Abstract
Objectives
The emotional adjustment of couples undergoing assisted reproductive technology (ART) treatments has been widely studied; however, it remains unclear whether infertility history contributes to couples' adjustment. This study examined the impact of infertility history (duration of infertility and number of previous ART treatment cycles) on the emotional adjustment of couples undergoing an ART cycle and the mediating effect of importance of parenthood on that association.
Methods
In this cross‐sectional study, 70 infertile couples (70 women and 70 men) completed self‐report questionnaires assessing emotional adjustment and infertility stress during the hormonal stimulation phase of an ART cycle. Path models accounting for the dyadic nature of the data examined the direct and indirect effects (by affecting representations about parenthood and childlessness) of infertility history on emotional adjustment.
Results
The number of previous cycles affected men's, but not women's, emotional adjustment by affecting the representations on the importance of parenthood and of childlessness. Duration of infertility had the opposite effect, as couples with longer infertility reported heightened importance of parenthood, which negatively affected their emotional adjustment.
Conclusions
Infertility history was associated with emotional adjustment in men and women, although these associations were complex. The results suggest that progression through treatment is harder for those men and women who attribute higher importance to being parents, which is aggravated by longer infertility.
Statement of contribution.
What is already known about the subject?
Infertility is an unexpected and stressful life event
Assisted reproductive treatments (ART) are emotionally demanding
What does this study add?
The influence of infertility history on adjustment is mediated by the importance of parenthood
Men and women are affected by their past history of infertility differently
Keywords: infertility, adjustment, depression, anxiety, assisted reproduction, in vitro, Fertilization
Background
Infertility affects 9% to 10% of the population (Boivin, Bunting, Collins, & Nygren, 2007) and is clinically defined as the failure to achieve a clinical pregnancy after 12 months of regular unprotected sexual intercourse (Zegers‐Hochschild et al., 2009). It has been described as an unexpected and stressful life event (Stanton & Dunkel‐Schetter, 1991) that threatens one of the most important goals in a couples' life: Parenthood (Koert & Daniluk, 2010). To achieve pregnancy, many infertile couples undergo assisted reproductive technology (ART) treatments, which have been steadily increasing across Europe every year (Andersen et al., 2009).
The emotional burden of infertility and ART is well documented (cf. Eugster & Vingerhoets, 1999; Greil, 1997; Verhaak et al., 2007; for reviews), although variability in adjustment has also been recognized (Benyamini, Gozlan, & Kokia, 2005). Research has focused on the investigation of psychosocial factors affecting psychosocial adjustment to infertility and ART. However, less attention has been devoted to specifically investigating the effect of clinical factors on adjustment to infertility and ART, namely the effect of the patients' infertility and treatment history. As a chronic stressor, it can be expected that time‐related variables affect emotional adjustment to the stressor (Dunkel‐Schetter & Lobel, 1991). We argue that this effect occurs by affecting the representations on the importance of parenthood and childlessness during the infertility experience. The goal of this study was to investigate the association between couples' infertility history (i.e., duration of infertility and the number of previous ART treatment attempts) and their emotional adjustment (i.e., depression and anxiety symptoms), at the beginning of an in vitro fertilization (IVF) cycle, while taking into consideration the mediating role of their representations of the importance of parenthood in their lives. A better understanding of how the patients' infertility history relates to their emotional adjustment during treatment can help fertility health care services to identify which patients experience more emotional difficulties at treatment start and will need more support during treatment.
The effect of infertility history on emotional adjustment
Few studies have investigated the impact of infertility history on the emotional adjustment of infertile couples undergoing ART, but results that have been obtained are inconsistent. Some studies have revealed no impact of infertility history in adjustment (Fekkes et al., 2003; Lowyck et al., 2009; Matsubayashi, Hosaka, Izumi, Suzuki, & Makino, 2001; Sina, Ter Meulen, & Carrasco de Paula, 2010); others found significant association between the variables (Benyamini et al., 2005; Lok et al., 2002; Wang et al., 2007), indicating that longer duration of fertility problems and higher number of previous treatments were associated with more emotional difficulties. The inconsistency in study findings may be due, in part, to the assumption that the association between infertility history and emotional adjustment would be linear and constant along time. However, as Aldwin and Stokols (1988) highlighted, contextual factors (such as time, change, and personal resources) may account for different patterns of adjustment to distress, namely nonlinear patterns.
Indeed, some studies have defied this assumption by examining the nonlinear impact of infertility history on emotional adjustment, that is, by examining whether emotional adjustment of infertile couples would be different along the infertility journey, namely across different stages of medical treatment or duration of that experience.
Studies that have examined specifically the effect of previous treatments on emotional adjustment found opposite effects. Markestad, Montgomery, and Bartsch (1998) examined the effect of number of treatments on psychological distress and found a linear and nonlinear tendency of a decrease and subsequent stabilization of this decrease in distress (namely anxiety and depression) after a higher number of treatments. On the contrary, Slade, Emery, and Lieberman (1997), in a prospective study of 144 couples, found a U‐shaped pattern, with higher negative mood in the beginning of the first cycle, lower in the second cycle, and again higher in the third cycle. Boivin, Takefman, Tulandi, and Brender (1995) examined the impact of treatment failure on psychological functioning by comparing three groups of women with various amounts of treatment failure, while controlling for the effect of duration of infertility: Patients with no previous treatments; patients who were undergoing conventional first‐line treatments; and patients starting IVF after unsuccessful first‐order treatments. The results indicated that patients undergoing first‐line treatments reported the highest level of distress (marital, sexual, personal, and infertility related) of the three groups, suggesting an inverted U‐shape curvilinear trend. The authors concluded that the relationship between treatment failure and patients adjustment is independent of time and that it is the amount of treatment failure, and not the time spent in treatment nor the duration of infertility, that better explains their adjustment. According to the authors, these results support Menning's model of infertility (Menning, 1980), where infertility is a developmental process consisting of different phases, and its resolution occurs in the final phase, through the acceptance of infertility. This acceptance would be facilitated after a higher amount of treatment failure (and not necessarily by a longer duration of infertility), because it reinforces the definite childlessness expectation.
Studies that have specifically examined the effect of duration of infertility in psychological adjustment also reported heterogeneous findings. Markestad et al. (1998) found that distress was lower at the beginning and after longer periods of medical attention, mainly for men, which was interpreted as a result of dealing with the crisis of infertility and putting this experience ‘in proper perspective in their lives’ (p. 242), and is in accordance with Boivin et al. (1998) interpretation. However, this result is in contradiction with Berg and Wilson (1991) study, who found that psychological distress (namely anxiety, depression, and interpersonal sensitivity) was higher in the first stage of diagnosis and treatment progression (diagnostic procedures and initial treatments) and the third stage (where individuals poorly responded to previous treatments, therefore facing lower expectations of success) of infertility experience. In the second stage, where couples were undergoing treatments, holding higher success expectations, psychological distress was in normal range. Based on this U‐shaped pattern, Berg and Wilson proposed an acute vs. chronic reaction model, where they claimed that infertility could produce both short‐term and long‐term symptoms of emotional adjustment. The authors concluded that infertility imposes an acute stress reaction related to the early events of diagnosis and infertility treatment, which diminishes over time. This acute reaction is replaced by a chronic strain in the third stage, when past strategies have failed, options are diminishing and a chronic stress response tends to develop.
In summary, it has been suggested that that the relation between history of infertility and emotional adjustment may be nonlinear, although previous studies on the topic revealed contradicting findings. This may be due to some methodological shortcomings, such as (1) the great heterogeneity of concepts used to assess duration of infertility (e.g., time trying to get pregnant, length of medical attention) and previous treatments (by including all type of medical procedures in infertility), and (2) the use of comparative procedures between groups of participants to study nonlinear associations, which does not allow for the analysis for individual changes, and it assumes that patients progress through treatment at the same pace, which is unlikely (Gameiro, Boivin, Peronace, & Verhaak, 2012). Additionally, the previously described studies included all type of medical procedures for infertility and did not address the specific challenges of ART treatments, which are described as especially demanding (Verhaak et al., 2007). Thus, it remains unclear how duration of infertility and previous ART treatment cycles affect emotional adjustment of infertile couples undergoing IVF.
The importance of parenthood, acceptance of childlessness, and emotional adjustment
When studying emotional adjustment to infertility, it is of foremost importance to take into consideration the subjective meaning of parenthood and childlessness in one's life (Greil, 1997; Greil, Shreffler, Schmidt, & McQuillan, 2011). In their review about women's emotional adjustment to ART treatments, Verhaak et al. (2007) suggested that the negative emotional responses that have been observed were strongly related to the treatment outcome, that is, the threat of permanent childlessness. Thus, acceptance of childlessness was identified as an important predictor of the emotional response to treatment (Verhaak et al., 2007). In a study by Fekkes et al. (2003), cognitions regarding parenthood (e.g., ‘A life without children is useless and empty’) were one of the main factors that accounted for more difficulties regarding emotional functioning and lower quality of life during ART treatment. Benyamini, Gozlan, and Kokia (2004) also highlighted the importance of considering cognitions on the specific health threat when examining patients' emotional adjustment. Because a longer infertility history and cumulative failed ART treatments confront infertile couples with the possibility of permanent childlessness (Berg & Wilson, 1991; Boivin et al., 1995), we hypothesize that these factors make the importance of parenthood more salient along the infertility process, which affects couples' emotional adjustment during IVF treatment.
Gender differences in adjustment to infertility and childlessness
Gender differences in the adjustment to infertility have been widely discussed in the literature, namely focusing on differences between men and women regarding psychological symptoms and emotional responses and on differences attributed to parenthood. Findings document that in general women reported higher emotional difficulties than men in almost every stages of infertility (Holter, Anderheim, Bergh, & Moller, 2006; Markestad et al., 1998), although patterns of reactions along the infertility experience are similar (Boivin et al., 1998). When examining gender differences on the importance attributed to parenthood, no differences have been found (Moura‐Ramos, Gameiro, Canavarro, Soares, & Santos, 2012). As a result, it has been argued that gender differences on the adjustment to parenthood may be due not to different experiences of infertility and ART, but due to differences in expressing and reporting emotional difficulties (Edelmann & Connolly, 2000). However, we should also consider that unintended childlessness may have a different meaning for men and women (Berg, Wilson, & Weingartner, 1991) and therefore a different impact on their adjustment to infertility and assisted reproduction. Consequently, it may be that the processes by which their distress is affected are different.
The present study
In this study, we investigated the association between infertility history (i.e., duration of infertility and number of previous ART treatment cycles) and emotional adjustment in couples undergoing ART. More specifically, this study investigated the indirect effect of infertility history on emotional adjustment through influencing representations of the importance of parenthood and childlessness, while accounting for gender differences in those effects. We aim to clarify some inconsistencies observed in the literature regarding the role of infertility history on the emotional adjustment of infertile couples. Understanding how patients' infertility history relates to their emotional adjustment during ART treatment will contribute to a more comprehensive view of the adjustment process to infertility. This understanding may help fertility health care services to identify patients who are at higher risk for emotional distress and stages at which patients may need more support and to delineate targeted interventions to the patients.
Methods
Participants
One hundred and twenty married or cohabiting couples entering an IVF programme at a University Hospital were invited to participate in the study. Inclusion criteria were age (18 years or older) and sufficient proficiency of the Portuguese language to understand and complete the assessment protocol. No one refused to participate, but only protocols from 86 couples (71.7%) were received by the research team. The reasons for not responding were mainly lack of time to participate in the study and cancellation of ART treatment, although these were not assessed systematically. Because the use of bootstrap procedure does not allow for missing data, and due to the dyadic nature of the study, all couples that had missing data were excluded from the sample. The final sample constituted of 140 participants (70 women and 70 men) (58.3% participation rate).
Mean age of participants was 32.51 (±3.92) for women and 34.77 (±4.20) for men. Most couples had medium socio‐economic status (72.9%) and lived in an urban area (54.3%). Couples were trying to get pregnant for about 5 years (4.77 ± 2.65, range: 1–16) and had already been submitted to an average of one (1.30 ± 1.37, range: 0–5) ART cycle (IVF or ICSI). Distribution of infertility factors reported by participants was female, 41.4%; male, 30.0%; mixed, 12.9%; and idiopathic, 15.7%.
Procedures
This study was approved by the Research Ethics Committee of the University Hospital. Participants were systematically recruited to participate in the study by the researcher, at the beginning of their ART cycle. A full explanation of the research objectives, the participants' role, and the researchers' obligations was given when recruiting participants. Participants filled out a consent form if they agreed to collaborate. Participants' representations about the importance of parenthood in one's life and emotional adjustment were assessed during the hormonal simulation phase (5th day) of the IVF treatment.
Measures
Socio‐demographic and clinical form
This form included socio‐demographic data and clinical information on infertility history: Number and type of previous treatment attempts and duration of infertility.
Duration of infertility was defined as time (in years) spent trying to get pregnant, regardless of the time of infertility diagnosis. The number of previous ART treatment attempts refers to the number of previous initiated treatments using assisted reproductive technologies (IVF) with fresh embryos.
Representations about the importance of parenthood in one's life
Representations about the importance of parenthood in one's life were assessed with the Fertility Problem Inventory (FPI; Newton, Sherrard, & Glavac, 1999; Portuguese version by Moura‐Ramos, Gameiro, Canavarro, & Soares, 2012). The FPI is a 46‐item scale, where participants are asked to rate how much they agree or disagree with fertility‐related concerns or beliefs, and responses are given in Likert‐type format, ranging from 0 (Strongly disagree) to 6 (Strongly agree). Representations about the importance of parenthood in one's life were assessed based on the approach proposed by Moura‐Ramos, Gameiro, Canavarro, and Soares (2012), which comprises two main subscales: Need for parenthood (NP) and Rejection of a childfree lifestyle (RCL). The NP subscale assesses close identification with the role of parent and parenthood perceived as essential goal in life (e.g., ‘Pregnancy and childbirth are the two most important events in a couple's relationship'; ‘I will do just about anything to have a child’). RCL captures negative views of a childfree lifestyle or status quo and future satisfaction or happiness dependent on having a child (e.g., ‘Having a child is not necessary for my happiness’; ‘Couples without a child are just as happy as those with children’, all coded inversely). In the present sample, Cronbach's alpha coefficients were .78 and .76 for NP and .77 and .72 for RCL for women and men, respectively. The scores of these two subscales were averaged to compute a global score of representations about the importance of parenthood in one's life (Cronbach's alpha coefficients of .86 and .81 for women and men, respectively). Higher scores indicate higher importance of parenthood.
Emotional adjustment
Emotional adjustment was assessed with the Depression and Anxiety subscales of the Portuguese version (Canavarro, 1999) of the Brief Symptom Inventory (BSI) (Derogatis, 1982). In this 53‐item scale, participants were asked to evaluate the frequency which they experienced specific symptoms during the past week on a 5‐point Likert scale ranging from 0 (Never) to 4 (Very often). In the present sample, Cronbach's alpha coefficients for the Depression and Anxiety subscales were .85 and .82 (Women) and .81 and .72 (Men).
Data analysis
Data were analysed using IBM SPSS, version 20.0 (IBM Corporation, Armonk, NY, USA) and IBM AMOS, version 20.0 (IBM Corporation, Meadville, PA, USA). Correlations were used to describe the association between the study variables. To account for the non‐independence of partners' scores, the database was restructured to consider each partner score as a different variable (Kenny, Kashy, & Cook, 2006). Multivariate analyses of variance for repeated measures were used to test differences between couple partners on the importance of parenthood and emotional adjustment. Bivariate correlations were calculated to examine the pattern of direct relationships between the study variables.
Analyses were conducted with path analysis examining direct and indirect effects using AMOS with the maximum‐likelihood estimation method. Models were tested separately for each predictor and each outcome, as the inclusion of all predictors and outcomes would increase the complexity of the model, requiring a larger sample size. According to Kline (2005), the sample size required to perform a path analysis should take into consideration the complexity of the model, namely the ratio between the number of participants and parameters to be estimated. This ratio should be above 5. In this study, the ratio between sample size and free parameter estimates was 6.7. Linear and curvilinear terms were included in the analysis following the recommendations of Aiken and West (1991). To build the linear and the quadratic terms of the regression equation, predictors (number of previous ART treatments attempts and duration of infertility) were mean‐centred (linear term) and then squared (quadratic term). The predicted values of the outcomes for the curvilinear effects presented in the figures were calculated by computing the regression equation for every value of the predictors (Aiken & West, 1991).
To test for the significance of the indirect effects, bootstrap procedures using 5000 samples were used (Cheung, 2009; Hayes, 2009; MacKinnon & Fairchild, 2009; MacKinnon, Lockwood, & Williams, 2004; Shrout & Bolger, 2002). To evaluate overall model fit, the chi‐square goodness‐of‐fit statistic, the comparative fit index (CFI), the standardized root‐mean‐square residual (SRMR), and the root‐mean‐square error of approximation (RMSEA) fit indices were used. A model is considered to have very good fit if the chi‐square statistic is non‐significant, the CFI is >0.95, the SRMR is below .08, and the RMSEA is below .05 (Hu & Bentler, 1998).
Results
Preliminary analyses
Preliminary analysis (cf. Table 1) revealed that duration of infertility had a small (r = .10) and non‐significant correlation with the number of previous ART cycles. Additionally, duration of infertility and the number of previous failed ART treatment cycles were not related with emotional adjustment at any of the times assessed for either men or women. A strong and significant association (r = .70, p < .001) was found between the importance that each couple partners attributed to parenthood in their lives, indicating high consistency in partners' importance of parenthood. Women reported more symptoms of depression and anxiety than men, Wilks' λ = .636, F(2, 68) = 19.45, p < .001. No significant differences were found between partners in representations about the importance of parenthood, Wilks' λ = .999, F(1, 69) = 0.49, p = .825.
Table 1.
Descriptives and bivariate correlations among study main variables
| Mean ± SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| 1. Duration of infertility | 4.77 ± 2.65 | – | ||||||
| 2. Number ART cycles | 1.30 ± 1.37 | .10 | – | |||||
| 3. Importance of parenthood – Women | 37.08 ± 7.14 | .21 | −.17 | – | ||||
| 4. Importance of parenthood – Men | 37.22 ± 6.72 | .16 | .37* | .70*** | – | |||
| 5. Anxiety symptoms – Women | 1.07 ± .75 | −.01 | .00 | .40** | .35** | – | ||
| 6. Anxiety symptoms – Men | .60 ± .49 | .18 | .00 | .14 | .30** | .48*** | – | |
| 7. Depressive symptoms – Women | .97 ± .75 | .08 | .08 | .41** | .31** | .84*** | .49*** | – |
| 8. Depressive symptoms – Men | .52 ± .56 | .17 | .02 | .33** | .40*** | .47*** | .74*** | .53*** |
Previous ART cycles refer to initiated IVF and ICSI treatments with fresh embryos.
*p ≤ .05; **p ≤ .01; ***p ≤ .001.
Path models examining direct and indirect effects of number of previous ART cycles in couples' emotional adjustment
Figure 1 describes the direct and indirect effects of the number of previous ART cycles on women's and men's anxiety and depression symptoms.
Figure 1.
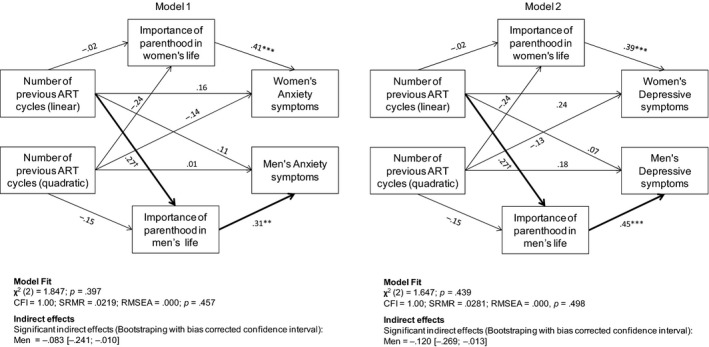
Direct and indirect effects of the number of previous ART cycles on women's and men's anxiety and depression symptoms. Path model of direct and indirect effects of number of previous ART cycles on men's and women's anxiety and depressive symptoms with linear and quadratic terms, controlling for all other paths in the model. Thick lines represent significant indirect effects. Notes. Partners' errors of mediated and dependent errors were correlated, but were not included in the figure for clarity. ART = assisted reproduction technology CFI = comparative fit index; SRMR = standardized root‐mean‐square residual; RMSEA = root‐mean‐square error of approximation. † p ≤ .1; * p ≤ .05; ** p ≤ .01; ***p ≤ .001.
The number of previous ART treatment cycles was linearly and indirectly associated with the male partner's depression and anxiety symptoms (Anxiety = −0.083; BC 95% CI [−0.241; −0.010]; Depression = −0.120; BC 95% CI [−0.269; −0.013]) by affecting men's representations about the importance of parenthood in their lives. That is, the more treatment attempts the couple had undergone, the lower was the importance men attributed to parenthood on their lives decreasing their anxiety and depressive symptoms. No significant indirect effects were found regarding women's emotional adjustment.
Path models examining direct and indirect effects of duration of infertility in couples' emotional adjustment
As displayed in Figure 2, indirect effects regarding the association between duration of infertility and anxiety and depression were found to be significant for both women (Anxiety = 0.106, with BC 95% CI [0.019; 0.219; Depression = 0.099, with BC 95% CI [0.014; 0.197]) and men (Anxiety = 0.057, BC 95% CI [0.002; 0.166]; Depression = 0.081 BC 95% CI [0.004; 0.211]).
Figure 2.
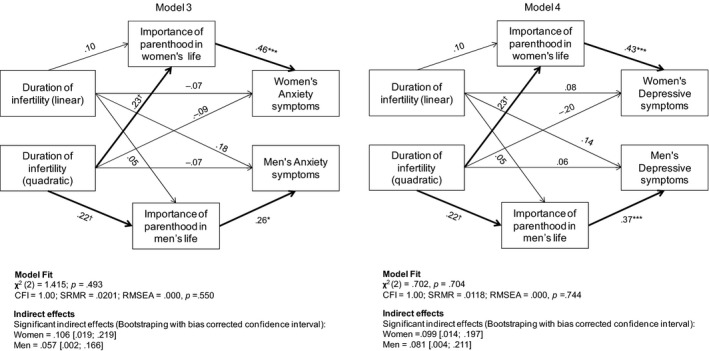
Direct and indirect effects of duration of infertility on women's and men's anxiety and depression symptoms. Path model of direct and indirect effects of duration of infertility on men's and women's anxiety and depressive symptoms with linear and quadratic terms, controlling for all other paths in the model. Thick lines represent significant indirect effects. Notes. Partners' errors of mediation and dependent errors were correlated, but these correlations were not included in the figure for clarity. CFI = comparative fit index; SRMR = standardized root‐mean‐square residual; RMSEA = root‐mean‐square error of approximation. † p ≤ .1; *p ≤ .05; **p ≤ .01; ***p ≤ .001.
In both cases, the quadratic term was the best predictor of the model. An opposite effect of duration of infertility on women's depression and anxiety symptoms was found: Both depression and anxiety progress steadily in couples with few years of infertility; as couples experienced infertility throughout years, anxiety remained high and tends to increase, while there was a sharp decrease in women's depressive symptoms, namely after 6 years trying to get pregnant, as can be detected by the inflection point of the line of depression scores, which represents the point from which the linear tendency starts changing its trajectory (cf. Figure 3). Regarding men's adjustment, the longer infertility was associated with accentuated importance of parenthood in their lives, and consequently, they reported more anxiety and depressive symptoms.
Figure 3.
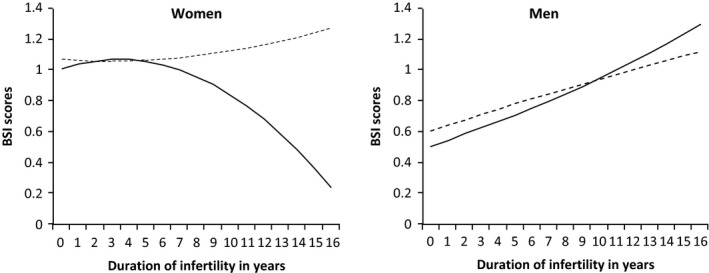
Quadratic (curvilinear) effects of duration of infertility on women's and men's anxiety and depressive symptoms. The figure shows the regression curves that best fit the regression model, based on the regression equation for every value of the predictor. The outcomes scores were calculated by including the linear and curvilinear (quadratic) term on the duration of infertility (Aiken & West, 1991). Note. Dotted lines refer to anxiety symptoms scores. Straight lines refer to depressive symptoms scores.
Discussion
The present study examined the role of infertility history in the emotional adjustment of infertile patients undergoing ART. The main results of the study were twofold: (1) duration of infertility and number of previous treatments had a different impact on adjustment, although in both situations throughout an indirect pathway, by affecting women and men's representations about the importance of parenthood; and (2) women and their partners were affected differently by their infertility history.
Indirect effects of history of infertility on men and women's emotional adjustment
The results of the present study underline that adjustment to infertility is a highly personal experience, influenced by previous experience and by each person's own representations of the importance of parenthood in their own lives. Indeed, duration of infertility and number of past ART treatments only affected adjustment indirectly, by affecting men and women's representations of parenthood.
The number of previous ART treatments influenced men's adjustment but not their partner's. Men in couples who had undergone a greater number of treatment cycles attributed a lower importance to parenthood and had fewer symptoms of depression and anxiety. A higher number of previous treatments, as suggested by Boivin et al. (1995), may have confronted patients with the increasingly more probable prospect of childlessness, promoting its acceptance and reducing their distress, which is underlined by the indirect effect found in the study. At the time the sample was recruited, ART in public settings in Portugal was limited to three cycles, unless otherwise clinically recommended. Men undergoing more treatment cycles could have adjusted their expectations to more easily accept future childlessness. These men may have perceived themselves as having diminished options to achieve parenthood, due to financial (having to move to private clinics) or medical reasons (lower chances of conceiving after three cycles, Pinborg, Hougaard, Andersen, Molbo, and Schmidt, 2009), resulting in less emotional difficulties. According to Lazarus and Folkman (1984), the persistence of a chronic stressor (such as repeated failures in pursuing treatment to achieve pregnancy) can give the opportunity to address its demands, by developing new goals and replacing or reappraising old ones. However, this response pattern was not found for women. The number of previous ART cycles did not affect women's emotional adjustment directly or indirectly, and it was not associated with representations regarding the importance of parenthood in one's life. This result was surprising, as it would be expected that past treatment failure would be associated with emotional adjustment (Boivin et al., 1995).
According to this argument, it could also be considered that longer infertility would be associated with lower distress; however, this did not occur. The pattern of association between duration of infertility and couples' emotional distress was clearly distinct, as this association was positive and curvilinear, apart from the effect on women's depression. Men with longer infertility reported higher importance for parenthood, which was associated with their anxiety and depressive symptoms. Duration of infertility was not associated with the number of previous ART treatment cycles; therefore, we can presume that some couples had periods of time during which their infertility was untreated and unresolved. This may have increased their emotional difficulties by sustaining expectations regarding treatment and by not allowing for the confrontation of treatment failure. Conversely, depression tended to be lower in women with longer infertility, namely those trying to get pregnant for more than 6 years. Considering that couples in our study were entering treatment, which is a moment of high uncertainty and hope, it can be expected that anxiety is heightened but feelings of loss, which are related depression, may be decreasing after a long‐time experiencing infertility. Nevertheless, this result was surprising and future studies should clarify this issue.
In summary, these results suggest that the resolution and acceptance of the infertility condition occurs not after a long duration of infertility but as a consequence of the experience of repeated ART treatment failure. It seems that it is the process of dealing with treatment failure, confronting couples with childlessness, leads couples to reappraise their life goals and expectations for the future. Couples, who have difficulty envisioning themselves in the future without children and believe that parenthood is the major goal of their life, tend to experience psychological distress when entering treatment. Previous research has shown that this distress is accentuated if they experience failure (Verhaak, Smeenk, Evers et al., 2005; Verhaak, Smeenk, van Minnen, Kremer, & Kraaimaat, 2005). Early detection of these difficulties can be important for professionals to help couples dealing with this distress.
Gender differences on the effects of history of infertility on emotional adjustment
This study showed that the number of previous ART cycles and the duration of infertility affected women's and men's adjustment differently. Having undergone a higher number of treatment cycles may have confronted men with the increasingly more probable prospect of childlessness, promoting its acceptance and reducing their distress, but it did not occur with women, who probably envision every new ART cycle as a moment of hope for achieving pregnancy. This is coherent with past research that underlines that men are more prone to consider treatment termination (Greil, Leitko, & Porter, 1988; Sydsjo, Ekholm, Wadsby, Kjellberg, & Sydsjo, 2005), which may translate in easiness to accept future childlessness when compared to women (Peddie, van Teijlingen, & Bhattacharya, 2005; Volgsten, Skoog Svanberg, & Olsson, 2010). These results should be interpreted considering the specificities of the Portuguese social and cultural context, which shapes gender roles and expectations regarding parenthood. Indeed, as other southern European countries, Portugal has rooted traditional views on family and gender roles (Nishioka, 2003) and is conservative regarding parenthood and children. Indeed, although children are equally important for men and women (Aboim, 2007), they play a core role in women's identity making more difficult for them to accept future childlessness.
Examining the effect of duration of infertility in men's and women's adjustment also underlines how the processes of adjusting can be different among couple partners. While it is clear that being unsuccessfully trying to get pregnant is associated with an increase in psychological symptoms, with a tendency to accentuate in the later years, women's depressive symptoms are an exception. To interpret these results, we should bear in mind that data were collected in the beginning of treatment, which is a moment of heightened hope and expectations (Benyamini, 2003). In this situation, women who have been infertile for a long time but are now in treatment may exacerbate positive emotions (hope, optimism) and diminishing depressive symptoms. In men, the process was the opposite, which may be the result of a lower involvement with the treatment procedures, preventing the experiencing of positive emotions that occur in the beginning of the treatment after several years infertile, associated with a lower use of positive reframing in that situation in order to better adapt to it (Jordan & Revenson, 1999). These results underline how different may be the experience of undergoing assisted reproduction treatments and that couple members may cope differently with past experiences. Nevertheless, more studies are needed to further explore the different mechanisms affecting men and women's adjustment to infertility.
Strengths and limitations
A major contribution of the present study was the test of nonlinear and indirect associations contributing to the effect of infertility history on emotional adjustment in couples entering ART. Albeit several studies have previously examined the influence of clinical variables on couples' adjustment, these results contributed to highlight the process by which that influence operates. The inclusion of both couple members within a dyadic design that explores the experiences of both men and women while controlling for the non‐independence of couples' scores (Kenny et al., 2006) was an important contribution, as it allows studying the specificities of adjustment in men and women while controlling for the interdependence of their experience.
The identification of infertility history as a significant predictor of emotional adjustment is an important contribution because it allows health care providers to direct their attention to more specific characteristics of infertile couples presenting for ART and to target their interventions in order to meet the specific needs of each couple. Additionally, it highlights the importance of referral of infertile patients to fertility clinics in due time.
In addition to the aforementioned contributions, several limitations of the present study are worth noting. The sample size is small, which reduces the power to detect a significant effect; therefore, small effects could have been detected if the sample was larger. The cross‐sectional design does not allow the establishment of causality. Future studies should focus on investigating the impact of infertility history in couples' long‐term adjustment and in different stages of ART treatment. Lastly, when interpreting these results, it is important to take into consideration the regulation constraints of ART in Portugal, as the law regulating assisted reproduction was developed in 2006 and fully applied since 2009. Therefore, when participants from this study started to try to get pregnant, the referral routine was not well established, and the timely referral for the fertility care would largely depend on the geographical zone of residence of the patients and on each medical centre approach.
Implications for research and clinical practice
The results of our study have several implications for research and for clinical practice with infertile couples. First, studies directed at further investigating the impact of infertility history on adjustment should consider the nonlinearity of the associations between these variables. It is noteworthy that some of the linear or direct associations that were tested were non‐significant, which would have led us to conclude that history of infertility did not have any impact on the couples' adjustment. It is then important to explore more complex patterns of associations. Second, our results highlight individual variability in the experience of infertility and ART treatments, which was related to the past experience on infertility and to the different meanings attributed to parenthood and childlessness. Indeed, although recognized as a stressful life event for all couples, undergoing ART treatments may impose distinct demands on couples depending on their previous infertility history. Therefore, patients at different treatment phases may require different types and levels of support. Additionally, results underline the role of sociocultural differences that may shape the importance attributed to parenthood. Therefore, these results can be translated in recommendations for health care, namely (1) to develop health policies to ensure that couples who meet the criteria for infertility diagnosis are directed to infertility centres in a timely manner; (2) that psychosocial interventions directed at couples who present emotional difficulties when entering an ART programme consider their previous infertility history and discuss all treatment scenario possibilities and consequences; (3) to discuss the meaning of parenthood and childlessness with couples, to adjust their expectations regarding treatment; and (4) to assure that fertility care takes into account cultural, social, and religious differences that are known to affect the importance attributed of parenthood and therefore the adjustment to infertility.
Conflict of interest
All authors declare no conflict of interest.
Acknowledgement
This study was developed within the Relationships, Development & Health Research Group of the R&D Unit Cognitive‐Behavioral Center for Research and Intervention (PEst‐OE/PSI/UI0730/2014). Mariana Moura‐Ramos is supported by a postdoctoral grant by the Portuguese Foundation for Science and Technology (SFRH/BPD/87514/2012).
References
- Aboim, S. (2007). Clivagens e continuidades de género face à família em Portugal e noutros países Europeus [Gender cleavages and continuities toward the family in Portugal and other European countries] In Wall K. & Amâncio L. (Eds.), Famıília e género em Portugal e na Europa [Family and gender in Portugal and Europe] (pp. 35–91). Lisbon, Portugal: Imprensa das Ciências Sociais. [Google Scholar]
- Aiken, L. S. , & West, S. G. (1991). Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage. [Google Scholar]
- Aldwin, C. M. , & Stokols, D. (1988). The effects of environmental change on individuals and groups: Some neglected issues in stress research. Journal of Environmental Psychology, 8, 57–75. doi:10.1016/S0272‐4944(88)80023‐9 [Google Scholar]
- Andersen, A. N. , Goossens, V. , Bhattacharya, S. , Ferraretti, A. P. , Kupka, M. S. , de Mouzon, J. , … ESHRE . (2009). Assisted reproductive technology and intrauterine inseminations in Europe, 2005: Results generated from European registers by ESHRE. Human Reproduction, 24, 1267–1287. doi:10.1093/humrep/dep035 [DOI] [PubMed] [Google Scholar]
- Benyamini, Y. (2003). Hope and fantasy among women coping with infertility and its treatments In Jacoby R. & Keinan G. (Eds.), Between stress and hope: From a disease‐centered to a health‐centered perspective (pp. 141–166). Westport, CT: Praeger. [Google Scholar]
- Benyamini, Y. , Gozlan, M. , & Kokia, E. (2004). On the self‐regulation of a health threat: Cognitions, coping, and emotions among women undergoing treatment for infertility. Cognitive Therapy and Research, 28, 577–592. doi:10.1023/B:COTR.0000045566.97966.22 [Google Scholar]
- Benyamini, Y. , Gozlan, M. , & Kokia, E. (2005). Variability in the difficulties experienced by women undergoing infertility treatments. Fertility and Sterility, 83, 275–283. doi:10.1016/j.fertnstert.2004.10.014 [DOI] [PubMed] [Google Scholar]
- Berg, B. J. , & Wilson, J. F. (1991). Psychological functioning across stages of treatment for infertility. Journal of Behavioral Medicine, 14, 11–26. doi:10.1007/BF00844765 [DOI] [PubMed] [Google Scholar]
- Berg, B. J. , Wilson, J. F. , & Weingartner, P. J. (1991). Psychological sequelae of infertility treatment: The role of gender and sex‐role identification. Social Science & Medicine, 33, 1071–1080. doi:10.1016/0277‐9536(91)90012‐2 [DOI] [PubMed] [Google Scholar]
- Boivin, J. , Andersson, L. , Skoog‐Svanberg, A. , Hjelmstedt, A. , Collins, A. , & Bergh, T. (1998). Psychological reactions during in‐vitro fertilization: Similar response pattern in husbands and wives. Human Reproduction, 13, 3262–3267. doi:10.1093/humrep/13.11.3262 [DOI] [PubMed] [Google Scholar]
- Boivin, J. , Bunting, L. , Collins, J. A. , & Nygren, K. G. (2007). International estimates of infertility prevalence and treatment‐seeking: Potential need and demand for infertility medical care. Human Reproduction, 22, 1506–1512. doi:10.1093/humrep/dem046 [DOI] [PubMed] [Google Scholar]
- Boivin, J. , Takefman, J. E. , Tulandi, T. , & Brender, W. (1995). Reactions to infertility based on extent of treatment failure. Fertility and Sterility, 63, 801–807. [PubMed] [Google Scholar]
- Canavarro, M. C. (1999). Inventário de sintomas psicopatológicos: BSI [The Brief symptom inventory] In Simões M. R., Gonçalves M. M. & Almeida L. S. (Eds.), Testes e provas psicológicas em Portugal [Assessment instruments in Portugal], Vol. 2 (pp. 95–109). Braga, Portugal: APPORT. [Google Scholar]
- Cheung, M. W.‐L. (2009). Comparison of methods for constructing confidence intervals of standardized indirect effects. Behavior Research Methods, 41, 425–438. doi:10.3758/BRM.41.2.425 [DOI] [PubMed] [Google Scholar]
- Derogatis, L. R. (1982). BSI: Brief symptom inventory. Minneapolis, MN: National Computers Systems. [Google Scholar]
- Dunkel‐Schetter, C. , & Lobel, M. (1991). Psychological reactions to infertility In Stanton A. L. & Dunkel‐Schetter C. (Eds.), Infertility: Perspectives from stress and coping research (pp. 29–57). New York, NY: Plenum Press. [Google Scholar]
- Edelmann, R. J. , & Connolly, K. J. (2000). Gender differences in response to infertility and infertility investigations: Real or illusory? British Journal of Health Psychology, 5, 365–375. doi:10.1348/135910700168982 [Google Scholar]
- Eugster, A. , & Vingerhoets, A. J. J. M. (1999). Psychological aspects of in vitro fertilization: A review. Social Science & Medicine, 48, 575–589. doi:10.1016/S0277‐9536(98)00386‐4 [DOI] [PubMed] [Google Scholar]
- Fekkes, M. , Buitendijk, S. E. , Verrips, G. H. W. , Braat, D. D. M. , Brewaeys, A. M. A. , Dolfing, J. G. , … Macklon, N. S. (2003). Health‐related quality of life in relation to gender and age in couples planning IVF treatment. Human Reproduction, 18, 1536–1543. doi:10.1093/humrep/deg276 [DOI] [PubMed] [Google Scholar]
- Gameiro, S. , Boivin, J. , Peronace, L. , & Verhaak, C. (2012). Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment. Human Reproduction Update, 18, 652–669. doi:10.1093/humupd/dms031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greil, A. L. (1997). Infertility and psychological distress: A critical review of the literature. Social Science & Medicine, 45, 1679–1704. doi:10.1016/S0277‐9536(97)00102‐0 [DOI] [PubMed] [Google Scholar]
- Greil, A. L. , Leitko, T. A. , & Porter, K. L. (1988). Infertility: His and hers. Gender & Society, 2, 172–199. doi:10.1177/089124388002002004 [Google Scholar]
- Greil, A. L. , Shreffler, K. M. , Schmidt, L. , & McQuillan, J. (2011). Variation in distress among women with infertility: Evidence from a population‐based sample. Human Reproduction, 26, 2101–2112. doi:10.1093/humrep/der148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, A. F. (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76, 408–420. doi:10.1080/03637750903310360 [Google Scholar]
- Holter, H. , Anderheim, L. , Bergh, C. , & Moller, A. (2006). First IVF treatment–short‐term impact on psychological well‐being and the marital relationship. Human Reproduction, 21, 3295–3302. doi:10.1093/humrep/del288 [DOI] [PubMed] [Google Scholar]
- Hu, L. , & Bentler, P. M. (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3, 424–453. doi:10.1037/1082‐989X.3.4.424 [Google Scholar]
- Jordan, C. , & Revenson, T. A. (1999). Gender differences in coping with infertility: A meta‐analysis. Journal of Behavioral Medicine, 22, 341–358. doi:10.1023/A:1018774019232 [DOI] [PubMed] [Google Scholar]
- Kenny, D. A. , Kashy, D. A. , & Cook, W. L. (2006). Dyadic data analysis. New York, NY: The Guilford Press. [Google Scholar]
- Kline, R. B. (2005). Principles and practice of structural equation modeling (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Koert, E. , & Daniluk, J. C. (2010). Sexual transitions in the lives of adult women In Miller T. W. (Ed.), Handbook of stressful transitions across the lifespan (pp. 235–252). New York, NY: Springer. [Google Scholar]
- Lazarus, R. S. , & Folkman, S. (1984). Stress, appraisal, and coping. New York, NY: Springer. [Google Scholar]
- Lok, I. H. , Lee, D. T. , Cheung, L. P. , Chung, W. S. , Lo, W. K. , & Haines, C. J. (2002). Psychiatric morbidity amongst infertile chinese women undergoing treatment with assisted reproductive technology and the impact of treatment failure. Gynecologic and Obstetric Investigation, 53, 195–199. doi:10.1093/humrep/deh414 [DOI] [PubMed] [Google Scholar]
- Lowyck, B. , Luyten, P. , Corveleyn, J. , D'Hooghe, T. , Buyse, E. , & Demyttenaere, K. (2009). Well‐being and relationship satisfaction of couples dealing with an in vitro fertilization/intracytoplasmic sperm injection procedure: A multilevel approach on the role of self‐criticism, dependency, and romantic attachment. Fertility and Sterility, 91, 387–394. doi:10.1016/j.fertnstert.2007.11.052 [DOI] [PubMed] [Google Scholar]
- MacKinnon, D. P. , & Fairchild, A. J. (2009). Current directions in mediation analysis. Current Directions in Psychological Science, 18, 16–20. doi:10.1111/j.1467‐8721.2009.01598.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon, D. P. , Lockwood, C. M. , & Williams, J. (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–128. doi:10.1207/s15327906mbr3901_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markestad, C. L. , Montgomery, L. M. , & Bartsch, R. A. (1998). Infertility and length of medical treatment effects on psychological, marital, and sexual functioning. International Journal of Rehabilitation and Health, 4, 233–243. doi:10.1023/A:1022966829561 [Google Scholar]
- Matsubayashi, H. , Hosaka, T. , Izumi, S.‐I. , Suzuki, T. , & Makino, T. (2001). Emotional distress of infertile women in Japan. Human Reproduction, 16, 966–969. doi:10.1093/humrep/16.5.966 [DOI] [PubMed] [Google Scholar]
- Menning, B. E. (1980). The emotional needs of infertile couples. Fertility and Sterility, 34, 313–319. [DOI] [PubMed] [Google Scholar]
- Moura‐Ramos, M. , Gameiro, S. , Canavarro, M. C. , & Soares, I. (2012). Assessing infertility stress: Re‐examining the factor structure of the Fertility Problem Inventory. Human Reproduction, 27, 496–505. doi:10.1093/humrep/der388 [DOI] [PubMed] [Google Scholar]
- Moura‐Ramos, M. , Gameiro, S. , Canavarro, M. C. , Soares, I. , & Santos, A. T. (2012). The indirect effect of contextual factors on the emotional distress of infertile couples. Psychology and Health, 27, 533–549. doi:10.1080/08870446.2011.598231 [DOI] [PubMed] [Google Scholar]
- Newton, C. R. , Sherrard, W. , & Glavac, I. (1999). The Fertility Problem Inventory: Measuring perceived infertility‐related stress. Fertility and Sterility, 72, 54–72. doi:10.1016/S0015‐0282(99)00164‐8 [DOI] [PubMed] [Google Scholar]
- Nishioka, H. (2003). Low fertility and family policies in Southern European countries. Journal of Population and Social Security, 1(Suppl), 262–294. [Google Scholar]
- Peddie, V. L. , van Teijlingen, E. , & Bhattacharya, S. (2005). A qualitative study of women's decision‐making at the end of IVF treatment. Human Reproduction, 20, 1944–1951. doi:10.1093/humrep/deh857 [DOI] [PubMed] [Google Scholar]
- Pinborg, A. , Hougaard, C. O. , Andersen, A. N. , Molbo, D. , & Schmidt, L. (2009). Prospective longitudinal cohort study on cumulative 5‐year delivery and adoption rates among 1338 couples initiating infertility treatment. Human Reproduction, 24, 991–999. doi:10.1093/humrep/den463 [DOI] [PubMed] [Google Scholar]
- Shrout, P. E. , & Bolger, N. (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7, 422–445. doi:10.1037/1082‐989X.7.4.422 [PubMed] [Google Scholar]
- Sina, M. , Ter Meulen, R. , & Carrasco de Paula, I. (2010). Human infertility: Is medical treatment enough? A cross‐sectional study of a sample of Italian couples. Journal of Psychosomatic Obstetrics and Gynaecology, 31, 158–167. doi:10.3109/0167482x.2010.487952 [DOI] [PubMed] [Google Scholar]
- Slade, P. , Emery, J. , & Lieberman, B. A. (1997). A prospective, longitudinal study of emotions and relationships in in‐vitro fertilization treatment. Human Reproduction, 12, 183–190. doi:10.1093/humrep/12.1.183 [DOI] [PubMed] [Google Scholar]
- Stanton, A. L. , & Dunkel‐Schetter, C. (1991). Psychological adjustment to infertility: An overview of conceptual approaches In Stanton A. L. & Dunkel‐Schetter C. (Eds.), Infertility: Perspectives from stress and coping research (pp. 3–16). New York, NY: Plenum Press. [Google Scholar]
- Sydsjo, G. , Ekholm, K. , Wadsby, M. , Kjellberg, S. , & Sydsjo, A. (2005). Relationships in couples after failed IVF treatment: A prospective follow‐up study. Human Reproduction, 20, 1952–1957. doi:10.1093/humrep/deh882 [DOI] [PubMed] [Google Scholar]
- Verhaak, C. M. , Smeenk, J. M. , Evers, A. W. , Kremer, J. A. , Kraaimaat, F. W. , & Braat, D. D. (2007). Women's emotional adjustment to IVF: A systematic review of 25 years of research. Human Reproduction Update, 13, 27–36. doi:10.1093/humupd/dml040 [DOI] [PubMed] [Google Scholar]
- Verhaak, C. M. , Smeenk, J. M. , Evers, A. W. , van Minnen, A. , Kremer, J. A. , & Kraaimaat, F. W. (2005). Predicting emotional response to unsuccessful fertility treatment: A prospective study. Journal of Behavioural Medicine, 28, 181–190. doi:10.1007/s10865‐005‐3667‐0 [DOI] [PubMed] [Google Scholar]
- Verhaak, C. M. , Smeenk, J. M. J. , van Minnen, A. , Kremer, J. A. , & Kraaimaat, F. W. (2005). A longitudinal, prospective study on emotional adjustment before, during and after consecutive fertility treatment cycles. Human Reproduction, 20, 2253–2260. doi:10.1093/humrep/del355 [DOI] [PubMed] [Google Scholar]
- Volgsten, H. , Skoog Svanberg, A. , & Olsson, P. (2010). Unresolved grief in women and men in Sweden three years after undergoing unsuccessful in vitro fertilization treatment. Acta Obstetrica Gynecologica Scandinavica, 89, 1290–1297. doi:10.3109/00016349.2010.512063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, K. , Li, J. , Zhang, J. X. , Zhang, L. , Yu, J. , & Jiang, P. (2007). Psychological characteristics and marital quality of infertile women registered for in vitro fertilization ‐ intracytoplasmic sperm injection in China. Fertility and Sterility, 87, 792–798. doi:10.1016/j.fertnstert.2006.07.1534 [DOI] [PubMed] [Google Scholar]
- Zegers‐Hochschild, F. , Adamson, G. D. , de Mouzon, J. , Ishihara, O. , Mansour, R. , Nygren, K. , … van der Poel, S. (2009). The international committee for monitoring assisted reproductive technology (ICMART) and the World Health Organization (WHO) revised glossary on ART terminology. Human Reproduction, 24, 1–5. doi:10.1093/humrep/dep343 [DOI] [PubMed] [Google Scholar]


