Abstract
Background
Informed decision making is recognized as important in screening. Invitees should be provided with relevant information, enabling them to make an informed decision. This may be more difficult in ethnic minority and low socio‐economic status groups. We aimed to assess the proportion of informed decisions to participate in a faecal immunochemical test (FIT)‐based colorectal cancer (CRC) screening pilot and to explore differences in knowledge and attitude across various subgroups.
Methods
Asymptomatic persons aged 50–74 were invited to a second round of a Dutch FIT‐based pilot screening programme for CRC. An information leaflet containing all information relevant to enable informed decision making accompanied the invitation. Informed choice was assessed by a mailed questionnaire. Knowledge was elicited through 18 items and attitude towards screening through four items. Main outcome measure was the proportion of informed decision makers among participants. Differences between subgroups were evaluated using logistic regression.
Results
Of 5367 screening participants, 2774 (52%) completed the questionnaire. Knowledge was adequate in 2554 (92%); 2736 (99%) showed a positive attitude towards screening. A total of 2525 persons had made an informed choice (91%); male gender, low education level, non‐Dutch ethnicity and not speaking Dutch at home were negatively associated with having adequate knowledge in multivariable analysis.
Conclusion
In FIT‐based screening for CRC, the majority of responders made an informed decision to participate. However, we did not succeed in equally providing all population subgroups with sufficient information. Future initiatives should be aimed at reaching these groups to further enable informed decision making.
Keywords: attitude, colorectal cancer, informed decision making, knowledge, prevention, screening
Introduction
Mass screening programmes for colorectal cancer (CRC) are aimed at decreasing disease‐related morbidity and mortality. In any mass screening programme, high participation rates are desirable because the effectiveness of screening depends on the proportion of persons that choose to participate. However, it is even more important to achieve a high informed participation rate; the choice to accept the invitation to participate should be a well‐balanced decision free from coercion.
One of the criteria of the UK National Screening Committee for appropriateness of screening is that evidence‐based information, explaining the consequences of testing, investigation and treatment, should be made available to potential participants to assist them in making an informed choice.1 This includes information on harms and benefits of the initial screening test and of possible follow‐up tests and treatments or interventions. Possible harms include complications of investigations of screen‐detected abnormalities, increased morbidity and mortality from side‐effects, overdetection (identification of disease that would not have become symptomatic in the absence of screening) and adverse psychosocial effects.2
Although providing potential screenees with adequate information is a prerequisite for enabling informed decision making, previous studies in the fields of CRC, prostate, lung and cervical cancer screening have shown that it can be difficult to adequately reach all those eligible for screening.3, 4, 5, 6, 7 According to the definition of Marteau,8 a decision based on adequate knowledge alone is not enough to classify as informed. In addition, actual screening behaviour should reflect a person's attitude towards screening.
Although several countries worldwide have stool test based nationwide screening programmes for CRC in place or are on the verge of implementing such a programme, no data exist on the actual number of informed decisions in an average risk population invited for screening with the faecal immunochemical test (FIT). We aimed to evaluate the proportion of informed decision makers among participants in a second round of a FIT‐based CRC screening pilot in the Netherlands. We also explored differences in determinants of informed decision making – knowledge and attitude – between various subgroups based on demographic and socio‐economic characteristics.
Methods
Data were collected in the second round of a Dutch faecal immunohistochemical test (FIT)‐based CRC screening pilot in the Amsterdam region. In the first screening round, that was conducted 2 years previously, the same group of persons was approached for participation.9 In this first round, invitees were randomized to FIT or guaiac stool test. Because our results showed that the FIT had better test characteristics and test acceptability, only this test was used in the second round. The programme design has been published in detail elsewhere.10 A summary will be given below.
Design of the second round of the screening pilot
A random sample of average risk persons aged 50–75, living in the screening pilot catchment area, was selected from the population database based on date of birth and postal code and sent an invitation package for the second screening round. Institutionalized persons were excluded from participation. The invitation package included an invitation letter, an information leaflet, a frequently‐asked‐questions card, an illustrated test instruction and the actual stool test. All information material was developed in close relation with a linguistic expert from the patient education department of our institution.
Stool test
The FIT that was used was the OC‐Sensor by Eiken (Tokyo, Japan). Invitees were instructed to perform the test at home by swapping a small brush through their stool. The brush could then be put back in the sample bottle and could be returned to the laboratory in a postage free envelope by regular mail. After arrival at the laboratory, tests were stored at 4°C and processed in batches using an automated clinical analyzer (OC‐Sensor Micro®; Eiken). A single test was used at one occasion and a haemoglobin value of 50 ngHb/ml was used as threshold for test positivity.
Invitation letter
The invitation letter included detailed information on the background of screening and on the screening procedure itself emphasizing the voluntary basis of participation. Invitees were instructed not to take part in screening but to contact their general practitioner in case of bloody stool and/or changed bowel habits during the last 3 months. The information package further emphasized that screening by faecal tests relies on repeated participation every 2 years. To enable informed decision making about participation, invitees were referred to the accompanying leaflet for additional information.
Information leaflet
The content of the information leaflet was developed according to Marteau's8 principles of informed decision making. For screening in general, these principles stipulate that invitees should be provided with information on at least eight domains including aim of screening; disease that is screened for; prevalence in the general population of disease that is screened for; screening test; meaning of a high‐risk test result; meaning of a low‐risk test result; possible side‐effects of screening; detection rate; follow‐up after a high‐risk test result; possible findings at follow‐up investigations; follow‐up after detection of disease and finally the voluntary basis of participation.11, 12, 13 An expert panel consisting of four members was formed to decide on what information would be indispensable to enable informed decision making in the context of FIT screening, based on the eight domains described above. The wording of the information leaflet was done in close relation with a linguistic expert specialized in patient information provision. First drafts of the leaflet were then presented to a convenience sample of 10 hospital patients to check for clarity and were adjusted according to their feedback. The information leaflet was available in Dutch only.
Informed choice questionnaire
Knowledge and attitude were elicited with a questionnaire that was sent to all invitees 2 weeks after the invitation.
Knowledge
Knowledge was assessed with 18 items (Table 2). These items were developed by an expert panel consisting of two gastroenterologists, and two clinical epidemiologists experienced in the field of screening. Items were selected to cover all of the eight knowledge domains described above. These could be broadly organized into general items (six items) and into items specific to the screening procedure (12 items). Knowledge items were formulated as statements that could be scored as ‘correct’ or ‘incorrect’. A correct answer was scored 1 and an incorrect answer 0. For each person, a summary knowledge score was calculated, ranging from 0 to 18. In addition, separate general knowledge scores (ranging from 0 to 6) and screening specific knowledge scores (ranging from 0 to 12) were calculated.
Table 2.
Proportion of correct answers on 18 knowledge items (n = 2774)
| Question | Correct answer, n (%) | Significance of the difference in proportion of correct responses | ||
|---|---|---|---|---|
| General items | Education | Ethnicity | Gender | |
| A mass screening programme can detect CRC before it becomes symptomatic (correct) | 2518 (91) | |||
| CRC has a better chance of survival when detected in an early stage (correct) | 2771 (99.9) | * | ||
| Persons can die from CRC when not treated on time (correct) | 2613 (94) | |||
| CRC can be hereditary (correct) | 2038 (74) | ** | * | |
| CRC is one the most prevalent cancers in the Netherlands (correct) | 1921 (69) | * | ||
| Younger persons have a higher chance of being diagnosed with CRC than older persons (incorrect) | 2670 (96) | ** | ||
| Screening items | ||||
| In the absence of symptoms, participation in not useful (incorrect) | 2690 (97) | * | * | |
| The presence of blood in stool can be a sign of CRC (correct) | 2539 (92) | |||
| The stool test has to be repeated every 2 years (correct) | 2639 (95) | * | * | |
| If the stool test detects blood, there is a 100% chance of CRC (incorrect) | 2690 (97) | ** | ** | |
| If a person has CRC, there is a 100% chance the stool test will detect this (incorrect) | 2076 (75) | ** | * | |
| The follow‐up investigation (a colonoscopy) can cause a colonic perforation or bleeding (correct) | 1866 (67) | * | ||
| If a perforation or bleeding occurs, surgery is the only treatment option (incorrect) | 1438 (52) | ** | * | * |
| The follow‐up investigation (a colonoscopy) is in almost 100% of cases correct in detecting CRC (correct) | 2189 (79) | |||
| If the stool test detects blood, a follow‐up investigation is necessary to check for the presence of CRC | 2589 (93) | * | ||
| If the colonoscopy detects precursors of CRC, these can almost always be removed in the same procedure (correct) | 2079 (75) | * | ||
| After removal of precursor lesions, regular check ups of the bowel are not necessary (incorrect) | 2685 (97) | ** | * | |
| Participation in the screening programme is obligatory for persons between the ages of 50 and 75 (incorrect) | 2424 (87) | ** | ** | |
CRC, colorectal cancer.
*P < 0.05, **P < 0.01.
Attitude
Attitude towards screening was assessed with four items that that could all be scored on a 7‐point Likert scale. Invitees were asked to indicate the extent to which they would describe participating in the screening pilot for themselves as a bad idea, beneficial, harmful or a good idea. For each person, a summary score was calculated, which ranged from 4 to 28, with a lower score indicating a more negative attitude. The measure of attitude used in this study was adapted from the attitude item used in Dutch prenatal and neonatal screening which was based on Dormandy et al.12, 13, 14 Cronbach's alpha of the attitude scale was 0.83.14
Additional information
Gender and date of birth were extracted from the municipal database. Educational level, employment status, self‐appointed ethnicity and language spoken at home were elicited in the questionnaire. Educational level could be scored as ‘primary education’, ‘lower secondary vocational education’, ‘intermediate vocational education’, ‘higher secondary general education’, ‘higher vocational education’ or ‘university’. Employment status could be scored as ‘employed’, ‘unemployed but taking care of the household’, ‘unemployed because of health‐related issues’, ‘unemployed for other reasons’ or ‘retired’. Ethnicity was elicited with the item ‘to what ethnic group do you feel you belong?’ which could be responded to as ‘Dutch’, ‘Turkish/Moroccan’, ‘Afro‐Caribbean’ or ‘other’. Language spoken at home could be scored as ‘Dutch only’, ‘Dutch and another language’ or ‘other language’.
Data analysis
Informed decision making was operationalized according to the definition of Marteau.8 The concept of informed decision is based on three dichotomous measures: (i) knowledge about FIT screening (classified as adequate or inadequate) (ii) attitude towards FIT screening (classified as positive or negative) and (iii) screening behaviour (either participation or non‐participation). For a decision to be classified as informed, knowledge has to be adequate, and the attitude towards screening has to be in line with actual screening behaviour. In this case, a person is considered to have made an informed decision to participate if knowledge is adequate, her or his attitude is positive, and the FIT is actually returned. Because the proportion of non‐participants who returned the questionnaire was disproportionally low, too low to draw any conclusions (155/4898; 3%), we chose not to include them in the analysis.
Screening participants from whom both a knowledge score and an attitude score were available were included in the final analysis. Persons were considered participants if they returned the FIT before closure of the trial. We described the proportion of persons with adequate knowledge and the proportion of persons with a positive attitude towards screening (attitude score ≥16). The expert panel decided that knowledge can be considered adequate if at least two‐thirds of knowledge items had been answered correctly (total knowledge score ≥12) under the condition that at least half of the items on general knowledge (general knowledge score ≥4) and at least two‐thirds of screening specific items (screening specific knowledge score ≥8) were answered correctly. Based on the combination of these measures of knowledge and attitude the proportion of informed decision makers was calculated.
We evaluated whether there was any difference in knowledge and attitude between men and women, across various age and socio‐economic subgroups (education level, employment status, ethnicity, language spoken at home). Differences in knowledge and attitude between groups were tested for statistical significance using the chi‐square test statistic. In addition, multivariable logistic regression models were used to evaluate associations between socio‐economic and demographic variables and the likelihood of having adequate knowledge or having a positive attitude towards screening. Gender, age, employment status, educational level, ethnicity, language spoken at home and previous response were included as predictors. Age was included as a categorical variable (<54, 55–59, 60–64, 65–69, >69). Employment status was recoded into three categories: employed, unemployed (unemployed but taking care of the household, unemployed because of health‐related issues, unemployed for other reasons), retired. Educational level was recoded into three categories: low (primary school or lower secondary vocational education); intermediate (intermediate vocational education or higher secondary general education); high (higher vocational education or university). Ethnicity and language spoken at home were recoded into two categories: Dutch and other.
If one or more predictors were significantly associated with having adequate knowledge after multivariate analysis, we analysed these differences in more detail on a question level.
We also explored the proportion of uninformed decisions in screening participants using descriptive statistics. Data were analysed using the statistical software SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
Ethical approval
Ethical approval was provided by the Dutch Health Council (2005/03WBO, The Hague, the Netherlands).
Results
Questionnaire completion
A total of 10 265 average risk persons were invited for participation in the second screening round (49% men, mean age 60 ± 7). Of these, 5367 persons (52%) actually participated in the screening trial; 2774 of them (52%) completed the informed choice questionnaire (Fig. 1). Males and older persons were less likely to return the questionnaire (Table 1). Demographic and socio‐economic characteristics of questionnaire responders are displayed in Table 3.
Figure 1.
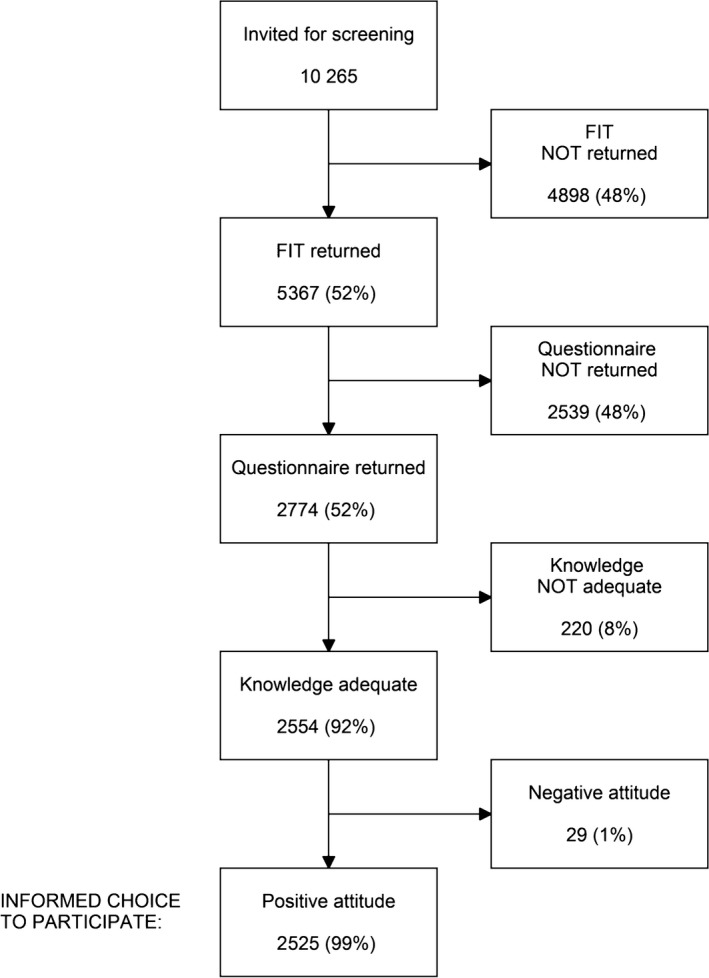
Flowchart leading to informed decisions.
Table 1.
Age and gender of questionnaire responders and non‐responders
| Responders (n = 2774) | Non‐responders (n = 2593) | P‐value | |
|---|---|---|---|
| Men, n (%) | 1286 (46) | 1090 (42) | 0.001 |
| Mean age ± SD, years | 59.8 ± 6.7 | 60.2 ± 6.9 | 0.004 |
Table 3.
Demographic and socio‐economic characteristics of questionnaire responders (n = 2774) for knowledge and attitude
| Knowledge adequate, n (%) | P‐value | Attitude positive, n (%) | P‐value | |
|---|---|---|---|---|
| Total (2774) | 2554 (92) | 2736 (99) | ||
| Gender | ||||
| Males (1286) | 1174 (91) | 0.16 | 1267 (99) | 0.65 |
| Females (1488) | 1380 (93) | 1469 (99) | ||
| Age | ||||
| <55 (742) | 695 (94) | 0.085 | 730 (98) | 0.27 |
| 55–59 (721) | 671 (93) | 716 (99) | ||
| 60–64 (6612) | 554 (91) | 605 (99) | ||
| 65–69 (397) | 365 (92) | 389 (98) | ||
| >69 (297) | 266 (90) | 291 (98) | ||
| Education level | ||||
| Low (552) | 471 (85) | <0.001a | 535 (97) | <0.001a |
| Intermediate (1217) | 1117 (92) | 1208 (99) | ||
| High (910) | 884 (97) | 899 (99) | ||
| Employment status | ||||
| Employed (984) | 920 (94) | 0.16 | 971 (99) | 0.39 |
| Unemployed (412) | 380 (92) | 403 (98) | ||
| Retired (942) | 859 (91) | 930 (99) | ||
| Ethnicity | ||||
| Dutch (2580) | 2390 (95) | <0.001a | 2546 (99) | 0.97 |
| Other (147) | 124 (84) | 145 (99) | ||
| Language spoken at home | ||||
| Dutch (2418) | 2246 (93) | <0.001a | 2386 (99) | 0.73 |
| Other (321) | 280 (87) | 316 (98) | ||
Significant difference in univariate analysis using chi‐square test.
Knowledge
Of all persons who completed the questionnaire, 2554 (92%) could be classified as having adequate knowledge (Fig. 1; Table 4). The proportion of correct responses per knowledge item is shown in Table 2. The item ‘CRC has a better chance of survival when detected in an early stage’ was most often answered correctly followed by ‘in the absence of symptoms participation is not useful’ and ‘if the stool test detects blood, there is a 100% chance of CRC’. Six items were answered incorrectly by at least 25% of participants. These were ‘CRC can be hereditary’; ‘CRC is one of the most prevalent cancers in the Netherlands’; ‘if a person has CRC, there is a 100% chance the stool test will detect this’; ‘the follow‐up investigation can cause a colonic perforation or bleeding’; ‘if a perforation or bleeding occurs surgery is the only treatment option’ and ‘if the colonoscopy detects precursors of CRC these can almost always be removed in the same procedure’.
Table 4.
Informed decision classification of questionnaire responders (n = 2774) based on a combination of knowledge and attitude measures. Number in upper left quadrant (positive attitude and adequate knowledge) qualifies as informed decision [2525 (91%)]
| Attitude | ||
|---|---|---|
| Positive | Negative | |
| Knowledge (%) | ||
| Adequate | 2525 (91) | 29 (1) |
| Inadequate | 211 (8) | 9 (0.3) |
As can be appreciated from Table 3, the proportion of correct answers was significantly higher in persons with a higher education level, in persons of Dutch ethnicity and in persons speaking Dutch at home. When analysed in a multivariable logistic regression model, gender, education level and ethnicity were significantly associated with having adequate knowledge (P = 0.035; P < 0.001 and P = 0.034 respectively). Table 2 shows in more detail the items that were answered significantly less often correctly by men, persons with a lower educational level and persons of non‐Dutch ethnic origin.
Attitude
A total of 2736 participants (99%) showed a positive attitude towards screening (Fig. 1; Table 2). The mean attitude score was 26 (range 4–28, with a lower score indicating a more negative attitude). The lower quartile value was 27, and the upper quartile value was 28. As displayed in Table 2, the proportion of persons with a positive attitude towards screening was significantly lower in invitees with a lower level of education. When gender, age, education level, employment status, ethnicity and language spoken at home were analysed in a multivariable logistic regression model, education level remained significantly associated with having a positive attitude (P = 0.009).
Informed decisions
Based on a combination of the knowledge and attitude scores, 2525 of the total of 2774 questionnaire responders (91%) could be classified as having made an informed decision to participate (Fig. 1; Table 4). Of the 249 non‐informed decisions, 211 (85%) were classified as such based on inadequate knowledge, 29 (12%) based on a non‐corresponding attitude and 9 (3%) based on a combination of the latter two.
Discussion
To our knowledge, this is the first study that describes informed decision making in an average risk population participating in CRC screening using the FIT. The majority of screenees, 91%, could be classified as informed decision makers. Knowledge about the CRC and the screening programme was sufficient in 92% of screenees. However, the knowledge level was not equally distributed over all screenee subgroups: men, invitees with a lower education level and persons of non‐Dutch ethnicity had significantly less knowledge. While almost all participants, 99%, could be classified as having a positive attitude towards screening, participants with a lower education level significantly more often displayed a negative attitude.
One of the strengths of the current study is the fact that the population studied was an average risk population in a real‐life screening situation. Our questionnaire allowed us to look in more detail at differences in knowledge and attitude with respect to several demographic and socio‐economic variables. This study also has several limitations that must be acknowledged. First, we only have data of those participants who returned the questionnaire, which has a response rate of roughly 50%. This could have introduced some form of selection bias. Possibly, responders know more about screening and have a more positive attitude towards screening than non‐responders which could have led to an overestimation of knowledge levels and the proportion of persons with a positive attitude towards screening in our study sample.
Although we do not have baseline data on the ethnicity of all persons invited to the second screening round, it is probable that the response rate was relatively lower among ethnic minorities than among ethnic Dutch invitees. In our first screening round, which included largely the same population, 18% of invitees was of non‐Dutch ethnic origin.15 Our study sample included only 5% of persons of non‐Dutch ethnicity. Possibly, those invitees who had sufficient comprehension of the invitation were more likely to return the questionnaire. This would have resulted in an overestimation of the knowledge level in these ethnic minority groups, and the observed differences would even be larger in the general population. Another limitation is that we were only able to include data from screening participants. Unfortunately, the questionnaire response rate among non‐participants was too small to be included in the analysis.
We are not aware of any other reports on informed decision making in an average risk screening population using FIT, although several others have studied barriers to FIT‐based screening.16, 17, 18
A recent German trial that studied informed choice about CRC screening (including primary colonoscopy screening) found that 60% of persons in the group that was supplied with evidence‐based information regarding screening had adequate knowledge, 93% had a positive attitude, and 44% had made an informed choice.19 These numbers are substantially lower than the numbers we found probably due to differences in methodology and population. In the German study, the questionnaire used to assess knowledge was multiple choice (we used correct/incorrect) and contained multiple items on risk estimation of which we think these are difficult for persons to answer correctly. When we compare the results of our study to other screening initiatives in the Netherlands, however, we find that the observed rate of 91% informed decision makers in this FIT‐based CRC screening trial compares well to a recently published paper on informed choice in a Dutch cervical cancer screening programme, in which the proportion of informed decision makers among screening participants was also 91% (when the lower threshold for adequate knowledge was applied).6
Most of the items that were less likely to be answered correctly were about the screening procedure. Exceptions to this were the items on the hereditary nature of CRC and on CRC prevalence (‘CRC is one of the most prevalent cancers in the Netherlands’). These items were also often answered incorrectly. We observed a relatively low understanding of the possibility of a false negative FIT result. This question was answered incorrectly by one quarter of screening participants. This is particularly worrisome in the case of faecal occult blood test screening, because stool tests have limited sensitivity for significant lesions when used only once.20 Participants should be aware of the fact that one should participate in screening every 2 years because repeated participation can minimize the chance of missing significant lesions. Fortunately, understanding of the importance of programme sensitivity (‘the stool test has to be repeated every 2 years’) was much better: only 5% of invitees answered this question incorrectly.
In contrast to the cervical cancer programme mentioned earlier, the item on possible false‐positive screening results of the FIT was answered correctly by almost all screenees (97%) in our study. In a Dutch trial of computed tomography screening for lung cancer, 94% of screening participants answered the question on the possibility of a false negative test result correctly.7 In that trial, the proportion of informed decisions makers among screening participants was 73%, lower than the rate that we observed.
The concept of informed decision making states explicitly that invitees should be aware of all possible adverse events relating to the screening test and possible follow‐up investigations before making an decision on participation. It was therefore striking to find that the items that were most often answered incorrectly dealt with the possibility of the occurrence of complications should a colonoscopy be necessary and the subsequent management of these complications. Only two‐thirds of screenees were aware of the fact that complications could occur. Almost half of screenees thought that if such a complication occurred, surgery would be the only treatment option.
Although overall knowledge appeared to be acceptable, our study results showed that some groups more often have insufficient knowledge than others. Men, those with a lower education level, and invitees of non‐Dutch ethnicity were more likely to have insufficient knowledge. We showed in our first screening round that it can be difficult to adequately inform persons about the screening programme.5 Apparently, certain invitee subgroups are even less effectively reached than others.
A Dutch lung cancer screening trial also found a significantly lower proportion of correct responses to knowledge items in men and in lower‐educated participants.6 A UK study that examined awareness of screening programmes among white and ethnic minority groups found that awareness of breast and cervical cancer was around 20% lower in an ethnic minority sample. These ethnic disparities persisted after controlling for age, gender and occupational group. Knowledge of breast and cervical screening was also lower among more socio‐economically deprived groups.21
Decision aids could remedy these deficiencies. In a randomized controlled trial, participants allocated to a bowel cancer screening decision aid especially designed for low‐educated persons showed significantly higher levels of knowledge than the control group.22 Several other studies have demonstrated that decision aids can increase knowledge in persons invited for screening.23, 24
In conclusion, a substantial part of participants to a FIT‐based CRC screening programme appear to make an informed decision about participation, Despite the high degree of IDM, there are, however, small but significant disparities in the level of CRC screening‐related knowledge where men, lower‐educated persons and persons of non‐Dutch ethnicity more often lack the necessary information to be able to make an informed decision on participation.
Conflicts of Interest
None declared.
Acknowledgements
The authors thank ZonMW for funding (project numbers 120710007 and 63000004). We also thank the Comprehensive Cancer Centre Amsterdam for their contributions to the study and Karin de Groot for research assistance.
References
- 1. UK National Screening Committee . Criteria for appraising the viability, effectiveness and appropriateness of a screening programme. 2011.
- 2. Irwig L, McCaffery K, Salkeld G, Bossuyt P. Informed choice for screening: implications for evaluation. BMJ, 2006; 332: 1148–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hewitson P, Austoker J. Part 2: patient information, informed decision‐making and the psycho‐social impact of prostate‐specific antigen testing. BJU International, 2005; 95 (Suppl. 3): 16–32. [DOI] [PubMed] [Google Scholar]
- 4. Philips Z, Avis M, Whynes DK. Knowledge of cervical cancer and screening among women in east‐central England. International Journal of Gynecological Cancer, 2005; 15: 639–645. [DOI] [PubMed] [Google Scholar]
- 5. van Rijn AF, van Rossum LG, Deutekom M et al Getting adequate information across to colorectal cancer screening subjects can be difficult. Journal of Medical Screening, 2008; 15: 149–152. [DOI] [PubMed] [Google Scholar]
- 6. Korfage IJ, van Ballegooijen BM, Wauben B, Habbema JD, Essink‐Bot ML. Informed choice on Pap smear still limited by lack of knowledge on the meaning of false‐positive or false‐negative test results. Patient Education and Counseling, 2011; 85: 214–218. [DOI] [PubMed] [Google Scholar]
- 7. van den Bergh KA, Essink‐Bot ML, van Klaveren RJ, de Koning HJ. Informed participation in a randomised controlled trial of computed tomography screening for lung cancer. European Respiratory Journal, 2009; 34: 711–720. [DOI] [PubMed] [Google Scholar]
- 8. Marteau TM, Dormandy E, Michie S. A measure of informed choice. Health Expectations, 2001; 4: 99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van Rossum LG, van Rijn AF, Laheij RJ et al Random comparison of guaiac and immunochemical fecal occult blood tests for colorectal cancer in a screening population. Gastroenterology, 2008; 135: 82–90. [DOI] [PubMed] [Google Scholar]
- 10. Denters MJ, Deutekom M, Fockens P, Bossuyt PM, Dekker E. Implementation of population screening for colorectal cancer by repeated fecal occult blood test in the Netherlands. BMC Gastroenterology, 2009; 9: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wald N. Information leaflets in medical screening. Journal of Medical Screening, 2006; 13: 109. [DOI] [PubMed] [Google Scholar]
- 12. Schoonen HM, Essink‐Bot ML, van Agt HM, Wildschut HI, Steegers EA, de Koning HJ. Informed decision‐making about the fetal anomaly scan: what knowledge is relevant? Ultrasound in Obstetrics and Gynecology, 2011; 37: 649–657. [DOI] [PubMed] [Google Scholar]
- 13. Schoonen HM, van Agt HM, Essink‐Bot ML, Wildschut HI, Steegers EA, de Koning HJ. Informed decision‐making in prenatal screening for Down's syndrome: what knowledge is relevant? Patient Education and Counseling, 2011; 84: 265–270. [DOI] [PubMed] [Google Scholar]
- 14. Dormandy E, Tsui EY, Marteau TM. Development of a measure of informed choice suitable for use in low literacy populations. Patient Education and Counseling, 2007; 66: 278–295. [DOI] [PubMed] [Google Scholar]
- 15. Deutekom M, van Rijn AF, Dekker E et al Uptake of faecal occult blood test colorectal cancer screening by different ethnic groups in the Netherlands. European Journal of Public Health, 2009; 19: 400–402. [DOI] [PubMed] [Google Scholar]
- 16. van Rijn AF, van Rossum LG, Deutekom M et al Low priority main reason not to participate in a colorectal cancer screening program with a faecal occult blood test. Journal of Public Health (Oxford), 2008b; 30: 461–465. [DOI] [PubMed] [Google Scholar]
- 17. Quick BW, Hester CM, Young KL, Greiner KA. Self‐reported barriers to colorectal cancer screening in a racially diverse, low‐income study population. Journal of Community Health, 2012; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hol L, de Jonge V, van Leerdam ME et al Screening for colorectal cancer: comparison of perceived test burden of guaiac‐based faecal occult blood test, faecal immunochemical test and flexible sigmoidoscopy. European Journal of Cancer, 2010; 46: 059–066. [DOI] [PubMed] [Google Scholar]
- 19. Steckelberg A, Hulfenhaus C, Haastert B, Muhlhauser I. Effect of evidence based risk information on “informed choice” in colorectal cancer screening: randomised controlled trial. BMJ, 2011; 342: d3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Graser A, Stieber P, Nagel D et al Comparison of CT colonography, colonoscopy, sigmoidoscopy and faecal occult blood tests for the detection of advanced adenoma in an average risk population. Gut, 2009; 58: 241–248. [DOI] [PubMed] [Google Scholar]
- 21. Robb K, Wardle J, Stubbings S et al Ethnic disparities in knowledge of cancer screening programmes in the UK. Journal of Medical Screening, 2010; 17: 125–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Smith SK, Trevena L, Simpson JM, Barratt A, Nutbeam D, McCaffery KJ. A decision aid to support informed choices about bowel cancer screening among adults with low education: randomised controlled trial. BMJ, 2010; 341: c5370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mathieu E, Barratt A, Davey HM, McGeechan K, Howard K, Houssami N. Informed choice in mammography screening: a randomized trial of a decision aid for 70‐year‐old women. Archives of Internal Medicine, 2007; 167: 2039–2046. [DOI] [PubMed] [Google Scholar]
- 24. Chan EC, McFall SL, Byrd TL et al A community‐based intervention to promote informed decision making for prostate cancer screening among Hispanic American men changed knowledge and role preferences: a cluster RCT. Patient Education and Counseling, 2011; 84: e44–e51. [DOI] [PubMed] [Google Scholar]


