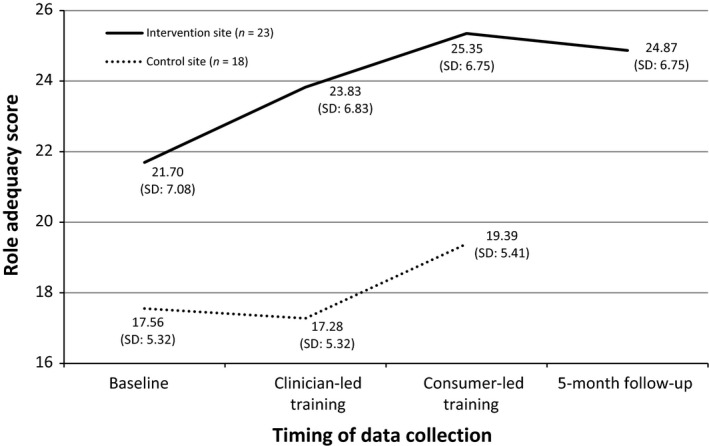
Based on one‐way repeated measures anova, only the cumulative effect of both clinician‐led and consumer‐led training was associated with a significant change in role adequacy at the intervention site.
Role legitimacy
Most probably reflective of the presence of a relatively large AOD team at the intervention site, role legitimacy levels were higher (P < 0.05) at baseline [mean (M) = 24.26, standard deviation (SD) = 6.98] compared to the control site (M = 19.39, SD = 5.73) and remained so after the clinician‐led training (M intervention = 25.09, SD = 5.30; M control = 21.44, SD = 5.23; P < 0.05) and after the consumer‐led training (M intervention = 24.78, SD = 6.15; M control = 20.39, SD = 5.15; P < 0.05). No significant changes were observed in role legitimacy over time, at either site.
Personal views
Mean personal views scores were similar across the two sites at baseline (M intervention = 15.78, SD = 2.78; M control = 16.22, SD = 2.21; P = 0.59), as well as after the clinician‐led training (M intervention = 16.74, SD = 2.28; M control = 16.33, SD = 1.97; P = 0.55) and the consumer‐led training (M intervention = 17.09, SD = 1.86; M control = 16.00, SD = 2.11; P = 0.09). Personal views, however, were higher at the intervention site following the consumer‐led training (P < 0.05) and at the 5‐month follow‐up (P < 0.01) compared with baseline. At the control site, no such difference was found over time.
Training outcomes
As illustrated in Fig. 4, intervention site participants rated the training outcomes of the clinician‐led training significantly higher than participants at the control site did (P < 0.05). In respect to the difference of training outcomes at the intervention site between the clinician‐led and consumer‐led training, outcomes were higher for the latter, although not significant (P = 0.067).
Figure 4.
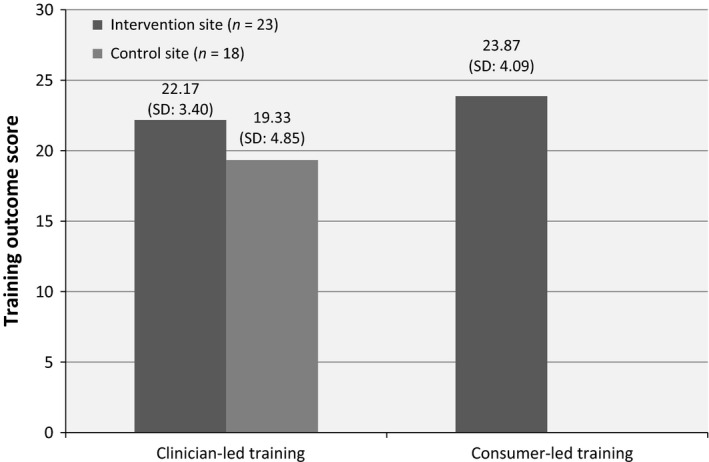
Based on an independent samples t‐test, the scores of training outcomes were significantly greater at the intervention site than at the control site, for the clinician‐led training.
Training relevance
No difference in training relevance was found between sites following the clinician‐led training (Fig. 5). A paired samples t‐test revealed that participants at the intervention site rated training relevance significantly higher for the consumer‐led training than for the clinician‐led training (P < 0.05).
Figure 5.
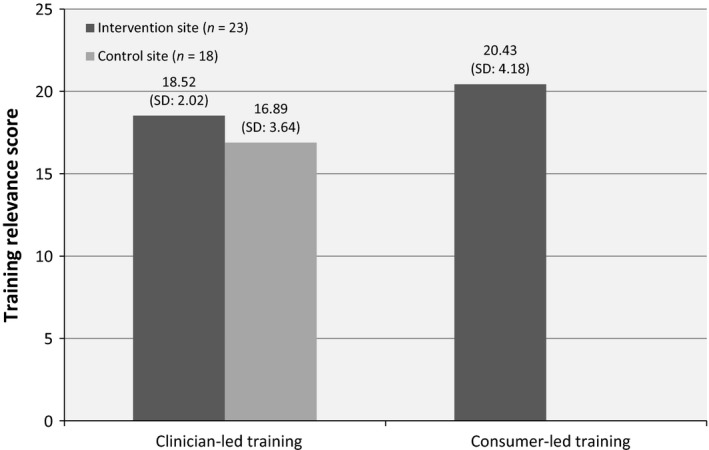
Training relevance scores were not different across sites, for the clinician‐led training. The relevance score of the consumer‐led training was significantly higher than that of the clinician‐led training, at the intervention site.
Discussion
Our study demonstrates that consumer‐led training by people with dual diagnosis has a positive impact on community health staff's understanding and feelings of role adequacy in working with and responding to the needs of people living with dual diagnosis. Furthermore, it appears that the change in understanding created has the potential to be sustained over time for each participant involved. This was reflected in comments made by focus group participants:
I felt the consumer‐led training stuck in my memory a lot more than the first training.
(fg1)
Even if you asked us in three or four months what the consumers talked about, we would be able to recall it.
(fg2)
The maintained levels of understanding which we observed 5 months post‐intervention support previous findings regarding the involvement of consumers on student learning.21 Studies from Klein et al.30 and Wood and Wilson‐Barnett31 have both demonstrated that medical and nursing students who were exposed to consumers showed more empathy and concern about the impact of illness and symptoms upon the patients' lives. In the case of Klein's study, the medical students who had been in contact with patients had maintained their more positive attitude at the 2‐year follow‐up.30 Similarly, O'Reilly et al.32 demonstrated the maintenance over 12 months of decreased stigma and improved attitudes towards the provision of pharmaceutical services to consumers with a mental illness, for pharmacy students who had been exposed to a consumer‐led teaching intervention.
That being said, participants' enhanced understanding and feelings of role adequacy will not remain high by themselves. We could reasonably anticipate that the effects of time, changing roles and staff turnover will slowly lessen the gains observed following the consumer‐led training, unless additional individual and/or organizational training and developmental strategies are put into place. Our study, however, did not seek to evaluate these.
As expected, participants who worked in care‐giving roles, those who spend more of their time responding to dual‐diagnosis issues and/or who had participated in previous dual diagnosis, AOD or mental health‐related training had higher baseline understanding, role adequacy and role legitimacy scores. Consistent with the presence of an AOD team and previous dual‐diagnosis‐focussed capacity building, higher baseline understanding, role adequacy, role legitimacy and personal view scores were also observed at the intervention site. In light of this, it appears that when clinician‐led training is presented in workplaces that already have a history of dual diagnosis (or similar) training and development, this does not result in substantial change – be that in understanding, role adequacy or role legitimacy. In contrast, at the control site where staff had not enjoyed such training and development, a significant shift in their understanding of dual diagnosis was observed. Acknowledging the intervention site as a ‘primed’ environment is an important factor in interpreting the significant increase in understanding following the consumer‐led training. According to intervention site focus group participants, the personal stories shared by consumers living with a dual diagnosis were the main reason for the impact of this form of training:
Personal story, it touches you in places that text book stuff can't.
(fg2)
Furthermore, commenting on the salience of the consumer‐led training, an experienced AOD counsellor commented:
It enlivened me in a way that I haven't had training do that in a long time, because of its real quality, and like, real people talking about their real experience and articulating it so well. Yeah, I was inspired.
(fg2)
The current findings are consistent with other studies looking at reducing stigma and promoting understanding of marginalized and discriminated populations. Findings over the last decade, for example, suggest that contact between the public and members of a minority group (i.e. mental illness, transgender/transsexual) is a more effective strategy to diminish stigma than education alone.33, 34, 35, 36 Furthermore, a meta‐analysis from Pettigrew and Tropp37 suggests that anxiety is reduced and empathy increased following contact with a minority population and that both these changes mediate the reduction in prejudice. Our observation of enhanced staff understanding and role adequacy following contact with people living with dual diagnosis through consumer‐led training is consistent with these previous findings and adds to the current body of evidence.
With regard to role adequacy, neither type of training resulted in significant change when considered in isolation at either study site. The findings suggest that it was the combination of both clinician‐led and consumer‐led training that resulted in an enhanced sense of confidence and role adequacy. This suggests that both types of training were valued, with one complementing the other. An explanation of why this might be the case can again be found from the intervention site focus groups:
She [expert trainer] actually set the scene for the other stuff [consumer‐led training].
(fg1)
I mean, if I had to choose one [training session] it would be consumer, but the two together I thought worked really well.
(fg2)
As both training sessions primarily sought to change participants' perceptions of people living with dual diagnosis and the complexity of their lives, it is not surprising that, overall, no significant increase in participants' sense of role legitimacy was found. Increasing role legitimacy is dependent on the organizational context and limitations of the work performed. Given the range of participant roles in our project, from administration to clinical services, it is to be expected that the training alone may not impact on role legitimacy. Indeed, Skinner et al.38 noted that organizational initiatives and approaches are needed alongside workforce development interventions to enhance workers' sense of role legitimacy. Simply put, organizational‐level change and support are needed for workers to feel confident in the scope of their roles: training on its own is not adequate.
That said, understanding, role adequacy and role legitimacy were all positively and significantly associated. As such, workers with a good understanding of dual diagnosis were more likely to feel adequate when working with people living with dual diagnosis and that they have a legitimate role to play in supporting these consumers. Additionally, understanding, role adequacy and role legitimacy were all positively correlated with training outcomes and training relevance. Emphasizing the prominence of consumer‐led training in particular, one focus group participant commented:
I barely remember exactly the content of the first training but the second one I think about almost every couple of days as I'm seeing clients, I think. You remember what that client said because it impacts on your work.
(fg1)
Personal views, on the other hand, were not linked to either training outcomes or training relevance. This suggests that seeking to merely dispel misconceptions and assumptions might not be enough to create a change in staff's approach to consumers. Rather, to be effective, training should seek to enhance empathy for a particular consumer group,21, 37 understanding of the complex issues they face in everyday life and how best to respond to their needs within a professional environment.15 Personal views did change, but only following the consumer‐led training. The following focus group quote from the intervention site illustrates the increased empathy felt by a participant after they had attended the consumer‐led training:
So I recall seeing this young couple in my local supermarket and clearly they were substance affected with their toddler in the chair and – whereas before I might have been judgemental about them and what they were doing. I remember thinking back to that session when I saw them and thinking about all this other stuff that could be going on in their life.
(fg3)
Finally, training outcomes and training relevance were also significantly correlated. In the light of the significantly higher scores for training outcomes at the intervention site, we can hypothesize again that primed environments are more receptive to training.
Limitations
Our study had a number of limitations. First of all, participant fatigue resulted in substantial attrition at both sites. This meant that our final sample size constrained the range of statistical tests that could be performed with confidence (e.g. within‐group comparisons were not possible). Significant participant attrition is unfortunately not unusual for studies conducted with health professionals using a repeated measures design.39, 40, 41, 42 Common challenges to the continuity of sample size over time include staff turnover and having minimal time and flexibility to accommodate research activities among one's usual clinical duties.41, 42 We also acknowledge that a small sample size may have resulted in a biased data set, with only staff interested in working with people living with dual‐diagnosis participating. However, where applicable and meaningful, appropriate adjustments were made to control for the risk of Type 1 error, that is, Bonferroni corrections. Needless to say, additional research conducted with larger samples and better participant retention rates is needed to confirm and extend the current findings.
Finally, our study did not seek to examine the impact of consumer‐led training on practice change or service users' experiences. Rather, we sought to assess its impact on workers' understanding and role adequacy. Training is only one of many strategies required to create long‐term practice change. For example, it has been shown that for the effects of training to persist and lead to tangible change in consumers' experience and outcomes, organizations must implement complementary strategies such as mentoring and formal support, among others.38, 43, 44 As such, the fact that consumer‐led training was delivered in parallel to other dual‐diagnosis capacity building activities at the intervention site might help to explain the current findings.
Conclusion
Consumer‐led training appears to be a promising and effective approach in enhancing primary health‐care workers' understanding of the issues faced by dual‐diagnosis clients, with the positive effects of such training persisting over time. Used in conjunction with other organizational capacity building strategies, consumer‐led training has the potential to help address one of the key barriers faced by this consumer group to access the services they need. Other sectors, such as mental health, could also benefit from a similar initiative, especially given the current national and state reforms to improve the health‐care workforce's dual‐diagnosis capability.13
Source of funding
Funding for this project was provided under the Evaluating Effectiveness of Participation (EEP) initiative, from the Quality, Safety and Patient Experience Branch of the Victorian Government Department of Health (Melbourne, Victoria, Australia).
Ethical approval
This study was approved by Monash University's Human Research Ethics Committee.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
Special thanks are extended to the passionate consumers who made this project possible; Regina Brindle, Miriam Clarke and Kelly Muldoon from the Association of Participating Service Users; Bronwyn Williams from the Eastern Dual Diagnosis Service (Eastern Health); Adina Heilbrunn for her support with data collection; staff at Manningham Community Health Service who trialled our questionnaire; and to the staff and management who actively supported and participated in the research at Knox Community Health Service and Whitehorse Community Health Service.
References
- 1. Lubman DI, Allen NB, Rogers N, Cementon E, Bonomo Y. The impact of co‐occurring mood and anxiety disorders among substance‐abusing youth. Journal of Affective Disorders, 2007; 103: 105–112. [DOI] [PubMed] [Google Scholar]
- 2. Staiger PK, Thomas AC, Ricciardelli LA, McCabe MP. Identifying depression and anxiety disorders in people presenting for substance use treatment. Medical Journal of Australia, 2011; 195: S60–S63. [DOI] [PubMed] [Google Scholar]
- 3. AIHW . 2010 National Drug Strategy Household Survey Report – Drug Statistics Series No. 25, 25th edn Canberra: Australian Institutes of Health and Welfare, 2011. [Google Scholar]
- 4. Stafford J, Burns L. Australian Drug Trends 2010 – Findings From the Illicit Drug Reporting System (IDRS). Sydney: National Drug and Alcohol Research Centre, University of New South Wales, 2011. [Google Scholar]
- 5. Teesson M, Proudfoot H. Comorbid Mental Disorders and Substance Use Disorders: Epidemiology, Prevention and Treatment. Canberra: Commonwealth Department of Health and Ageing, 2003. [Google Scholar]
- 6. Hunt IM, Kapur N, Robinson J et al Suicide within 12 months of mental health service contact in different age and diagnostic groups: National clinical survey. British Journal of Psychiatry, 2006; 188: 135–142. [DOI] [PubMed] [Google Scholar]
- 7. Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit drug users. Drug and Alcohol Dependence, 2007; 88: 188–196. [DOI] [PubMed] [Google Scholar]
- 8. Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. Journal of Health and Social Behavior, 1997; 38: 177–190. [PubMed] [Google Scholar]
- 9. Todd FC, Sellman JD, Robertson PJ. Barriers to optimal care for patients with coexisting substance use and mental health disorders. Australian and New Zealand Journal of Psychiatry, 2002; 36: 792–799. [DOI] [PubMed] [Google Scholar]
- 10. Staiger PK, Thomas AC, Ricciardelli LA, McCabe MP, Cross W, Young G. Improving servicers for individuals with a dual diagnosis: a qualitative study reporting on the views of service users. Addiction Research and Theory, 2011; 19: 47–55. [Google Scholar]
- 11. Donald M, Dower J, Kavanagh D. Integrated versus non‐integrated management and care for clients with co‐occurring mental health and substance use disorders: a qualitative systematic review of randomised controlled trials. Social Science & Medicine, 2005; 60: 1371–1383. [DOI] [PubMed] [Google Scholar]
- 12. Kavanagh DJ, Greenaway L, Jenner L et al Contrasting views and experiences of health professionals on the management of comorbid substance misuse and mental disorders. Australian and New Zealand Journal of Psychiatry, 2000; 34: 279–289. [DOI] [PubMed] [Google Scholar]
- 13. DHS . Dual Diagnosis: Key Directions and Priorities for Service Development. Melbourne: Victorian Government Department of Human Services, 2007. [Google Scholar]
- 14. Holt M, Treloar C, McMillan K, Schultz L, Schultz M, Bath N. Barriers and Incentives to Treatment for Illicit Drug Users with Mental Health Comorbidities and Complex Vulnerabilities, 61st edn Canberra: Australian Government Department of Health and Ageing, 2007. [Google Scholar]
- 15. Ralley C, Allott R, Hare DJ, Wittkowski A. The use of the repertory grid technique to examine staff beliefs about clients with dual diagnosis. Clinical Psychology & Psychotherapy, 2009; 16: 148–158. [DOI] [PubMed] [Google Scholar]
- 16. Knightbridge SM, King R, Rolfe TJ. Using participatory action research in a community‐based initiative addressing complex mental health needs. The Australian and New Zealand Journal of Psychiatry, 2006; 40: 325–332. [DOI] [PubMed] [Google Scholar]
- 17. Richmond I, Foster J. Negative attitudes towards people with co‐morbid mental health and substance misuse problems: an investigation of mental health professionals. Journal of Mental Health, 2003; 12: 393–403. [Google Scholar]
- 18. Hayward M, West S, Green M, Blank A. Service innovations: service user involvement in training: case study. The Psychiatrist, 2005; 29: 428–430. [Google Scholar]
- 19. Lathlean J, Burgess A, Coldham T et al Experiences of service user and carer participation in health care education. Nurse Education Today, 2006; 26: 732–737. [DOI] [PubMed] [Google Scholar]
- 20. Dogra N, Anderson J, Edwards R, Cavendish S. Service user perspectives about their roles in undergraduate medical training about mental health. Medical Teacher, 2008; 30: e152–e156. [DOI] [PubMed] [Google Scholar]
- 21. Repper J, Breeze J. User and carer involvement in the training and education of health professionals: a review of the literature. International Journal of Nursing Studies, 2007; 44: 511–519. [DOI] [PubMed] [Google Scholar]
- 22. Livingston G, Cooper C. User and carer involvement in mental health training. Advances in Psychiatric Treatment, 2004; 10: 85–92. [Google Scholar]
- 23. Cooper H, Spencer‐Dawe E. Involving service users in interprofessional education narrowing the gap between theory and practice. Journal of Interprofessional Care, 2006; 20: 603–617. [DOI] [PubMed] [Google Scholar]
- 24. Townend M, Tew J, Grant A, Repper J. Involvement of service users in education and training: a review of the literature and exploration of the implications for the education and training of psychological therapists. Journal of Mental Health, 2008; 17: 65–78. [Google Scholar]
- 25. Cook JA, Jonikas JA, Razzano L. A randomized evaluation of consumer versus nonconsumer training of state mental health service providers. Community Mental Health Journal, 1995; 31: 229–238. [DOI] [PubMed] [Google Scholar]
- 26. Young AS, Chinman M, Forquer SL et al Use of a consumer‐led intervention to improve provider competencies. Psychiatric Services, 2005; 56: 967–975. [DOI] [PubMed] [Google Scholar]
- 27. Meehan T, Glover H. Using the recovery knowledge inventory (RKI) to assess the effectiveness of a consumer‐led recovery training program for service providers. Psychiatric Rehabilitation Journal, 2009; 32: 223–226. [DOI] [PubMed] [Google Scholar]
- 28. Addy D, Skinner N, Shoobridge J et al Handbook of the Work Practice Questionnaire (WPQ): A Training Evaluation Measurement Tool for the Alcohol and Other Drugs Field. Canberra: Australian Government Department of Health and Ageing, 2004. [Google Scholar]
- 29. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology, 2006; 3: 77–101. [Google Scholar]
- 30. Klein S, Tracy D, Kitchener HC, Walker LG. The effectiveness of the participation of patients with cancer in teaching communication skills to medical undergraduates: a randomised study with follow‐up after 2 years. European Journal of Cancer, 1999; 35: 1448–1456. [DOI] [PubMed] [Google Scholar]
- 31. Wood J, Wilson‐Barnett J. The influence of user involvement on the learning of mental health nursing students. Nursing Times Research, 1999; 4: 257–270. [Google Scholar]
- 32. O'Reilly CL, Bell JS, Chen TF. Consumer‐led mental health education for pharmacy students. American Journal of Pharmaceutical Education, 2010; 74: 167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Corrigan PW, Larson J, Sells M, Niessen N, Watson AC. Will filmed presentations of education and contact diminish mental illness stigma? Community Mental Health Journal, 2007; 43: 171–181. [DOI] [PubMed] [Google Scholar]
- 34. King ME, Winter S, Webster B. Contact reduces transprejudice: a study on attitudes towards transgenderism and transgender civil rights in Hong Kong. International Journal of Sexual Health, 2009; 21: 17–34. [Google Scholar]
- 35. Corrigan P, Gelb B. Three programs that use mass approaches to challenge the stigma of mental illness. [Review]. Psychiatric Services, 2006; 57: 393–398. [DOI] [PubMed] [Google Scholar]
- 36. Pettigrew TF, Tropp LR. A meta‐analytic test of intergroup contact theory. Journal of Personality and Social Psychology, 2006; 90: 751–783. [DOI] [PubMed] [Google Scholar]
- 37. Pettigrew TF, Tropp LR. How does intergroup contact reduce prejudice? Meta‐analytic tests of three mediators. European Journal of Social Psychology, 2008; 38: 922–934. [Google Scholar]
- 38. Skinner N, Roche AM, Freeman T, Addy D. Responding to alcohol and other drug issues: the effect of role adequacy and role legitimacy on motivation and satisfaction. Drugs: Education, Prevention, and Policy, 2005; 12: 449–463. [Google Scholar]
- 39. Hughes E, Wanigaratne S, Gournay K et al Training in dual diagnosis interventions (the COMO Study): randomised controlled trial. BMC Psychiatry, 2008; 8: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hogh A, Sharipova M, Borg V. Incidence and recurrent work‐related violence towards healthcare workers and subsequent health effects. A one‐year follow‐up study. Scandinavian Journal of Public Health, 2008; 36: 706–712. [DOI] [PubMed] [Google Scholar]
- 41. Ferraz H, Wellman N. Fostering a culture of engagement: an evaluation of a 2‐day training in solution‐focused brief therapy for mental health workers. Journal of Psychiatric and Mental Health Nursing, 2009; 16: 326–334. [DOI] [PubMed] [Google Scholar]
- 42. Estabrook B, Zapka J, Lemon SC. Evaluating the implementation of a hospital work‐site obesity prevention intervention: applying the RE‐AIM framework. Health Promotion Practice, 2012; 13: 190–197. [DOI] [PubMed] [Google Scholar]
- 43. Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. [Review]. The Lancet, 2003; 362: 1225–1230. [DOI] [PubMed] [Google Scholar]
- 44. Miller WR, Mount A. A small study of training in motivational interviewing: does one workshop change clinician and client behavior? Behavioural and Cognitive Psychotherapy, 2001; 29: 457–471. [Google Scholar]


