Abstract
Objective
To develop and pilot study an information aid for women with a family history of breast cancer.
Design, setting and participants
The information aid, consisting of a booklet and audiotape, was developed by a multi‐disciplinary team of health care professionals, breast cancer survivors and their relatives. Women with no personal history of breast cancer, on the waiting list for a familial breast cancer clinic at either of two centres, who could read English, were eligible for the pilot study which consisted of three sets of mailed questionnaires.
Main outcome measures
The baseline questionnaires included: demographic information: the Breast Cancer and Heredity Knowledge Scale (BCHK); psychological measures (the State‐Trait Anxiety Inventory [STAI], Centre for Epidemiologic Studies Depression Scale [CES‐D] and an item about breast cancer worry), and an item about breast cancer risk perception. Immediately after reviewing the information aid, participants completed a satisfaction survey, the risk perception and cancer worry items and a checklist about their personal family history. The third set of questionnaires, completed 2–4 weeks after reviewing the aid, was identical to the first. Patients then attended their scheduled clinic visit and an objective hereditary breast cancer risk assessment was made by the genetic counselling team.
Results and conclusions
Of 97 eligible women who were contacted, 67 completed all three sets of questionnaires. Overall, women were very satisfied with the aid and 96% would recommend it to other women. There was a highly significant improvement in their knowledge scores after they reviewed the aid. Anxiety and depression did not change and there was a decline in breast cancer worry. Risk perception did not change significantly. Ninety per cent of women completed their personal family history checklist accurately. Several important improvements have been made in the information aid and it will now be evaluated in the community.
Keywords: audiotape, booklet, family history, hereditary breast cancer, information aid, risk assessment
Introduction
Women are exposed to a barrage of news reports and television programmes discussing breast cancer genes, and those with a family history of breast cancer are likely to seek further information. Their primary care physician may be unaware of the current scientific developments relevant to hereditary breast cancer (HBC). Whilst up to 20% of women in the general population have a family history of breast cancer, less than 5% are at high risk of carrying a gene predisposing them to breast cancer. The latter should be offered referral to a specialized familial cancer clinic for genetic assessment and possible testing. The other 15% require education about their breast cancer risk, their present ineligibility for genetic testing, and counselling about screening recommendations. 1 However, many of these women who are at low and moderate risk for HBC may either inappropriately attend familial cancer clinics, resulting in increased anxiety for them and long waiting lists for truly high risk women, or may not receive adequate information. Several studies have shown that low and moderate risk women greatly overestimate their risk of breast cancer, 2 , 3, 4, 5, 6, 7, –8 and that overestimation of risk is a major barrier to compliance with screening. 8 , 9 At the same time, women at high risk for HBC, may not be referred to familial cancer clinics. Moreover, a recent study found that 65% of women referred to a familial cancer clinic felt they had been inadequately prepared and would have appreciated receiving information beforehand. 10 Whilst much effort has recently been devoted to developing educational materials and refining counselling techniques for women who are referred to familial cancer clinics, particularly those who are candidates for genetic testing, there has been much less attention devoted to lower risk women, 2 , 3 , 6 , 8 , 11 , 12 and little, if anything, available in the community.
Accordingly, we sought to develop an information aid for women with a family history of breast cancer, consisting of an audiotape and booklet, which could be used in a variety of settings such as the family doctor’s office or at home. Its purpose would be to enable women to self‐stratify their HBC risk status, to reassure those at low HBC risk and provide them with screening recommendations, and to direct women at higher risk to see their family doctor for further evaluation and discussion. We are currently developing a companion package for use by family physicians to enable them to identify women at moderate HBC risk who may require earlier or more frequent screening, and women at high risk for HBC who should be offered referral to familial cancer clinics.
Before testing the information aid in the community, we elected to perform a pilot study of the aid in a population of women on a waiting list for a familial breast cancer clinic. This setting was selected to ensure that if the aid increased their anxiety, participants would have rapid access to a genetic counsellor. The primary goals of the pilot study were to determine these women’s satisfaction with the aid, and its impact on their knowledge, psychological status and risk perception. A secondary goal of the study was to determine whether these women could correctly self‐identify as being at increased risk for HBC using the criteria specified in the information aid in the form of a personal family history checklist. This paper describes the development and initial evaluation of this information aid.
Methods
Development of the information aid
The content of the information aid was developed through focus groups, literature review and key informants. Four focus groups were conducted: one group of breast cancer survivors, one group of relatives of breast cancer patients, and two groups of women from the general population, aged 23–46 and 45–65. The discussion format was semi‐structured. Many women in the groups had misconceptions about breast cancer or lacked knowledge in specific areas including: risk factors, options for primary and secondary prevention, symptoms, natural history and treatment. Knowledge about genetics and HBC was generally poor. The overall consensus was that the booklet and audiotape should include women’s personal stories and that statistics should be avoided.
After a thorough review of the published literature, key content issues were identified by the multidisciplinary team which included health care professionals (medical oncologist, epidemiologist, surgical oncologist, geneticist, psychologist, family physician, medical ethicist, nurse, sociologist), breast cancer survivors with a positive family history, and a first degree relative of a breast cancer patient. The topics chosen included: breast cancer overview; breast cancer risk factors; HBC; a personal family history checklist; lifestyle and screening recommendations; a glossary of special terms used; list of books and other resources. Three case scenarios of women at low, moderate, and high risk for HBC were presented at the beginning of the booklet and audiotape, and discussed further along to illustrate the more general principles and recommendations.
The personal family history checklist contained four items: a first or second degree relative with breast cancer diagnosed before age 50; two or more first or second degree relatives with breast or ovarian cancer; a first or second degree relative with either bilateral breast cancer or breast and ovarian cancer; and a first or second degree male relative with breast cancer.
Content of the aid was finalized through an iterative process. The booklet was geared to a grade eight reading level 13 and the audiotape edited to just under 30 min in length. The aid was pretested on five women who had undergone HBC counselling and 10 women from the general population for feedback re: wording, content, and layout.
Development of the Breast Cancer and Heredity Knowledge Scale (BCHK)
Since no knowledge scale appropriate for women with a low or moderate risk of HBC could be found in the literature, 14 such a scale had to be developed. Four domains were selected: incidence and risk factors; disease presentation and treatment; screening; and genetics. Using the content of the information aid as well as selected questions from previously validated breast cancer knowledge scales, a draft self‐administered scale of 27 items to be rated on a 5‐point Likert scale was generated. This scale was then tested on a sample of 53 women of varying ages and breast cancer knowledge levels. Thirty‐eight women were retested 2–4 weeks later to confirm reliability. Sixteen items were deleted due to: too many correct responses (11 items), wording difficulties (two items), too many unsure responses (one item), and too high a correlation with other items (two items). The resulting final scale, the Breast Cancer and Heredity Knowledge Scale (BCHK), consisted of 11 items in three domains: incidence and risk factors (three items); screening, disease presentation and treatment (four items); and genetics (four items). Full details of the development of this scale have recently been published. 14
Study design
Women on the waiting list for familial breast cancer clinics at The Toronto Sunnybrook Regional Cancer Centre (TSRCC) and at Women’s College Hospital (WCH), who could read English and had no personal history of breast cancer, were eligible for participation. Letters inviting them to participate in the study were mailed at least 8 weeks before their scheduled clinic appointment together with a consent form and the first set of questionnaires to be completed and returned if they agreed to participate. This set of questionnaires included: demographic information; the BCHK; psychological measures (the Centre for Epidemiologic Studies Depression Scale [CES‐D], 15 the State Trait Anxiety Inventory [STAI], 16 an item about breast cancer worry); and an item about breast cancer risk perception. As soon as these questionnaires were returned with a signed consent form, the information aid was mailed, together with the next set of questionnaires to be completed after listening to the audiotape with the booklet. This second set of questionnaires consisted of the risk perception item, a survey of satisfaction with the aid, the breast cancer worry item, and the personal family history checklist as it appeared in the booklet. The third and final set of questionnaires, completed 2–4 weeks after reviewing the aid, was identical to the first set, but without the demographics.
Study participants proceeded with their clinic appointment as scheduled. Based on the family pedigree recorded by the genetic counsellor, participants were classified as being at low, moderate or high risk for HBC. The personal family history checklist, as completed by the participant, was compared to the pedigree in her chart and scored for correlation.
Assignment of objective risk categories for HBC
After the development of the booklet and audiotape, criteria for categorizing women as being at high, moderate, or low risk for HBC were derived empirically from data in the literature as well as the clinical experience of the authors and their colleagues. High risk was defined as having any of the following: ≥3 relatives on one side of the family with breast cancer <age 70 or ovarian cancer; ≥2 first or second degree relatives on the same side of the family with breast cancer <age 50 or ovarian cancer; or ≥1 first or second degree relative with breast and ovarian cancer. For women who lacked the criteria for high risk, moderate risk was defined as: ≥3 relatives on one side of the family with breast or ovarian cancer; ≥2 first or second degree relatives on one side of the family with breast or ovarian cancer; or one first or second degree relative with either breast cancer before the age 50, bilateral breast cancer, or male breast cancer. Women who lacked any of the criteria for moderate risk were considered to be at low risk for HBC. These criteria were assessed in a retrospective review of 172 consecutive charts of patients referred to the TSRCC familial beast cancer clinic and found to correlate extremely well with the independent risk assessment of the multidisciplinary team.
Assessment of satisfaction
Satisfaction with the information aid was assessed using an 11 item 5‐point Likert questionnaire addressing the format and content of the aid as a package, adapted from Reinders and Singer. 17 Participants were then specifically asked to evaluate the length and amount of detail of the booklet and tape individually. They were also asked whether they would recommend the aid to other women and to provide qualitative comments.
Statistical analysis and sample size calculation
Analysis consisted of initial examination of the data with descriptive statistics. Contingency tables were used to compare proportions across groups. Pre‐ and post‐comparisons for continuous measures were assessed using paired t‐tests.
A minimum sample size of 52 subjects suitable for evaluation was required to detect an effect size of 0.4 on a paired t‐test for the main outcome measures (BCHK, CES‐D, and STAI) for a two‐tailed test with 5% significance and 80% power, and accounting for an intertemporal correlation of 0.60.
Ethics approval
Approval for this study was obtained from the Research Ethics Board at Sunnybrook Health Science Centre, Toronto, Canada.
Results
Patient characteristics
Of 107 eligible women to whom letters of invitation were mailed, eight could not be contacted and 14 refused to participate in the study because they were ‘too busy’ at the time. Six others said they were ‘interested’ but did not enrol. Of the 79 who enrolled in the study, 12 were not suitable for evaluation: eight because they couldn’t complete all three questionnaires prior to their familial clinic appointment; one developed breast cancer before completing the study; one had undergone genetic counselling for ovarian cancer prior to study entry; one could not be contacted; and one questionnaire was lost in the mail. Sixty‐seven participants were suitable for evaluation, 49 from TSRCC and 18 from WCH. All TSRCC patients had been referred to the high risk clinic by either their family doctor (64%), breast surgeon (22%) or another physician, whilst the majority of WCH patients had been referred by a breast surgeon with whom they had ongoing follow‐up. The mean age of the 67 participants was 42 years (range 24–78). All but one spoke English at home and 83% were born in Canada. The majority were employed at the time of the study (77%) and 80% had at least some post‐secondary education.
For the 62 participants who had already undergone genetic assessment and counselling at the time of data analysis, an objective assessment of their HBC risk could be made. According to the criteria, 12% of participants were at low risk, 48% were at moderate risk, and 40% were at high risk.
The mean time between enrolment (receipt of the consent form and first set of questionnaires) and receipt of the final set of questionnaires was 6 weeks (range 2–17 weeks).
Satisfaction (Table 1)
Table 1.
Satisfaction with information aid as a package
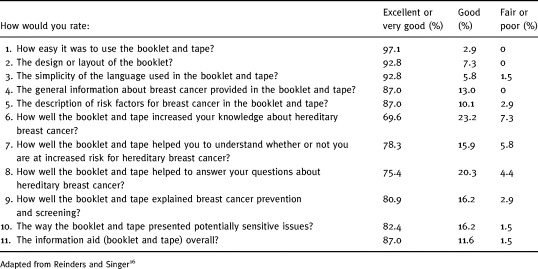
On eight of the 11 items in the questionnaire adapted from Reinders and Singer, the aid was given a rating of ‘excellent’ or ‘very good’ by over 80% of the respondents, and 87% of respondents gave the aid an overall rating of ‘very good’ or ‘excellent’. The highest rating was given for ease of use with 97% giving it a ‘very good’ or ‘excellent’ rating. Although the lowest rating was given to the three items about HBC, 70% of the women considered this portion of the aid to be ‘very good’ or ‘excellent’. In general the same group of women gave low ratings to all three HBC questions. Low satisfaction on these three items was not associated with age, education, knowledge, worry, risk perception, or objective HBC risk.
Although just over one‐third of participants felt the booklet did not have enough detail, 71% of these same women thought the booklet length was just right. Similarly, of the participants who felt the tape had too little detail, 60% thought the tape length was just right and 20% thought the tape was too long. Of the women who were dissatisfied with the HBC section of the aid, 67% thought the booklet lacked detail and 43% thought the tape lacked detail, compared with 25 and 18% of those who were satisfied. More WCH patients than TSRCC patients thought the booklet lacked detail (61 vs. 29%).
Despite these criticisms, 96% of participants said they would recommend the aid to other women. Most of the qualitative comments were very favourable, e.g. ‘eases mind; short and sweet’, ‘up‐to‐date, informative, easily understood, concise’, ‘cuts through the information overload and quickly answers women’s important questions’, ‘describes risks very well, dispels myths (e.g. stress not a known risk factor)’. Some women however, did not feel their needs were met, e.g. ‘good summary; problem personally is I can’t assess my risk from stories or facts’, ‘reassuring but I didn’t get much new information’. Several women mentioned that they became very anxious when they completed the personal family history checklist, and worried that if they ticked off more than one item this put them in a particularly high risk category.
Knowledge (Table 2)
Table 2.
Knowledge (n = 67)

For the BCHK, items correctly answered as ‘agree’ or ‘disagree’ were assigned a score of +1 and those correctly answered as ‘strongly agree’ or ‘strongly disagree’ were assigned a score of +2. Scores of –1 and –2 were assigned to corresponding incorrect responses. A response of ‘unsure’ received a score of 0. Total scores for each domain and for the questionnaire as a whole were expressed as a number with a maximum value of 2.
Knowledge scores increased in all three domains and the mean total score increased from 0.55 (95% C1 0.47–0.63) to 1.16 (95% CI 1.06–1.26) (P < 0.0001). After using the information aid, nine of the 11 items were answered correctly by over 80% of the participants compared with two at baseline.
Although baseline knowledge was significantly higher amongst the women who had a college diploma or at least some university education women (P = 0.04), the improvement in score was the same regardless of education level. Neither baseline knowledge nor change in knowledge score appeared to be associated with age, site (TSRCC vs. WCH), risk perception, objective risk, or satisfaction (as measured by response to the question about how well the aid increased knowledge about hereditary breast cancer).
Psychological measures and risk perception
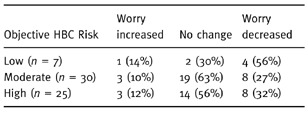
Anxiety and depression as measured by the STAI and CES‐D did not appear to be affected by the aid. The mean STAI score changed from 36.9 ± 10.6 to 36.4 ± 12.0 (P = 0.60) whilst the mean CES‐D score changed from 10.1 ± 8.1 to 10.6 ± 9.6 (P = 0.44). Participants were also asked on the second and third questionnaires how worried they were about developing breast cancer compared with before they used the information aid. These results are summarized in Table 3. Although 19% of the 67 respondents said they were more worried immediately after using the aid, by the time they completed the third questionnaire only 10% were ‘somewhat more worried’, and none were ‘much more worried’. Moreover, 32% of all participants were ‘less worried’ by the end of the third questionnaire. Changes in cancer worry were fairly consistent across the objective HBC risk groups, but it was encouraging to find that four of the seven patients (56%) objectively considered to be at low risk for hereditary breast cancer reported a decrease in breast cancer worry. (Table 4).
Table 3.
Breast cancer worry (n = 67)
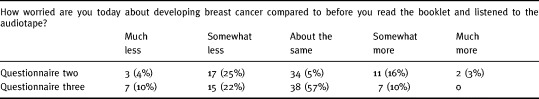
Table 4.
Breast cancer worry in women stratified by objective HBC risk (n = 62)
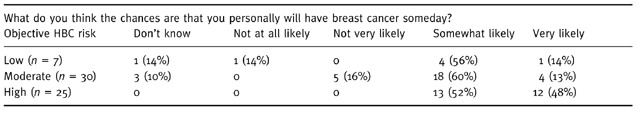
Cancer risk perception was evaluated with the question:
What do you think the chances are that you personally will have breast cancer some day? Is it very likely, somewhat likely, not very likely, or not at all likely?
Risk perception was not substantially affected by exposure to the aid. Only 7% of respondents showed an increase in perceived risk whilst 12% showed a decrease. Participants’ cancer risk perception correlated fairly well with their objective risk. On the third questionnaire, personal risk of getting breast cancer was rated as ‘very likely’ by 48% of those considered to be at high risk for HBC, compared with 13.5% of those considered to be at low or moderate risk. (Table 5).
Table 5.
Breast cancer risk perception in women stratified by HBCrRisk (n = 62)
Accuracy of completion of personal family history checklist
Of the 62 patients for whom pedigree information was available, 56 (90%) correctly identified themselves as being at low risk (no ticks) or moderate/high risk (one or more ticks) for HBC. Only three of 55 (5%) of women, whose pedigrees indicated they should have ticked off at least one item, did not do so and thus misclassified themselves as low risk. Three of seven truly low risk patients ticked off at least one item despite a pedigree suggesting this was inappropriate.
Discussion
An information aid is an educational tool that uses an unbiased approach to present all aspects of an issue in a comprehensive, easily understood format. Information aids assist the health care provider/consumer interaction by providing a focus for communication. The information aid can standardize the information that is communicated, ensure that all relevant items are included, and provide the consumer with a source of information that can be shared with family and friends and can be discussed further after a consultation. The information aid can help to prepare for follow‐up consultations by assisting the consumer in identifying important questions to ask the health care provider. 18 Women with a family history of breast cancer are an ideal target group for such an aid because of the complexity of the information involved, the potential benefits of identifying women at increased risk for cancer, and the potential harms of the misinformation that is prevalent in the community. We chose a self‐administered audiotape and booklet as the format for our information aid because such a format has been successfully used for decision aids for women considering hormone replacement therapy 19 and for women eligible for either lumpectomy or mastectomy for breast cancer. 20
This pilot study of the information aid demonstrated that despite their high level of education, many of these women had significant gaps at baseline in their knowledge of breast cancer in general and HBC in particular. Sixty per cent were not aware of the generally favourable prognosis of breast cancer, 83% thought stress was a proven risk factor, 38% were not aware that incidence increases with age, and 67% were not aware of the significance of changes in one breast. More than half thought testing for gene mutations would tell a woman if she had breast cancer, and that they were at high risk if their mother had breast cancer at age 69, and almost 40% were unaware that men could inherit HBC gene mutations.
There was a highly significant improvement in knowledge across all three domains of BCHK after use of the information aid. Also, the aid was generally very favourably received by the women, did not increase anxiety or depression, and caused an overall decline in their subjective assessment of their worry about breast cancer. The study also showed that the majority of women could correctly self‐identify as being either at low or higher risk for hereditary breast cancer when presented with a standard set of criteria.
We recognize certain limitations of this pilot study including the lack of a control group, the selective study population, the small number of women in each subset, and the short duration of follow‐up.
The results agree with those of several other researchers who showed that whilst an educational intervention may have improved the level of knowledge of women with a family history of breast cancer, it had little impact on their risk perception. 6 , 12 , 21 In three other studies the intervention did decrease perceived risk to a more realistic level, 2 , 3 , 8 but quantitative measures of risk were used which may be more sensitive than the qualitative item used in this study. In all these studies, however, the educational intervention consisted of individual genetic counselling which is expensive and time‐consuming. Our information aid might be a more efficient way to achieve similar results.
The pilot study did suggest several ways in which the information aid could be improved. Once the criteria for objective HBC risk categories were developed and shown to correlate well with clinical practice, it became apparent that the four criteria for higher risk in the personal family history checklist were not adequate and that two further criteria should be added. These are: three or more relatives on the same side of the family had breast or ovarian cancer, and a closely related female relative of Jewish ancestry had breast or ovarian cancer. Also, we were concerned because some women in the pilot study became inappropriately anxious when they ticked off more than one box, assuming this indicated particularly high risk when, in fact, this was not necessarily the case. We have now changed the format of the booklet so that, rather than presenting a checklist to be ticked off, it lists six statements that might apply to one’s family history. The woman is asked to note the relevance of any of these to her family history, which may indicate increased risk for hereditary breast cancer and therefore the need for further assessment by her family doctor. Thus the absolute number of relevant statements is de‐emphasized.
Since one of the key functions of the aid is to allow women at low and higher risk for HBC to self‐identify, we were somewhat concerned about the 10% of women who did not do so correctly, and particularly about the 5% who mis‐classified themselves as being at low risk. We have accordingly clarified the wording of this section.
One potential limitation of our information aid is that it deals with a topic that is being studied intensely and new developments are occurring at a rapid pace. Indeed over the course of the pilot study early results from the Breast Cancer Prevention Trial 22 were released to the public and we felt these had to be incorporated into the next version of the booklet. Although such occurrences are inevitable, the aid deals for the most part with principles which will not quickly become outdated, whilst specific details can be filled in by the family doctor whose information package can be readily updated. Also, an audiotape and booklet can be updated periodically much more easily than a videotape, which was the original format we considered. Although our focus groups indicated that most women were less comfortable with computer software than with an audiotape and booklet, this situation is quickly changing, and our information aid can be easily adapted to an interactive computer format. Such a tool is currently being developed for women who are candidates for HBC genetic testing. 11 Of possible concern is the fact that 30% of women did not feel the aid had taught them enough about HBC, despite the fact that their knowledge scores improved as much as those of the more satisfied women. The dissatisfaction probably relates to the fact that these women already assumed they were at increased risk for HBC by virtue of their familial cancer clinic appointment, and likely expected more specific information about their own personal risk. Also, a disproportionate number of the dissatisfied women were from the WCH site where they had likely already heard much of the information in the aid from their breast surgeon. The aid is intended, however, to be used by the generally lower risk women in the community, most of whom have probably never discussed their risk with a physician. Thus we would hope to expect a higher level of satisfaction from women in the community.
Our next goal is to test the information aid in the community to determine the feasibility of having family physicians distribute it to women in their practices with a family history of breast cancer, and to evaluate the acceptability of the aid and its accompanying physician information package to these women and physicians. The physician information package will include the booklet and audiotape; a transcript of the audiotape; three review articles about HBC to be published this year in Canadian Family Physician; a short review of HBC risk factors with references; and a summary of the criteria for stratifying patients into low, moderate and high risk for HBC, with corresponding management recommendations. The study will also determine whether these women, most of whom are at low or moderate risk for hereditary breast cancer, will be satisfied with the booklet and audiotape and learn as much from them as the higher risk, highly educated women in the pilot study. In addition, the community study will attempt to look at the impact of the aid on outcomes such as quantitative risk perception, attitudes towards screening, and breast cancer worry. The latter will be evaluated both with the item pertaining to subjective assessment of changes which was used in the pilot study, and an objective measure of worry taken before and after use of the information aid. Finally, it will be essential to determine the long‐term impact of the information aid on knowledge, risk perception, breast cancer worry, and compliance with screening recommendations.
Acknowledgements
This study was funded by a grant from the Canadian Breast Cancer Research Initiative. The authors acknowledge the valuable contributions of Ms. Jane Edwards, Ms. Margaret Rao and Ms. S. Anne Parker to the content and design of the information aid. We also wish to thank Ms. Jane Burton for her secretarial assistance.
References
- 1. Hoskins KF, Stopfer JE, Calzone et al. Assessment and counselling for women with a family history of breast cancer: a guide for clinicians. Journal of the American Medical Association, 1995; 273 : 577 585. [PubMed] [Google Scholar]
- 2. Evans DGR, Blair V, Greenhalgh R, Hopwood P, Howell A. The impact of genetic counselling on risk perception in women with a family history of breast cancer. British Journal of Cancer, 1994; 70 : 934 938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alexander NE, Ross J, Summer W, Nease RF, Littenberg B. The effect of an educational intervention on the perceived risk of breast cancer. Journal of General Internal Medicine, 1995; 11 : 92 97. [DOI] [PubMed] [Google Scholar]
- 4. Black WC, Nease RF, Tosteson AN. Perceptions of breast cancer risk and screening effectiveness in women younger than 50 years of age. Journal of the National Cancer Institute, 1995; 87 : 720 731. [DOI] [PubMed] [Google Scholar]
- 5. McCaul KD & O’Donnell SM. Naive beliefs about breast cancer risk. Women’s Health: Research on Gender, Behaviour, and Policy, 1998; 4 : 93 101. [PubMed] [Google Scholar]
- 6. Lerman C, Lustbader E, Rimer B et al. Effects of individualized breast cancer risk counseling: a randomized trial. Journal of the National Cancer Institute, 1995; 87 : 286 292. [DOI] [PubMed] [Google Scholar]
- 7. Smith BL, Gadd MA, Lawler C et al. Perception of breast cancer risk among women in breast centre and primary care settings: Correlation with age and family history of breast cancer. Surgery, 1996; 120 : 297 303. [DOI] [PubMed] [Google Scholar]
- 8. Kash KM, Holland JC, Osborne MP, Miller DG. Psychological counseling strategies for women at risk of breast cancer. Monograph of the National Cancer Institute. 1995; 17 : 73 79. [PubMed] [Google Scholar]
- 9. Polednak AP, Lane DS, Burg MA. Risk perception, family history and use of breast cancer screening tests. Cancer Detection and Prevention, 1991; 15 : 257 263. [PubMed] [Google Scholar]
- 10. Hallowell N, Murton F, Statham H, Green JM, Richards MPM. Woman’s need for information before attending genetic counselling for familial breast or ovarian cancer: a questionnaire, interview, and observational study. British Medical Journal, 1997; 314 : 281 283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Green MJ & Fost N. An interactive computer program for educating and counseling patients about genetic susceptibility to breast cancer. Journal of Cancer Education, 1997; 12 : 204 208. [DOI] [PubMed] [Google Scholar]
- 12. Lerman C, Biesecker B, Benkendorf JL et al. Controlled trial of pre‐test education approaches to enhance informed decision‐making for BRCA1 gene testing. Journal of the National Cancer Institute, 1997; 89 : 148 157. [DOI] [PubMed] [Google Scholar]
- 13. Clariana RB. Using readability formulas to establish the grade level of difficulty of software. Journal of Computing in Childhood Education, 1993; 4 : 155 161. [Google Scholar]
- 14. Ondrusek NK, Warner E, Goel V. Development of a knowledge scale about breast cancer and hereditary (BCHK). Breast Cancer Research and Treatment, in press. [DOI] [PubMed]
- 15. Radloff LS. The CES‐D Scale: a self‐report depression scale for research in the general population. Applied Psychological Measures, 1977; 1 : 385 401. [Google Scholar]
- 16. Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State‐Trait Anxiety Inventory (Self‐Evaluation Questionnaire) Palo Alto: Consulting Psychologists Press, 1970.
- 17. Reinders M & Singer PA. Which advance directives do patients prefer? Journal of General Internal Medicine, 1994; 9 : 49 51. [DOI] [PubMed] [Google Scholar]
- 18. Degner LJ, Martin J, Till J. Communication in cancer: report on the Terry Fox workshop. Canadian Medical Association Journal, 1991; 144 : 1417 1418. [PMC free article] [PubMed] [Google Scholar]
- 19. O’Connor AM, Tugwell P, Wells G et al. Randomized trial of a portable, self‐administered decision aid for post‐menopausal women considering long‐term preventive hormone therapy. Medical Decision Making, 1998; 18 : 249 255. [DOI] [PubMed] [Google Scholar]
- 20. Sawka CA, Goel V, Mahut CA et al. Development of a patient decision aid for choice of surgical treatment for breast cancer. Health Expectations, 1998; 1 : 23 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cull A, Miller H, Porterfield T et al. The use of videotaped information in cancer genetic counselling: a randomized evaluation study. British Journal of Cancer, 1998; 77 : 830 837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fisher B, Constantino JP, Wickerham L et al. Tamoxifen for prevention of breast cancer. Report of the National Surgical Adjuvant Breast and Bowel Project P‐1 Study. Journal of the National Cancer Institute, 1998; 40 : 1371 1388. [DOI] [PubMed] [Google Scholar]


