Abstract
Background
Uptake of colorectal cancer screening programmes needs to be improved or at least maintained in order to achieve projected reductions in mortality and morbidity. Understanding the origins of non‐participation in screening is therefore important.
Objective
To explore the beliefs and experiences of individuals who had not responded either to their screening invitation or reminder.
Design
A qualitative study using in‐depth interviews with non‐participants from England's population‐based colorectal cancer screening programme. Data collection and analysis were carried out using a grounded theory approach, with an emphasis on the constant comparison method, and continued until saturation (27 interviews).
Findings
The interviews provided an in‐depth understanding of a range of reasons and circumstances surrounding non‐participation in screening, including contextual and environmental influences as well as factors specific to the screening test. Non‐participation in screening was not necessarily associated with negative attitudes towards screening or a decision to not return a kit. Reasons for non‐participation in screening included not feeling that participation is personally necessary, avoiding or delaying decision making, and having some degree of intention to take part but failing to do so because of practicalities, conflicting priorities or external circumstances. Beliefs, awareness and intention change over time.
Discussion and conclusions
A range of approaches may be required to improve screening uptake. Some non‐participants may already have a degree of intention to take part in screening in the future, and this group may be more responsive to interventions based on professional endorsement, repeat invitations, reminders and aids to making the test more practical.
Keywords: attitudes, behaviour, beliefs, bowel cancer screening, colorectal cancer screening, non‐participation
Background
Colorectal cancer (CRC) is the third most common cancer, and the second greatest cause of cancer death in the UK, with over 41 000 new cases and 16 000 deaths per year attributable to CRC.1 The 5‐year survival rate for CRC in the UK is currently around 50%, and although this is an improvement upon previous years, it still represents one of the poorest rates in Europe.2
CRC screening was introduced in England in July 2006 and fully implemented by 2010.3 The programme offers biennial guaiac faecal occult blood test (FOBT) screening to men and women aged 60–74 years. The guaiac FOBT kit is completed at home and requires six stool samples taken from three separate bowel motions. Samples need to be collected before they are contaminated with toilet water. Once opened, the kit has to be completed and despatched for testing within 14 days.
Biennial FOBT screening has been shown to reduce CRC mortality by 16%.4 If uptake of 60% is realized, it has the potential to prevent 20 000 deaths in the UK over the next 20 years.5 However, uptake during the first 28 months of the programme was only 54%6, which is lower than other population‐based screening programmes in the UK, and needs to be increased in order to achieve the projected reductions in mortality.
FOBT screening uptake has been shown to be considerably lower among some population subgroups, including men, younger people, ethnic minorities and people with lower educational levels or living in areas of deprivation.6, 7, 8, 9 Low uptake in CRC screening has also been linked to low health literacy, health beliefs and behaviours including cancer fatalism, psychosocial factors such as lack of knowledge about screening, underestimation of CRC risk and negative perceptions of the screening test.7, 10, 11, 12, 13 In addition to the range of deliberative factors associated with uptake of screening, there is also recognition that intentions do not always translate into action (the so‐called ‘intention‐action’ gap). Among individuals who intended to attend for flexible sigmoidoscopy, those who failed to keep their appointment tended to report higher pre‐screening levels of life stress and difficulty as indicated by socioeconomic disadvantage and poor health.14 A variety of interventions to improve uptake have been studied, which have focused mainly on methods of invitation and follow‐up, endorsement by health professionals and supporting materials. In general, these studies have reported modest but discernible impacts on uptake.15, 16, 17, 18, 19, 20, 21, 22
The aims of this study were to explore non‐participation in CRC screening to identify potential mechanisms for improving uptake, through an understanding of the beliefs, health behaviours and decision‐making processes of those who did not respond to their FOBT CRC screening invitation. Existing studies have focused mainly on respondents who have taken part in screening, different cancer sites or CRC screening modalities or have reflected hypothetical reactions to an invitation to screening.23, 24, 25, 26, 27 The focus of this study was on individuals who were able to reflect on their actual decision‐making process and reasons for non‐participation, rather than relying upon hypothetical reactions to a screening invitation. Qualitative methods were chosen to allow maximum opportunity for exploration and inductive hypothesis generation.
Methods
In line with principles of grounded theory,28 our sampling strategy was initially purposive to achieve a maximal variation sample of information‐rich participants. Primary care practices from the North East of England mailed interview invitations to patients who had not returned their FOBT screening kits, as sent from the North East Hub of the screening programme. We recruited through primary care as we hoped that potential participants would be reassured by the study being endorsed by their GP practice and thereby allow us to recruit ‘difficult to reach’ participants. We purposively over‐sampled practices serving areas of high deprivation and with low screening uptake because we anticipated that patients from these practices would be more difficult to recruit and that their accounts were likely to be of particular interest. Participants who volunteered to be interviewed were then selected to ensure variation in terms of age, gender, GP practice and how many screening rounds individuals had been invited to take part in.
Interviews started with a general open‐ended question ‘Could you explain to me your reaction when you received your invitation to take part in screening?’ This allowed general beliefs about the screening programme to be elucidated and the participant to start the interview by telling their ‘non‐participation narrative’ without feeling judged. This open ‘grand tour’ question enabled topics of relevance to the interviewee to be followed up, alongside other prompts covering beliefs associated with the FOBT, CRC screening, reasons for non‐participation, perceived barriers to participation and potential mechanisms for improving uptake. Transcripts were coded following the principles of grounded theory. Initial categories were identified by coding each transcript line by line. These categories were then developed and refined into more general codes by relating categories to each other. Transcripts were coded by a second researcher. Where there were discrepancies, categories were compared and discussed until consensus was reached. The constant comparative method was used to ensure that attention was paid to negative cases as well as the differences and similarities between accounts.28 Recruitment continued in three phases until sufficient accounts were obtained to enable maximum comparison of the themes identified during data collection and that additional data no longer revealed new categories or insights about existing ones.
The reply slip from the invitation to take part in the study included a section to allow those who did not wish to be interviewed to state their reasons for not taking part in screening. These responses were analysed separately and compared to the themes emerging from the main qualitative analysis.
Results
Individuals from 15 family practices (n = 923), who had not responded to their invitation(s) to take part in the CRC screening programme, were mailed an invitation to take part in the study. Of these, 35 agreed to be interviewed, of whom 27 were selected for interview. A further 32 declined interview but provided written reasons for their non‐participation in the screening programme. A separate analysis based on these comments confirmed that we had sampled a full range of accounts within the main interview data in terms of reasons for non‐participation in screening.
Interviewees (14 women and 13 men) varied in terms of working status, number of times invited for screening, reasons for non‐participation and socio‐economic status. A quarter of our interviewees lived within areas belonging to the most deprived quintile in England (based on ranked scores of indices of multiple deprivation); however, our sample also included three interviewees from the least deprived quintile. Ages ranged from 60 to 72 years. None were from an ethnic minority group.
Intention and decision making
Despite none of our interviewees having returned a kit, accounts demonstrated wide differences in reported intention to take part in screening. Only 10 interviewees had not intended to take part in screening, 10 intended to take part and seven had put off making a decision.
A previous decision or lack of decision to take part was not always reflective of future intention or decision making. Processes could change over time and differ between the rounds of invitations sent biennially by the programme. For example, some interviewees, who had decided that screening was appropriate for them, showed an increased strength in intention to take part in the next round after having had time to consider the practicalities and implications of returning a kit and because of their awareness that a previous screening round had been missed.
I don't think I went beyond having a quick glance at the first pack.. when the next one came I was determined to do something about it.. it may be by the time you get the third request, you're in gear, you know in terms of prepared for it and organised for it (B15, male, 62 years).
For others, however, having considered participation the first time round and decided against it meant that less or no consideration was required upon receipt of the second invitation.
It was a quicker decision the second time. The first time I did think about it.. the second time I didn't (B13, female, 66 years).
Although the majority of interviewees reported some degree of intention to participate in screening if invited again, three said that they would not consider future participation. One interviewee felt she may reconsider if the sampling procedures were changed.
Figure 1 illustrates the differences between interviewees in reported decision making and level of intention to take part at the time of their screening invitation and includes examples of related contexts surrounding non‐participation within these categories. This helps to demonstrate that non‐participation in screening is not necessarily due to an uninformed decision‐making process or a lack of understanding of the value of screening.
Figure 1.
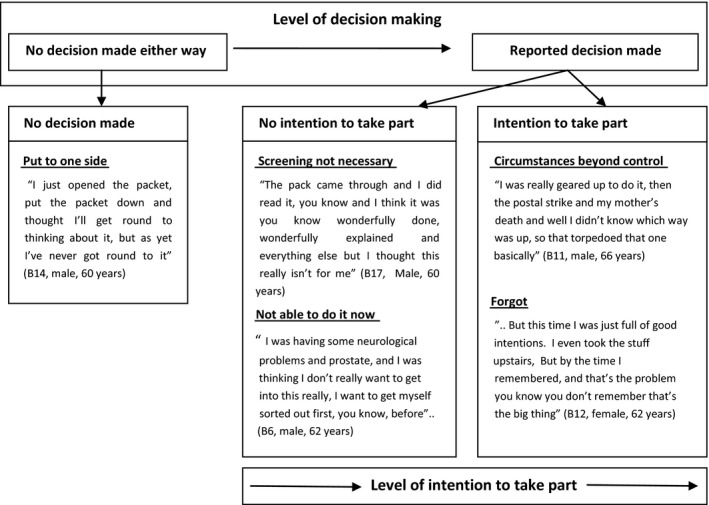
Variation in decision making and intention to take part at invitation, including examples of non‐participation.
A range of difficulties and reasons for non‐participation were described by the interviewees. These ‘barriers’ occured at both the decision‐making stages as well as subsequent to a decision or intention to take part. For example, ‘other health priorities’ were cited as a reason to avoid decision making, deciding not to take part, and as a barrier for those who had already intended to participate (See Table 1).
Table 1.
Other health priorities as a barrier to participation – example of differences in timing of influence
| Other health priorities as a barrier prior to decision making |
| it's just when you're in pain all the time these things don't seem to matter. I know they do matter… I just didn't want to find anything else wrong, head in the sand you know, I just put it to one side and forgot about it to be perfectly honest with you (B16, female, 64 years). |
| Other health priorities as a barrier during decision making |
| there's so many things going on, you know, I have to see a hematologist and I have to see the prostate guy and then the urologist which is slightly different. And I'm thinking well, you know, I don't, I just don't want to get involved in this (screening)’ (B6, male, 62 years). |
| Other health priorities as a barrier after decision making |
| I was well up for it you know, it was just I was just about to do it and then I was rushed into hospital’ (B5, Male, 60 years). |
Influences on screening behaviour that were identified in the interviews are summarized in Table 2. They included psychosocial factors (knowledge, attitudes, beliefs, emotions and the influence of others), contextual factors (conflicting demands and life events, recent health‐care monitoring) and test‐specific factors (the practicalities of the sampling requirements and distaste for the FOBT).
Table 2.
Summary of barriers to participation
| Theme | Open codes |
|---|---|
| Knowledge, beliefs and awareness | Lack of awareness of others who have taken part (social norms difficult to assess) |
| Perceived low awareness of bowel cancer generally and screening programme specifically | |
| Preference to go to GP with symptoms/belief that screening more necessary if symptoms apparent | |
| Belief that treatment is likely to be unsuccessful or that bowel cancer is untreatable | |
| Perception that screening is not personally needed (e.g. lack of symptoms, feeling well) | |
| Unrealistic optimism/low perceptions of risk | |
| Age‐related beliefs (e.g. decreased ability to fight off illness with age) | |
| Perception that it is better not to know (e.g. when there is no interest in receiving treatment) | |
| Traditional male gender roles and beliefs regarding health care and related activities | |
| Bowels are private and not discussed | |
| Belief that rectal bleeding (haemorrhoids or IBD) will affect test results | |
| Emotional reactions to invitation | Disgust/distaste at dealing with faeces |
| Avoidance of decision making (put at back of mind or ignored) | |
| Anxiety and fear about susceptibility, potential cancer diagnosis, further testing and hospitals | |
| Unable to ‘cope’ with additional demands (e.g. due to depression, illness, stressful life events) | |
| Embarrassment/difficult topic to discuss | |
| Lack of need for reassurance | |
| Circumstances | Other more pressing priorities, (stressful life events, health concerns and illness, caring for others) or not prioritising own health |
| Not wanting to waste resources by completing kit unnecessarily | |
| Previous negative experiences of health care and health‐care system | |
| Recent GI medical intervention | Recent colonoscopy or other surveillance procedure |
| Recent bowel cancer diagnosis | |
| Ongoing monitoring or medical review for bowel condition (e.g. IBD) | |
| Practicalities of completing kit | Perceived complexity of sampling procedures |
| Disgust/distaste at dealing with faeces | |
| Lack of understanding of information provided | |
| Unfamiliarity of taking own samples | |
| Inability to take sample due to disability | |
| Need for contemplation, planning and organization | |
| Lack of confidence in being able to carry out sampling procedures | |
| Lack of understanding of whether/when screening is appropriate when under medical review, or recent endoscopy investigations taken place | |
| Not having read the information thoroughly or at all | |
| Practicalities associated with going to the toilet, for example where and when bowel movements take place, regularity of bowel movements | |
| Test seen as unable to provide definitive answer re: cancer diagnosis | |
| Concerns about hygiene (storage, disposal of equipment and posting) |
Psychosocial influences
The importance of cancer screening and early detection was recognized by almost all interviewees. Screening for CRC, specifically, was viewed by all but one interviewee as a ‘good thing to do’, a ‘good opportunity’ and a worthwhile use of NHS resources.
I'm totally convinced of its necessity in the sense that if you're offered something that can save your life, you're stupid to turn it down (B11, male, 66 years).
Positive attitudes towards screening, in principle, were reported even by those who believed that screening was unnecessary for them personally, whether due to recent medical investigations or procedures, feeling ‘well’ and not experiencing bowel symptoms, or a preference to rely on symptom detection. Interviewees who had intended to take part often struggled to reconcile their beliefs about the importance of screening with their own non‐participation. Some found their non‐participation in screening more difficult to rationalize than others, and for some, was associated with feelings of guilt. Study participants varied widely in their levels of health literacy. Although we did not specifically request occupational information, interviewees volunteered this information within their accounts as they felt it helped to explain their attitudes towards screening, particularly for those who were currently or previously employed as health professionals, including two who had cared for patients with CRC. Many interviewees, particularly the women, were keen to impress that they took care of their health and were regular attenders for other health and screening checks.
Most interviewees reported a perceived lack of knowledge about the condition. This was the case even among those who had friends or relatives with a CRC diagnosis. Specific awareness of the programme was low, and only five of the interviewees had some prior knowledge of it when they had received their first kit in the post. Interviewees commented that it had arrived ‘out of the blue’ or they had been surprised at both having received the invitation to take part as well as the procedures that they were being asked to undertake, which were often described as ‘unfamiliar’ or ‘alien’. The people we spoke to would have received their first invitation to take part in screening during the very early phases of the screening programme in England. Awareness of the screening programme was reported to be increasing over time. Although all our interviewees should have received a letter 2 weeks before their kit arrived advising them this was going to be received, this was rarely mentioned or remembered. Those who described receiving a warning letter still felt unprepared for what was being asked of them when the kit had arrived.
Accounts showed variation in the level of personal reflection and consideration of the consequences of taking part in screening. When they were considered, these centred not only on the benefits of early detection, but also on more negative potential consequences such as anticipated anxiety associated with waiting for and receiving results, fear of a potential cancer diagnosis, and fear or avoidance of further testing treatment and hospital visits. The potential need for a colonoscopy after FOBT provoked anxiety and specifically acted as a deterrent for some interviewees. Consideration of the consequences of screening was, nevertheless, not always associated with a lack of intention to take part. This was often rationalized as part of a normal decision‐making process, involving natural anxiety over the contemplation of an intrusive test and a potential cancer diagnosis alongside the benefits of early detection.
They're not the nicest of tests to have I believe (endoscopy), if they did say ‘come back there is a problem,’ I would get very anxious about having those tests done, there's no doubt about it but you've got to do these things haven't you? (B25, female, 67 years).
Influence of others
Accounts demonstrated how others had influenced interviewees’ decision making or future intention by, for example, changing associated beliefs or social norms in relation to screening behaviour. This occurred in a number of ways, including: personal experience of friends and relatives diagnosed with bowel cancer; awareness of others invited or who had taken part in screening; and encouragement (or lack or) from family and friends.
we heard of a dear friend who has been picked up as having bowel polyps as a result of this screening, so I was completely reinforced in the urgency and necessity of all of this and have no question about it at all, in principle (B11, Male, 66 years).
One interviewee described how her own CRC diagnosis, subsequent to her non‐participation in screening, had prompted her neighbour to request another screening kit.
The perceived social acceptability of talking about CRC with others was an important subtheme in this area. Cancer was a topic that was felt to be difficult and frightening to discuss generally. There was acknowledgement, nevertheless, that this was more openly discussed than it used to be, particularly among the age group involved in screening. Health concerns could also be discussed more openly with age, particularly for the men. Public awareness about CRC was perceived to be lower than for other more ‘common’ cancers. Breast and cervical cancer, in particular, were most commonly and openly discussed by the women, usually in the context of screening, as was prostate cancer by the men.
so in a blokey, jokey kind of way, that (prostate cancer) is something that you, well not so much discuss as, it's a kind of male acknowledgement that it's going on,.. but we can make a joke of it and have another pint, but I don't think that would be the case for bowel cancer (B11, male, 66 years).
The practical requirements of completing and returning a kit, and bowels or bowel movements, were perceived as embarrassing and difficult to broach. Embarrassment and reluctance to talk to others in the household about the screening process was a problem for some, particularly as completion of the kit, which includes storage and disposal of equipment, is difficult to carry out in a totally private manner. On the other hand, screening was also viewed to be possibly beneficial as it could help to avoid future embarrassment associated with having to consult a GP with symptoms.
None of the people we spoke to had discussed their participation in screening with a health professional, even those who reported having contact for other reasons around the time of their invitation, and this included individuals who were unsure about their need to take part. Neither had they considered their need for information sufficient enough to contact the screening hub for advice. Some interviewees suggested, however, that they may have taken part in screening if they had been advised to do so by their doctor and saw their family practice as an appropriate place for screening‐related activity. Being able to hand in completed kits or collect additional resources or equipment to help with sampling procedures from their local surgery are examples of some of the suggestions provided.
Contextual influences
Conflicting priorities or events were the most commonly mentioned ‘reasons’ for not having returned a kit among those who had not actively decided against taking part. Other health priorities included acute and chronic health conditions as well as mental health issues and health or cancer ‘scares’. Additional influences were associated with stressful life events, such as bereavement, caring for others, work or other time pressures. These became barriers to participation when the individual felt unable to manage additional pressure or demands, were unable to physically manage the requirements of screening procedures, for example during a flare‐up of arthritis, or when they did not have easy access to the kit because of life events. The perceived complexity and unfamiliar nature of the procedures required to participate in screening, which are discussed in more detail below, became more of a barrier at these times. One interviewee, for example, described how mild depression and dealing with stressful family events had meant she had not felt capable of taking in the information provided despite her positive attitudes towards screening.
Yeah, I mean normally I cope with things, and then when I saw that (screening invitation), and it was just let's be honest, I'm not going to blame anything other than myself because I could have sat down and just given it half an hour to work out what I had to do. But I didn't. …when I opened it all up I thought god this looks complicated, and I didn't really read it properly’ (B24, female, 62 years).
Arrival of the screening kit at a ‘bad time’ was usually associated with delayed decision making, or a decision not to take part at that particular time, rather than an intention not to take part in screening at all.
Test‐specific influences
Interviewees’ accounts demonstrated that the processes involved in collecting stool samples required a certain amount of planning and consideration. Most interviewees who had intended to complete their kit described ‘mentally rehearsing’ these processes, but many did not feel at all confident in their ability to complete their kit correctly. Commonly mentioned issues included suitable equipment to catch the stools with, avoidance of contamination with toilet water, hygienic disposal of any equipment used, storage of the kit and having required equipment when and where it was needed.
I thought about it and then I thought, I can't practically do this at work. You know, I mean the mechanics would be sort of putting newspaper or something in the toilet bowl and taking the sample from there and then you've got to dispose of the newspaper which wouldn't be a problem at home (B15, male, 62 years).
Other practical concerns related to the time required to take each sample, remembering to complete the kit and completing all the samples within the required time frame. Women, in particular, compared the process to other screening programmes which were perceived to require less ‘consideration’ and preparation.
It's not like your smears or mammograms or anything like that. You get an appointment you do it and that's a lot easier.. you go, you get it done, that's it.. This is actually having to organise yourself and I think that's more difficult…. You can almost join in the rest of the screening programmes quite mindlessly if you know what I mean. (B12, Female, 62 years).
Interviewees who had recently undergone colonoscopy or had had a recent bowel cancer diagnosis demonstrated some confusion over whether or when they needed to complete a screening kit and how to ‘opt out’ of the screening process. There was, in particular, a reluctance to waste health‐care resources by completing kits unnecessarily or appear to be a ‘bad patient’ by not responding to their invitation.
Distaste, embarrassment and hygiene concerns associated with having to deal with faeces were mentioned by everyone interviewed. The majority, however, did not feel this was a major concern and were keen to highlight that it had not been the main reason for their non‐participation. For most interviewees the procedures involved in providing three samples in a hygienic manner, including disposal of equipment needed and storage of samples, was more problematic than the distaste of dealing with faeces per se. Some, however, did report that ‘distaste’ was a particular problem, and four interviewees reported this had been the main reason for their non‐participation. For a minority of participants, hygiene concerns about putting the samples in the post were also off putting.
Discussion
This study provides in‐depth insights into the perspectives of non‐participants in the English CRC screening programme. These individuals were uniquely able to reflect upon their actual decision making and actions taken in response to their screening invitation. We found that non‐participation is not necessarily associated with negative attitudes towards screening or a decision to not return a kit. Individuals who do not participate on any one round have a range of reasons, including not feeling that participation is personally necessary (which in some cases would be viewed as medically justified, for example, those who have had a recent colonoscopy prior to their screening invitation), avoiding or delaying decision making, and having some degree of intention to take part but failing to do so because of practicalities, conflicting priorities or external circumstances.
Attitudes towards the FOBT and required sampling procedures were varied, but a common theme was low confidence in the ability to carry out the required sampling procedures. The test was consistently seen as distasteful, inconvenient, embarrassing to discuss and unhygienic, although many interviewees made clear that this had not been the primary barrier to participation.
Our result extends findings from a previous interview study on experiences of screening and decision making23 by including perspectives from a wider sample of non‐participants with variation in their reasons for non‐participation, socio‐economic status, number of invitations, gender and beliefs about their own need for screening. Other qualitative research in the UK, although of relevance, has been based on flexible sigmoidoscopy screening or has focused on intention and decision making rather than actual participation,25, 26 and the transferability of findings from other countries,29 or screening programmes, is not always clear.
We had anticipated from the outset that this would be a difficult group of respondents to recruit. Every effort was made to ensure that the invitation to take part in the study provided assurances that the study researchers would be objective and non‐judgmental and would not be making any screening‐related recommendations. As this was a qualitative study, we were not aiming to achieve representativeness, but to gain an understanding of the contexts, processes and meanings attached to non‐participation in bowel cancer screening in a sample of volunteers who were able to reflect upon their actual decision making and actions taken in response to their screening invitations. The low response to our invitation to participate could, however, be argued to represent a potential bias in the type of respondents we were able to include, with those with negative attitudes to screening or who find the topic embarrassing to discuss being less likely to take part in our study, for example. The accounts from the people we spoke to, nevertheless, seem to have been open and honest and demonstrated varying degrees of difficulty and embarrassment when talking about bowels, bowel movements and their personal experiences of cancer. Variation was also evident in their reasons for non‐participation, decision making and intention to take part, despite their non‐participation, and even for those with generally positive attitudes towards cancer screening in principle. High levels of positive attitudes towards screening in principle have been reported by others.24, 25, 26, 30, 31 For example, in a UK quantitative survey,31 only 1.1% reported they would be definitely not interested in taking part in FOBT screening, demonstrating generally positive attitudes which are not reflected in actual uptake. Despite limitations, our findings allow useful insights into decision‐making processes and behaviours which are currently not well understood and which would otherwise be difficult to obtain.
Further quantitative research would be required to ascertain the proportion of non‐participants who may benefit from the suggestions for improving uptake from our interviewees and analysis, the frequency of reasons for non‐participation within this population and the views of people from ethnic minority groups who are reported to have lower uptake rates and who were not represented in this study.
Confidence in our findings is further strengthened by the fact that all the reasons for non‐participation in screening provided to us by respondents declining interview emerged unprompted within the interviews and that our findings allow elaboration of themes identified in other qualitative and quantitative studies,23, 24, 30, 31, 32, 33, 34, 35 including, for example, an appreciation of a ‘public responsibility’ to participate in population screening programmes and a reluctance to be seen as using NHS resources inappropriately, both attitudes that have been reported by others.23, 24 In addition, however, our findings also showed that many of the reasons provided for taking part in screening, such as positive experience of women's screening programmes and encouragement from others,23 are also reported by those who do not return a kit. As would be expected, our findings confirm the relevance of concepts from existing models of health behaviour within this setting and their potential as a foundation for interventions to improve uptake.27, 34, 35, 36, 37
Interviewees who held strong beliefs about the importance of screening or described more ‘emotional’ responses to the screening request tended to find ‘rationalising’ their non‐participation during the interview more difficult and often reported a degree of guilt or self‐blame for not having taken up the opportunity of screening provided to them. Available information or existing knowledge about risks and benefits of screening, when taken into account at all, appears to be considered in the light of other influences, including wider social contexts, practicalities and pressures of daily life. This reflects the conclusion from previous work that ‘informed choice’ in the context of screening is conceptualized differently by lay people and policymakers.32 Although lack of knowledge and understanding have a role in decision making and screening uptake,12, 31, 38 our findings indicate that these factors are not sufficient. Similar conclusions were reached in a study from the United States,39 and studies from Germany and Australia have shown that interventions to improve informed choice had either no effect or a detrimental one on uptake.32, 40
Improved understanding and information may be beneficial, however, to ensure that people's decisions to take part in CRC screening are not based on the presence or absence of bowel symptoms. There may also be a related concern that people who do proceed to screening and have a negative screening test result may then dismiss symptoms that develop later, an issue which is the subject of a current Cancer Research UK funded project.
In contrast to a prevailing view that better information is key to improving uptake, the most commonly mentioned suggestions from interviewees in this study related to practical issues, including the provision of different kits or aids to help collect (and in particular catch) their stool with and avoiding contamination with toilet water. Timing was also an issue. Other types of FOBT kits exist, which require fewer samples or allow the stool to be sampled in the toilet water. Different test requirements may have helped at least some of the people we spoke to overcome their lack of confidence in providing a sample correctly and in a hygienic manner. Other studies have also identified a preference for, and higher participation rates with, an immunochemical FOBT, which requires only one sample, compared to the gFOBT.29, 41, 42, 43 Simplifying the test requirements could also benefit uptake by helping to minimize the impact of other inevitable and conflicting priorities and life events on screening behaviour.
The majority of our interviewees had not expected to receive their invitation and described it as arriving ‘out of the blue’ or ‘an invasion of privacy’. Some suggested that more warning and time to consider the practicalities of sampling would have been beneficial. Findings from the Netherlands suggest that sending an advance notification letter significantly improves uptake,44 yet the letter sent prior to the kit by the screening programme was very rarely remembered or referred to during our interviews.
None of our interviewees had discussed participation with a health professional, although there were indications that some may have been more inclined to take part if they had been advised to do so by their doctor. This is consistent with findings from a recent trial which demonstrated that endorsement letters from GPs and enhanced procedural leaflets could increase uptake by 10%.18
Conclusions
A range of different approaches may be required to improve uptake in CRC screening depending on the experiences, circumstances, beliefs and existing levels of intention of non‐participants. Our findings show that some individuals who do not participate in CRC screening have a positive attitude to screening in principle and may already have a degree of intention to take part despite not having responded to previous screening invitations. Interventions are needed that can help convert this intention into action. Focusing solely on the way information is presented is unlikely to be productive in this group. These individuals are more likely to respond to professional endorsement, repeat invitations, reminders and aids to making the test more practical. Changing the screening test to one with simpler sampling requirements could reduce the perceived barriers at the decision‐making stage as well as the actual difficulties encountered, thus minimizing the inevitable impact of conflicting priorities and life events.
Ethical and governance considerations
The study was carried out in full accordance with NHS Research Governance regulations. Ethical approval was obtained from the University of Durham, appropriate Local Research Ethics Committees and Primary Care Trusts. Confidentiality of data was assured, and all transcripts and subsequent reports have been anonymized. Written informed consent was obtained from all participants.
Source of funding
This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB‐PG‐0609‐19082). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Conflict of interests
None.
Acknowledgements
Thanks are due to the North East Hub of the BCSP, PCRN N&Y and the GP practices for assisting us with participant recruitment, as well as to all the interview participants for sharing their experiences and time with us.
References
- 1. CRUK . Bowel cancer statistics. Available at: http://www.cancerresearchuk.org/cancer-info/cancerstats/types/bowel/: Cancer Research UK; accessed 13 December 2012.
- 2. Coleman MP, Forman D, Bryant H et al Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of population‐based cancer registry data. The Lancet, 2011; 377: 127–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Programmes NCS . NHS Bowel Cancer Screening Programme. Available at: http://www.cancerscreening.nhs.uk/bowel/, accessed 13 December 2012.
- 4. Hewitson P, Glasziou P, Irwig L, Towler B, Watson E. Screening for colorectal cancer using the faecal occult blood test, Hemoccult. Cochrane Database of Systematic Reviews, 2007; (1): CD001216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Parkin DM, Tappenden P, Olsen AH, Patnick J, Sasieni P. Predicting the impact of the screening programme for colorectal cancer in the UK. Journal of Medical Screening, 2008; 15: 163–174. [DOI] [PubMed] [Google Scholar]
- 6. von Wagner C, Baio G, Raine R et al Inequalities in participation in an organized national colorectal cancer screening programme: results from the first 2.6 million invitations in England. International Journal of Epidemiology, 2011; 40: 712–718. [DOI] [PubMed] [Google Scholar]
- 7. Javanparast S, Ward P, Young G et al How equitable are colorectal cancer screening programs which include FOBTs? A review of qualitative and quantitative studies. Preventive Medicine, 2010; 50: 165–172. [DOI] [PubMed] [Google Scholar]
- 8. Moss SM, Campbell C, Melia J et al Performance measures in three rounds of the English bowel cancer screening pilot. Gut, 2012; 61: 101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Weller D, Coleman D, Robertson R et al The UK colorectal cancer screening pilot: results of the second round of screening in England. British Journal of Cancer, 2007; 97: 1601–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hiatt R, Wardle J, Vernon S et al Workgroup IV: public education. UICC International Workshop on Facilitating Screening for Colorectal Cancer, Oslo, Norway (29 and 30 June 2002). Annals of Oncology, 2005; 16: 38–41. [DOI] [PubMed] [Google Scholar]
- 11. Miles A, Simon A, Wardle J. Answering patient questions about the role lifestyle factors play in cancer onset and recurrence: what do health care professionals say? Journal of Health Psychology, 2010; 15: 291–298. [DOI] [PubMed] [Google Scholar]
- 12. von Wagner C, Semmler C, Good A, Wardle J. Health literacy and self‐efficacy for participating in colorectal cancer screening: the role of information processing. Patient Education and Counseling, 2009; 75: 352–357. [DOI] [PubMed] [Google Scholar]
- 13. Wender RC. Barriers to screening for colorectal cancer. Gastrointestinal endoscopy clinics of North America, 2002; 12: 145–170. [DOI] [PubMed] [Google Scholar]
- 14. Power E, Van Jaarsveld CHM, McCaffery K, Miles A, Atkin W, Wardle J. Understanding Intentions and Action in Colorectal Cancer Screening. Annals of Behavioural Medicine, 2008; 35: 285–294. [DOI] [PubMed] [Google Scholar]
- 15. Cole SR, Young GP, Byrne D, Guy JR, Morcom J. Participation in screening for colorectal cancer based on a faecal occult blood test is improved by endorsement by the primary care practitioner. Journal of Medical Screening, 2002; 9: 147–152. [DOI] [PubMed] [Google Scholar]
- 16. Federici A, Valle S, Rossi PG, Grassi A, Borgia P, Guasticchi G. Colorectal cancer screening: recommendations and guideline adherence by physicians from digestive endoscopy centers in the Lazio region, Italy. Preventive Medicine, 2006; 43: 183–186. [DOI] [PubMed] [Google Scholar]
- 17. Gimeno‐Garcia AZ, Quintero E, Nicolas‐Perez D, Parra‐Blanco A, Jimenez‐Sosa A. Impact of an educational video‐based strategy on the behavior process associated with colorectal cancer screening: a randomized controlled study. Cancer Epidemiology, 2009; 33: 216–222. [DOI] [PubMed] [Google Scholar]
- 18. Hewitson P, Ward AM, Heneghan C, Halloran SP, Mant D. Primary care endorsement letter and a patient leaflet to improve participation in colorectal cancer screening: results of a factorial randomised trial. British Journal of Cancer, 2011; 105: 475–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Libby G, Bray J, Champion J et al Pre‐notification increases uptake of colorectal cancer screening in all demographic groups: a randomized controlled trial. Journal of Medical Screening, 2011; 18: 24–29. [DOI] [PubMed] [Google Scholar]
- 20. Myers RE, Sifri R, Hyslop T et al A randomized controlled trial of the impact of targeted and tailored interventions on colorectal cancer screening. Cancer, 2007; 110: 2083–2091. [DOI] [PubMed] [Google Scholar]
- 21. Siddiqui MRS, Sajid MS, Khatri K, Kanri B, Cheek E, Baig MK. The role of physician reminders in faecal occult blood testing for colorectal cancer screening. The European Journal of General Practice, 2011; 17: 221–228. [DOI] [PubMed] [Google Scholar]
- 22. Steele RJC, Kostourou I, McClements P et al Effect of repeated invitations on uptake of colorectal cancer screening using faecal occult blood testing: analysis of prevalence and incidence screening. British Medical Journal, 2010; 27: 341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chapple A, Ziebland S, Hewitson P, McPherson A. What affects the uptake of screening for bowel cancer using a faecal occult blood test (FOBt): a qualitative study. Social Science & Medicine, 2008; 66: 2425–2435. [DOI] [PubMed] [Google Scholar]
- 24. Jepson RG, Hewison J, Thompson A, Weller D. Patient perspectives on information and choice in cancer screening: a qualitative study in the UK. Social Science & Medicine, 2007; 65: 890–899. [DOI] [PubMed] [Google Scholar]
- 25. McCaffery K, Borril J, Williamson S et al Declining the offer of flexible sigmoidoscopy screening for bowel cancer: a qualitative investigation of the decision‐making process. Social Science & Medicine, 2001; 53: 679–691. [DOI] [PubMed] [Google Scholar]
- 26. O'Sullivan I, Orbell S. Self‐sampling in screening to reduce mortality from colorectal cancer: a qualitative exploration of the decision to complete a faecal occult blood test (FOBT). Journal of Medical Screening, 2004; 11: 16–22. [DOI] [PubMed] [Google Scholar]
- 27. Wardle J, Sutton S, Williamson S et al Psychosocial influences on older adults' interest in participating in bowel cancer screening. Preventive Medicine, 2000; 31: 323–334. [DOI] [PubMed] [Google Scholar]
- 28. Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, 3rd edn London: Sage Publications, 2008. [Google Scholar]
- 29. Clavarino AM, Janda M, Hughes KL et al The view from two sides: a qualitative study of community and medical perspectives on screening for colorectal cancer using FOBT. Preventive Medicine, 2004; 39: 482–490. [DOI] [PubMed] [Google Scholar]
- 30. van Rijn AF, van Rossum LGM, Deutekom M et al Low priority main reason not to participate in a colorectal cancer screening program with a faecal occult blood test. Journal of Public Health, 2008; 30: 461–465. [DOI] [PubMed] [Google Scholar]
- 31. McCaffery K, Wardle J, Waller J. Knowledge, attitudes, and behavioral intentions in relation to the early detection of colorectal cancer in the United Kingdom. Preventive Medicine, 2003; 36: 525–535. [DOI] [PubMed] [Google Scholar]
- 32. Steckelberg A, Huelfenhaus C, Haastert B, Muehlhauser I. Effect of evidence based risk information on “informed choice” in colorectal cancer screening: randomised controlled trial. British Medical Journal, 2011; 342: d3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sutton S, Wardle J, Taylor T et al Predictors of attendance in the United Kingdom flexible sigmoidoscopy screening trial. Journal of Medical Screening, 2000; 7: 99–104. [DOI] [PubMed] [Google Scholar]
- 34. Wardle J, McCaffery K, Nadel M, Atkin W. Socioeconomic differences in cancer screening participation: comparing cognitive and psychosocial explanations. Social Science and Medicine, 2004; 59: 249–261. [DOI] [PubMed] [Google Scholar]
- 35. Costanza ME, Luckmann R, Stoddard AM et al Applying a stage model of behavior change to colon cancer screening. Preventive Medicine, 2005; 41: 707–719. [DOI] [PubMed] [Google Scholar]
- 36. Manne S, Markowitz A, Winawer S et al Correlates of colorectal cancer screening compliance and stage of adoption among siblings of individuals with early onset colorectal cancer. Health Psychology, 2002; 21: 3–15. [PubMed] [Google Scholar]
- 37. Sifri R, Rosenthal M, Hyslop T et al Factors associated with colorectal cancer screening decision stage. Preventive Medicine, 2010; 51: 329–331. [DOI] [PubMed] [Google Scholar]
- 38. Robb KA, Power E, Atkin W, Wardle J. Ethnic differences in participation in flexible sigmoidoscopy screening in the UK. Journal of Medical Screening, 2008; 15: 130–136. [DOI] [PubMed] [Google Scholar]
- 39. Weinberg DS, Miller S, Rodoletz M et al Colorectal cancer knowledge is not associated with screening compliance or intention. Journal of Cancer Education, 2009; 24: 225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Smith SK, Trevena L, Simpson JM, Barratt A, Nutbeam D, McCaffery KJ. A decision aid to support informed choices about bowel cancer screening among adults with low education: randomised controlled trial. British Medical Journal, 2010; 26: 341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Federici A, Rossi PG, Borgia P, Bartolozzi F, Farchi S, Gausticchi G. The immunochemical faecal occult blood test leads to higher compliance than the guaiac for colorectal cancer screening programmes: a cluster randomized controlled trial. Journal of Medical Screening, 2005; 12: 83–88. [DOI] [PubMed] [Google Scholar]
- 42. van Rossum LG, van Rijn AF, Laheij RJ et al Random comparison of guaiac and immunochemical fecal occult blood tests for colorectal cancer in a screening population. Gastroenterology, 2008; 135: 82–90. [DOI] [PubMed] [Google Scholar]
- 43. vonWagner C, Good A, Smith SG, Wardle J. Responses to procedural information about colorectal cancer screening using faecal occult blood testing: the role of consideration of future consequences. Health Expectations, 2011; 15: 176–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. van Roon AHC, Hal L, Wilschut JA et al Advance notification letters increase adherence in colorectal cancer screening: a population‐based randomized trial. Preventive Medicine, 2011; 52: 448–451. [DOI] [PubMed] [Google Scholar]


