Abstract
Context
Existing measurements of patient preferences cover only a limited range of health information and participation in decision making. A broader approach is necessary to understand the breadth and variations in patient preferences.
Objective
To explore the breadth and variances in patient preferences for health information and participation in decision making and to understand the relationship between age and each type of preference.
Design
The Health Information Wants Questionnaire (HIWQ) was administered during May–December 2010 to gather data about the information and corresponding decision‐making autonomy participants would want in seven areas: diagnosis, treatment, laboratory tests, self‐care, complementary and alternative medicine (CAM), psychosocial factors and health‐care providers.
Setting
A large state university, public libraries and senior centres in Maryland, USA.
Participants
A convenience sample of 438 individuals, including 226 undergraduates (mean age = 20; SD = 2.15) and 212 community‐dwelling older adults (mean age = 72; SD = 9.00).
Main Outcome Measures
Ratings on the information and decision‐making items of the HIWQ.
Results
Participants expressed higher levels of preference for information than for participation in decision making on six of seven subscales. On the psychosocial subscale, they expressed stronger desire for participation in decision making than for information. Age had no predictive effect on the overall preferences or specific preferences for information and participation in decision making about standard treatments and CAM. The predictive effect of age on the other types of preferences varied significantly.
Conclusions
Physicians should take into account the breadth and variations in patient preferences. The predictive effect of age on patient preferences varied depending on the specific area of preferences.
Keywords: age, health information wants, patient preference, shared decision making
Introduction
Until the late 1970s, the dominant health‐care decision‐making model had been the paternalistic model where patients were expected to play a passive role in their own health‐care decision making while physicians made the important decisions on behalf of their patients.1 Since then, there has been a major paradigm shift in the literature to the shared decision‐making model where patients are now expected to stay informed and work with their physicians to collaboratively make decisions.2, 3, 4 Some even argue for a stronger patient‐centred approach, the informed decision‐making model, where physicians are to merely present the information to patients and patients would then (independently or in consultation with family/friends) make the final decisions.5, 6
Despite this increasing interest in patient participation in health‐care decision making, there is little consensus regarding exactly what patient participation entails 7 or how it should be measured.8 Not surprisingly, multiple review articles have come to the same conclusion that patient preferences are ‘highly variable’ across studies.9, 10, 11, 12, 13 Patient preferences or desires for health information and participation in decision making are commonly used as two major indicators of patient participation,9 despite their indirect connection with actual participation. Prior instruments only cover a limited range of patient information and decision‐making preferences that reflect what physicians think their patients would need,14, 15, 16, 17, 18, 19, 20, 21, 22 despite evidence showing poor correlation between what physicians think their patients would need and what patients really want.23, 24, 25 As such, the validity of prior instruments is questionable.26
To begin to address these gaps in the literature, we developed a theory‐driven patient‐oriented instrument, the Health Information Wants Questionnaire (HIWQ), through a multi‐stage, multi‐year process.25, 27, 28 Compared with prior instruments, the HIWQ has two unique features. First, it encompasses a broad range of the types of health information and decision making that patients typically encounter (i.e. diagnosis, treatment, laboratory tests, self‐care, complementary and alternative medicine, psychosocial factors and health‐care providers), promoting a patient‐centred approach to patient participation in their own health care. Second, the HIWQ features parallel items in the information and decision‐making scales, making it possible to investigate nuances in the relationship between potential predictive factors (e.g. age) and each type of information and decision‐making preferences.27 Reported in this paper are key findings from the first large sample study using the HIWQ.
Preferences for health information and participation in decision making
Accompanying the recent paradigm shift in health‐care decision‐making is an increasing interest, largely driven by more practice‐minded researchers, in patients' preferences for health information and participation in decision making, that is, whether patients would actually want to be informed of the health information and, subsequently, use the information to participate in decision making about their own health care.29 A common assumption is that, in general, patients would like to have detailed health information; however, they have less desire to participate in decision making, suggesting a discrepancy between preferences for health information and participation in decision making.22, 30, 31, 32, 33, 34
Existing instruments typically only measure a limited range of preferences,14, 15, 16, 17, 18, 19, 20, 21, 22 reflecting a physician‐centred approach to patient preferences.27 Commonly used instruments for measuring information preferences do not include aspects such as information about CAM and the credentials of health‐care providers.14, 15, 16, 17, 18, 19, 20, 21 In contrast, commonly used instruments for measuring preferences for participation in decision making all measure primarily preference for participation in (standard) treatment decision making.14, 16, 17, 18, 22 These types of measurements of information and decision‐making preferences are summarized in Table 1.
Table 1.
Types of health information and decision making measured in existing instruments
| Type of health information/decision making measured | |||||
|---|---|---|---|---|---|
| Treatment | Disease‐specific | Lab test/medical exam | Physical/self‐care | Psycho‐social aspects | |
| Instrument (information) | |||||
| API‐Information Preference Subscale16 | X | X | X | ||
| KHOS‐Information Subscale17 | X | X | X | ||
| ISQ‐Information Needs Subscale18 | X | X | |||
| Patient Information Needs Questionnaire (PINQ)19 | X | X | X | X | |
| Toronto Informational Needs Questionnaire‐Breast Cancer20 | X | X | X | ||
| Information and Support Needs Questionnaire (ISNQ)15 | X | X | X | X | X |
| Desire for Medical Information Scale (DMIS)14 | X | X | X | X | |
| Information Needs Questionnaire (INQ)21 | X | X | X | ||
| Instrument (decision making) | |||||
| Control Preferences Scale22 | X | ||||
| KHOS‐Behavioural Involvement Subscale17 | X | X | |||
| Participation preference items in ISQ18 | X | ||||
| API‐Decision‐making Preference Subscale16 | X | X | X | ||
| Locus of Authority Scale (LAS)14 | X | X | X | ||
This comparison of existing instruments also reveals that measurements of the types of decisions cover a narrower range than those of information. This sheds new light on the widely reported discrepancy between preferences for information and participation in decision making: It is possible that the widely reported discrepancy between information and decision‐making preferences is at least in part due to measurement differences. There may be important types of decision making that patients would like to participate; yet, these other types of decisions are insufficiently captured by existing instruments, which led to the findings of lower level of desire for participation in decision making than that for information.27
Recently, there has been a trend in the literature promoting a broader view of patient participation that includes but is not limited to (standard) treatment decision making. These additional types of decision making include, for instance, setting the agenda for a medical consultation,35 asking questions and expressing concerns in the consultation 36 and establishing partnership between the patient and the physician.37 A broader view of cancer patients' information needs proposes to include information along the ‘cancer care continuum’ of diagnosis, treatment, post‐treatment/survivorship, relapse/recurrence and end of life.38 It has also been suggested that breast cancer patients' involvement in treatment decision making should include decision making about indigenous medical knowledge and CAM.39
A grounded theory‐driven study identified the concept of Health Information Wants (HIW), or ‘health information that one would like to have and use to make important health decisions that may or may not be directly related to diagnosis or standard treatment’25. This concept incorporates a broad range of health information and decision‐making autonomy that patients might want (which may differ from what their physicians think they would need), thus promoting an understanding of patient preferences from the perspective of the patient, rather than the physician.25 The subsequently developed HIW theoretical framework entails four types of HIW:
Type 1 (Basic HIW): generic, basic information about specific diseases and treatments, used to make decisions about how to cope with psychosocial feelings/concerns;
Type 2 (Advanced HIW): detailed information about specific diseases and standard treatments, used to make decisions about how to interact with health‐care providers to understand and monitor a diagnostic or treatment decision;
Type 3 (Complementary HIW): information about complementary/alternative treatments used to make decisions about a complementary/alternative treatment and
Type 4 (Provider‐related HIW): information about health‐care providers, used to make decisions regarding whether to use a particular health‐care provider.25
The HIW framework25 provides a fresh approach to explaining the widely circulated (but previously largely unexplained) discrepancy between preferences for health information and participation in decision making. This fresh approach rests on the key assumption that, from the patient's perspective, both information and decision making involve a broader range of information and decision making than previously measured in existing instruments. By identifying different types of health information and decision making, the HIW framework also helps reveal the possibility that there might be variability among preferences for different types of information and decision making (e.g. individuals may have a stronger desire for some types of health information and/or decision‐making autonomy than for other types of information and/or decision‐making autonomy).
Based on the HIW framework,25 the HIW Questionnaire (HIWQ) was subsequently developed through a comprehensive multi‐stage, multi‐year process.27, 28 The first step was to determine what types of health information and decision making should be included in the HIWQ. As discussed earlier (Table 1), prior instruments measure five major types of health information. Two of these types are missing from prior decision‐making measurements: decision making about the diagnosis and psychosocial coping. Because the Xie study25 and other studies40, 41, 42, 43, 44, 45, 46 indicate that these two types of decision making are also important, they are included in the HIW Questionnaire (note that the psychosocial type corresponds well with the Type 1 HIW category, and the other four types all fall in the Type 2 HIW category as reported in the Xie25 study). Two other major types are also revealed in recent research: information and decision making about CAM and health‐care providers,42, 47, 48 which are identified in the HIW framework as Type 3 and Type 4 HIW, respectively. Thus, the HIWQ included these seven types of information and decision making: diagnosis; treatment; laboratory tests; self‐care; CAM; psychosocial factors and health‐care providers.27
Next, items were created to represent the construct domain in each of the seven subscales within both the information dimension and the decision‐making dimension. Boundaries of the construct domain were specified with direct connection to the literature and the exploratory study.25 Third, content validity testing was conducted,27 followed by the cognitive testing procedure27 to ensure the point of view of the participant, a technique commonly used in the health science and psychology fields to validate questionnaires.49, 50 The resulting HIWQ was then pilot‐tested, with the results suggesting that it has strong reliability and validity.28
This paper reports key findings from the first large sample study using the HIWQ. Study objectives were to explore the breadth and variances in preferences for health information and participation in decision making and to understand the relationship between age and each type of preference. Our focus on the comparison between the younger and older age groups was motivated by prior literature where younger age is reportedly ‘the most important positive correlate’ of preferences for health information and participation in decision making.16 Studies across populations and health conditions find older adults expressing lower levels of desire for both health information and decision‐making autonomy than younger adults,18, 20, 29, 30, 51, 52 possibly due to age‐related declines in cognition and motivation.51, 53, 54 Still, a review article, after examining relevant studies, concludes that evidence about the relationship between age and preferences is ‘inconclusive’ because of contradictory evidence from studies using different measurements.26 The present study, by distinguishing between and measuring a wider range of preferences using the same instrument, the HIWQ, may shed light on prior inconclusive, contradictory findings to develop a better understanding of the relationship between age and preferences for health information and participation in decision making.
Research questions
-
1
RQ1: How much interest is there in having a broad range of health information and participation in decision making including information and decision making regarding diagnosis, treatment, laboratory tests, self‐care, CAM, psychosocial factors and health‐care providers?
-
2
RQ2: Is there any significant difference between older and younger adults' overall preferences for health information and between their overall preferences for participation in decision making?
-
3
RQ3: How might the significant differences between older and younger adults' preferences for health information and participation in decision making differ with respect to different aspects of the medical encounter (i.e. diagnosis, treatment, laboratory tests, self‐care, CAM, psychosocial factors and health‐care providers)?
Methods
Study participants
A convenience sample of 438 individuals participated in this study during May–December 2010. This included 226 undergraduate students in a variety of disciplines at a large state university and 212 community‐dwelling older adults in Maryland, United States. Participants were recruited using standard recruitment techniques. These included posting recruitment flyers in various buildings of the university (for the younger adult group) and senior‐oriented local organizations such as senior centres, community centres and public libraries (for the older adult group) and recruiting through word of mouth.
The average age for the younger adult group was 20 (SD = 2.15) and for the older adult group was 72 (SD = 9.00). Other demographic characteristics are summarized in Table 2 below.
Table 2.
Participant characteristics
| Variable | Younger (n = 226) | Older (n = 212) | Total (n = 438) |
|---|---|---|---|
| Age, mean (SD), years | 20 (2.15) | 72 (9.00) | 44 (26.50) |
| Gender | |||
| Female, no. (%) | 165 (73.01) | 139 (65.57) | 304 (69.41) |
| Marital status | |||
| Married, no. (%) | 2 (0.88) | 72 (33.96) | 74 (16.90) |
| Single, no. (%) | 217 (96.02) | 30 (14.15) | 247 (56.39) |
| Separated, no. (%) | 2 (0.88) | 4 (1.89) | 6 (1.37) |
| Divorced, no. (%) | 1 (0.44) | 32 (15.09) | 33 (7.53) |
| Widowed, no. (%) | 3 (1.33) | 74 (34.91) | 77(17.58) |
| Living as married, no. (%) | 1 (0.44) | 0 (0) | 1 (0.23) |
| Highest level of education | |||
| Less than high school graduate, no. (%) | 0 (0) | 8 (3.77) | 8 (1.83) |
| High school graduate/GED, no. (%) | 72 (31.86) | 63 (29.72) | 135 (30.82) |
| Vocational training, no. (%) | 1 (0.44) | 13 (6.13) | 14 (3.20) |
| Some college/associate's degree, no. (%) | 135 (59.73) | 58 (27.36) | 193 (44.06) |
| Bachelor's degree, no. (%) | 17 (7.52) | 35 (16.51) | 52 (11.87) |
| Master's degree or other post‐graduate training, no. (%) | 1 (0.44) | 29 (13.68) | 30 (6.85) |
| Doctoral degree, no. (%) | 0 (0) | 6 (2.83) | 6 (1.37) |
| Ethnic group | |||
| Asian, no. (%) | 22 (9.73) | 11 (5.19) | 33 (7.53) |
| African American, no. (%) | 117 (51.77) | 105 (49.53) | 222 (50.68) |
| Latino/Hispanic, no. (%) | 8 (3.54) | 8 (3.77) | 16 (3.65) |
| Native American/American Indian/Alaska Native, no. (%) | 1 (0.44) | 2 (0.94) | 3 (0.68) |
| Native Hawaiian/Pacifica Islander, no. (%) | 0 (0) | 2 (0.94) | 2 (0.46) |
| White, no. (%) | 78 (34.51) | 84 (39.62) | 162 (36.99) |
| Household income | |||
| Less than $20 000, no. (%) | 56 (24.78) | 45 (21.23) | 101 (23.06) |
| $20 000–$29 999, no. (%) | 7 (3.10) | 32 (15.09) | 39 (8.90) |
| $30 000–$39 999, no. (%) | 7 (3.10) | 42 (19.81) | 49 (11.19) |
| $40 000–$49 999, no. (%) | 7 (3.10) | 29 (13.68) | 36 (8.22) |
| $50 000–$59 999, no. (%) | 9 (3.98) | 26 (12.26) | 35 (7.99) |
| $60 000–$69 999, no. (%) | 17 (7.52) | 14 (6.60) | 31 (7.08) |
| $70 000–$99 999, no. (%) | 23 (10.18) | 14 (6.60) | 37 (8.45) |
| $100 000 or more, no. (%) | 100 (44.25) | 10 (4.72) | 110 (25.11) |
| Health condition | |||
| Major, no. (%) | 36 (15.93) | 134 (63.21) | 170 (38.81) |
| Minor, no. (%) | 190 (84.07) | 78 (36.79) | 268 (61.19) |
| Time of condition | |||
| Had in the past, no. (%) | 114 (50.44) | 63 (29.72) | 177 (40.41) |
| Currently have, no. (%) | 112 (49.56) | 149 (70.28) | 261 (59.59) |
Materials
Data reported in this paper were derived from the 21‐item HIWQ, a psychometrically further‐improved version of the original 40‐item HIWQ.27 This self‐administered instrument includes two scales: the Information Preference Scale and the Decision‐making Preference Scale. Each contains seven subscales with parallel items in the following areas: diagnosis (four items); treatment (three items); laboratory tests (three items); self‐care (three items); CAM (three items); psychosocial factors (three items) and health‐care providers (two items).
In the Information Preference Scale, participants were asked to indicate how much information they prefer to have regarding each health‐related area on a five‐point Likert scale (1: None; 2: A little; 3: Some; 4: Most and 5: All). In the Decision‐making Preference Scale, participants were asked to indicate their preferences for participation in each type of health decision making on a five‐point Likert scale. Adapted from Ende et al.,16 response choices were the doctor alone (1), mostly the doctor (2), the doctor and myself equally (3), mostly myself (4) and myself alone (5). A portion of the HIWQ is illustrated in Tables 3 and 4 below.
Table 3.
Excerpt of the Information Preference Scale of the HIW Questionnaire
| Instruction: Place an ‘X’ in the appropriate cell of each row to indicate how much information you would like to have about each of the following areas related to this specific health condition: How much information would you like to have? | |||||
|---|---|---|---|---|---|
| None | A little | Some | Most | All | |
| 1 | 2 | 3 | 4 | 5 | |
| 1. Information about what areas should be covered in the medical appointment to help to diagnose this health condition | |||||
| 2. Information about the stage of this health condition (e.g. how advanced it is, how far it has spread) | |||||
| 3. Information about how severe this health condition is | |||||
These three sample items are from the Diagnosis Subscale of the Information Preference Scale.
Table 4.
Excerpt of the Decision‐making Preference Scale of the HIW Questionnaire
| Instructions: Place an ‘X’ in the appropriate cell of each row to indicate who you think should make the decision in each of the following areas: Who do you think should make the decision? | |||||
|---|---|---|---|---|---|
| The doctor alone | Mostly the doctor | The doctor and myself equally | Mostly myself | Myself alone | |
| 1. Decision regarding what areas to cover in the medical appointment to help to diagnose this health condition | |||||
| 2. Decision regarding what stage of this condition it is (e.g. how advanced it is, how far it has spread) | |||||
| 3. Decision regarding how severe this health condition is | |||||
These three sample items are from the Diagnosis Subscale of the Decision‐making Preference Scale; these decision‐making items correspond with the information items shown in Table 3 above.
Before completing the HIWQ, participants were asked to first think about a specific health condition they had in the past or currently have, and continue thinking about this health condition while filling out the rest of the questionnaire. Preliminary evidence in the literature suggests that there is a relationship between preferences and demographic, personality and other factors.9 Thus, the following variables were also measured and controlled for as covariates in all relevant analyses: gender, general health status, health condition, whether the condition was current or past, how long the condition lasted, perception of severity of the condition, how knowledgeable about the condition, marital status, education level, ethnicity, income level and the Big‐five personality traits.1
Results
Reliability
In the younger adult group, the Cronbach's α coefficients were 0.93 and 0.79 for the overall information and decision‐making dimension, respectively. For the subscales within the information dimension, the range of Cronbach's αs was 0.80–0.95 (mean = 0.87). For the subscales within the decision‐making dimension, the range of Cronbach's αs was 0.71–0.84 (mean = 0.77). In the older adult group, the Cronbach's α coefficients were 0.97 and 0.92 for the overall information and decision‐making dimension, respectively. For the subscale within information dimension, the range of Cronbach's αs was 0.89–0.98 (mean = 0.93). For the subscales within the decision‐making dimension, the range of Cronbach's αs was 0.78–0.92 (mean = 0.87). These results indicate that both overall scales and subscales were reliable and internally consistent for both the younger and older adult groups.
Construct validity
Confirmatory factor analyses were conducted to test the construct validity of the HIWQ. Specifically, these analyses tested whether the items within each dimension (information vs. decision making) reflected the seven distinctive factors measured by the subscales. The hypothesized seven‐factor model was specified by loading items on their respective latent factors and freely estimating the correlations between latent factors. Results showed that in the younger adult group, the seven‐factor model fit the data well for both the information dimension [χ2 (d.f. = 168) = 325.06, Comparative Fit Index (CFI) = 0.96, Standardized Root Mean Square Residual (SRMR) = 0.07 and Root Mean Square Error of Approximation (RMSEA) = 0.06] and the decision‐making dimension [χ2 (d.f. = 168) = 229.49, CFI = 0.92, SRMR = 0.07 and RMSEA = 0.06]. In the older adult group, the seven‐factor model also fit the data well for both the information dimension [χ2 (d.f. = 168) = 307.28, CFI = 0.97, SRMR = 0.03 and RMSEA = 0.06] and the decision‐making dimension [χ2 (d.f. = 168) = 300.30, CFI = 0.96, SRMR = 0.06 and RMSEA = 0.06]. These results supported the hypothesized seven‐factor structure of the HIWQ among both the younger and older age groups.
Findings regarding research question 1
The original subscale scores and overall dimension scores were calculated as means across relevant items. Following Ende et al.,16 these original scores were rescaled to have a mean of 50 and ranges from 0 to 100, where 100 indicates the strongest desire for information or decision‐making autonomy and 0 indicates no desire. The findings suggest that there is interest in a broad range of health information and participation in decision making, including information and decision making regarding diagnosis, treatment, laboratory tests, self‐care, CAM, psychosocial factors and health‐care providers, although the levels of interest vary across these seven subscales. Descriptive findings (means and standard deviations of the preference ratings for each subscale and the overall ratings) are reported in Table 5 below (significance levels from the analysis of variance are reported in the following two subsections).
Table 5.
Subscale and overall ratings as a function of age group and rating dimension
| Subscale | Information | Decision making | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Younger | Older | Younger | Older | |||||||||
| Mean | SD | α | Mean | SD | α | Mean | SD | α | Mean | SD | α | |
| Diagnosis | 76.42 | 24.29 | 0.80 | 66.59 | 31.58 | 0.89 | 16.39 | 13.38 | 0.71 | 32.32 | 21.32 | 0.84 |
| Treatment | 81.06 | 22.40 | 0.83 | 76.50 | 30.06 | 0.91 | 34.93 | 17.92 | 0.73 | 32.74 | 22.09 | 0.90 |
| Laboratory tests | 67.64 | 27.53 | 0.88 | 73.96 | 31.73 | 0.96 | 16.89 | 16.61 | 0.81 | 25.66 | 20.55 | 0.91 |
| Self‐care | 79.02 | 25.75 | 0.80 | 69.58 | 34.20 | 0.89 | 55.30 | 20.61 | 0.74 | 50.88 | 20.86 | 0.78 |
| CAM | 68.15 | 29.41 | 0.95 | 69.84 | 36.42 | 0.98 | 45.56 | 21.55 | 0.80 | 47.91 | 23.34 | 0.92 |
| Psychosocial Factors | 47.56 | 33.29 | 0.88 | 59.28 | 36.61 | 0.93 | 80.67 | 16.22 | 0.78 | 67.08 | 21.42 | 0.89 |
| Health‐care providers | 67.56 | 35.14 | 0.95 | 71.19 | 35.71 | 0.93 | 61.67 | 22.10 | 0.84 | 54.61 | 23.63 | 0.87 |
| Overall | 70.40 | 20.61 | 0.93 | 69.60 | 28.09 | 0.97 | 42.34 | 9.59 | 0.79 | 43.27 | 15.82 | 0.92 |
α: Cronbach's α coefficient.
Findings regarding research question 2
A 2 (age group: younger vs. older adults) × 2 (rating dimension: information vs. decision making) mixed analysis of covariance (ancova) with rating dimension as the within‐subject factor was performed to test the main effect of age group and the interaction effect between age and rating dimension on the overall preference rating. Neither the main effect of age group (F = 0.29, P > 0.10) nor the interaction between age group and rating dimension (F = 2.33, P > 0.10) was significant.
Findings regarding research question 3
A 2 (age group: younger vs. older adults) × 2 (rating dimension: information vs. decision making) × 7 (subscale: diagnosis, treatment, laboratory tests, self‐care, CAM, psychosocial and health‐care providers) mixed ancova with repeated measures on the last two factors was performed. This analysis revealed a significant three‐way interaction among age group, rating dimension and subscale [F (6, 2202) = 9.31, P < 0.01, η2 = 0.03].
To understand this three‐way interaction, seven 2 (age group: younger vs. older) × 2 (rating dimension: information vs. decision making) mixed ancovas were performed to analyse the simple two‐way interaction for each subscale. For diagnosis, the main effects of age group [F(1, 391) = 7.50, P < 0.01, η2 = 0.02] and rating dimension [F(1, 391) = 683.78, P < 0.01, η2 = 0.64] were both significant. The interaction between age group and rating dimension was also significant [F(1, 391) = 43.10, P < 0.01, η2 = 0.10]. These results suggested that for information and decision making about diagnosis, in general, both younger and older adults preferred having more information than decision making. However, the difference in preferences was larger for younger than older adults. Younger adults preferred having more information than older adults, whereas older adults preferred having more decision making than younger adults (Fig. 1).
Figure 1.
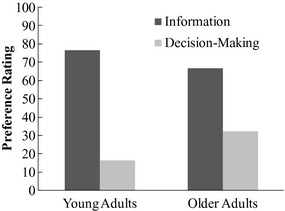
Interaction between age group and rating dimension for diagnosis subscale.
For treatment, only the main effect of rating dimension (F(1, 391) = 658.38, P < 0.01, η2 = 0.63) was significant, suggesting that for information and decision making about treatment, in general, regardless of age, all participants preferred having more information than decision making.
For laboratory tests, the main effects of age group (F(1, 391) = 22.58, P < 0.01, η2 = 0.06) and rating dimension [F (1, 391) = 736.11, P < 0.01, η2 = 0.65] were both significant. These results suggested that for information and decision making about laboratory tests, in general, regardless of age, all participants preferred having more information than decision making. In addition, older adults preferred more information and decision making than younger adults.
For self‐care, the main effects of age group [F(1, 391) = 13.04, P < 0.01, η2 = 0.03] and rating dimension [F(1, 391) = 124.31, P < 0.01, η2 = 0.24] were both significant. These results suggested that for information and decision making about self‐care, in general, regardless of age, all participants preferred having more information than decision making. In addition, younger adults preferred more information and decision making than older adults.
For CAM, only the main effect of rating dimension [F(1, 391) = 101.64, P < 0.01, η2 = 0.21] was significant, suggesting that for information and decision making about CAM, in general, regardless of age, all participants preferred having more information than decision making.
For psychosocial factors, both the main effect of the rating dimension [F(1, 391) = 82.90, P < 0.01, η2 = 0.18] and the interaction between age group and rating dimension were significant [F(1, 391) = 33.53, P < 0.01, η2 = 0.08]. These results suggested that for psychosocial aspects of information and decision making, in general, regardless of age, all participants preferred having more decision making than information. However, the difference in preferences was larger for younger than older adults. Older adults prefer having more information than younger adults, whereas younger adults prefer having more decision making than older adults (Fig. 2).
Figure 2.
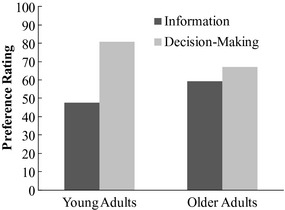
Interaction between age group and rating dimension for psychosocial subscale.
For health‐care providers, both the main effect of rating dimension [F(1, 391) = 35.46, P < 0.01, η2 = 0.08] and the interaction between age group and rating dimension were significant [F(1, 391) = 10.57, P < 0.01, η2 = 0.03]. These results suggested that for health‐care providers–related information and decision making, in general, regardless of age, all participants preferred having more information than decision making. However, the difference in preferences was larger for older than younger adults. Older adults preferred having more information than younger adults, whereas younger adults preferred having more decision making than older adults (Fig. 3).
Figure 3.
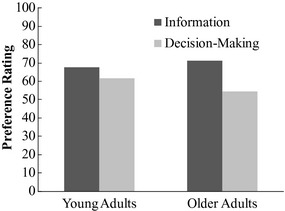
Interaction between age group and rating dimension for health‐care provider subscale.
Discussion
The HIWQ is designed to explore the breadth and variances in preferences for health information and participation in decision making.27 The findings of this study show that participants had high levels of desire for information about several aspects of medical encounters, including information about CAM and health‐care providers that were previously not included in prior instruments, as well as information about the self‐care and psychosocial aspects that are often understudied in prior instruments (see Table 1 above). Consistent with prior studies,22, 30, 31, 32, 33, 34 participants of this study expressed relatively low level of desire for participation in (standard) treatment decision making.
Interestingly, compared with their low desire for participation in standard treatment decision making, participants had high levels of desire for participation in several other types of decision making that were not measured in prior instruments, including decision making regarding self‐care, CAM, psychosocial factors and health‐care providers. Further, on the psychosocial subscale, participants expressed a stronger desire for participation in decision making than for information. These new findings provide strong empirical support for the HIW theoretical framework that promotes a patient‐centred approach to patient preferences. These findings suggest the importance of including all these aspects in understanding patients' preferences for health information and participation in decision making.
Prior research suggests that there is a positive correlation between younger age and preferences for health information and participation in decision making,16, 18, 20, 29, 30, 51, 52 although a review article points out that existing evidence is ‘inconclusive’ owing to contradictory findings from studies using different measurements.26 This study finds no predictive effect of age on the overall preferences for health information and participation in decision making, adding to the ‘inconclusiveness’ of available evidence.
Interesting findings emerged for the seven subscales. For standard treatment and CAM, no significant difference was found between younger and older adults' levels of desire for information or participation in decision making. For laboratory tests, older adults had significantly higher levels of desire for both information and participation in decision making than their younger counterparts. Only for self‐care did younger adults express significantly stronger desire than older adults for both information and participation in decision making.
The interaction between age group (younger vs. older adults) and rating dimension (information vs. decision making) was significant for diagnosis, psychosocial factors and health‐care providers. For diagnosis, younger adults preferred having more information than older adults, whereas older adults preferred having more participation in decision making than younger adults. A possible reason is that younger adults in general have had less life‐experience with health conditions (and thus are less knowledgeable about the conditions) than older adults. As such, younger adults would want to focus more on obtaining the information while older adults would want to participate more in decision making using the knowledge they have developed about the health conditions. In contrast, for both psychosocial factors and health‐care providers, older adults preferred having more information than younger adults, whereas younger adults preferred having more participation in decision making than older adults. A possible reason might be that older adults are more motivated to gather information about their social relationships and evaluate them before taking actions whereas younger adults are more motivated to exert control on the social environment.56
These novel findings help reveal nuances in the relationship between age and each type of preference. Revealing these nuances may help make explicit the previously unspoken, implicit focus on treatment decision making. For instance, while many studies report patients' low interest in participation in ‘decision making’,14, 16, 17, 18, 22, 30, 31, 32, 33, 34 such a claim should be specified as being limited to only (standard) treatment decision making. The findings of this study may also help health‐care providers and educators provide better opportunities for patient participation. For instance, in promoting patient participation in decision making, perhaps health‐care professionals should focus less on promoting patient participation in treatment decision making and focus more on other types of participation opportunities that may be of more interest to patients of different ages.
These findings also have strong implications for both health education interventions and physician–patient interactions. Health education interventions and programmes that are targeted (i.e. reflecting the relevant attitudes and preferences of specific groups) are more effective than generalized programmes.57 In our study, we found group differences with younger adults (undergraduates) preferring more information and participation in decision making about self‐care than older adults, while older adults preferred having more information and participation in decision making about laboratory tests than younger adults. Therefore, health education programmes for younger adults may want to target issues related to information and decision making about self‐care, while programmes for older adults may want to target issues related to information and decision making about laboratory tests.
In terms of physician–patient interaction, our findings suggest that when addressing issues related to, for example, diagnosis, medical professionals should be sensitive to younger adults' greater desire for information and older adults' greater desire for a role in decision making and tailor their communications accordingly, which should help to customize communications at the personal level to address the perceptions and social factors of the individual.57, 58
Importantly, our findings also suggest that there may be new factors that, once revealed, can help better predict preferences. Specifically, by including and measuring a broader range of preferences and by examining each type of preferences both individually and in relation to other types of preferences, we may be able to develop a more refined understanding of each type of preferences and its relationship with other types of preferences. This may reveal patterns previously not recognized when different types of preferences were lump‐summed together. For instance, could factors other than age or gender better predict preferences? Could some factors better predict some types of preferences while other factors better predict other types of preferences? By breaking down preferences into more refined categories, we may be able to better identify predictive factors of preferences, and, subsequently, to provide more specific information and decision‐making opportunities that better match patients' specific preferences.
Limitations and future directions
This study used a convenience sample. Caution should be taken in generalizing the findings to the population. The sample consists of two age groups. Additional research should address the middle ages to determine whether these results could be replicated across the age groups. Also, the younger and older age groups did not have similar disease context (the younger participants were healthier than the older participants, not surprisingly). Future research may benefit from testing the constructs in a population that has similar disease context (e.g. currently having the same health condition and facing similar information and decision‐making choices). A related point is that the HIWQ provides only a snapshot view of preferences. However, experiences of illness can span across months or even years, and preferences for health information and participation in decision making may change over time. In future research, it may be necessary to administer the HIWQ multiple times to assess and compare if and how the preferences of patients may evolve throughout different stages of their conditions.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgements
We thank Ivan Watkins and Man Huang (graduate students, College of Information Studies, University of Maryland) for their assistance in collecting data for the older age group, Makda Kassahun (undergraduate, Department of Behavioral and Community Health, University of Maryland) for her assistance in collecting data for the younger age group and Man Huang for her assistance in entering the data for the older age group of this study.
Footnotes
Coding for health condition followed the Health and Retirement Study55 where high blood pressure, diabetes, cancer, lung disease, heart disease, stroke, psychiatric problems and arthritis were coded as major health conditions and others were coded as minor health conditions.
References
- 1. Brody DS. The patient's role in clinical decision‐making. Annals of Internal Medicine, 1980; 93: 718–722. [DOI] [PubMed] [Google Scholar]
- 2. McNutt RA. Shared medical decision making: problems, process, progress. Journal of the American Medical Association, 2004; 292: 2516–2518. [DOI] [PubMed] [Google Scholar]
- 3. Charles C, Gafni A, Whelan T. Decision‐making in the physician‐patient encounter: revisiting the shared treatment decision‐making model. Social Science & Medicine, 1999; 49: 651–661. [DOI] [PubMed] [Google Scholar]
- 4. Epstein RM, Alper BS, Quill TE. Communicating evidence for participatory decision making. JAMA, 2004; 291: 2359–2366. [DOI] [PubMed] [Google Scholar]
- 5. Braddock CH, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice – time to get back to basics. Jama‐Journal of the American Medical Association, 1999; 282: 2313–2320. [DOI] [PubMed] [Google Scholar]
- 6. Leucht HJ, Kissling W. Shared decision making in psychiatry. Acta Psychiatrica Scandianvica, 2003; 107: 403–409. [DOI] [PubMed] [Google Scholar]
- 7. Entwistle VA, Watt IS. Patient involvement in treatment decision‐making: the case for a broader conceptual framework. Patient Education and Counseling, 2006; 63: 268–278. [DOI] [PubMed] [Google Scholar]
- 8. Elwyn G, Edwards A, Mowle S, et al Measuring the involvement of patients in shared decision‐making: a systematic review of instruments. Patient Education and Counseling, 2001; 43: 5–22. [DOI] [PubMed] [Google Scholar]
- 9. Bagley‐Burnett C. Measuring information‐seeking behaviors and decision‐making preferences In: Frank‐Stromborg M, Olsen SJ. (eds) Instruments for Clinical Health‐Care Research, 3rd edn Sudbury, Massachusetts: Jones and Bartlett Publishers, 2004: 455–471. [Google Scholar]
- 10. Say R, Murtagh M, Thomson R. Patients' preference for involvement in medical decision making: a narrative review. Patient Education and Counseling, 2006; 60: 102–114. [DOI] [PubMed] [Google Scholar]
- 11. Davis RE, Jacklin R, Sevdalis N, Vincent CA. Patient involvement in patient safety: what factors influence patient participation and engagement? Health Expectations, 2007; 10: 259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jung HP, Baerveldt C, Olesen F, Grol R, Wensing M. Patient characteristics as predictors of primary health care preferences: a systematic literature analysis. Health Expectations, 2003; 6: 160–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chewning B, Bylund CL, Shah B, Arora NK, Gueguen JA, Makoul G. Patient preferences for shared decisions: a systematic review. Patient Education & Counseling, 2012; 86: 9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Beisecker AE, Beisecker TD. Patient information‐seeking behaviors when communicating with doctors. Medical Care, 1990; 28: 19–28. [DOI] [PubMed] [Google Scholar]
- 15. Chalmers KI, Luker KA, Leinster S, Ellis I, Booth K. Information and support needs of women with primary relatives with breast cancer: development of the information and support needs questionnaire (ISNQ). Journal of Advanced Nursing, 2001; 35: 497–507. [DOI] [PubMed] [Google Scholar]
- 16. Ende J, Kazis L, Ash A, Moskowitz MA. Measuring patients' desire for autonomy: decision making and information‐seeking preferences among medical patients. Journal of General Internal Medicine, 1989; 4: 23–30. [DOI] [PubMed] [Google Scholar]
- 17. Krantz DS, Baum A, Wideman MV. Assessment of preferences for self‐treatment and information in health care. Journal of Personality and Social Psychology, 1980; 39: 977–990. [DOI] [PubMed] [Google Scholar]
- 18. Cassileth BR, Zupkis RV, Sutton‐Smith K, March V. Information and participation preferences among cancer patients. Annals of Internal Medicine, 1980; 92: 832–836. [DOI] [PubMed] [Google Scholar]
- 19. Galloway SC, Graydon JE. Uncertainty, symptom distress, and information needs after surgery for cancer of the colon. Cancer Nursing, 1996; 19: 112–117. [DOI] [PubMed] [Google Scholar]
- 20. Galloway SC, Graydon JE, Harrison D, et al Informational needs of women with a recent diagnosis of breast cancer: development and initial testing of a tool. Journal of Advanced Nursing, 1997; 25: 1175–1183. [DOI] [PubMed] [Google Scholar]
- 21. Luker KA, Beaver K, Leinster S, Owens RG, Degner LF, Sloan JA. The information needs of women newly diagnosed with breast cancer. Journal of Advanced Nursing, 1995; 22: 134–141. [DOI] [PubMed] [Google Scholar]
- 22. Degner LF, Sloan JA. Decision making during serious illness: what role do patients really want to play? Journal of Clinical Epidemiology, 1992; 45: 941–950. [DOI] [PubMed] [Google Scholar]
- 23. Laine C, Davidoff F, Lewis CE, et al Important elements of outpatient care: a comparison of patients' and physicians' opinions. Annals of Internal Medicine, 1996; 125: 640–645. [DOI] [PubMed] [Google Scholar]
- 24. Heisler M, Vijan S, Anderson RM, Ubel PA, Bernstein SJ, Hofer TP. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? Journal of General Internal Medicine, 2003; 18: 893–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Xie B. Older adults' health information wants in the Internet age: implications for patient‐provider relationships. Journal of Health Communication, 2009; 14: 510–524. [DOI] [PubMed] [Google Scholar]
- 26. Hubbard G, Kidd L, Donaghy E. Preferences for involvement in treatment decision making of patients with cancer: a review of the literature. European Journal of Oncology Nursing, 2008; 12: 299–318. [DOI] [PubMed] [Google Scholar]
- 27. Xie B, Wang M, Feldman R Preferences for health information and decision‐making: development of the Health Information Wants questionnaire. Proceedings of iConference 2011 (pp 237–280). Seattle, WA: 2011. DOI: 10.1145/1940761.1940799. [Google Scholar]
- 28. Xie B, Wang M, Feldman R, Zhou L. Health information and decision‐making preferences in the Internet age: a pilot study using the Health Information Wants Questionnaire. Proceedings of the 2010 ACM International Health Informatics Symposium (pp 610‐619). Arlington, VA, 2010. DOI:10.1145/1882992.1883090. [Google Scholar]
- 29. Benbassat J, Pilpel D, Tidhar M. Patients' preferences for participation in clinical decision making: a review of published surveys. Behavioral Medicine, 1998; 24: 81–88. [DOI] [PubMed] [Google Scholar]
- 30. Levinson W, Kao A, Kuby A, Thisted R. Not all patients want to participate in decision making: a national study of public preferences. Journal of General Internal Medicine, 2005; 20: 531–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kaplan RM, Frosch DL. Decision making in medicine and health care. Annual Review of Clinical Psychology, 2005; 1: 525–556. [DOI] [PubMed] [Google Scholar]
- 32. Gaston CM, Mitchell G. Information giving and decision‐making in patients with advanced cancer: a systematic review. Social Science and Medicine, 2005; 61: 2252–2264. [DOI] [PubMed] [Google Scholar]
- 33. Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play in treatment decision making? Archives of Internal Medicine, 1996; 156: 1414–1420. [PubMed] [Google Scholar]
- 34. Strull WM, Lo B, Charles G. Do patients want to participate in medical decision‐making? JAMA, 1984; 252: 2990–2994. [PubMed] [Google Scholar]
- 35. Murray E, Charles C, Gafni A. Shared decision‐making in primary care: tailoring the Charles et al. model to fit the context of general practice. Patient Education and Counseling, 2006; 62: 205–211. [DOI] [PubMed] [Google Scholar]
- 36. Street RL, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: why some patients are more involved than others. Medical Care, 2005; 43: 960–969. [DOI] [PubMed] [Google Scholar]
- 37. Montori V, Gafni A, Charles C. A shared treatment decision‐making approach between patients with chronic conditions and their clinicians: the case of diabetes. Health Expectations, 2006; 9: 25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rutten LJF, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information amount cancer patients: a systematic review of research (1980–2005). Patient Education & Counseling, 2005; 57: 250–261. [DOI] [PubMed] [Google Scholar]
- 39. Szumacher E. The feminist approach in the decision‐making process for treatment of women with breast cancer. Annals of the Academy of Medicine, Singapore, 2006; 35: 655–661. [PubMed] [Google Scholar]
- 40. Baker L, Wagner TH, Singer S, Bundorf MK. Use of the Internet and e‐mail for health care information: results from a national survey. Journal of the American Medical Association, 2003; 289: 2400–2406. [DOI] [PubMed] [Google Scholar]
- 41. Fox S. Online Health Search. Washington DC: PEW Internet & American Life, 2006. Available at: http://www.pewinternet.org/~/media//Files/Reports/2006/PIP_Online_Health_2006.pdf.pdf, accessed 18 August 2009. [Google Scholar]
- 42. Fox S, Raine L. Vital decisions: how Internet users decide what information to trust when they or their loved ones are sick. Plus a guide from the Medical Library Association about smart healthsearch strategies and good Web sites. Washington DC: Pew Internet & American Life Project. Available at: http://www.pewinternet.org/~/media//Files/Reports/2002/PIP_Vital_Decisions_May2002.pdf.pdf, accessed 20 August 2009; 2002.
- 43. Fox S. Health Information Online. Washington, DC: Pew Internet and American Life Project; Available at: http://www.pewinternet.org/~/media//Files/Reports/2005/PIP_Healthtopics_May2005.pdf.pdf, accessed 7 June 2012; 2005. [Google Scholar]
- 44. Fox S, Raine L. The online health care revolution: how the Web helps Americans take better care of themselves. Washington DC: Pew Internet and American Life Project; Available at: http://www.pewinternet.org/~/media//Files/Reports/2000/PIP_Health_Report.pdf.pdf, accessed 20 August 2009. 2000. [Google Scholar]
- 45. Dickerson S, Reinhart AM, Feeley TH, et al Patient Internet use for health information at three urban primary care clinics. Journal of the American Medical Informatics Association, 2004; 11: 499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rozmovits L, Ziebland S. What do patients with prostate or breast cancer want from an Internet site? A qualitative study of information needs. Patient Education & Counseling, 2004; 53: 57–64. [DOI] [PubMed] [Google Scholar]
- 47. Fox S. E‐patients with a disability or chronic disease. Washington DC: PEW Internet & American Life, Available at: http://www.pewinternet.org/~/media//Files/Reports/2007/EPatients_Chronic_Conditions_2007.pdf.pdf, accessed 20 August 2009, 2007. [Google Scholar]
- 48. Ziebland S, Chapple A, Dumelow C, Evans J, Prinjha S, Rozmovits L. How the internet affects patients' experience of cancer: a qualitative study. BMJ, 2004; 328: 564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Drennan J. Cognitive interviewing: verbal data in the design and pretesting of questionnaires. Journal of Advanced Nursing, 2003; 42: 57–63. [DOI] [PubMed] [Google Scholar]
- 50. Willis GB. Cognitive Interviewing and Questionnaire Design: A Training Manual. Washington DC: National Center for Health Statistics, 1994. [Google Scholar]
- 51. Pinquart M, Duberstein PR. Information needs and decision‐making processes in older cancer patients. Critical Reviews in Oncology/Hematology, 2004; 51: 69–80. [DOI] [PubMed] [Google Scholar]
- 52. Hill SA, Laugharne R. Decision making and information seeking preferences among psychiatric patients. Journal of Mental Health, 2006; 15: 75–84. [Google Scholar]
- 53. Finucane ML, Mertz CK, Slovic P, Scholze Schmidt ES. Task complexity and older adults' decision‐making competence. Psychology and Aging, 2005; 20: 71–84. [DOI] [PubMed] [Google Scholar]
- 54. Lockenhoff CE, Carstensen LL. Aging, emotion, and health‐related decision strategies: motivational manipulations can reduce age differences. Psychology and Aging, 2007; 22: 134–146. [DOI] [PubMed] [Google Scholar]
- 55. Juster F, Suzman R. The health and retirement study: an overview. Journal of Human Resources, 1995; 30 (Suppl.): 7–56. [Google Scholar]
- 56. Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously. American Psychologist, 1999; 54: 165–181. [DOI] [PubMed] [Google Scholar]
- 57. Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders‐Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Education & Behaviour, 2003; 30: 133–146. [DOI] [PubMed] [Google Scholar]
- 58. Kreuter MW, Strecher VJ, Glassman B. One size does not fit all: the case for tailoring print materials. Annals of Behioural Medicine, 1999; 21: 276–283. [DOI] [PubMed] [Google Scholar]


