Abstract
Background
This paper presents results from a public engagement effort in Nebraska, USA, which measured public opinions about governmental involvement in encouraging the use of electronic health records (EHRs).
Objective
We examine the role of trust in government in contributing to public support for government involvement in the development of EHR technologies. We hypothesize that trust in government will lead to support for federal and state governmental encouragement of the use of EHRs among doctors and insurance companies. Further, because individual experiences with health‐care professionals will reduce perceptions of risk, we expect that support for governmental involvement will be tempered by greater personal experience with the health‐care industry.
Design and Results
Examining a small survey of individuals on the issue, we find general support for both of our hypotheses. The findings suggest that trust in government does have a positive relationship with support for government involvement in the policy domain, but that the frequency of personal experiences with health‐care providers reduces the extent to which the public supports governmental involvement in the development of EHR technology.
Discussion and Conclusion
This inquiry contributes to our understanding of public attitudes towards government involvement in EHRs in the United States specifically and contributes to social science examining links between trust in government and support for governmental activity in the emerging policy domain regarding electronic health records systems.
Keywords: electronic health records, electronic medical records, public engagement, public participation, trust in government
Introduction
The rapid growth of health information technology has led to the increasing use and sharing of patient medical information electronically through electronic health records (EHRs). EHRs enable providers not only to collect patient information, but also to share that information with other clinicians involved in the patient's care.1 Proponents of EHRs assert that they increase efficiency and quality of care and decrease medical errors or redundant procedures.2, 3 In recognition of this possibility, both the federal and state governments in the United States in recent years have initiated programmes to support the expansion of EHR systems through various grant‐making strategies, incentives and research.4, 5
While the implementation of electronic records systems in the United States will take place primarily in private settings, the adoption of EHRs has implications for both public and private health administrators. That is, it will likely take considerable government involvement to ensure that technology systems are functional across providers and to help guarantee that information is shared across entities in a secure manner. These realities, in conjunction with public opinion polls that show security is a primary concern of the public in the development of EHRs6 suggest that this responsibility may be a critical one for governments across the United States and throughout the world as EHRs become more prevalent. But does the general public foresee a role for government in this particular policy realm? And, if so, what factors shape how the public views how government should proceed in this policy area? Currently, there is little in the literature that would allow us to address these questions. The purpose of this paper is to provide preliminary evidence related to such questions.
Working with a governmental agency tasked with handling technology issues for the State of Nebraska, USA, we organized a set of public engagement activities related to government involvement in the promotion of EHRs systems. The state agency – the Nebraska Information Technology Commission – had recently created an advisory body, the eHealth Council, responsible for making recommendations to the Governor about EHRs and other eHealth technologies, such as telehealth. At the time of the eHealth Council's formation, considerable EHR‐related activity was underway in the state. Three regional health organizations, funded through federal grants and private funds, were active or planned. The state medical association received a grant to help physicians adopt EHRs. The state had also applied for federal funding to participate in national discussions about EHRs, but had not received an award. The public engagement that is the focus of this paper was an opportunity to explore citizens' views of EHRs to meet its chartered goal ‘to foster the collaborative and innovative use of eHealth technologies through partnerships between public and private sectors, and to encourage communication and coordination among eHealth initiatives in Nebraska’.7
The specific purpose of the public engagement effort described in this paper was to determine whether individuals want the state and/or federal government to encourage the development of EHR systems and was designed to provide a more textured look at how the public views the role of state government in this area. One way we made this determination was through a small survey of the public regarding attitudes towards government involvement in the development of EHR systems. In addition to questions regarding peoples' perceptions of governmental activity in this area, we wanted to examine whether trust in government was predictive of support for government involvement in the encouragement of the use of EHRs. Because evidence has consistently shown that the public perceives potential risk in the implementation of EHRs, we sought out to explore how trust in government might impact attitudes towards government involvement in this critical policy domain.
Drawing on scholarly research showing that trust in government positively impacts attitudes towards governmental policy in situations where risk is involved,8 we hypothesized that trust in government would lead to support for federal and state governments' involvement in encouraging the use of EHRs. However, because individuals have varying degrees of experience with health‐care providers and the health‐care system in general, we also suspected that experiential factors would impact attitudes regarding government involvement. In particular, drawing on research that has examined consumer control in health‐care decision making, we expected that consumers with greater experience with the health‐care industry would be less likely to support government involvement. In general, the results of our analysis support our hypotheses regarding the role of trust and experience in shaping the views of respondents in this policy area.
Therefore, this paper contributes to the literature in two primary ways. First, this paper provides evidence regarding the factors that affect public support for government involvement in the encouragement of EHR systems and related technologies. Second, and more broadly, this paper demonstrates how trust in government and familiarity through personal experience within an industry can shape public attitudes about the appropriate role of government in regulating emerging technologies with which consumers interact.
Trust in government
Scholarship has generally viewed trust in two ways. First, trust concerns the expectations that one individual has of another individual or entity.9 Second, trust in an individual or institution involves acceptance of risk and exposure to vulnerability.10 Thus, in order to trust, one must first have expectations regarding the actions of others and must also be willing to take on risk by exposing one's self to those actions. In the domain of EHR adoption, trust may be a central component to willingness to accept governmental action because consumers consistently view EHRs as carrying some level of security risk,11 yet the seeming inevitability of EHRs means that it will be up to someone or something to put protocols and regulations in place. Viewed from this perspective, trust in government may serve to increase one's willingness to support governmental activity in a risk‐laden endeavour such as the encouragement of EHR adoption. While not necessarily within the trust/risk paradigm of study, the effects of trust in government have been found to be consistently positive in a wide range of studies. For example, Scholz and Lubell12 found that governmental trust positively predicts compliance with tax laws. Tyler and colleagues13 have consistently found that trust in government leads to general acceptance of authoritative directives. Research has also shown that trust in government can positively predict support for zoning policies.14 Alternatively, low levels of trust have been shown to have negative consequences. For instance, Chanley, Rudolph and Rahn15 found evidence that low levels of trust can negatively impact elections and policy making at the national level.
On balance, the literature on trust suggests that there is a positive relationship between trust in government and support for governmental activities. Drawing on this literature and working from the position that support for governmental involvement entails accepting vulnerability to governmental action in this relatively high‐risk policy domain, we posit that trust in government will increase the probability that individuals will support government's encouragement in the development of EHR technologies and systems.
Experience with health care
Studies have shown that health‐care consumers highly value their relationships with physicians and other health‐care providers.16, 17 Patients particularly value the feeling of having control over their health‐care decisions, while in close consultation with their physicians.18, 19, 20 Some studies indicate that patients prefer to have their physicians do the bulk of decision making,21, 22, 23, 24 while others prefer a relationship in which decision making and information are shared.25, 26 The extent to which consumers actually exercise decision‐making autonomy within the patient–physician relationship varies and depends on patient characteristics, type and severity of illness and other factors.27, 28, 29 Regardless, consumers place great amounts of trust in their physicians and perceive the patient–physician relationship as the critical context for reviewing their health‐care options and making informed decisions.30, 31 In contrast, studies have shown a lack of consumer trust in health‐care plans with significant government involvement.32, 33 Americans' mistrust of government health insurance could be due to more general attitudes towards limited government,34, 35 or could be due to more specific objections to the notion of government interference in health care.36, 37, 38 Taken together, this literature raises the issue of whether individuals who interact with health‐care providers fairly often may have different perceptions of EHR technologies than those who do not. Specifically, this literature suggests the possibility that consumers who have obtained a level of comfort with their providers owing to frequent interaction might be more likely to favour EHR adoption without the involvement of government.
Hypotheses
Integrating the lines of scholarship on trust in government and source of control over medical decisions, we are able to develop two primary hypotheses regarding public support for governmental encouragement of EHR usage. In particular, we hypothesize that trust in government, both federal and state, will lead to greater support for federal and state governments' encouragement of the use of EHRs among doctors and insurance companies. Furthermore, because some individuals have more frequent interactions with health‐care providers and because a large proportion of the population works in the health‐care industry (the health‐care industry is one of the largest employment sectors in the US economy, providing 14.3 million jobs for wage and salary workers39), we hypothesize that individuals with greater familiarity with an industry will be less likely to support government involvement in this area, because these individuals are less likely to favour third‐party involvement in health‐care decisions in general.
Data and methods
We worked with the Nebraska Information Technology Commission to develop an online survey administered to a small sample of the general public in Nebraska. We examined surveys conducted previously by two other organizations – a Kaiser Permanente poll11 and Harris Interactive poll40 – and incorporated identical or similar survey items into the Nebraska survey. (At the time of the study, the terms ‘electronic health records’ and ‘electronic medical records’ were being used somewhat interchangeably by some and were new terms to others. While the online survey emphasized ‘electronic medical records’, we use the term ‘electronic health records’ (EHRs) throughout this article for purposes of consistency and in reflection of the accepted terminology that has since emerged.) The remaining survey questions were developed by the research team. As a cost‐saving measure, the participant sample was identified through previously randomly generated lists of Nebraska households with land telephone lines, or random samples or over‐samples of publicly available addresses obtained from previous survey projects. A total of 1759 residents were mailed an invitation to complete the online survey about EHRs. One wave of invitations were sent to residents of the cities of Lincoln (n = 376), Omaha (n = 262) and a six‐county area in central Nebraska (n = 1121). A total of 138 respondents completed the entire online survey about EHRs. The sample was predominantly female (54.4%); older (modal age between 55 and 64 years old); highly educated (over 45% had at least a bachelor's degree) and mostly white (92.6% white). The sample was older and more educated than the general Nebraska population. We will discuss the implications of our sampling strategy later.
Results
Upon answering a general question about whether individuals feel that the benefits of using EHRs outweighs the risks, respondents were asked about their attitudes towards federal and state governments' involvement in encouraging doctors and insurance companies to use EHRs. In total, respondents were asked four questions about their feelings towards government involvement: two questions about whether the US federal government should encourage doctors and insurance companies to use EHRs and two questions about whether the state government should encourage the use of EHRs. These four questions serve as dependent variables in the multivariate analyses. The results of the questions showed that attitudes were fairly evenly split among those who favour government involvement and those who do not (Table 1).
Table 1.
Support for federal and state governments' involvement in the use of EHRs
| Do you feel that the federal government has a role in encouraging doctors to use electronic medical records? | Do you feel that the federal government has a role in encouraging insurance companies to use electronic medical records? | Do you feel that the Nebraska state government has a role in encouraging doctors to use electronic medical records? | Do you feel that the Nebraska state government has a role in encouraging insurance companies to use electronic medical records? | |
|---|---|---|---|---|
| Yes | 45.2% | 41.0% | 51.5% | 48.1% |
| No | 54.8% | 59.0% | 48.5% | 51.9% |
| N | 135 | 134 | 134 | 133 |
To measure trust in government, respondents were then asked two questions derived from questions routinely asked on the General Social Survey: “How often do you think you can trust the federal government to do what is right?” (M = 2.27 on a four‐point scale where 1 = ‘never’ and 4 = ‘just about always’) and “How often do you think you can trust state government to do what is right?” (M = 2.58 using the same scale). Next, we measured peoples' experience with the health‐care industry either as patients or providers. To measure experience as consumers, respondents were asked a subjective question regarding whether they perceived themselves to know more or less about EHRs than the average individual (M = 2.18 on a three‐point scale, with higher numbers indicating higher levels of perceived knowledge). As a more objective measure, we also asked respondents about their frequency of visits to primary care providers in the last year (42.4% had been to their primary care provider either once or not at all, while the remaining 57.6% had been there twice or more); this was transformed into a dichotomous variable where 0 = one or fewer visits and 1 = two or more visits. While this question does not do a perfect job of measuring experience/familiarity with health‐care providers, it does allow us to approximate this measure through a variable that captures the extent to which individuals utilize health‐care services. Furthermore, two or more annual visits to a health‐care provider does not necessarily indicate an extremely high usage of health care41; however, isolating those individuals who only visit a primary care physician allows us to examine the effect of extremely low levels of health‐care utilization. To measure respondents' experience as providers, we asked whether they had been trained in some aspect of health care [this was a dichotomous variable where 0 = ‘no’ (66.6% of respondents) and 1 = ‘yes’ (33.3%)]. Finally, respondents were asked to respond to the three demographic questions described above (education, gender and age); each was included as a control variable in the regression analyses. Ideally, a question measuring the ideology of the respondent would have been included in this analysis. However, because the research was carried out in conjunction with a governmental entity, we refrained from posing ideological or party affiliation questions to the participants to avoid the perception that the poll was conducted for political purposes.
Because of the dichotomous nature of the dependent variable, logistic regression was used to estimate the impact of trust in government and experience with the health‐care industry upon support for government involvement in promoting the use of EHRs. Four models were estimated: one for each of four questions that served as the dependent variables. The results are presented in Table 2.
Table 2.
Logistic regressions predicting support for federal and state governments' involvement in encouraging the use of EHRs
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Federal government should encourage doctors to use EHRs | Federal government should encourage insurance companies to use EHRs | State government should encourage doctors to use EHRs | State government should encourage insurance companies to use EHRs | |||||
| B (SE) | Exp(b) | B (SE) | Exp(b) | B (SE) | Exp(b) | B (SE) | Exp(b) | |
| Trust in federal government | 1.091 (0.336)b | 2.977 | 1.108 (0.336)b | 3.028 | – | – | – | – |
| Trust in state government | – | – | – | – | 0.863 (0.317)a | 2.369 | 0.203 (0.285) | 1.225 |
| Worked in health care | −0.457 (0.464) | 0.633 | −0.412 (0.461) | 0.662 | 0.009 (0.475) | 1.010 | 0.003 (0.449) | 1.003 |
| Knowledge of EHRs | 0.364 (0.252) | 1.439 | 0.229 (0.249) | 1.257 | 0.428 (0.248) | 1.535 | 0.205 (0.234) | 1.227 |
| Times visited primary care provider in the last year | −0.974 (0.427)a | 0.378 | −0.852 (0.422)a | 0.426 | −1.113 (0.429)a | 0.328 | −0.969 (0.405)a | 0.379 |
| Education | 0.091 (0.112) | 1.095 | 0.027 (0.112) | 1.027 | 0.015 (0.112) | 1.015 | 0.059 (0.108) | 1.061 |
| Gender | 0.056 (0.428) | 1.057 | 0.071 (0.425) | 1.074 | −0.259 (0.435) | 0.772 | −0.172 (0.409) | 0.842 |
| Age | 0.081 (0.141) | 1.084 | 0.028 (0.139) | 1.028 | 0.029 (0.141) | 1.029 | 0.053 (0.134) | 1.054 |
| Constant | −4.004 (1.429)a | 0.018 | −3.387 (1.399)a | 0.034 | −2.647 (1.380) | 0.071 | −0.886 (1.292) | 0.412 |
| Psuedo r 2 | 0.163 | 0.136 | 0.152 | 0.072 | ||||
| −2 log likelihood | 152.534 | 152.383 | 153.714 | 163.864 | ||||
| N | 127 | 126 | 126 | 125 | ||||
P < 0.05.
P < 0.01.
P < 0.001.
As Table 2 shows, the impact of trust in government was significantly positive across three of the four models. In model 1, the odds of favouring federal government involvement in encouraging the use of EHRs increased by a factor of 2.98 with a one‐unit increase in an individual's trust in government. Similarly, the odds of favouring federal government involvement in the encouragement of insurance company's use of EHRs increased by a factor of 3.03 when trust in the federal government increases by one unit. The effect of trust in state government upon support for state government involvement in the use of EHRs was also positive, although the effect was not as strong as the odds of favouring state government involvement with doctors, which increased by a factor of 2.37 with each one‐unit increase in trust in state government. However, the effect of trust in state government was not as acute in model 4, as there was no significant relationship between trust in government and support for government involvement in the encouragement of insurance companies using EHRs.
Among the three variables measuring experience with the health‐care industry, only one variable reached statistical significance: the number of times a person has visited their primary care provider in the past year. In particular, when an individual had been to their primary care provider two or more times in the past year, support for federal government encouragement of the use of EHRs among doctors decreased by a factor of 0.38. Likewise, the odds of supporting government encouragement of EHR use among insurance companies decreased by a factor of 0.43 when an individual had visited his or her primary care provider twice or more in the past year. Similarly, the odds that an individual supported state government encouragement of EHR use among doctors and insurance companies decreased by factors of 0.33 and 0.38, respectively, when the individual had been to a primary care provider two or more times in the previous year.
As noted, none of the other experience variables reached statistical significance in predicting support for government encouragement of EHR use. Only one of the remaining experience variables, perceived knowledge of EHRs, approached significance in predicting support for government involvement. In Model 3, this variable approaches conventional levels of significance, but does not cross the 0.05 threshold. Notably, none of the three demographic variables predicted support for government involvement in this area of EHR use. Indeed, none of the three variables came close to significantly predicting support for government involvement.
Discussion
The results of these analyses supported our expectation that trust in government predicts support for government encouragement of EHR usage. In three of the four models, there was a significant, positive relationship between these variables. However, the test of our hypothesis that experience with the medical industry will negatively predict support for government involvement produced mixed results. The variables controlling for work experience in the health‐care industry and perceived knowledge of EHRs had no statistically significant relationship with government support, although we found that the frequency of visits to primary care providers negatively predicted support for government involvement. Thus, the results provided a notable relationship where trust in government led to support for government involvement, but where experience as a consumer within the health‐care industry reduced support for government action. To more clearly illustrate this relationship, we ran a number of simulations. [All simulations were conducted using the CLARIFY module in STATA].45 Controlling for all other variables in the model, the simulations measured the probability of an individual supporting federal government encouragement of the use of EHRs among doctors for respondents who differed in their frequency of visits to their primary care provider. As in the regression models earlier, the consumer frequency variable was dichotomized with individuals who visited primary care providers one time or less in the past year categorized together and individuals who had two or more visits placed in the same category. To run the simulations, all variables in the model were held constant, with the ‘times visited’ and trust in federal government terms allowed to vary.
As Fig. 1 shows, the two groups differed in their support for federal government involvement at different levels of trust in government. In particular, the probability of support for federal government involvement was about 0.15% lower for individuals with low levels of trust in the federal government who had visited their primary care provider twice or more in the past year than those who had only visited one time or fewer. Similarly, the probability of support among frequent visitors to primary care providers was about 0.23% lower at the second level of trust (trust government some of the time), 0.21% lower at the third level of trust (trust government most of the time) and 0.12% lower at the highest level of trust in the federal government (trust government almost all of the time). Table 3 presents the actual differences among the groups. In addition, the right‐hand columns of Table 3 present the predicted probabilities of support for state government involvement at different levels of trust for those who did and did not frequently visit their primary care provider. As the table shows, the relationships observed on questions regarding federal government involvement were largely seen on the questions about state government involvement.
Figure 1.
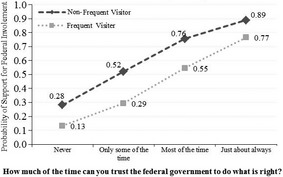
Predicted probability of supporting federal government involvement in the use of EHRs among Doctors as a function of trust in federal government and frequency of visits to primary care physician.
Table 3.
Estimated change in p(y) at different levels of trust when respondent has been to primary care provider twice or more in the past yeara
| How often can you trust the federal government to do what is right? | Predicted change in p(y) when respondent has been to primary care provider twice or more in the past year | How often can you trust the state government to do what is right? | Predicted change in p(y) when respondent has been to primary care provider twice or more in the past year |
|---|---|---|---|
| Never | −0.149 | Never | −0.186 |
| Some of the time | −0.227 | Some of the time | −0.253 |
| Most of the time | −0.209 | Most of the time | −0.252 |
| Almost always | −0.123 | Almost always | −0.182 |
All simulations were conducted using the CLARIFY module in STATA 10 (see King, Tomz, Wittenberg 2000). Gender was set at female; all other variables were set at their mean value when simulations were run.
In sum, these analyses provide a picture of public support for federal and state governments' encouragement of the use of EHRs that is bolstered by trust in each respective level of government, but that is reduced as a result of the frequency with which an individual visits his or her primary care physician. Again, because the use of EHRs is viewed by many as carrying a substantial security risk, the findings related to trust in government are consistent with what we would expect from the literature. That is, in this instance where individuals are asked to make themselves vulnerable with regard to governmental action in the sphere of EHR adoption, it is logical that trust – the willingness to make one's self vulnerable – would be a positive predictor of support for governmental activity. Furthermore, to the extent that a reduction in support for government involvement among individuals with relatively frequent contact with primary care providers indicates a preference for no third‐party involvement, the findings provide evidence in partial support of our second hypothesis regarding personal experience and decreased support for governmental involvement. Through such an interpretation, the findings of this study mirror the results of broader inquiries into third‐party involvement in the health‐care industry – particularly public opinion studies of government regulation of the health‐care industry more generally32, 33 – which show the public to be unwilling to abdicate control over medical decisions to governmental agencies and other entities.42, 43
Limitations
Several methodological limitations of our study should be acknowledged. First, the online survey sample was composed of residents of Nebraska. As a result, we recognize that the results of the study reflect the opinions of individuals in these geographical areas and may not be representative of other parts of the United States. Second, the fact that an online survey tool was used to obtain opinion data may have biased the results, as individuals who are more likely to use the Internet for such activities as surveys might also be more likely to view the use of EHRs more positively because of their comfort with technology. Third, and related to the previous limitation, the initial response rate of the online survey was only 8% (although the low response rate is not unlike those found in other studies44). And although a degree of comfort is provided by the fact that our online survey responses were generally similar with results from other national surveys, the low response rate, and resulting small sample size, remains a concern as it limits our ability to extrapolate the findings to a larger public and keeps us from making stronger claims regarding the relationship between trust in government and support for governmental encouragement of the use of EHRs. Instead, we are left to suggest future research that might allow us to further explore these relationships with more representative samples. In addition to the methodological limitations of our study, we also acknowledge the benefits that might be obtained from measuring the political attitudes of survey respondents; inclusion of such variables might improve the predictive ability of the models included here and are recommended for future study. Finally, we recognize that views on technologies such as EHRs are constantly evolving. Consequently, we recommend that scholars continue to explore the relationship between trust in government and support for governmental activity in this rapidly changing policy domain.
Conclusion
This paper has provided evidence that trust in government predicts public support for government involvement in encouraging doctors and insurance companies to adopt EHR technology. Additionally, this paper has also shown that as individuals become more frequent consumers of services in the health‐care industry, their support/perception of the need for government involvement diminishes. While this study has only focused on the adoption of EHRs with a limited sample in the United States, it can serve to inform future studies of the public's support for government involvement in the areas of health care in which advanced technologies are being adopted, but where the adoption of such technologies carry inherent privacy and security risks. As the evolution of information technologies that can be used to share private and personal information quickens and as demographic shifts continue to change the face of the United States, it is imperative that social scientists strive to understand public attitudes in this policy context so that the relationships between trust in government, consumer behaviours and support for government involvement in the health‐care industry can be better understood.
References
- 1. National Institutes of Health, National Center for Research Resources . Electronic Health Records Overview. Bethesda, MD: National Institutes of Health, 2006. [Google Scholar]
- 2. Gloth F, Coleman E, Phillips S, Zorowitz R. Using electronic health records to improve care: will ‘high tech’ allow a return to ‘high touch’ medicine? Journal of the American Medical Directors Association, 2005; 6: 270–275. [DOI] [PubMed] [Google Scholar]
- 3. Miller RH, West C, Brown TM, Sim I, Ganchoff C. The value of electronic health records in solo or small group practices. Health Affairs, 2005; 24: 1127–1137. [DOI] [PubMed] [Google Scholar]
- 4. DesRoches CM, Jha AK, editors. Health Information Technology in the United States: On the Cusp of Change, 2009. Princeton, NJ: Robert Wood Johnson Foundation, 2009. [Google Scholar]
- 5. National Conference of State Legislatures . Health Information Technology and States: A Project Report from NCSL's Health Information Technology Champions. Denver, CO: National Conference of State Legislatures, 2009. [Google Scholar]
- 6. California Health Care Foundation . National Consumer Health Privacy Survey 2005. Oakland, CA: California Health Care Foundation, 2005. [Google Scholar]
- 7. Nebraska Information Technology Commission . eHealth Council Charter, 2007. Available at http://www.nitc.nebraska.gov/ehc/eHealthcharterapprovedJune2007.pdf, accessed 6 March, 2012.
- 8. Rudolph TJ. Political trust, ideology, and public support for tax cuts. Public Opinion Quarterly, 2009; 73: 144–158. [Google Scholar]
- 9. Barber B. The logic and limits of trust. New Jersey: Rutgers University Press, 1983. [Google Scholar]
- 10. Mayer RC, Davis JH, Schoorman FD. An integrative model of organizational trust. Academy of Management Review, 1995; 20: 709–734. [Google Scholar]
- 11. Kaiser Permanente . Health Care Information Technology Summit Survey Results Revealed, 2007. Available at http://xnet.kp.org/newscenter/EMR/2007/050207healthcareitsummit.html, accessed 29 March 2011.
- 12. Scholz JT, Lubell M. Trust and taxpaying: testing the heuristic approach to collective action. American Journal of Political Science, 1998; 42: 903–920. [Google Scholar]
- 13. Tyler T, Huo YJ. Trust in the Law: Encouraging Public Cooperation with the Police and the Courts. New York: Russell Sage Foundation, 2002. [Google Scholar]
- 14. Cooper CA, Knotts HG, Brennan KM. Trust in government, citizen competence, and public opinion on zoning. Public Administration Review, 2008; 45: 279–295. [Google Scholar]
- 15. Chanley VA, Rudolph TJ, Rahn WM. The origins and consequences of public trust in government: a time series analysis. Public Opinion Quarterly, 2000; 64: 239–256. [DOI] [PubMed] [Google Scholar]
- 16. Jenkinson C, Coulter A, Bruster S, Richards N, Chandola T. Patients' experiences and satisfaction with health care: results of a questionnaire study of specific aspects of care. Quality and Safety in Health Care, 2002; 11: 335–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wald H, Dube C, Anthony D. Untangling the web – the impact of internet use on health care and the physician‐patient relationship. Patient Education and Counseling, 2007; 68: 218–224. [DOI] [PubMed] [Google Scholar]
- 18. Auerbach SM. Do patients want control over their own health care? A review of measures, findings, and research issues. Journal of Health Psychology, 2001; 6: 191–203. [DOI] [PubMed] [Google Scholar]
- 19. Deber RB, Kraetschmer N, Urowitz S, Sharpe N. Do people want to be autonomous patients? Preferred roles in treatment decision‐making in several patient populations. Health Expectations, 2007; 10: 248–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Institute of Medicine . Crossing the Quality Chasm. A New Health System for the 21st Century. Washington, DC: The National Academies Press, 2001. [PubMed] [Google Scholar]
- 21. Beaver K, Luker K, Owens R., Leinster SJ, Degner LS, Sloan JA. Treatment decision‐making in women newly diagnosed with breast cancer. Cancer Nursing, 1996; 19: 8–19. [DOI] [PubMed] [Google Scholar]
- 22. Ende J, Kazis L, Ash A, Moskowitz MA. Measuring patients' desire for autonomy: decision making and information‐seeking preferences among medical patients. Journal of General Internal Medicine, 1989; 4: 23–30. [DOI] [PubMed] [Google Scholar]
- 23. Guadagnoli E, Ward P. Patient participation in decision‐making. Social Science and Medicine, 1998; 47: 329–339. [DOI] [PubMed] [Google Scholar]
- 24. Schain WS. Patients' rights in decision making: the case for personalism versus paternalism in health care. Cancer, 1980; 46: 1035–1041. [PubMed] [Google Scholar]
- 25. Kumar R, Korthuis PT, Saha S et al Decision‐making role preferences among patients with HIV: associations with patient and provider characteristics and communication behaviors. Journal of General Internal Medicine, 2010; 25: 517–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tait AR, Voepel‐Lewis T, Munro HM, Malviya S. Parents' preferences for participation in decisions made regarding anaesthetic care. Pediatric Anesthesia, 2001; 11: 283–290. [DOI] [PubMed] [Google Scholar]
- 27. Benbassat J, Pilpel D, Tidhar M. Patients' preferences for participation in clinical decision making: a review of published surveys. Behavioral Medicine, 1998; 24: 81–88. [DOI] [PubMed] [Google Scholar]
- 28. Gerber BS, Eiser AR. The patient‐physician relationship in the internet age: future prospects and the research agenda. Journal of Medical Internet Research, 2001; 3: 315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Neame R, Hammond A, Deighton C. Need for information and for involvement in decision making among patients with rheumatoid arthritis: a questionnaire survey. Arthritis Care and Research, 2005; 53: 249–255. [DOI] [PubMed] [Google Scholar]
- 30. Epstein RM, Alper BS, Quill TE. Communicating evidence for participatory decision making. Journal of the American Medical Association, 2004; 291: 2359–2366. [DOI] [PubMed] [Google Scholar]
- 31. Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making: a national study of public preferences. Journal of General Internal Medicine, 2005; 20: 531–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Blendon RJ, Benson JM. Americans' views on health policy: a fifty‐year historical perspective. Health Affairs, 2001; 20: 33–46. [DOI] [PubMed] [Google Scholar]
- 33. Blendon RJ, Brodie M, Benson JM, Altman DE, Buhr T. Americans' views of health care costs, access, and quality. The Milbank Quarterly, 2006; 84: 623–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Blake CH, Adolino JR. The enactment of national health insurance: a boolean analysis of twenty advanced industrial countries. Journal of Health Politics, Policy and Law, 2001; 26: 679–708. [DOI] [PubMed] [Google Scholar]
- 35. Steinmo S, Watts J. It's the institutions, stupid! Why comprehensive national health insurance always fails in America. Journal of Health Politics, Policy and Law, 1995; 20: 329–372. [DOI] [PubMed] [Google Scholar]
- 36. Gallup . Americans on Healthcare Reform: Five Key Realities, October 30, 2009. Available at http://www.gallup.com/poll/123989/Americans-Healthcare-Reform-Five-Key-Realities.aspx, accessed 29 March 2011.
- 37. Gallup . Healthcare Bill Supporters Cite Uninsured; Foes, Big Government, September 16, 2009. Available at http://www.gallup.com/poll/122957/Healthcare-Bill-Supporters-Cite-Uninsured-Foes-Big-Govt.aspx, accessed 29 March 2011.
- 38. Gallup . More in U.S. Say Health Coverage is not Government Responsibility, November 13, 2009. Available at http://www.gallup.com/poll/124253/Say-Health-Coverage-Not-Gov-Responsibility.aspx, accessed 29 March 2011.
- 39. U.S. Department of Labor, Bureau of Labor Statistics . Career Guide to Industries, 2010‐2011 edition. Available at http://www.bls.gov/oco/cg/, accessed 29 March 2011.
- 40. Harris Interactive . The benefits of electronic medical records sound good, but privacy could become a difficult issue, 2007. Available at http://www.harrisinteractive.com/NEWS/allnewsbydate.asp?NewsID=1174, accessed 29 March 2011.
- 41. Centers for Disease Control and Prevention . Americans make nearly four medical visits a year on average, 2008. Available at: http://www.cdc.gov/nchs/pressroom/08newsreleases/visitstodoctor.htm, accessed 2 December 2011.
- 42. Davies HT, Rundall TG. Managing patient trust in managed care. Milbank Quarterly, 2000; 78: 609–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mechanic D, Schlesinger M. The impact of managed care on patients' trust in medical care and their physicians. Journal of the American Medical Association, 1996; 275: 1693–1697. [PubMed] [Google Scholar]
- 44. Cohen AB, Restuccia JD, Shwartz M et al A survey of hospital quality improvement activities. Medical Care Research and Review, 2008; 65: 571–595. [DOI] [PubMed] [Google Scholar]
- 45. King G, Tomz M, Wittenberg J. Making the most of statistical analyses: improving interpretation and presentation. American Journal of Political Science, 1998; 44: 341–555. [Google Scholar]


