Abstract
Objective To evaluate the incremental effect of a graphic weigh‐scale values clarification exercise to explicitly consider the personal importance of the benefits versus the risks in a woman's decision aid regarding postmenopausal hormone therapy.
Design Randomized controlled trial.
Intervention Decision aid including information on options, benefits and risks, and their probabilities either followed by: (1) a graphic weigh‐scale values clarification exercise to explicitly consider the personal importance of each benefit and risk; or (2) a summary of the main benefits and risks to implicitly consider benefits versus the risks.
Sample Two‐hundred and one women aged 50–69 years from Ottawa, Canada, who had never used hormone therapy.
Outcome Perceived clarity of values, a sub‐scale of the decisional conflict scale; congruence between personal values of benefits and risks (measured on 0–10 importance rating scale) and choices (accept, decline, unsure regarding preventive hormone therapy [HRT]) using discriminant function analysis.
Results There were no statistically significant differences between interventions in perceived clarity of values and overall congruence between values and choices. Amongst those choosing HRT, there was a trend in those exposed to the graphic weigh‐scale exercise to have better congruence between values and choices compared to implicit values clarification (P = 0.06).
Conclusion The use of the graphic weigh‐scale exercise in a decision aid conveys no overall short‐term benefit. Further study is needed to specifically determine effects in those changing the status quo and on the quality of patient‐practitioner communication and persistence with decisions.
Keywords: decision making, decision support techniques, hormone replacement therapy, informed consent, patient participation, values
Introduction
Practice guidelines for treatment decisions that are considered `values sensitive' recommend that practitioners discuss with their patients not only the personal probability or likelihood of the benefits and harms, but also the personal value or desirability that patients attach to them. 1 , 2, 3, –4 For example, in the case of preventive hormone therapy (HRT) after menopause, a woman needs to weigh up both the likelihood and the desirability of protection from osteoporosis and heart disease and relief of menopausal symptoms against the possible increased risk of breast and endometrial cancer, the side‐effects of HRT, and her attitudes toward taking long‐term preventive medication. To support decision making about such complex issues, shared decision making programmes or patient decision aids have been developed as adjuncts to counselling. 5 , 6, 7, 8, 9, 10, –11 All of the decision aids provide information on the options and outcomes, including details regarding their functional impact and probabilities of occurrence for a given set of risk factors. Although the detailed information on outcomes assists patients to judge their value, it is not known whether the implicit consideration of outcomes goes far enough in clarifying for the patients and practitioners the values patients attach to the outcomes. Some decision aids also include explicit valuing exercises 6 , 7 , 9 , 10, 11, –12 whereas others do not. 5 , 8 Some 5 , 6, –7 also include examples of others' values so that patients can learn how values influence decisions and can recognize which value profiles apply to them.
The incremental benefit of including explicit valuing exercises and examples of other patients' values in decision aids is unknown, but it does add to the cost and complexity of administering decision aids. Our study objective was to evaluate the incremental effect of explicit values clarification using a weigh‐scale exercise that included examples of other patients' values, by comparing women's responses to an HRT decision aid in which the exercise was included in one version but not in another. Although in previous studies 7 , 13 we demonstrated that the HRT decision aid that included the exercise had positive effects on awareness of personal values and congruence between values and the patients' choices, we were not able to determine the extent to which the exercise in the decision aid contributed to the overall benefit. Such information would be useful in determining how to streamline the decision aid; values clarification accounts for a quarter of the time to complete the programme.
Theory underpinning decision aids and values clarification
Although the developers of decision aids have different conceptual frameworks of decision support, 7 , 9 , 14 , 15, 16, 17, –18 many have their roots in decision theories from economics or cognitive psychology 19 , 20, 21, –22 that structure decisions according to options, outcomes, and probabilities of outcomes so that individuals are better able to judge the value of the benefits versus the risks. Many frameworks broaden this rather cognitive perspective by including emotional, social, or environmental dimensions. 23 , 24, 25, 26, –27 In those that use explicit valuing approaches, some handle probabilities and values for outcomes separately, asking patients to value each outcome via formal utility assessments 9 , 10 and then combining the values for outcomes with their associated probabilities using expected utility decision analysis to arrive at a recommendation for the patient. Others ask patients to value treatments, by considering both probabilities and values together, using probability trade‐off tasks, 11 , 12 relevance charts, 6 and weigh‐scale exercises. 7 The purpose of these valuing exercises are to structure and provide insight into the deliberation process.
Decision aids have been shown to impact favourably on patients' perceived clarity of values 7 , 13 and the congruence between values and the decision. 7 , 10 , 28 , 29 One of the studies used an implicit valuing approach but also included examples of how others made decisions. 28 The three remaining studies used explicit values clarification techniques such as utility assessments, 10 relevance charts, 14 , 29 and graphic weigh‐scale exercises. 7 Two of the three explicit approaches 6 , 7 also used examples of how others value benefits versus risks.
There are at least three possible mechanisms explaining improvements in perceived values clarity and congruence between values and choices.
The first mechanism, common to all decision aids, was described by Fischhoff et al. 21 who found that individuals are better able to form an opinion about the value of an outcome when it is familiar, simple and directly experienced. The detailed descriptions of outcomes including their physical, emotional and social impact, may translate each outcome into simpler and more familiar terms and may provide vicarious experience from which to better judge the personal value of each benefit and risk and to select an option consistent with personal values.
The second mechanism for decision aids with explicit valuing methods may further increase awareness of personal values. All of the explicit valuing methods involve quantifying a patient's strength of preference for outcomes or treatments. There is an active grappling with the trade‐offs inherent in the decision: the relevance chart and the weigh‐scale exercise ask patients to shade the personal importance of each benefit and risk relative to one another. The utility assessments and trade‐off tasks provide patients with a series of paired choices in which the probability of benefit from the preferred option is systematically varied until patients switch choices. These active exercises may increase one's personal awareness of the importance one attaches to benefits versus risks and the value trade‐offs one needs to make in choosing an option. As a consequence, patients may be more likely to choose an option consistent with the way they value the outcomes.
A third mechanism is possible in decision aids that include examples of how other patients make decisions based on their values. The use of examples may enhance patients' understanding of what values are and how values contribute to the different choices people make. Patients may be better able to recognize the value profiles of others that correspond to their own, and those that do not, and to learn how to select an option consistent with their personal values.
The downstream benefits of clearer values and better value congruence with choices have yet to be established. Patients may be more satisfied with the choice and more likely to persist with the choice. They may also be better at communicating their values to their practitioners and therefore more satisfied with the decision making process and the patient‐practitioner interaction. Possible disadvantages of explicit valuing methods include the increased complexity and potential for confusion, and the increased time and cost of producing and administering the decision aid.
The present study examined the incremental short‐term benefits (over and above outcomes description in familiar simple and experiential terms) of a values clarification exercise using a weigh‐scale exercise that included examples of others' values. This method was chosen because: it was simpler than other methods; could be self‐administered; and had the potential to convey to others, at a glance, anything that was personally important to an individual.
Hypotheses
The hypotheses were that a decision aid with explicit values clarification using a graphic weigh‐scale exercise and examples of others' values would improve perceived clarity of values and improve the congruence between personal values and choices made. In this study we did not evaluate the downstream impact on patient‐practitioner communication, persistence with decisions, or satisfaction with the decision‐making process.
Methods
Design
Following screening for eligibility and written informed consent, we randomized postmenopausal participants to use either: (1) a decision aid with the explicit values clarification exercise using a graphic weigh‐scale and examples of others' values; or (2) a decision aid without the values clarification exercise. Immediately after the participants used the assigned decision aid, they completed a self‐administered questionnaire.
Randomization of participants was handled centrally. Research assistants called the research office with screening information and were issued the participant's identification number and intervention assignment. Participants were blinded to intervention assignment in that they were told we were comparing different methods of decision support, but not the specific differences in the intervention. Research assistants were not blind to the intervention but were provided with strategies for remaining neutral during the participant's self‐review of the intervention and self‐completion of the questionnaire (e.g. refraining from expressing opinions or conveying approval or disapproval in facial expressions; postponing questions until after the completion of data collection). Data analysts were blind to the assignment of the intervention.
The study received approval from the local ethics committee.
Decision aid interventions
Both groups used an HRT decision aid delivered via a self‐administered, self‐paced booklet and audiotape providing information on:
• coronary heart disease (CHD), osteoporosis, endometrial cancer, and breast cancer including definition, incidence, median age of onset, mortality rates, and the social impact of these diseases;
• major risk factors for CHD, osteoporosis and breast cancer;
• disease prevention and early detection strategies;
• HRT regimens, benefits and risks including effects on CHD, osteoporosis, menopausal symptoms, endometrial cancer, breast cancer, side‐effects, contraindications, and other reasons women decide not to take HRT;
• probabilities of disease with and without HRT tailored to the woman's risk of disease and hysterectomy status; 30 and
• prompts to identify her own: probabilities of HRT benefits and risks according to her risk factor profile; preferences for decision participation, and questions.
For the group assigned to the decision aid without explicit values clarification, the last section of the decision aid involved having the audiotape guide them in considering the importance of the benefits and risks by reviewing a summary of the main benefits and risks that had been described previously ( Fig. 1).
Figure 1.
Completion of decision aid without explicit values clarification involved a review of main benefits and risks.
For the group assigned to the decision aid with a values clarification exercise, the last section of the decision aid involved having the audiotape guide them to consider how important the benefits and risks were to them using a weigh‐scale exercise ( Fig. 2).
Figure 2.
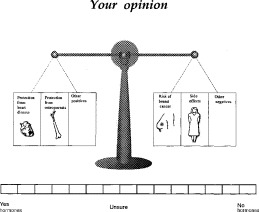
Weigh scale values clarification exercise.
There were three steps in the exercise. Firstly, a woman was provided with an overview of the exercise. Secondly, examples of how other women had completed the weigh‐scale exercise were provided: one who was considering accepting HRT; one who was considering declining HRT; and two who were unsure. This segment re‐enforced the steps of the exercise and helped the women: to understand how values influence decisions; to understand that decisions do vary and that there is no right or wrong answer; and to identify from the sample value profiles which ones corresponded to their own. Thirdly, women were guided in completing their own weigh‐scale exercise which involved: (1) reviewing each benefit and risk box situated in the weigh‐scale; (2) personalizing the boxes labelled `other positives' and `other negatives' by inserting other reasons one would take or not take HRT in addition to those listed; (3) valuing the personal importance of each benefit and risk by shading the boxes in the scale (completely shaded = very important to me; partially shaded = quite or slightly important; no shading = not at all important to me); and (4) indicating her predisposition or `leaning' toward taking HRT using a 15‐point scale situated under the weigh‐scale anchored by `yes HRT' and `no HRT' with `unsure' situated at the midpoint.
Sample
We recruited 201 participants for the trial using convenience sampling. Inclusion criteria were: female; aged 50–69; cessation of menses at least 1 year either surgically or naturally; and ability to read English. Exclusion criteria were: previous HRT use; and absolute contraindications to HRT. We recruited women interested in learning more about HRT via: referrals from health practitioners; posters in clinics and community billboards; newspaper and radio announcements; and personal networking by 12 research assistants. A broad age range was used to accommodate women who might have one of several reasons for being interested in HRT: relief of symptoms such as hot flashes or genitourinary problems, or prevention of disease such as osteoporosis or heart disease. We eliminated those already on HRT, having discovered in a previous study that these women had less uncertainty and more familiarity with the issue and a strong predisposition to continue taking hormones. 7
Evaluation measures
The self‐administered questionnaire was completed by participants immediately after using the decision aid and elicited: perceived clarity of values; personal values for benefits and risks; decisions; decisional conflict; and acceptability of the decision aid.
The three‐item Values Clarity Subscale of the Decisional Conflict Scale was used to measure perceived clarity of personal values. 31 , 32 Participants used a 5‐point Likert scale ranging from strongly agree to strongly disagree to indicate their agreement that they were: (1) clear about the personal importance of the benefits; (2) clear about the personal importance of the risks; and (3) clear which were more important (the benefits or the risks). The subscale is sensitive to change, 7 and discriminates between groups exposed to decision support interventions versus general educational interventions. 13 Scores range from 1 (strongly agree clear re personal values) to 5 (strongly disagree clear re personal values) and those who make (as opposed to delay) decisions usually have mean scores at 2.0 or below.
Personal values or importance ratings of HRT benefits and risks were assessed by having women rate each benefit and risk using a scale anchored by 0 `not at all important to me' and 10 `extremely important to me'. Decisions were assessed by asking what decision they would make about taking HRT with the information they currently had: taking it; not taking it; unsure. Congruence between personal values and choices was determined by examining the degree to which personal values discriminated between the choices women made using discriminant function analysis.
The questionnaire also included the remaining subscales of the Decisional Conflict Scale measuring uncertainty and perceptions of feeling informed, supported, and having made an effective decision. 31 Acceptability of the decision aid was also assessed by asking women to: (1) rate the comprehensibility of each component of the decision aid on a 100 mm visual analogue scale anchored by `poor' and `excellent'; and (2) evaluate the length; pace; amount of information; and balance using structured response categories (e.g. too long; just right; too short; slanted toward HRT; balanced; slanted against HRT).
Analysis plan and sample size
To analyse differences between intervention groups in perceived clarity of values (hypothesis 1), we used the Student t‐test. We also described the differences between the interventions groups according to their choices (accept, decline, unsure) by examining means and 95% confidence intervals of the differences between the means.
Differences between interventions in the congruence between personal values and choices (hypothesis 2) were evaluated using discriminant function analysis (DFA). For each intervention group, we performed a DFA using choice as the dependent variable (accept, decline, unsure) and values as the dependent variable. We then compared the intervention groups using Fishers Exact tests on the percentage of cases correctly classified overall, and for each choice group. We were particularly interested in the value congruence of acceptors because their decisions represents a change in the status quo and, therefore, they are more susceptible to non‐persistence with decisions.
For the remaining outcomes, differences between intervention groups were analysed using t‐tests or chi‐square tests as appropriate. The sample size of 100 participants per arm was selected to detect an absolute difference of 0.25 in the values clarity subscale and an effect size of 0.40 with a significance level of 0.05 and 80% power. The effect size was judged clinically important because effect sizes observed between those who make and delay decisions have ranged between 0.43 and 0.82. 31 , 32
Limitations
The study results are generalizable only to women who have never been on HRT and are interested in the HRT issue; they may be considering the issue for the first time or reconsidering the issue having discussed HRT previously and deciding or being advised not to take it. No baseline assessment of the dependent variables was obtained to avoid exposing the groups to measurement of values prior to the use of the decision aid. Only short‐term effects were assessed post‐intervention; the impact on long‐term persistence and satisfaction with the decision in a population with varying motivations and HRT use patterns cannot be ascertained. In this phase of the evaluation, the intervention was not directly linked to follow‐up with a primary care practitioner. Therefore, the degree to which participants thought they were truly making a decision may have varied and the impact on patient‐practitioner communication was not assessed.
Results
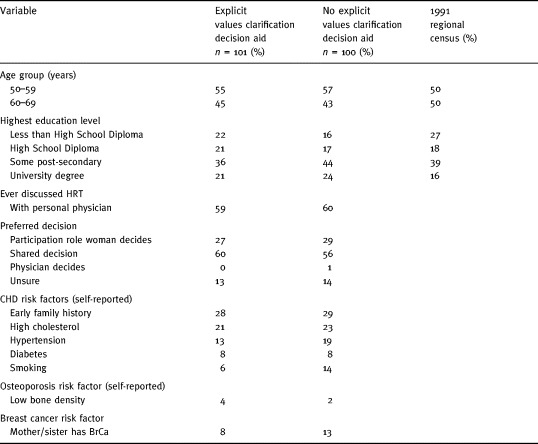
Baseline characteristics of the sample
We recruited 201 participants; 101 were randomly assigned to use the decision with explicit values clarification and 100 used the decision aid with implicit values clarification. The two intervention groups were comparable in their baseline demographic or clinical characteristics (Table 1). The modal respondent was: in the 50–59 age bracket; had some post‐secondary education; had discussed HRT previously with her physician; preferred a shared role in decision making regarding HRT; and had no major risk factors for CHD, osteoporosis or breast cancer.
Table 1.
Baseline demographic and clinical characteristics of the participants
Tests of hypotheses
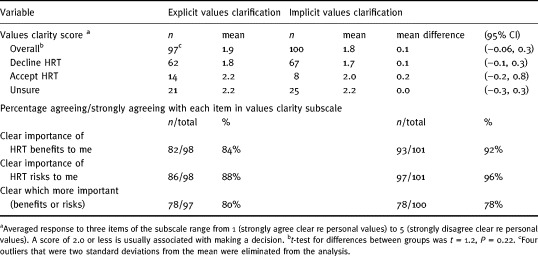
Perceived clarity of values
As shown in Table 2, the primary hypothesis that explicit values clarification using the weigh‐scale exercise and examples' of others values would increase clarity of personal values was not supported. There were no statistically significant differences in perceived clarity of values between intervention groups (t = 1.24, P = 0.22). The percentage agreeing or strongly agreeing they were clear regarding their values was high (>78%) following both interventions.
Table 2.
Post‐intervention differences in perceived clarity of values
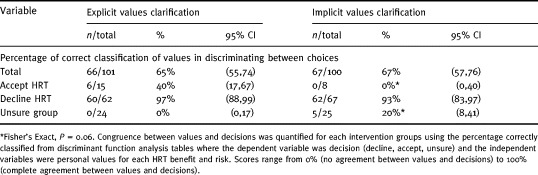
Congruence between personal values and the decision
Following the use of the decision aid, about two thirds declined HRT (62% explicit group; 67% implicit). The next most frequent response was unsure (24% explicit; 25% implicit). The proportion of those accepting HRT when exposed to the explicit weigh‐scale exercise was 15 versus 8% for those exposed to implicit values clarification, but the difference was not statistically significantly different (P = 0.10).
The hypothesis that explicit values clarification using the graphic weigh‐scale would improve the correspondence between personal values and the decision was not supported. As shown in Table 3, there were no significant differences between groups in the discrimination of personal values amongst choices (65 versus 67%). However, in the small group accepting HRT, there was a non‐significant trend toward better discrimination (P = 0.06) in the group exposed to the weigh‐scale exercise (40%) than the group that was not exposed (0%).
Table 3.
Post‐intervention differences in congruence between values and choice
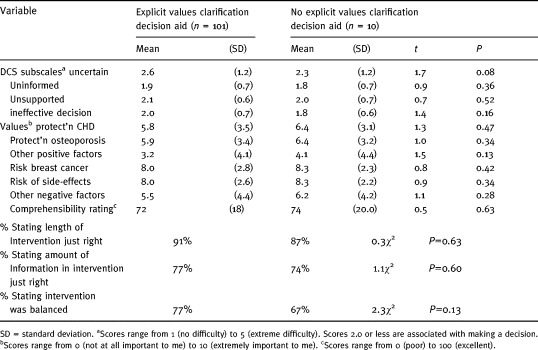
Test of differences in other variables
As shown in Table 4, there were no statistically significant differences in the remaining subscales of the DCS nor in the acceptability of the decision aid.
Table 4.
Post intervention differences in other outcomes
Discussion
For the participants in our study, explicit values clarification using a graphic weigh‐scale exercise and the provision of examples how other women values outcomes was no more beneficial than an implicit approach in promoting clarity of values and congruence between values and choices. This result suggests that the main mechanism explaining the improvements in perceived clarity of values we observed in our previous studies 7 , 13 was likely due to the description of benefits and risks in familiar, simple, experiential terms from which one can better judge their personal value and select an option consistent with personal values. The perceived values clarity scores in this study (1.9, 1.8) were comparable to the group exposed to the HRT decision aid with the graphic weigh‐scale exercise in a previous trial (2.0), 13 but better than baseline scores before administering a decision aid (2.6), 7 or after women used a simple pamphlet (2.3). 13 For most of our current study participants, who were low risk for CHD and osteoporosis, and who had discussed HRT in the past but declined, implicit approaches were enough to make women feel clear about their values and to make a choice consistent with personal values and consistent with their current status quo.
Amongst those considering a change in the status quo by accepting HRT, there was a trend toward a better congruence between values and choices in the group exposed to the weigh‐scale exercise. However, this trend must be interpreted with caution because of the small numbers accepting HRT and the multiple comparisons made. If the result was confirmed in a larger study, it may be important for two reasons. Firstly, non‐persistence with HRT is a problem. Over 20% of women prescribed HRT never fill their prescriptions; 33 suggesting women are not convinced they should be taking it. Moreover, an additional 20% of those who fill prescriptions stop taking them within 9 months. 33 Therefore, it would be important to determine in larger, longitudinal studies whether the improved value congruence with a decision to take HRT can be replicated and whether such an effect leads to better satisfaction and persistence with decisions. Secondly, the decision aid may stimulate some women who had never been on HRT before to consider taking it. Indeed, the proportion of those accepting HRT was nearly doubled in those exposed to the weigh‐scale exercise. It would be important to ensure that any decision support intervention that changes the acceptance of HRT does so in a way that is commensurate with personal values.
The mechanism for promoting increased acceptance and better congruence between values and choice should be studied further with a larger sample. It would be important to ensure that better congruence is not merely due to better statistical precision because of larger numbers accepting HRT when exposed to weigh‐scale compared to implicit approaches. Also, one would need to tease out the separate effects of: the act of considering whether an outcome is personally important or not; the act of quantifying the amount of personal importance; or exposure to different examples of women's values and decisions. An understanding of these separate effects may provide direction for future decision aid development. For example, if it were found that merely considering which benefits and risks were important to them was just as beneficial as quantifying their importance, the values clarification exercise could be simplified. Moreover, it would be interesting to determine if the acceptance of HRT is comparable in those who are exposed to examples of different women making decisions (including acceptance) as in decision aids where this example is not provided.
Our study results highlight the importance of analysing the value of decision‐supporting interventions based on the extent to which the choice represents a change in the status quo. In future studies it would be important to measure baseline predispositions in order to identify the type of intervention from which a person is most likely to benefit. In those who are not predisposed to change, possibly because of polarized values, there may be less need for intensive values clarification once it is clear to them what the benefits and risks are.
Although the results suggest that for the majority of participants, we should be using implicit approaches to values clarification, this recommendation may be premature for four reasons. Firstly, the current sample was likely predisposed toward not taking HRT, given their low risk status and previous discussion regarding HRT. The generalizability of these results needs to be established in situations where predispositions are more variable.
Secondly, it would be important to study decision making that is directly linked to follow‐up discussions with women's practitioners to establish the communication value of the values clarification exercise. Given that 60% preferred a shared decision, and many were unsure about what to do, it is likely that their practitioner's advice would be important in the deliberation process. The weigh‐scale exercise may be useful as a communication tool and may have a positive impact on patient‐practitioner interaction. For example, the practitioner may be better able to `hear' the woman because she is more able in expressing her values; both in words and pictures.
Thirdly, other explicit approaches to values clarification have not been evaluated (e.g. relevance charts, probability trade‐off tasks, utility assessments). These approaches use different strategies and are administered personally.
Finally, the downstream effects on decision persistence and satisfaction with the decision should be examined.
In conclusion, there were no short‐term benefits of explicit values clarification using a graphic weigh‐scale in the majority of participants who were not predisposed to change the status quo; but a benefit for those making a change cannot be ruled out. Further investigations are required to establish the replicability of these effects in groups with varying baseline predispositions and to observe the downstream effects on persistence with decisions and satisfaction with patient‐practitioner communication. Moreover, the efficacy of other values clarification approaches should be examined.
Footnotes
This project was supported by the Medical Research Council of Canada.
References
- 1. American College of Physicians . Guidelines for counselling postmenopausal women about preventive hormone therapy. Annals of Internal Medicine, 1992; 117 (12): 1038 1041. [DOI] [PubMed] [Google Scholar]
- 2. Society of Obstetricians and Gynaecologists of Canada . Canadian Menopause Consensus Conference. Journal of the Society of Obstetricians and Gynaecologists of Canada, 1994; 16: 4 40. [Google Scholar]
- 3. Kassirer JP. Incorporating patients' preferences into medical decisions. New England Journal of Medicine, 1994; 330 (26): 1895 1896. [DOI] [PubMed] [Google Scholar]
- 4. Eddy DM. A Manual for Assessing Health Practices & Designing Practice Policies the Explicit Approach Philadelphia: American College of Physicians, 1992.
- 5. Kasper JF, Mulley AG, Wennberg JE. Developing shared decision making programs to improve the quality of health care. Quality Review Bulletin, 1992; 18 (6): 183 190. [DOI] [PubMed] [Google Scholar]
- 6. Rothert ML, Holmes‐Rovner M, Rovner D et al. An educational intervention as decision support for menopausal women. Research in Nursing and Health, 1997; 20: 377 387. [DOI] [PubMed] [Google Scholar]
- 7. O'Connor AM, Tugwell P, Wells GA et al. A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Education and Counselling, 1998; 33 (3): 267 279. [DOI] [PubMed] [Google Scholar]
- 8. Levine MN, Gafni A, Markham B, MacFarlane D. A bedside decision instrument to elicit a patient's preference concerning adjuvant chemotherapy for breast cancer. Annals of Internal Medicine, 1992; 117 (1): 53 58. [DOI] [PubMed] [Google Scholar]
- 9. Pauker SP & Pauker SG. The amniocentesis decision: Ten years of decision analytic experience. Birth Defects, 1987; 23 (2): 151 169. [PubMed] [Google Scholar]
- 10. Clancy D, Cebul R, Williams S. Guiding individual decisions: a randomized trial of decision analysis. American Journal of Medicine, 1988; 84: 283 288. [DOI] [PubMed] [Google Scholar]
- 11. Llewellyn‐Thomas HA, McGreal MJ, Thiel EC, Fines S, Erlichman C. Patients' willingness to enter clinical trials: measuring the association with perceived benefit and preference for decision participation. Social Science and Medicine, 1991; 32 (1): 35 42. [DOI] [PubMed] [Google Scholar]
- 12. Llewellyn‐Thomas HA. Investigating patients' preferences for different treatment options. Canadian Journal of Nursing Research, 1997; 29 (3): 45 64. [PubMed] [Google Scholar]
- 13. O'Connor A, Tugwell P, Wells G et al. Randomized trial of a portable, self‐administered decision aid for post‐menopausal women considering long‐term preventive hormone therapy. Medical Decision Making, 1998; 18 (3): 295 303. [DOI] [PubMed] [Google Scholar]
- 14. Llewellyn‐Thomas H. Presidential Address. Medical Decision Making, 1995; 15 (2): 101 116. [DOI] [PubMed] [Google Scholar]
- 15. Charles C, Gafni A, Whelan T. Shared decision‐making in the medical encounter: what does it mean? Social Science and Medicine, 1997; 44: 681 692. [DOI] [PubMed] [Google Scholar]
- 16. Mulley A. Outcomes research: implications for policy and practice. In: Smith R, Delamother T (eds) Outcomes in Clinical Practice. London: BMJ Publishing Group, 1995: 13–27.
- 17. Rothert M & Talarcyzk GJ. Patient compliance and the decision making process of clinicians and patients. Journal of Compliance in Health Care, 1987; 2: 55 71. [Google Scholar]
- 18. Entwistle VA, Sheldon TA, Sowden A, Watt IS. Evidence‐informed patient choice. Internal Journal of Technology Assessment in Health Care, 1998; 14: 2 2. [DOI] [PubMed] [Google Scholar]
- 19. Keeney RL & Raiffa H. Decisions with Multiple Objectives: Preferences and Value Trade‐offs. New York: John Wiley and Sons, 1976.
- 20. Feather NT. Expectations and Actions: Expectancy‐Value Models in Psychology Hillsdale, USA: Lawrence Erlbaum Associates Inc., 1982.
- 21. Fischhoff B, Slovic P, Lichtenstein S. Knowing what you want: measuring labile values. In: Wallsten TS, (ed.) Cognitive Processes in Choice and Decision Behavior. Hillsdale, USA: Lawrence Erlbaum Associates Inc., 1980: 117–141.
- 22. Tversky A & Kahneman D. The framing of decisions and the psychology of choice. Science, 1981; 211: 453 458. [DOI] [PubMed] [Google Scholar]
- 23. Janis IL & Mann L. Decision Making New York: The Free Press, 1977.
- 24. Orem DE. Nursing: Concepts of Practice, 5th edn. Toronto: Mosby, 1995.
- 25. Norbeck JS. Social support. Annual Review of Nursing Research, 1988; 6: 85 109. [PubMed] [Google Scholar]
- 26. Ajzen I & Fishbein M. Understanding Attitudes and Predicting Social Behaviour . Englewood Cliffs: Prentice Hall, 1980.
- 27. Bandura A, 1982. Self‐efficacy mechanism in human agency. American Psychologist, 37: 122 147. [Google Scholar]
- 28. Barry MJ, Fowler FJ, Mulley AG, Henderson JV, Wennberg JE. Patient reactions to a program to facilitate patient participation in treatment decisions for benign prostatic hyperplasia. Medical Care, 1995; 33: 771 782. [DOI] [PubMed] [Google Scholar]
- 29. Holmes‐Rovner M, Rovner D, Kroll J, Rothert M, Padonu G, Talarczyk G. Does decision support make people more rational? (Abstract). Medical Decision Making, 1995; 15 (4): 418 418. [Google Scholar]
- 30. Grady D, Rubin SM, Petitti DB et al. Hormone therapy to prevent disease and prolong life in postmenopausal women. Annals of Internal Medicine, 1992; 117 (12): 1016 1037. [DOI] [PubMed] [Google Scholar]
- 31. O'Connor AM. Validation of a Decisional Conflict Scale. Medical Decision Making, 1995; 15 (1): 25 30. [DOI] [PubMed] [Google Scholar]
- 32. Bunn H & O'Connor AM. Validation of client decision making instruments in the context of psychiatry. Canadian Journal of Nursing Research, 1996; 28 (3): 13 27. [PubMed] [Google Scholar]
- 33. Ravnikar VA. Compliance with hormone therapy. American Journal of Obstetrics and Gynaecology, 1987; 156: 1332 1334. [DOI] [PubMed] [Google Scholar]


