Abstract
Introduction
This paper reports the key findings of the Faculty of Radiation Oncology 2014 workforce census and compares the results with earlier surveys.
Methods
The census was conducted in mid‐2014 with distribution to all radiation oncologists, educational affiliates and trainees listed on the college database. There were six email reminders and responses were anonymous. The overall response rate was 76.1%.
Results
The age range of fellows was 32–96 (mean = 49 years, median = 47 years). The majority of the radiation oncologists were male (n = 263, 63%). The minority of radiation oncologists were of Asian descent (n = 43, 13.4%). Radiation oncologists graduated from medical school on average 23 years ago (median = 22 years). A minority of fellows (n = 66, 20%) held another postgraduate qualification. Most radiation oncologists worked, on average, at two practices (median = 2, range 1–7). Practising radiation oncologists worked predominantly in the public sector (n = 131, 49%), but many worked in both the public and private sectors (n = 94, 37%), and a minority worked in the private sector only (n = 38, 14%). The largest proportion of the workforce was from New South Wales accounting for 29% of radiation oncologists. Radiation oncologists worked an average of 43 h/week (median = 43 h, range 6–80). Radiation oncologists who worked in the private sector worked less hours than their public sector or public/private sector colleagues. (38.3 vs. 42.9 vs. 44.3 h, P = 0.042). Victorians worked the fewest average hours per week at 38 h and West Australians the most at 46 h/week. Radiation oncologists averaged 48 min for each new case, 17 min per follow up and 11 min for a treatment review. Radiation oncologists averaged 246 new patients per year (median = 250, range = 20–600) with men (average = 268), Western Australians (average = 354) and those in private practice seeing more (average = 275). Most radiation oncologists considered themselves as specialists (n = 151, 60%), but nearly all those from South Australia were generalists (n = 15, 94%) as were three‐quarters of those from private practice. A minority of radiation oncologist respondents (10%) intended to retire within 5 years with a further 16% within 10 years.There was a stabilisation of trainee numbers in Australia and New Zealand with no increase compared with 2010 (142 in 2014 vs. 143 in 2010). The most common age bracket for trainees remained 31–35 years. One‐third of trainees were of Asian descent and nearly half held other degrees. The majority of trainees were satisfied with their career, but 30% were not entirely satisfied. Nearly half of trainee respondents would have reconsidered their choice of specialty had they known about the possible oversupply in the workforce with 12.4% undecided about continuing their career in radiation oncology. There were still 16% of trainees with no protected time during the working week, and a further 21% with only 1 h. Only one trainee respondent preferred to work in private practice, and job availability remained a concern for 89% of respondents.
Conclusions
The radiation oncologist workforce numbers have increased at a much slower rate, and unemployment remained low. Many parameters remained similar to the 2010 survey. However, there has been a decrease in the average number of new patients seen per year, working hours and also a slight decrease in the time spent per new patient. The trainee numbers have stabilised, but job availability remained a concern. A significant proportion of trainees were not satisfied with their career.
Keywords: census, radiation oncologist, trainee, workforce
Introduction
The Faculty of Radiation Oncology (FRO) undertook the fifth workforce survey of radiation oncologists and trainees across Australia and New Zealand in 2014. The previous surveys were undertaken in 1996, 2000, 2006 and 2010.1, 2, 3, 4 The purpose of the 2010 survey was to create a faculty workforce database that could be updated regularly to analyse workforce trends and to create workforce models to predict future staffing and training requirements.4 Hence, the 2014 survey built on the previous data and also supplemented information collected from the FRO facilities surveys and workforce projections.
For the first time, the survey was called a census which reflected the distribution to all radiation oncology members listed as active in the college membership database (life, fellow, educational affiliate, temporarily inactive, trainee and area of need practitioners).
A companion paper dealing specifically with New Zealand accompanies this one online. The census is included in Appendix S1.
Methods
The 2014 workforce census of all active radiation oncologists and trainees was conducted in July–September 2014. The questions were based on the FRO 2010 workforce survey and were discussed and tested by members of the Faculty Economics and Workforce Committee.
It was thought appropriate to replicate most of the 2010 questions as we wanted to establish workforce trends. However, the question on interest in systemic therapy was deleted. The principal author (JL) added a question on ethnic origin in this census.
The census invitation was distributed via Survey Monkey in July 2014 with six weekly email reminders. The census was closed on 10 September 2014. The decision was made to close the census at this date because there had been few responses in the last two email reminders. Hard copies were posted to those without an email address and to non‐respondents at the end of the 6 weeks.
The number of respondents was different between questions because the census was configured with certain rules. For example, if a respondent identified themselves as ‘fully retired’, then questions about work place and work hours were omitted. Some respondents also did not answer every question.
The responses were analysed to highlight the known and emerging workforce trends. The analysis was done with IBM Statistical Package for the Social Sciences (SPSS) Statistics V19 (IBM Corp., Armonk, NY, USA).
Results
Eligible study sample
Radiation oncologists and trainees registered in the Royal Australian and New Zealand College of Radiologists (RANZCR) database as of 30 June 2014 were eligible and invited to participate. This included those who were overseas at the time. The census was thus sent to 439 radiation oncologists with responses from 330 (75.2%). Table 1 summarises the population and respondents. There were 112 responses from the trainees (78.9%). The total response rate was 76.1%.
Table 1.
Population and respondents
| N | n | Response rate (%) | |
|---|---|---|---|
| Fellows | 397 | 303 | 76.3 |
| Life members | 1 | 1 | 100.0 |
| Retired members | 30 | 17 | 56.6 |
| Educational affiliates | 11 | 9 | 81.8 |
| Trainees | 142 | 112 | 78.9 |
| Total | 581 | 442 | 76.1 |
A number of radiation oncologists identified themselves as being retired (n = 17). These respondents were not asked the questions pertaining to practising radiation oncologists.
An analysis of non‐respondents was undertaken on member demographics, including age, gender and number of years as a fellow. Analysis revealed similarities between demographics and thus the results were not thought to be influenced by non‐responder bias within any one category.
The category of educational affiliates is equivalent to the previous category of International Medical Graduates. These educational affiliates typically are:
Currently assessed as comparable with an Australian or New Zealand trained radiation oncologist and working towards phase 2 examinations.
Working as an area of need consultant in Australia.
Working with vocational scope of practice registration in New Zealand.
Personal and demographic data
The average age of fellows was 49.3 years with a median of 46.8 years (range 31.6–95.5). The educational affiliates had an average age of 49.1 years with a median of 44.3 years (range 39.4–68.7).
Men accounted for the majority of radiation oncologists (n = 263, 62.5%), all life members and the majority of educational affiliates (n = 8, 72.7%). Men accounted for a small majority of trainees (n = 79, 55.6%) compared with women (n = 63, 44.0%). Most trainees were aged between 25 and 34 years old with one trainee aged over 45.
Most radiation oncologists were of either Australian (54.4%) or New Zealand (12.1%) ethnic origin, with a substantial minority of Asian (Chinese, South East Asian, other Asian) (13.4%) and Indian (7.9%) descent. No respondents identified themselves of Aboriginal or Torres Island descent. Thirty per cent of trainees were of Asian origin.
Radiation oncologists graduated from medical school on average 23 years ago (median = 22.0; range 8–48). A substantial minority of practising radiation oncologists held a postgraduate qualification (n = 66, 20.1%). This included 29 having an MD, 24 holding masters and 12 holding a PhD. With respect to trainees, nearly half of respondents (n = 51, 48.6%) held other degrees besides their basic medical degree including bachelors (n = 41), masters (n = 6), postgraduate diploma (n = 2) and doctorates (n = 2).
Practice location and work hours
Fellows worked at an average of 2.1 locations with a median of 2.0 (range 1–7). Figure 1 depicts the frequency for all practising radiation oncologists. Educational affiliates reported working at an average of 2.5 locations with a median of 2.0 (range 2–4).
Figure 1.
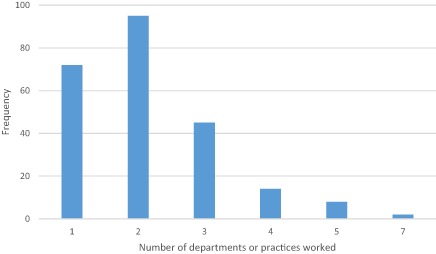
Number of practice locations worked by radiation oncologists.
The majority of practising radiation oncologists worked in the public sector (n = 131, 49%) with a minority working in the private sector (n = 38, 14%). However, a significant number worked in both public and private sectors (n = 100, 37%). All the educational affiliates worked in the public sector or a mixture of public/private with none working in the private sector only.
The largest proportion of the workforce was from New South Wales with the majority of radiation oncologists (n = 97, 29.4%) followed by Victoria, which had 65 radiation oncologists (19.7%). Table 2 gives the full breakdown.
Table 2.
Respondents by location
| State/country | n | % | Trainees (n) | Trainees (%) |
|---|---|---|---|---|
| New South Wales | 97 | 29.4 | 36 | 32.1 |
| Victoria | 65 | 19.7 | 20 | 17.9 |
| Queensland | 58 | 17.6 | 22 | 19.6 |
| South Australia | 21 | 6.4 | 6 | 5.4 |
| Western Australia | 14 | 4.2 | 2 | 1.8 |
| Tasmania | 5 | 1.5 | 2 | 1.8 |
| Northern Territory | 1 | 0.3 | 0 | 0.0 |
| Australian Capital Territory | 8 | 2.4 | 5 | 4.5 |
| New Zealand | 48 | 14.5 | 16 | 14.3 |
| Overseas | 13 | 3.9 | 3 | 2.7 |
| Total | 330 | 100.0 | 112 | 100.0 |
Work hours
The number of reported hours spent working at each practice location was summarised to provide the total number of actual hours and clinical hours spent per week (Table 3).
Table 3.
Reported actual and clinical hours per week
| Category | Actual hours | Clinical hours | ||||
|---|---|---|---|---|---|---|
| Mean | Median | Range | Mean | Median | Range | |
| Fellow (overall) | 42.7 | 43.0 | 8–80 | 33.5 | 34.0 | 8–80 |
| Educational affiliate (overall) | 51.5 | 52.0 | 45–57 | 42.4 | 43.0 | 31–50 |
There were significant differences between male and female fellows for reported actual and clinical hours per week, with men reporting an average of 45.5 actual hours (median 45.0) compared with an average of 38.3 h (median = 40.0) for women (P < 0.001). Men reported an average of 34 clinical hours (median 35.5) per week compared with an average of 31.5 h (median = 30.0) for women (P = 0.011).
Radiation oncologists in the private sector worked less average hours than their public sector or public/private sector colleagues (38.3 vs. 42.9 vs. 44.3 h, respectively; P = 0.042). Radiation oncologists in private practice spent a significantly a higher percentage of their time on clinical work than those in public or combined public/private practice (87.6%, 78.6% and 78.8%; P = 0.003).
The reported actual and clinical work hours worked per week for radiation oncologists and educational affiliates was broken down by geographical location (Table 4). Victorians worked the fewest average actual hours per week (38.3) and New Zealand members the highest (46.6), while New South Wales members reported the lowest average number of clinical hours per week (31.7) and Western Australians the highest (37.9). The one respondent from Northern Territory was excluded.
Table 4.
Reported actual and clinical hours per week by geographical location for radiation oncologists
| n | Actual hours | Clinical hours | |||||
|---|---|---|---|---|---|---|---|
| Mean | Median | Range | Mean | Median | Range | ||
| New South Wales | 81 | 43.4 | 42.0 | 16–80 | 31.7 | 30.0 | 4–56 |
| Victoria | 54 | 38.3 | 40.0 | 6–60 | 32.5 | 33.0 | 4–56 |
| Queensland | 49 | 42.8 | 42.5 | 8–78 | 34.2 | 34.0 | 5–58 |
| South Australia | 17 | 40.1 | 10.0 | 15–65 | 32.4 | 32.0 | 12–55 |
| Western Australia | 12 | 45.9 | 46.5 | 25–63 | 37.9 | 39.0 | 20–53 |
| Tasmania | 4 | 40.3 | 40.5 | 23–57 | 32.8 | 29.5 | 15–57 |
| Northern Territory | 1 | 45.0 | 45.0 | – | 40.0 | 40.0 | – |
| Australian Capital Territory | 6 | 46.0 | 46.0 | 32–60 | 35.3 | 30.0 | 20–55 |
| New Zealand | 43 | 47.0 | 50.0 | 24–60 | 36.3 | 40.0 | 15–50 |
Radiation oncologists spent their working hours on activities as depicted in Table 5. These figures do not exactly correlate with the previous estimate of 42 h/week because they provide estimates from two different questions.
Table 5.
Hours per week spent on activities for radiation oncologists
| Activity | Fellow | Educational affiliate/international medical graduates | ||||
|---|---|---|---|---|---|---|
| Mean | Median | Range | Mean | Median | Range | |
| New cases | 6.7 | 6.0 | 1–20 | 7.0 | 6.0 | 4–10 |
| Follow ups | 8.6 | 8.0 | 1–30 | 9.0 | 9.0 | 3–16 |
| On treatment reviews | 4.8 | 4.0 | 1–20 | 3.8 | 3.0 | 2–8 |
| Planning | 7.3 | 6.4 | 1–21 | 8.8 | 8.0 | 5–15 |
| Supervision | 4.6 | 3.0 | 1–40 | 2.6 | 2.0 | 2–5 |
| Teaching | 1.6 | 1.0 | 1–8 | 1.2 | 1.0 | 1–2 |
| Research | 3.5 | 2.0 | 1–24 | 1.2 | 1.0 | 1–2 |
| Department/practice management | 4.4 | 2.0 | 1–40 | 6.0 | 6.0 | 2–10 |
| Jurisdiction/quality committee | 2.5 | 2.0 | 1–12 | 3.0 | 2.5 | 1–6 |
| Other | 4.9 | 4.0 | 1–17 | 5.0 | 4.0 | 2–10 |
The median clinical hours per week for trainees were 36–45 h. Table 6 gives a detailed breakdown.
Table 6.
Reported ‘clinical time’ per week for trainees
| Hours per week | Number | Percentage |
|---|---|---|
| ≤15 | 2 | 1.9 |
| 16–25 | 5 | 4.8 |
| 26–35 | 14 | 13.3 |
| 36–45 | 54 | 51.4 |
| 46–55 | 24 | 22.9 |
| >55 | 6 | 5.7 |
| Total | 105 | 100.0 |
New cases, follow ups, treatment reviews and planning hours
Male radiation oncologists spent more hours per week on new cases than their female counterparts with an average of 7.1 h (median = 6.0 h) compared with 6.1 h (median = 6.0 h) (P = 0.001). Men also spent more time on planning with an average of 7.7 h/week (median = 8.0 h) compared with the women's average of 6.6 h/week (median = 6.0) hours (P = 0.016).
Respondents spent an average of 47.9 min (median = 45 min) per new case, 17 min (median = 15 min) per follow‐up case and 10.1 min (median = 10 min) per treatment review case. Women spent significantly more time on each treatment review (average 11.1 vs. 10.1; median 10.0 vs. 10.0 min) (P = 0.026). Those working exclusively in the private sector spent more time on follow‐up cases than their public or public/private sector colleagues with averages of 18.9 versus 17.2 versus 16.8 min, respectively (P = 0.043).
New Zealand radiation oncologists spent more time on new cases with an average of 57.5 min (median = 60.0 min, P = 0.001) and follow‐up cases with an average of 19.8 min (median = 20.0 min, P = 0.002) than others. Western Australian members spent the least amount of time on new cases and follow ups with averages of 41.9 and 15.0 min, respectively (P = 0.04).
Supervision, teaching and research hours
Women spent more time supervising registrars per week with an average of 6 h (median = 4 h) compared with the men's average of 3.6 h (median = 2 h; P = 0.001).
Those working in combined public/private sector roles also spent more time supervising registrars compared with those working in the public sector or private practices with averages of 5.9 versus 3.8 versus 3.2 h, respectively (P = 0.023).
Those in private practice spent more time per week on treatment reviews than those in public or combined public/private practice (6.6 vs. 4.1 vs. 4.8 h; P = 0.01).
Other hours
Male radiation oncologists spent more time on department/practice management than women with an average of 5 h (median = 3 h) compared with 3.2 h (median = 2 h; P = 0.025). Male radiation oncologists also spent more time on jurisdiction/hospital/quality committees than their female counterparts with an average of 2.9 h (median = 2.0 h) compared with 1.9 h (median = 1.0 h; P = 0.007).
New patients per year
Radiation oncologists reported seeing an average of 246 new patients per year (median 250; range 20–600). The Australian figure was 248 new patients per year (median 250; range 20–600). Table 7 depicts new patients per year by certain variables.
Table 7.
New patients seen per year
| Variable | N | Mean | Median | Range |
|---|---|---|---|---|
| Member type | ||||
| Fellow | 230 | 246 | 250 | 20–600 |
| Educational affiliate/international medical graduates | 7 | 251 | 250 | 200–300 |
| Australian fellow | 199 | 248 | 250 | 20–600 |
| Gender | ||||
| Male | 149 | 268 | 250 | 20–600 |
| Female | 88 | 208 | 200 | 25–480 |
| Sector | ||||
| Public | 115 | 227 | 225 | 20–600 |
| Private | 35 | 275 | 260 | 40–480 |
| Public/private | 87 | 260 | 250 | 25–600 |
| Branch | ||||
| New South Wales | 75 | 220 | 200 | 20–450 |
| Victoria | 47 | 235 | 240 | 25–600 |
| Queensland | 41 | 258 | 250 | 70–500 |
| South Australia | 14 | 320 | 275 | 150–600 |
| Western Australia | 13 | 354 | 350 | 220–500 |
| Tasmania | 3 | 250 | 250 | 200–300 |
| Northern Territory | 1 | 250 | 250 | – |
| Australian Capital Territory | 5 | 210 | 220 | 160–250 |
| New Zealand | 38 | 236 | 245 | 120–400 |
Male radiation oncologists reported seeing more new patients per year than women with averages of 268 and 208, respectively (P = 0.001). Western Australian members averaged 354 new patients per year compared with 210 per year for their Australian Capital Territory colleagues (P = 0.001). Those in the private sector averaged 275 new patients per year compared with 260 by those in combined public/private practice and 227 by those in the public sector. Figure 2 shows the overall distribution.
Figure 2.
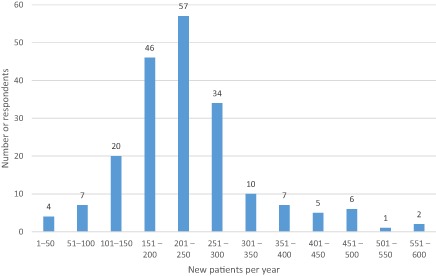
New patients per year.
Generalist or specialist
The majority (n = 151, 60.2%) indicated they were specialists and the minority (n = 100, 39.8%) identified themselves as generalists. A significant difference was from South Australia with nearly all indicating they were generalists (n = 15, 93.8%; P < 0.001).
Almost three‐quarters of those from private practice indicated that they were generalists, while two‐thirds from the public sector or combined public/private sectors were specialists. Those of European ethnic origin were more likely to identify as a generalist with those of Asian descent more likely to be specialists (P = 0.040). Two‐thirds of respondents (n = 160, 65.3%) indicated there should be more focus on subspecialty practice. The four most common areas of subspecialty practice were breast, head and neck, lung, and gastrointestinal cancers in descending order.
Future practice
Three‐quarters of respondents (n = 187, 74.2%) reported no intention to change their current work hours in the next 3 years, and over half of those who responded did not have an intention to retire in the foreseeable future (see Table 8). A small minority (10%) of respondents intended to retire within the next 5 years. In New Zealand, a quarter of the workforce intended to retire within 10 years and almost one half within 15 years.
Table 8.
Future intentions of radiation oncologists
| n | % | |
|---|---|---|
| Change work hours in next 3 years | ||
| Yes, increase hours | 18 | 7.2 |
| Yes, decrease hours | 47 | 18.7 |
| No change | 187 | 74.2 |
| Intention to retire | ||
| 0–5 years | 25 | 10.0 |
| 6–10 years | 39 | 15.5 |
| 11–15 years | 50 | 19.9 |
| Not in foreseeable future | 137 | 54.6 |
Early career
A small minority of five respondents (1.5%) indicated a period of unemployment following their election to fellowship (all women). The majority became a consultant (n = 157, 47.9%) or completed an advanced training or fellowship position (n = 125, 38.1%) or undertook locum work (n = 41, 12.5%).
Trainee perceptions of radiation oncology as a career
A majority of trainee respondents were satisfied with radiation oncology as a career (n = 74, 70.5%). However, when asked if they would have reconsidered their choice of specialty had they known there might be an oversupply in the workforce, half of the respondents (n = 53, 50.5%) agreed they would have.
The top factors influencing career choice were interest in oncology patients, lifestyle after training, use of technology and lifestyle during training. The detailed results are presented in Table 9.
Table 9.
Factors influencing career choice
| Factor | N | % |
|---|---|---|
| Interest in oncology patients | 97 | 86.6 |
| Lifestyle after training | 67 | 59.8 |
| Work hours | 62 | 55.4 |
| Use of technology | 59 | 52.7 |
| Lifestyle during training | 54 | 48.2 |
| Previous attachment as student or junior doctor | 53 | 47.3 |
| Family considerations | 38 | 33.9 |
| Interest in physics | 36 | 32.1 |
| Research opportunities | 32 | 28.6 |
| Reputation of staff | 30 | 26.8 |
| Training program reputation | 25 | 22.3 |
| Interest in radiobiology | 21 | 18.8 |
| Earning potential | 21 | 18.8 |
| Job availability | 14 | 12.5 |
| Other | 1 | 0.9 |
Trainee duties and protected time
The clinical duties and overtime are outlined in Appendix S2. The reported ‘protected’ time per week was a median of 2 h. Sixteen per cent reported no hours per week of protected time and 22% had 1 h or less. The results are listed in Table 10.
Table 10.
Protected time
| Hours per week | N (%) |
|---|---|
| 0 | 17 (16.2) |
| 1 | 23 (21.9) |
| 2 | 30 (28.6) |
| 3 | 19 (18.1) |
| 4 | 13 (12.2) |
| >5 | 3 (2.9) |
Part‐time training
A minority of respondents reported working (or planning to work) part‐time for a period of 12 months or longer during their training (n = 14, 13.3%). However, half of respondents (n = 52, 49.5%) reported that if given the option, they would prefer to do some training part‐time. Women were more likely than men to wish for part‐time training (P < 0.001).
Challenges associated with radiation oncology training
The most difficult aspects of radiation oncology training and sources of stress are included in Appendix S2.
The majority of respondents (n = 60, 57.7%) indicated they were not considering leaving the specialty. However, seven respondents (6.7%) reported that they were going to leave with the rest unsure.
Trainees future plans
The majority of respondents (84.8%, n = 89) reported that they plan to continue their career in radiation oncology, but a minority, 13 (12.4%) indicated that they were undecided. No differences were observed between gender, branch, country or age.
Three‐quarters of respondents indicated that they planned on undertaking a fellowship year after training (72.3%, n = 73) and 24 (23.8%) were undecided. Those aged less than 30 years were more likely than their older colleagues to be planning a fellowship year (P = 0.045). The majority of respondents who reported that they were planning a fellowship year were doing so to either be more competitive in the job market (94.5%, n = 69) or to gain specific skills and expertise (94.5%, n = 69). One‐fifth (21.9%; n = 16) indicated that it was required by the centre they would like to work at.
The majority of respondents (92.2%, n = 94) planned to have an academic component to their work. Of the eight respondents (7.8%) who indicated that they did not, they all noted that their primary interest was patient care, with two also reporting that writing papers was too time consuming or that they preferred not to do research.
Reasons for interest in an academic career included: interest in teaching (75.5%, n = 71), interest in clinical research (62.8%, n = 59), enjoyment of the academic environment (56.4%, n = 53), desire to practice in a large teaching centre (53.2%, n = 50), or interest in future leadership or administrative opportunities (41.5%, n = 39).
The majority of respondents were not bonded students (95.1%, n = 97).
Almost two‐thirds of the respondents (62.7%, n = 64) agreed/strongly agreed that they would like a job that allowed them to pursue their subspecialty clinical interests with a further 29.4% (n = 30) neutral/unsure.
Of the 48 trainees (47.5%) who wished to work part‐time during the first 10 years post training, 23 (47.9%) anticipated working 0.7–0.9 full‐time equivalent (FTE). Almost one‐quarter (22.9%, n = 11) were unsure what FTE they anticipated. Two‐thirds (66.7%, n = 32) indicated family commitments as the reason for planning part‐time work; half (50.0%, n = 24) cited lifestyle, and 41.6% (n = 20) cited maternity/parental leave.
Over half of the respondents (n = 60, 58.8%) reported that they intended to work in an urban department. Only three (2.9%) indicated an intent to work in a rural department. Over half (58.4%, n = 59) report a preference for combined public/private practice. One respondent preferred to work exclusively in private practice. The reasons for practice preference are outlined in Appendix S2.
Trainee concerns for the future
Participants were asked to identify their major concerns for the future. They were allowed to select more than one option. Job availability remained, by far, the major concern for 89.3% of respondents (Table 11).
Table 11.
Future concerns of trainees
| Concern | n | % |
|---|---|---|
| Job availability | 100 | 89.3 |
| Being potentially forced to work in a rural centre | 45 | 40.2 |
| Fellowship opportunities | 42 | 37.5 |
| Declining government resources | 42 | 37.5 |
| Other | 7 | 6.3 |
Comments by respondents
The last question allowed participants to add further comments regarding workforce issues. A small number provided comments including too many trainees coming through (n = 10), lack of consultant jobs (n = 5), suggestions for the census (n = 6), terminology (n = 3), the role of a radiation oncologist (n = 4) and reducing the number of new patients (n = 2).
Discussion
This was the fifth workforce survey of radiation oncologists across Australia and New Zealand, with previous surveys undertaken in 1996, 2000, 2006 and 2010.1, 2, 3, 4 The first trainees' survey was completed in 2012.5
The Economic and Workforce Committee and the Faculty noted the importance of doing regular workforce surveys, and it was thus resolved to do one every 4 years. It should also be noted that the results of the third survey in 2006 were not widely disseminated. Therefore some thought there was really a 10‐year gap between 2000 and 2010 before useful information could be accessed for college purposes. This was too long.
A separate New Zealand analysis will accompany this article online partly because potential workforce issues may be quite different between the two countries. New Zealanders have also been keen to have their own data. This paper presents the data for all Australian, New Zealand and overseas radiation oncologist respondents and trainees.
The response rate was 76.1%. Email reminders were sent out weekly to help ensure this reasonable response rate. The recent American workforce survey had a 29% response rate among radiation oncologists and trainees.6, 7 Similar surveys in the United States, United Kingdom and Canada have had response rates of around 50% and as low as 12%.8, 9, 10, 11, 12
The data revealed 439 active members (fellows, life members, educational affiliates and retired members) on the RANZCR database compared with 396 in 2010.4 The demographic data revealed the proportion of women in the workforce is increasing with them representing 37.5% of fellows.
The average and median age of fellows was 49.3 and 46.8 years, respectively (Australian figures 49.3 and 46.7 years), which was similar to 2010 (average = 49.4 years and median = 47.0 years). This might seem unusual as one would expect the workforce to be ageing, but a number of younger fellows have entered the profession.
This is the first time a question about ethnic origin has been asked. Ethnic origin in the American radiation oncology workforce was highlighted recently because of the lack of representation of American radiation oncologists from ethnic minorities to deal with an increasingly diverse society.13, 14
The work hours for radiation oncologists has also stabilised with an average of 42.7 h for fellows with the 2010 survey around 44 h and previous surveys up to 52 h. A surprising feature of the 2010 survey was that those in private practice averaged the least amount of hours at 40.9 h/week compared with those in the public sector or the combination. This trend has remained the same. The longer hours per week worked by Western Australians and New Zealanders reflected their relative shortage of radiation oncologists.
One of the more interesting and controversial areas is the number of new patients a radiation oncologist might and should see in a year. This single parameter in the past has defined a radiation oncologist workload more than any other. Some have highlighted that there are other important roles for radiation oncologists (communicator, collaborator, research expert, etc.), but nevertheless seeing new patients forms an integral part of a clinician's practice.15 This topic was researched several years ago and an attempt was made to make a definitive recommendation. However, there was such controversy that the final report was labelled as a report on contemporary practice rather than a guideline.15
The 2014 census showed a continual trend in a decrease in new patients seen per year, from averages of 342 in 1996, 300 in 1999, 275 in 2010 and 246 in 2014. Whether the decrease overall is due to an increased number in the workforce or other factors is unknown and beyond the scope of this paper. However, the optimal radiation therapy utilisation rate was recently revised down to 48.3%.16
The report on Contemporary Practice outlined the Faculty's view that 200–350 new patients per year was appropriate for full‐time clinical work with a lesser number for those devoting a significant period of time to administration, teaching, research and subspecialty areas such as brachytherapy/paediatrics/stereotactic radio surgery.
Radiation oncologists may be seeing fewer new patients per year compared with before, but a recent study showed nearly half (48.5%) of respondents scored highly in one dimension of burnout and over a third (37.5%) scored highly in two out of the dimensions of burnout, which would qualify them as having burnout.17
It was not surprising that those in private practice saw more new patients than their public sector or public/private sector colleagues (average of 278 versus 223 versus 262 in Australia), but the disparity was not as high as some might think.
The hours per week spent on specific activities were similar to the 2010 survey.4 The time spent on follow ups and treatment reviews were also similar to the 2010 survey, but time spent per new patient appeared to be less with 47.9 min on average (median = 45.0 min) compared with 51.9 min (median = 60.0 min) in 2010 (P = 0.023).4 Whether this is a statistical anomaly or because of other factors such as improved documentation is a matter of conjecture. There are some who might have thought it might take longer to see new patients in 2014 because of patient demands, compulsory consent forms and complexity of cases.
The findings that women spent less hours at work per week, saw less new cases per year and spent less time on certain activities than their male counterparts can certainly be partially explained by a greater proportion of them being involved in part‐time work.
The trend to subspecialisation continues with 60% considering themselves as specialists and one would expect that with increasing complexity of cases, specialised multidisciplinary meetings and complexity of contouring, this trend will continue. Two‐thirds of radiation oncologists thought more emphasis on subspecialty practice was needed which was similar to 2010 (72.1%).4
The minority of radiation oncology respondents (n = 25, 10.0%) intended to retire within the next 5 years. There are currently at least 20 trainees passing phase 2 examinations each year. It is unknown if this trend continues, whether the workforce will be able to absorb all these potential practitioners. However, in New Zealand, there may be a shortage of radiation oncologists with close to half intending to retire within 15 years. This may be exacerbated by the relative small number with even a small change in absolute numbers having a significant impact.
There were 143 trainees in Australia and New Zealand in 2010, compared with 142 in 2014. A major concern has been the potential oversupply of trainees flowing into the workforce. Job availability in this and the previous survey has been by far the major concern. These figures may partially alleviate this concern as it at least shows the trainee numbers are not increasing at the rapid rate documented previously. The period from the early 2000s to 2010 revealed trainee numbers increasing from 57 to 143.
The other relevant point to note was that 1.5% of members reported a period of unemployment prior to becoming a consultant (see census paper on radiation oncologists). This was actually less than in 2010 when 2.6% of members reported unemployment after passing their phase 2 examinations. This would suggest that trainees, despite concerns, are still managing to find employment at least in 2014. However, it is acknowledged that vigilance is still required on workforce numbers.
The majority of trainees were satisfied with their choice of radiation oncology as a career (70.5%), but this was less than the previous survey in 2012, which revealed over 90% satisfaction.5 This current lesser proportion may be related to the fact that nearly half would have reconsidered their career choice had they known about the potential lack of job availability. The current census could have explored why 30% of trainees were not satisfied with their career choice. Since this has not been adequately explored in the current census, the responsibility may fall upon the Radiation Oncology Education and Training Committee and Directors of Training to explore this further. The high proportion of trainees satisfied with their network was almost identical to the previous survey (82.9% vs. 82.0%), but again further analysis of those dissatisfied with their network might be undertaken.
A report commissioned by the College on curriculum evaluation and training networks found high satisfaction with the curriculum and networks. However, dissatisfaction was expressed sometimes with the lack of communication within the network especially by those not attending network governance meetings. Trainees also thought that the level of clinical supervisor engagement was low. This was in contrast to the high level of engagement by training network directors, directors of training and education support officers. Some measures to address these issues include circulation of the minutes of meetings, having open meetings and targeting and training clinical supervisors.18
A significant issue for trainees was protected time, with the last survey in 2012 revealing nearly half of trainees having one or less hours per week and over 30% having no hours, against the RANZCR recommendation of 4 h/week. The figures have improved, but there were still nearly 40% of trainees reporting one or less hours of protected time per week with 16% having no protected time at all. There were only 15% who had 4 h/week or more.
The other aspects of the trainees' census such as factors influencing career choice, clinical duties and overtime; most difficult aspects of radiation oncology; difficulty in maintaining currency in general medicine; approval of research mentor; desire for part‐time training; and sources of stress remained similar to the 2012 trainees survey.5 The detailed data are included in Appendix S2.
Conclusions
The 2014 RANZCR FRO workforce census continued the accumulation of data and established some workforce trends from previous surveys.
The average age of fellows remains similar to the 2010 survey, as did gender distribution, working hours, number of practices worked, interest in speciality practice and time spent on non‐clinical work. Radiation oncologists in private practice continue to spend less hours at work than their public sector or public/private sector colleagues. Radiation oncologists continue to see fewer new patients per year (average = 246) compared with previous surveys.
There has been a stabilisation of trainee numbers and there remained low unemployment after completion of training. Job availability remained the major concern and half of trainee respondents would have reconsidered their choice of career had they known about a possible oversupply in the workforce. One‐third were not entirely satisfied with radiation oncology as a career, and a minority were considering not completing training. Protected time remains a significant issue for trainees although this has improved from the last survey.
It is hoped that the future workforce studies will continue and the data will be analysed further in relation to workforce requirements and demand for radiotherapy services. This will assist the FRO RANZCR to support its members and develop strategies to deal with workforce issues.
Supporting information
Appendix S1. Workforce Census Questionnaire.
Appendix S2. Trainees.
File S1. Faculty of Radiation Oncology 2014 workforce census: New Zealand.
Acknowledgements
The authors would like to acknowledge members of the Economic and Workforce committee: Dion Forstner, Raphael Chee, Michael Poulsen, Marcus Dreosti, Art Kaminski, Gill Duchesne, Marie Burke, Thuy Pham, Sonja Cronjé and Legend Lee for their encouragement and advice. The authors would also like to thank Samantha Campbell for typing this manuscript and the fellows and trainees who participated in this census.
J Leung MB BS, FRANZCR; PL Munro BA, B Com, MEd, PhD, PGDIPArts; M James MB BS(Hons), BSC, FRANZCR.
Conflict of interest: None.
References
- 1. Stevens G, Berry M, Firth I. Faculty of Radiation Oncology Survey of work procedures. Australas Radiol 1999; 43: 233–242. [DOI] [PubMed] [Google Scholar]
- 2. Veness M, Rikard‐Bell G, Ward J. Australian and New Zealand radiation oncology work practices in 2000. Australia Radiol 2003; 47: 146–151. [DOI] [PubMed] [Google Scholar]
- 3. Robson C, Cheetham L. Faculty of Radiation Oncology Workforce Survey 2006. Royal Australian and New Zealand College of Radiologists, Sydney 2007.
- 4. Leung J, Vukolova N. Faculty of Radiation Oncology 2010 workforce survey. J Med Imaging Radiat Oncol 2011; 55: 622–632. [DOI] [PubMed] [Google Scholar]
- 5. Leung J, Le H, Tumer S et al Faculty of Radiation Oncology 2012 trainee survey; perspectives on choice of specialty training and future work practice preferences. J Med Imaging Radiat Oncol 2014; 58: 125–133. [DOI] [PubMed] [Google Scholar]
- 6. Pohar S, Fung CY, Hopkins S et al American Society for Radiation Oncology (ASTRO) 2012 workforce study: the radiation oncologists' and residents' perspectives. Int J Radiat Oncol Biol Phys 2013; 87: 1135–1140. [DOI] [PubMed] [Google Scholar]
- 7. Victare A, Washington R, Patton C et al An assessment of the current U.S. radiation oncology workforce: methodology and global results of the American Society for Radiation Oncology 2012 workforce study. Int J Radiat Oncol Biol Phys 2013; 87: 1129–1134. [DOI] [PubMed] [Google Scholar]
- 8. Wilson L, Flynn D, Haffty B. Radiation oncology career decision variables for graduating trainees seeking positions in 2003–2004. Int J Radiat Oncol Biol Phys 2005; 62: 519–525. [DOI] [PubMed] [Google Scholar]
- 9. MacLeod N, Hill E, Davis R et al Oncology Registrars' Forum trainee survey 2011 2012. [Cited 14 Sept 2014.] Available from URL: http://www.rcr.ac.uk/docs/oncology/pdf/ORF%20survey%202011%20oct%202011%20FINAL%2027%2010%2011.pdf
- 10. Debenham B, Banerjee R, Fairchild A et al 2009 Canadian radiation oncology resident survey. Int J Radiat Oncol Biol Phys 2012; 82: 1326–1331. [DOI] [PubMed] [Google Scholar]
- 11. Jagsi R, Chronowski G, Buck D et al Special report: results of the 2000–2002 Association of Residents in Radiation Oncology (ARRO) surveys. Int J Radiat Oncol Biol Phys 2004; 59: 313–318. [DOI] [PubMed] [Google Scholar]
- 12. Mattes M, Kharofa J, Zeidan Y et al Results of the 2012–2013 Association of Residents in Radiation Oncology (ARRO) job search and career planning survey of graduating residents in the United States. Int J Radiat Oncol Biol Phys 2014; 88: 25–32. [DOI] [PubMed] [Google Scholar]
- 13. Winkfield K, Gabeau D. Why workforce diversity in oncology matters. Int J Radiat Oncol Biol Phys 2013; 85: 900–901. [DOI] [PubMed] [Google Scholar]
- 14. Chapman C, Hwang W, Deville C. Diversity based on race, ethnicity and sex, of US radiation oncology physician workforce. Int J Radiat Oncol Biol Phys 2013; 85: 912–918. [DOI] [PubMed] [Google Scholar]
- 15. Faculty of Radiation Oncology . Report on Contemporary practice; the number of new patients per year. 2011. [Cited 14 Sept 2014.] Available from URL: www.ranzcr.edu.au/resources/professionaldocuments/practicestandards/radiationoncologystandards
- 16. Barton M, Jacob S, Shafiq J et al Estimating the demand for radiotherapy from evidence: a review ofchange from 2003 to 2012. Radiother Oncol 2014; 112: 140–144. [DOI] [PubMed] [Google Scholar]
- 17. Leung J, Rioseco P, Munro P. Stress, satisfaction and burnout amongst Australian and New Zealand radiation oncologists. J Med Imaging Radiat Oncol 2014; 58: 125–133. [DOI] [PubMed] [Google Scholar]
- 18. Siggins Miller . Evaluation of the Royal Australian and New Zealand College of Radiologists (RANZCR) training program curriculum for radiation oncology (Australia and New Zealand). Final training program curriculum evaluation report. RANZCR 2014.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Workforce Census Questionnaire.
Appendix S2. Trainees.
File S1. Faculty of Radiation Oncology 2014 workforce census: New Zealand.


