Abstract
Background In the past decade, the number of lawsuits for medical malpractice has risen significantly. This could affect the way doctors make decisions for their patients.
Objective To investigate whether and why doctors practice defensive medicine with their patients.
Design A questionnaire study was conducted in general practice departments of eight metropolitan hospitals in Spain, between January and February 2010.
Setting and participants Eighty general practitioners (48% men; mean age 52 years) with an average of 15.3 years of experience and their 80 adult patients (42% men; mean age 56 years) participated in the study.
Main outcome measurements Participants completed a self‐administered questionnaire involving choices between a risky and a conservative treatment. One group of doctors made decisions for their patients. Another group of doctors predicted what their patients would decide for themselves. Finally, all doctors and patients made decisions for themselves and described the factors they thought influenced their decisions.
Results Doctors selected much more conservative medical treatments for their patients than for themselves. Most notably, they did so even when they accurately predicted that the patients would select riskier treatments. When asked about the reasons for their decisions, most doctors (93%) reported fear of legal consequences.
Discussion and conclusions Doctors’ decisions for their patients are strongly influenced by concerns of possible legal consequences. Patients therefore cannot blindly follow their doctor’s advice. Our study, however, suggests a plausible method that patients could use to get around this problem: They could simply ask their doctor what he or she would do in the patient’s situation.
Keywords: conservative decision making, defensive medicine, medical decision making
Background and objective
In a highly publicized case, Dr. Daniel Merenstein 1 did not routinely prescribe a PSA test to a seemingly low‐risk patient. The PSA test is often used to detect early‐stage prostate cancer, but it has a high false‐positive rate, and the evidence that it can improve health outcomes is inconclusive at best. 2 Following evidence‐based national guidelines, Dr. Merenstein discussed the pros and cons with the patient, who decided against taking the test. Unfortunately, the patient later discovered an advanced‐stage prostate cancer, and the doctor and his residency were sued for not ordering the test. Although Merenstein was acquitted, his residency was found liable for $1 million. 1 Had Dr. Merenstein prescribed the test, he would have avoided the trial. After it, he said he regarded his patients as potential plaintiffs: ‘I order more tests now and I am more nervous around patients: I am no longer the doctor I should be.’
In the present study, we investigated whether doctors follow their patients’ preferences about medical treatments—like Dr. Merenstein did—or make more conservative decisions for their patients than these patients wish. Specifically, we asked doctors to choose between a risky and a conservative treatment for their patients and to predict which treatment their patients would select for themselves. We also asked both doctors and their patients what treatment they themselves would take. We compared doctors’ decisions for their patients and their predictions of their patients’ decisions with doctors’ and patients’ decisions for themselves.
Extant research on how people make decisions for others has shown that people often encourage others to take risks they themselves are not willing to take 3 , 4 , 5 and perceive others to be more risk seeking than oneself. 6 , 7 , 8 Such results have been found in a variety of domains (e.g. lotteries and financial investments, romantic relationships and time management), for decisions with both positive and negative outcomes, and even when monetary incentives were offered for accurate judgments. 6
Based on these studies, we could expect that doctors will perceive their patients to be more risk seeking than they are and will consequently make decisions for their patients that are riskier than the patients would wish. On the other hand, doctors might fear legal consequences of their decisions and therefore be overly conservative when deciding for their patients. We investigated these alternative hypotheses in a study involving general practitioners and their patients.
Methods
Participants
We interviewed 80 doctors working in general practice (average age 48, range 38–64; 48% men; worked on average for 15.3 years). We also interviewed the next patient each doctor attended after participating in the study (i.e. 80 patients in total; average age 56, range 18–84; 42% men; 15% with university degree). To be eligible for recruitment, patients needed to have known their doctor for at least 1 year before the study and had to have visited that doctor at least twice during that year. All participants were recruited from January 2010 to February 2010 by the first author from eight metropolitan hospitals in the cities of Granada, Seville and Jaen (Spain). The Ethics Committee of the University of Granada approved the methodology, and all participants consented to participation through a written consent form at the beginning of the study.
Measurements
Participants received a set of seven scenarios describing a risky and a conservative treatment (see Table 1 for a summary). The risky treatment had a 50–50 chance of leading either to immediate recovery or to a long period of illness. The conservative treatment, in contrast, always led to certain recovery after a short time, which varied across scenarios from 1 to 7 weeks (see Hsee and Weber 6 for a similar procedure). The short time spans were selected on the basis of a pilot study (n = 88). Half of the participants received the information about the risky treatment first, and the rest received the information about the conservative treatment first.
Table 1.
Treatment options in the seven scenarios
| Scenario | Conservative treatment | Risky treatment |
|---|---|---|
| 1 | 7 weeks | 7 months or no symptoms |
| 2 | 6 weeks | 7 months or no symptoms |
| 3 | 5 weeks | 7 months or no symptoms |
| 4 | 4 weeks | 7 months or no symptoms |
| 5 | 3 weeks | 7 months or no symptoms |
| 6 | 2 weeks | 7 months or no symptoms |
| 7 | 1 week | 7 months or no symptoms |
Amount of time that the symptoms remain before being cured, after taking the conservative and risky treatment in the seven scenarios.
Procedure
For each scenario, participants were asked to choose between the risky and the conservative treatment. Doctors were randomly divided into two groups. One group was asked to decide which treatment they would choose for their patient, and the other group was asked to predict which treatment their patient would choose for himself/herself. In addition, all doctors and their patients were asked to decide which treatment they would choose for themselves. In sum, we collected four types of judgments: (i) doctors’ decisions for their patients, (ii) doctors’ predictions of their patient’s decisions, (iii) doctors’ decisions for themselves and (iv) patients’ decisions for themselves.
Finally, all participants provided their demographic details and described the factors they thought influenced their decisions (or the patients’ decisions when doctors made predictions). In particular, participants listed factors in favour of or against the risky and conservative treatments.
Data analyses
Following Hsee and Weber, 6 a risk preference (RP) index was calculated from doctors’ and patients’ decisions in the seven scenarios. For each participant, the RP index was based on the point in the sequence at which the participant moved from choosing the risky treatment to choosing the safe one. For a participant who chose the risky treatment in Scenario 1 through Scenario i‐1 and the safe treatment in Scenario i through Scenario 7, the RP index is defined as i (i = 2, 3, ... 7). Note that we would not observe a shift when the participant either never or always chose the risky treatment. In such cases, the RP index takes the value of 1 or 8, reflecting extreme risk aversion or risk seeking, respectively. Thus, the RP index ranges from 1 to 8, with larger values indicating greater risk preference. For participants lacking consistency in their responses (i.e. 3%), the RP index is defined as a missing value.
In addition, two independent coders analysed the factors influencing risk preferences. They first agreed upon the thematic categories that were apparent and involved benefits and drawbacks of the risky and conservative treatments. Inter‐coder agreement was high (i.e. 95.5% for drawbacks and 93.1% for benefits). The few disagreements were adjudicated by a third coder. Benefits of the risky treatment and drawbacks of the conservative treatment and vice versa coincided in 84% of the cases. For the sake of simplicity, we report only benefits and drawbacks of the risky treatment.
Results
In line with the existing studies in other domains, 6 , 7 , 8 doctors predicted their patients would make riskier decisions for themselves than the doctors (t 39 = 3.87, P=.0003) and the patients actually made for themselves (t 78 = 2.63, P = 0.01; Fig. 1). At the same time, doctors made more conservative decisions for their patients than the doctors (t 39 = −4.18, P = 0.0001) and the patients actually made for themselves (t 78 = −5.07, P = 0.0001). These results are robust as they persisted after controlling for participants’ sex, age, education, length of doctor–patient relationship and presence of a chronic disease in patients.
Figure 1.
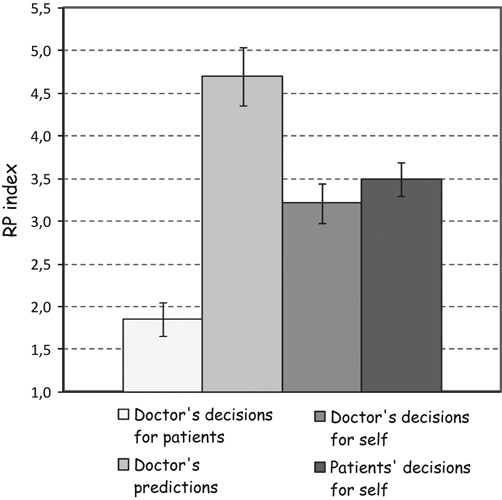
Participants’ mean risk preference (RP) index by type of judgment. The RP index ranges from 1 to 8; larger values indicate a more risk‐seeking preference. Error bars indicate one standard error.
Figure 2 shows the number of factors that participants reported as influencing their decisions/predictions. Overall, doctors considered more drawbacks and fewer benefits of the risky treatment when they made decisions for their patients than when they made decisions for themselves (t 39 =5.22, P = 0.0001, and t 39 = −3.74, P = 0.001 for drawbacks and benefits, respectively) and when they predicted their patients’ decisions (t 78 =5.47, P = 0.0001, and t 78 = −3.45, P = 0.001). They also considered more drawbacks and fewer benefits when deciding for their patients than their patients did when making decisions for themselves (t 78 = 5.43, P = 0.0001, and t 78 = −2.90, P = 0.005 for benefits and drawbacks, respectively). The correlation between the number of drawbacks of the risky treatment suggested by doctors and their risk preferences when they made decisions for their patients was −0.64 (P = 0.0017). In other words, the more drawbacks the doctors considered, the more conservative the decisions they made for their patients. There were no correlations between number of drawbacks and benefits and risk preferences for the other types of judgments.
Figure 2.
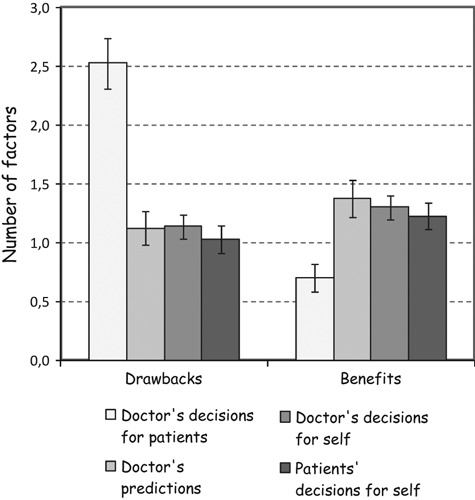
Average number of benefits and drawbacks influencing participants’ risk preferences by type of judgment. Error bars indicate one standard error.
Interestingly, 93% of the doctors cited possible ‘legal consequences’ for themselves (e.g. being sued by the patient or the patient’s family) as the main drawback when they made decisions for their patients. Other drawbacks included possible ‘problems at work,’ cited by 58% of the doctors. These drawbacks were not cited for other types of judgments.
Discussion and conclusion
It is apparent that many doctors in our study feared being sued by patients and regarded their patients as potential plaintiffs. Consistent with this finding, in the past decade, the number of lawsuits for medical malpractice has risen significantly around the world. 9 , 10 , 11 , 12 , 13 Malpractice payments, for instance, are growing at an annual rate of 5% in the United States, 10% in the United Kingdom and as much as 28% in Australia. 9 A study of 824 doctors in Pennsylvania who specialize in areas of medicine that are at a higher risk of litigation, such as emergency medicine, general surgery and gynaecology, found that 88% of the doctors had already been sued at least once. 14 The number of lawsuits against physicians in Spain is also high. At least 18% of the physicians had been sued for medical practice. 15 Litigations burden doctors more than just financially; they also take time and effort to defend against and can seriously damage a doctor’s reputation. 16 , 17
Given the high number of malpractice litigations, it is not surprising that more and more doctors practice some form of defensive medicine. In the study in Pennsylvania mentioned previously, 14 70% of the doctors reported that they were prescribing more diagnostic tests than necessary, and 51% were avoiding treatment of risky patients. It has been estimated that defensive medicine practices in the United States may cost $70–126 billion every year or 5–9% of total health expenditure. 18 Defensive medicine is practised around the world: Evidence for both positive (e.g. increased diagnostic testing and increased follow‐ups) and negative (e.g. avoiding treating certain conditions and patients) defensive practices has also been found in China, 10 Japan, 13 the United Kingdom, 19 the Netherlands, 20 Italy, 21 Germany 22 and Switzerland. 23
Our study adds to this body of literature by showing, for the first time, that doctors select much more conservative treatments for their patients than for themselves. Most notably, doctors did so even when they accurately predicted that the patients would select riskier treatments. Doctors, therefore, do not make decisions for their patients in line with their own intuitions of patients’ preferences but on the basis of the legal consequences that their decisions can bring them. Finally, our study is the first to show that doctors in Spain, like doctors in other countries, are not immune to practising defensive medicine.
Our results have clear implications for medical practice: Patients cannot blindly trust their doctors. Unfortunately, legal and financial aspects of our health system may make doctors afraid to do what is best for their patients. 24 , 25 Our study, however, also suggests a plausible method that patients could use to get around this problem: They should simply ask their doctor what he or she would do in the patient’s situation. Because doctors are not overly conservative when deciding for themselves, patients could learn what doctors really think is best for them. Alerting patients to the fact that their doctors are more cautious in how they handle their patients’ health than their own health would also yield important benefits. In particular, it might help patients take on some responsibility and actively participate in decision making about their own health.
Although the conclusions of our study are robust, our work leaves some questions open for further investigation. In particular, our conclusions are based on doctors’ self‐reports. Larger effects might be expected in medical practice. In addition, our study was conducted in a single country (i.e. Spain). Future investigation could provide additional data on self–other discrepancies in medical decision making by using different (e.g. observational) methods in different countries. Finally, future research could also explore whether self–other discrepancies in medical decision making depend on doctors’ and patients’ individual differences such as numeracy skills 26 , 27 and patients’ language proficiency. 28 Despite these limitations, we were able to demonstrate that legal concerns are the factors that most influence doctors’ decisions for their patients.
Conflict of interest
No conflict of interest.
Source of funding
This experiment is part of the projects ‘How to Improve Understanding of Risks about Health (PSI2008‐02019)’ funded by the Ministerio de Ciencia e Innovación (Spain), and ‘Helping Doctors and Their Patients Make Decisions about Health (PSI2011‐22954)’ funded by the Ministerio de Economía y Competitividad (Spain). The authors declare independence from these funding agencies in each of the following: design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript.
Acknowledgments
We thank Anita Todd for editing the manuscript.
References
- 1. Merenstein D . A piece of my mind: winners and losers . Journal of the American Medical Association , 2004. ; 291 : 15 – 16 . [DOI] [PubMed] [Google Scholar]
- 2. Barry MJ . Screening for prostate cancer — the controversy that refuses to die . Journal of the American Medical Association , 2009. ; 360 : 1351 – 1354 . [DOI] [PubMed] [Google Scholar]
- 3. Beisswanger AH , Stone ER , Hupp JM , Allgaier L . Risk taking in relationships: differences in deciding for oneself versus for a friend . Basic and Applied Social Psychology , 2003. ; 25 : 121 – 135 . [Google Scholar]
- 4. Stone ER , Allgaier L . A social values analysis of self‐other differences in decision making involving risk . Basic and Applied Social Psychology , 2008. ; 30 : 114 – 129 . [Google Scholar]
- 5. Wray LD , Stone ER . The role of self‐esteem and anxiety in decision making for self versus others in relationships . Journal of Behavioral Decision Making , 2005. ; 18 : 125 – 144 . [Google Scholar]
- 6. Hsee CK , Weber EU . A fundamental prediction error: self–other discrepancies in risk preference . Journal of Experimental Psychology: General , 1997. ; 126 : 45 – 53 . [Google Scholar]
- 7. Krishnamurthy P , Kumar P . Self–other discrepancies in waiting time decisions . Organizational Behavior and Human Decision Processes , 2002. ; 87 : 207 – 226 . [Google Scholar]
- 8. Siegrist M , Cvetkovich G , Gutscher H . Risk preference predictions and gender stereotypes . Organizational Behavior and Human Decision Processes , 2002. ; 87 : 91 – 102 . [Google Scholar]
- 9. Anderson GF , Hussey PS , Frogner BK , Waters HR . Health spending in the United States and the rest of the industrialized world . Health Affairs , 2005. ; 24 : 903 – 914 . [DOI] [PubMed] [Google Scholar]
- 10. Chen XY . Defensive medicine or economically motivated corruption? A confucian reflection on physician care in China today The Journal of Medicine and Philosophy , 2007. ; 32 : 635 – 648 . [DOI] [PubMed] [Google Scholar]
- 11. Garcia‐Retamero R , Galesic M . Transparent communication about health risks: Overcoming cultural differences . New York : Springer; , in press . [Google Scholar]
- 12. Gigerenzer G , Gaissmaier W , Kurz‐Milcke E , Schwartz LM , Woloshin S . Helping doctors and patients make sense of health statistics . Psychological Science in the Public Interest , 2007. ; 8 : 53 – 96 . [DOI] [PubMed] [Google Scholar]
- 13. Nakajima K , Keyes C , Kuroyanagi T , Tatara K . Medical malpractice and legal resolution systems in Japan . Journal of the American Medical Association , 2001. ; 285 : 1632 – 1640 . [DOI] [PubMed] [Google Scholar]
- 14. Studdert DM , Mello MM , Sage WM et al. Defensive medicine among high‐risk specialist physicians in a volatile malpractice environment . Journal of the American Medical Association , 2005. ; 293 : 2660 – 2662 . [DOI] [PubMed] [Google Scholar]
- 15. Fuertes Rocañin JC , Cabrera Forneiro J . Medicina y Derecho: una necesaria y fructifera relacion . Madrid : Editado por Grupo Luzan para laboratorios FAES; , 2000. . [Google Scholar]
- 16. Tussing AD , Wojtowycz MA . Malpractice, defensive medicine, and obstetric behavior . Medical Care , 1997. ; 35 : 172 – 191 . [DOI] [PubMed] [Google Scholar]
- 17. Gigerenzer G . Gut Feelings: The Intelligence of the Unconscious . New York, NY : Viking; , 2007. . [Google Scholar]
- 18. U.S. Department of Health and Human Services . Addressing the New Health Care Crisis: Reforming the Medical Litigation System to Improve the Quality of Health Care . U.S. Department of Health and Human Services (HHS) , 2003. . Available at: http://aspe.hhs.gov/daltcp/reports/medliab.htm, accessed April 9th 2010 . [Google Scholar]
- 19. Summerton N . Trends in negative defensive medicine within general practice . British Journal of General Practice , 2000. ; 50 : 565 – 566 . [PMC free article] [PubMed] [Google Scholar]
- 20. Veldhuis M . Defensive behaviour of Dutch family physicians: widening the concept . Family Medicine , 1994. ; 26 : 27 – 29 . [PubMed] [Google Scholar]
- 21. Catino M , Celotti S . The problem of defensive medicine: two Italian surveys . Studies in Health Technology & Informatics , 2009. ; 148 : 206 – 221 . [PubMed] [Google Scholar]
- 22. Brilla R , Evers S , Deutschlander A , Wartenberg KE . Are neurology residents in the United States being taught defensive medicine? Clinical Neurology & Neurosurgery , 2006. ; 108 : 374 – 377 . [DOI] [PubMed] [Google Scholar]
- 23. Steurer J , Held U , Schmidt M , Gigerenzer G , Tag B , Bachmann LM . Legal concerns trigger prostate‐specific antigen testing . Journal of Evaluation in Clinical Practice , 2009. ; 15 : 390 – 392 . [DOI] [PubMed] [Google Scholar]
- 24. Kessler DP , Summerton N , Graham JR . Effects of the medical liability system in Australia, the UK, and the USA . Lancet , 2006. ; 368 : 240 – 246 . [DOI] [PubMed] [Google Scholar]
- 25. Garcia‐Retamero R , Galesic M . Doc, what would you do if you were me? On self–other discrepancies in medical decision making Journal of Experimental Psychology, Applied , 2012. ; 18 : 38 – 51 . [DOI] [PubMed] [Google Scholar]
- 26. Garcia‐Retamero R , Galesic M . Communicating treatment risk reduction to people with low numeracy skills: a cross‐cultural comparison . American Journal of Public Health , 2009. ; 99 : 2196 – 2202 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Garcia‐Retamero R , Galesic M . How to reduce the effect of framing on messages about health . Journal of General Internal Medicine , 2010. ; 25 : 1323 – 1329 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Garcia‐Retamero R , Dhami MK . Pictures speak louder than numbers: on communicating medical risks to immigrants with limited non‐native language proficiency . Health Expectations , 2011. ; 14 : 46 – 57 . [DOI] [PMC free article] [PubMed] [Google Scholar]


