Abstract
Background
Increased spiritual well-being is related to quality of life (QOL) in patients with heart failure (HF). However, consistent and deliberate integration of spirituality into HF patient care has received limited attention.
Objective
To evaluate the feasibility, acceptability, and preliminary evidence regarding efficacy of a resource-sparing psychospiritual intervention to improve QOL in HF patients.
Methods
Developed and tested a 12-week mail-based intervention addressing spirituality, stress, coping, and adjusting to illness using a mixed-methods, one-group pre-test post-test pilot study design. A convenience sample of patients with HF completed pre- and post-study questionnaires, including Kansas City Cardiomyopathy Questionnaire (KCCQ), Patient Health Questionnaire (PHQ-9), Meaning in Life Questionnaire (MLQ), and Functional Assessment of Chronic Illness Therapy – Spiritual (FACIT-Sp). Research staff conducted semi-structured interviews with program completers. Interviews were coded and analyzed using conventional content analysis.
Results
Participants (N=33; 82% male, mean age 61 years) completed 87% of baseline data collection, an average of 9 intervention modules, and 55% of post-study questionnaires. Participants rated all the modules as at least moderately helpful, and qualitative themes suggested that patients found the intervention acceptable and beneficial. Most participants believed spirituality should continue to be included, though they disagreed on the extent to which religion should remain. Participants that completed the intervention reported evidence suggesting increased QOL (KCCQ effect size (ES) =.53), decreased depressive symptoms (PHQ-9; ES=.62), and less searching for meaning (MLQ; ES=.52).
Conclusions
Results indicate that a module-based program integrating spirituality and psychosocial coping strategies was feasible and acceptable and may improve QOL. This preliminary study suggests that clinicians be open to issues of spirituality as they may relate to QOL in patients with HF. Future research will test a revised intervention.
Keywords: heart failure, spirituality, quality of life, pilot study, telehealth
Heart failure (HF) is a progressive chronic disease causing debilitating physical symptoms, frequent hospitalizations, and high mortality.1 Not surprisingly, many patients with HF experience poor quality of life (QOL). Additionally, an estimated 11–42% of patients with HF meet criteria for depression2 and an estimated 29% experience clinically significant anxiety.3 QOL and depression have been found to independently predict hospitalization and mortality in patients with HF.4–6 Depressed patients with HF are also less likely to engage in self-care,7 an independent risk factor for cardiac events and hospitalizations.8
Multiple interventions have been developed to improve QOL in patients with HF, but interventions focusing on decreasing depressive symptoms and anxiety have largely failed to significantly improve outcomes.2,9,10 Within the QOL interventions designed for patients with HF, one important area of that has been overlooked is spiritual well-being.11 Though spirituality is often associated with religion, a more encompassing definition is “the ways individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature and to the significant or sacred.”12(p887) Both the World Health Organization13,14 and the Clinical Practice Guidelines for Quality Palliative Care15 emphasize the need to integrate psychological and spiritual aspects of well-being into patient care. Nevertheless, healthcare providers remain uncertain regarding how to include spirituality. One tested intervention has addressed the psychological and spiritual well-being of patients with HF.16 This intervention was an 8-week support group for patients with HF that included mindfulness-based stress reduction, coping skills training, and an expressive support group discussion. A presentation of non-denominational spirituality and health was included in one weekly session. The intervention demonstrated significant improvements in depressive symptoms in the treatment group. It differs from the present intervention in three major ways; the present intervention: 1) is much more resource sparing; 2) integrates spirituality throughout each intervention module; and 3) focuses more broadly on stress and coping with illness.
Issues of existential meaning and spirituality may be particularly salient for patients with HF as they confront the burden of living with an incurable, progressive condition. Research indicates that spirituality is very important to many patients with HF,17,18 particularly as HF worsens19 and patients anticipate death.20 Patients with HF may turn to spirituality to cope, and consequently, spiritual well-being represents an important modifiable construct to target for intervention. Recent research among patients with HF suggests that positive aspects of spirituality (e.g., meaning in life, spiritual well-being) are associated with higher QOL11,21,22 and greater survival23 and are negatively associated with emotional distress.24–25 Conversely, religious struggles are associated with more hospitalizations and depressive symptoms and poorer life satisfaction.26 As is true among patients with other chronic illnesses who lack spiritual support (e.g., cancer),13 some patients with HF describe an increased desire to search for meaning within the HF experience.27 Having meaning and purpose is important and is associated with better functioning; however, a non-directive search for meaning may be associated with greater emotional struggle, as perhaps indicated by the often found relationship with depression.28 Thus, helping patients with HF connect with positive aspects of spirituality may improve their overall QOL.
Given the relationship between spirituality and important health outcomes, and the lack of research on psychospiritual interventions among patients with HF, we set out to develop and implement an intervention targeting psychosocial and spiritual factors affecting patients with HF. The intervention was a 12-week, mail-based, patient-centered, and self-guided psychospiritual intervention for patients with HF (Denver Spirited Heart; DSH) created to be low-cost and to require minimal staff time and thus be feasible for broader dissemination. The aims of this study were to assess: 1) feasibility; 2) acceptability; and 3) preliminary evidence regarding intervention efficacy.
Methods
Design
A prospective pretest-posttest pilot study design with quantitative and qualitative methods was used to assess intervention feasibility, acceptability, and obtain preliminary evidence concerning efficacy. All patients provided written informed consent and the Institutional Review Board approved all procedures.
Participants
Prospective participants were prescreened through the electronic medical record system at two HF outpatient clinics: one at a university-based tertiary care hospital (site 1) and another at a Veterans' Affairs (VA) Medical Center (site 2). Patients were also recruited at inpatient wards in the VA hospital. Research staff screened for eligibility during patient visits. Patients were included if they were at least 18 years old, had a HF diagnosis, and were English speaking. Patients were excluded if they lived in an assisted-living facility; had metastatic cancer, dementia or hearing problems; or were deemed ineligible by their medical team.
Procedures
After consenting, participants completed baseline questionnaires. Next they received a binder with the materials for session one. Each week, research assistants mailed that week's materials to participants. Participants were encouraged to place the materials in the study binder so that they would have a complete collection at the end of the study. Additionally, research staff phoned participants weekly to assess whether the intervention materials were received and completed, to answer basic participant questions, and to gather module feedback. These phone calls encouraged completion of the weekly mailers but were not designed to be part of the intervention itself. At 12-weeks, participants completed post-treatment questionnaires and the qualitative interview.
Intervention
The DSH intervention integrated and emphasized psychosocial and spiritual factors that influence self-care and QOL in patients with HF (see Table 1 for topics). Intervention modules were developed by two members of the research team with experience in development and implementation of psychological interventions (SAH and AEH) and were edited and reviewed by two senior clinical psychologists with expertise in psychology, spirituality, and health (KSM and CLP). Topics were chosen based on literature review and clinical expertise to reflect psychosocial issues that are common in patients adjusting to life-threatening chronic illnesses, such as stress and coping, grief/loss, conflict management, and gratitude. In addition to the academic literature, patient-centered resources from the American Heart Association, Heart Failure Society of America, Centers for Disease Control and Prevention, the Heart Failure Association of the European Society of Cardiology, and the American Association of Heart Failure Nurses were also reviewed to ensure that HF-specific topics (e.g., coping with lifestyle changes) were addressed appropriately. Modules were written at a 5th grade reading level. Each weekly mailer contained an integrated spiritual component related to that week's topic and consisted of three sections: (1) educational information, addressing different psychospiritual topics, (2) questions to aid in reflecting on the material, and (3) behavioral activities eliciting practice of the new skills. See Table 2 for intervention examples.
Table 1.
Intervention topics, proportion completed, and participants' mean relevance and helpfulness ratings
| Module Number | Topic | % Complete | Relevance M (SD) | Helpfulness M (SD) |
|---|---|---|---|---|
| 1 | Introduction and Identifying Personal Resources | 79.4 | 2.8 (1.2) | 2.7 (1.3) |
| 2 | Optimism, Self-efficacy, and Control | 79.4 | 3.4 (1.1) | 3.1 (1.2) |
| 3 | Social and Spiritual Support | 84.4 | 3.4 (1.4) | 3.4 (1.2) |
| 4 | Identifying stressors and ways of coping | 83.9 | 3.5 (1.2) | 3.6 (1.2) |
| 5 | Active coping | 80.0 | 3.4 (1.2) | 3.3 (1.3) |
| 6 | Dealing with conflict | 73.3 | 3.6 (1.2) | 3.4 (1.4) |
| 7 | Emotion-focused coping techniques (e.g., deep breathing, meditation) | 65.5 | 3.9 (1.2) | 3.7 (1.4) |
| 8 | Relaxation and mindfulness skill development | 60.7 | 3.6 (1.3) | 3.6 (1.3) |
| 9 | Grief and loss | 66.6 | 4.0 (1.0) | 3.8 (1.5) |
| 10 | Lifestyle changes | 63.0 | 3.3 (1.3) | 3.0 (1.2) |
| 11 | Gratitude | 63.0 | 3.5 (1.2) | 3.4 (1.2) |
| 12 | Summary | 63.0 | 3.7 (1.3) | 3.4 (1.4) |
Note. In addition to the primary topic, spirituality was also included in each module. Relevance and helpfulness scores range from 1 (not at all helpful) to 5 (very helpful).
Table 2.
Intervention component examples
| Week | Education | Reflection & Activity | Spirituality |
|---|---|---|---|
| 1 | Identified resources that help in coping with and managing HF. Included both internal resources (e.g., humor, creativity, caring about health) and external resources (e.g., support from family and friends, a good healthcare team). | Listed resources (internal, external, and spiritual) and identified which resources were most important and which were most frequently used. | Discussed as a potential source of support and comfort, with the module explaining how spirituality can be a source of “strength and inspiration” during difficult times such as coping with an illness. |
| 5 | Introduced the topic of active coping, discussing techniques such as self-education and problem solving as active approaches to coping with stressors related to HF. | Reflect on coping styles in light of a recent stressor and identify the type of coping employed. Practiced skills by identifying ways to use active coping with current stressors, trying out one or two of the identifying uses, and evaluating the outcome. | Explained how spiritual beliefs can impact how individuals choose to cope, and it may be helpful to think of problem solving as “working together with God” or seeing actions as “partnering with God” to overcome obstacles. |
| 10 | Addressed the lifestyle changes often required of HF patients and provided techniques for decreasing dietary salt and increasing physical activity. | Reflected on goals for lifestyle modifications and changes already made. Encouraged to work on fitness goals by picking attainable goals for the week and maintaining an exercise log. Identified spiritual resources to tap when feeling tired or discouraged (e.g. can they read an inspiring religious passage or listen to certain songs). | Discussed as potential motivation for making and maintaining these lifestyle changes. For instance, the module explained how a person might make a better decision about food by “thinking about [the] body as sacred, connected to a higher power.” |
Abbreviation. HF = Heart Failure.
Measures
Baseline Characteristics
Basic demographic information was assessed by self-report. Patient medical history was assessed by electronic medical chart review for date of HF diagnosis, HF etiology, severity of disease (determined by the New York Heart Association [NYHA] class), presence of cardiac device(s), most recent left ventricular ejection fraction, comorbid conditions, and medications.
Acceptability
After completing each module, participants rated the relevance and helpfulness of the module on separate scales from 1 (not at all helpful/relevant) to 5 (very helpful/relevant). At the end of the intervention, participants in DSH completed the 30-minute structured in-person or telephone interview to elicit feedback regarding the individual's overall experience. Examples of interview questions include: (a) What was the most/least helpful part of the program?; (b) What did you think of the spiritual component in each module?; (c) Was participating in this program worth your time?; and (d) Who would benefit most from this type of program?
Preliminary Efficacy
Questionnaires included validated psychosocial measures of key constructs, including heart-failure specific quality of life (Kansas City Cardiomyopathy Questionnaire, KCCQ),29 depressive symptoms (Patient Health Questionnaire-9, PHQ-9),30,31 meaning in life (Meaning in Life Questionnaire, MLQ),32 and spiritual well-being (The Functional Assessment of Chronic Illness Therapy – Spiritual Well-Being, FACIT-Sp).33 The KCCQ was the primary outcome measure, and a 5 point change on KCCQ scale scores, either for a group mean or for an individual, was considered clinically significant.34
Data Analysis
Feasibility
Proportion of subjects approached that were consented and completed baseline and end-of-study questionnaires was used to examine intervention feasibility. Intervention dose was calculated using the number of modules completed per participant. Percentage of modules completed was calculated for each participant and each module and summarized with descriptive statistics.
Acceptability
Module helpfulness and relevance ratings were averaged for each module. Distributions of outcome measures were examined and all were in acceptable ranges. Participant comments from the interview were examined using a conventional content analysis approach35 and an iterative multi-step process.36 With oversight provided by a senior author (KSM), three members of the research staff conducted the analyses. The team consulted with a senior expert in qualitative research to develop a coding scheme and the consultant trained the raters to code the interviews. Two of the raters were research assistants with participant contact (SAH & KR), and one rater was a research assistant without participant contact and limited intervention involvement. In-depth collaborative review of the participants' coded comments was performed to identify important concepts and recurring themes. Steps of the analyses included: 1) initial reading of all interview data; 2) second reading and noting of concepts and themes to develop preliminary codes; 3) coding of five interviews using the preliminary coding system; 4) revising the coding system; 5) coding all interview data; and 6) extraction of themes. To avoid inter-rater contamination, all three raters coded all interviews independently. The results from each step of the analyses were compared and discussed among the three coders. Any coding discrepancies were further discussed with the senior author (KSM) for resolution.
Preliminary Efficacy
Independent samples t-tests were used to compare study completers to non-completers on outcome measures at baseline. We examined mean change from baseline to 12-weeks for study completers to determine trends and strength of effects, along with 95% Confidence Intervals (CI) around the mean change and Cohen's d effect sizes. Traditional cut-points for Cohen's d were used to describe intervention effects.37
Results
Baseline demographic and clinical characteristics of the sample are presented in Table 3.
Table 3.
Baseline Demographic and Clinical Characteristics (N=33)
| Mean ± SD or n (%) | |
|---|---|
| Age, y | 61.6 ± 9.5 |
| Male | 27 (81.8) |
| Ethnicity | |
| Black | 5 (15.2) |
| White | 25 (75.8) |
| Other | 3 (9.0) |
| Married | 18 (58.1) |
| Education | |
| High school or less | 4 (13.0) |
| Some college or college degree | 19 (61.2) |
| Graduate degree | 8 (25.8) |
| NYHA class | |
| I | 6 (18.2) |
| II | 19 (57.6) |
| III | 7 (21.2) |
| IV | 1 (3.0) |
| LVEF % | 35.2 ± 15.6 |
| BMI, kg/m2 | 29.2 ± 7.0 |
| Etiology | |
| CAD/Ischemic | 14 (42.4) |
| Hypertension | 4 (12.1) |
| Valvular | 1 (3.0) |
| Alcohol | 1 (3.0) |
| Idiopathic/Other | 13 (39.4) |
| Device | 24 (72.7) |
| Comorbidity | |
| Myocardial infarction | 8 (24.2) |
| PCI | 4 (12.1) |
| CABG | 7 (21.2) |
| Diabetes | 13 (39.4) |
| Hypertension | 21 (63.6) |
| Renal disease | 10 (30.3) |
| Depression | 10 (30.3) |
Abbreviations: NYHA, New York Heart Association; LVEF, left ventricular ejection fraction; BMI, body mass index; CAD, coronary artery disease; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft.
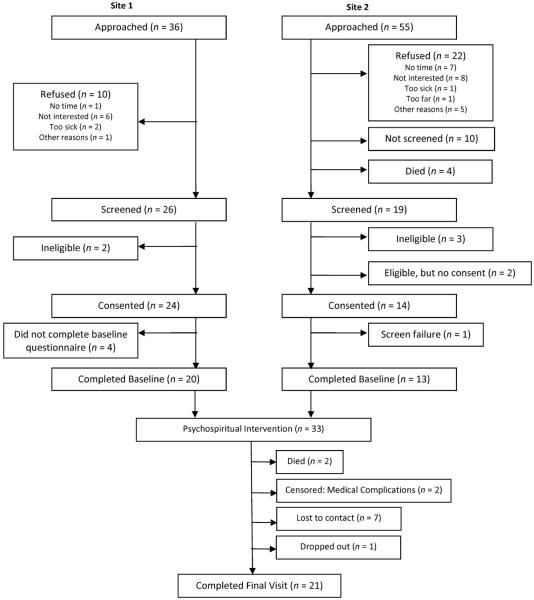
Objective I: Feasibility
Of the 91 patients approached at both sites, 35.2% declined to participate (see CONSORT diagram in Figure 1). Baseline data were obtained from 86.8% (n=33) of those who consented. End of study data were obtained from 63.6% (n=21) of the participants who completed baseline data collection. Those who did not complete the end of study questionnaires died (6.1%), were removed from the study because they became too ill to participate (6.1%), were lost to follow-up (21.2%), or dropped out of the study (3.0%).
Figure 1.
Study Flow Chart
All 12 modules were completed by more than 60% of participants who received them. Module 3 had the highest completion rate (84.4%; Table 1). On average, participants completed a mean of 9.2 out of 12 modules (SD=3.6). Similarly, in their verbal reports, 13 (62%) participants noted that completing 12 modules was likely too many, with seven (33%) participants specifically stating that the program should only include 8–10 modules. Participants' ratings of module helpfulness and relevance are presented in Table 1. Most modules were rated above 3 (out of 5), with only the introduction module receiving average ratings below 3. The modules discussing grief and loss and emotion-focused coping strategies received the highest average relevance (M=4.0) and helpfulness ratings (M=3.8).
Objective II: Acceptability
Twenty-one participants who completed the intervention completed the end-of-study qualitative interview. Qualitative themes and supporting quotes are presented in Table 4.
Table 4.
Qualitative themes and supporting quotes
| Theme | Supporting Quotes |
|---|---|
| Theme 1: Overall Benefit | □ “Absolutely – keeping in mind that there are resources available when you need it, whether internal or external, to help you through.” |
| □ “Got a lot [out of it]. The active coping, dealing with stress, identifying your stressors. Feels so much better when you get rid of [stress].” | |
| □ “The relaxation piece was the most helpful. Taught me new ways to relax-and it worked.” | |
| □ “Active coping… gave you a framework for evaluating your issues to be able to deal with them. I like the proactive aspect about them.” | |
| □ “[The program was] a refresher of things I already knew, but [it was] good to be reminded.” | |
| □ “It definitely changed my QOL. When I look at modules and speak with my wife about it…good for both of us.” | |
|
| |
| Theme 2: Interpersonal Aspects | □ “[The phone call] wasn't like a doctor visit- it was more personal. I looked forward to it. When you're sick, personal contact is important.” |
| □ “[The program] made me realize I'm not just sitting in a hole by myself. It made me feel more connected to others with HF and other people in my life.” | |
|
| |
| Theme 3: Spirituality | □ “I think [spirituality] is what heals you most. Medicine will only get you so far.” |
| □ “I am just an atheist/realist – other people might benefit from it.” | |
| □ “[The spirituality component] was good. Not too in depth. Beliefs were general. Left room for people to think about their own beliefs and what it means for them.” | |
| □ “It was helpful but I wanted it to have more scripture.” | |
| □ “[Including spirituality] should be dependent on the baseline questionnaire. If a person is not at all spiritual, then no. It might offend them. If they are, then yes.” | |
| □ “[Including spirituality should] depend on the person. You should directly ask if being diagnosed with HF has turned you more towards God/spirituality. If yes, then include.” | |
Theme 1: Overall Benefit
Most participants found the intervention beneficial. In response to the question, “Was being in this study worth your time?” 18 (85.7%) said yes. In addition, 17 (81.0%) reported that they benefited by participating in the intervention. Specifically, 12 (57.1%) mentioned that the relaxation and stress reduction pieces were helpful. Seven participants (33.3%) stated that the program served as a refresher for good self-care. Despite learning something from the intervention, 13 (61.9%) participants thought their QOL did not change as a result of participation, primarily because they felt that they had already “coped” with HF. On the other hand, eight participants (38.1%) thought that the intervention improved their QOL. Patients were asked whom they thought would benefit the most from this program, and 14 (66.7%) responded that newly-diagnosed HF patients would.
Theme 2: Interpersonal Aspects
Participants rated the helpfulness of the weekly phone call. Although the phone calls were developed to gather data about the modules and remind patients to complete them, many participants stated that they enjoyed the phone calls. Thirteen (61.9%) patients thought it was nice to be able to talk to someone every week, and seven (33.3%) thought the phone calls held them accountable to complete the intervention modules. The individually based intervention had no group component and face-to-face contact with staff was limited. Nevertheless, it was determined that there was a theme of connection. Four (19.0%) interviewees noted that the intervention provided a sense of connection in general either to other people in their lives, other patients with HF, or the study staff and three additional participants (14.2%) noted they felt connected to the research staff.
Theme 3. Spirituality
Seventeen (81.0%) thought spirituality should be included in a HF intervention. Only one participant (4.7%) thought it should be removed. Participants were asked directly to evaluate the spirituality component. Reactions were mixed. Two (9.5%) thought the spirituality section was the most helpful component, and eight more (38.1%) thought it was helpful. However, seven (33.3%) thought the spirituality component was the least helpful part. Some participants accurately ascertained that we developed a general spiritual intervention aimed at encouraging participants to think about their own spiritual beliefs in relation to living with HF. Conversely, five (23.8%) people thought the spirituality component was too religious (Christian), whereas two (9.5%) felt that the spirituality component was not religious enough. Interestingly, seven (33.3%) suggested it would be important to match patients with an intervention that suits their level of spirituality.
Objective III: Preliminary Evidence Regarding Efficacy
Preliminary evidence regarding intervention efficacy is presented in Table 5. First, there were no significant differences between participants who completed the study and participants who did not complete the study at baseline on any of the outcome measures. Adjectives describing the size of effects are based on the commonly accepted Cohen d classifications. Over the 12 weeks, there was a moderate and clinically meaningful increase in HF-specific quality of life, and a moderate decrease in depressive symptoms. There was also a moderate decrease in searching for meaning, despite no change in presence of meaning. There was a small increase in spiritual well-being.
Table 5.
Preliminary Test of Intervention Effects on Outcome Measures
| Pre (All) (n = 33) | Pre (Completers only) (n = 21) | Difference between completers and non-completers at baseline (t, p) | Post (n = 20) | Change: Post-pre | 95% CI | ES | ES Description | |
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| MIL: Presence* | 26.0 (4) | 25.5 (4) | t = 0.66, p = .51 | 25.5 (3) | 0.0 (4) | −2.2, 2.2 | .00 | No effect |
| MIL: Search* | 21.3 (7) | 21.4 (7) | t = −0.11, p = .91 | 17.5 (8) | −3.9 (8) | −8.4, 0.5 | .52 | Moderate |
| Spiritual well-being | 33.9 (7) | 33.1 (7) | t = 0.86, p = .40 | 34.5 (7) | 1.9 (6) | −0.8, 4.6 | .34 | Small |
| Depressive symptoms | 6.4 (4) | 6.2 (5) | t = 0.25, p = .80 | 4.1 (3) | −1.9 (3) | −3.5, 0.4 | .62 | Moderate |
| HF quality of life** | 71.1 (22) | 73.6 (16) | t = −0.71, p = .49 | 78.7 (15) | 5.1 (10) | 0.6, 9.6 | .53 | Moderate |
Data are presented as mean (SD).
Abbreviations. CI = Confidence Interval. ES = Cohen's d effect sizes. HF=heart failure. MIL = Meaning in Life.
The Meaning in Life Questionnaire was only given to patients at site 1. Therefore, total n = 20.
Scores form the KCCQ
Discussion
This study was designed to examine the feasibility, acceptability, and preliminary evidence regarding efficacy of a resource-sparing psychospiritual intervention to improve QOL for patients with HF. To our knowledge, this is the first fully integrated psychospiritual intervention for patients with HF. Overall, the piloted intervention was feasible and acceptable though it seems the number of modules was too large and should be reduced in the future. Approximately one-third of the patients approached to participate in the spirituality-based intervention agreed to participate, and of those who received the intervention, modules were completed at a high rate. This recruitment rate was similar to, or better than, other non-spiritual interventions (e.g., Gary and colleagues38), suggesting that patients with HF are willing to participate in an intervention that has spirituality as a major component. The intervention was also well accepted by patients. The majority stated that they thought spirituality should be included in a HF intervention. Additionally, on average, all modules were considered at least moderately helpful and relevant. Finally, preliminary evidence regarding efficacy suggests that the intervention was related to modest improvements in HF-specific quality of life, decreased search for meaning in life, and reduced depressive symptoms. Taken together, the results of this study suggest that this relatively low intensity and resource-sparing intervention addressed important needs, but there is clearly room for greater impact.
Despite most patients agreeing that spirituality should be included in a HF intervention, reactions to the spirituality component were mixed. This leaves several possible directions for future intervention development. First, one possibility would be to develop a spiritual intervention void of religious references. Two interventions for cardiovascular disease patients have used similar approaches, integrating techniques such as meditation, mindfulness, visualization, journaling, drawing, nature activities, and nature imagery.39,40 Another possibility would be to focus on meaning, as Breitbart and colleagues41 have done in a group psychotherapy for patients with advanced cancer that is based on the work of Frankl.42 This secular intervention is designed to improve meaning, purpose, and a sense of peace as patients approach the end of life, and it has been shown to improve spiritual well-being and sense of meaning and purpose.41 A third possibility would be to match participants on spirituality and religiousness to a particular form of the intervention, as suggested by some participants. This would call for development of several versions of the intervention guided by experts in various religious and spiritual perspectives. The approach is consistent with conceptualizations of religion and spirituality as culture43,44 but would require extensive effort to create. At this early stage of development, all three approaches should be pursued further.
It is important to note that participants were, by HF standards, rather healthy, with high levels of spiritual well-being at baseline. Nevertheless, on average, participants experienced a clinically significant improvement in their HF-related quality of life after the intervention.34 Moreover, intervention patients experienced a decreased search for meaning in life, a spiritual construct often associated with greater depression and anxiety.28,32 They also experienced decreased depressive symptoms. These findings suggest that the intervention may have encouraged participants to experience greater integrated connection with their own spirituality as previous research reports that better integrated spirituality predicts less search for meaning and greater psychological well-being.45 However, given the small sample size and lack of a control group, these results are preliminary, and the possible mechanism could not be statistically tested in this study. Future research is needed to examine this hypothesis.
Though many participants' reported in the qualitative feedback that their overall QOL did not change, more than half reported believing the intervention would have improved their QOL if they received it in closer proximity to their HF diagnosis. This may be because this group of HF outpatients was not particularly distressed. Evidence suggests that QOL and anxiety improve over the first six months after receiving a HF diagnosis but depressive symptoms do not.46 Future testing and implementation of a spiritual intervention is likely to have greater benefit if applied closer to time of diagnosis and/or in patients with more severe psychological symptoms.
One interesting finding was the interpersonal theme that emerged in the qualitative feedback. Given this intervention was designed to be individual and self-guided, and phone calls were intended only to collect data, this was unexpected. Nonetheless, several participants noted the increased social contact with the research staff and their family members as a beneficial aspect of this intervention. One recent study found that older adults who experienced greater social and spiritual connectedness also experienced greater life satisfaction and hope.47 Thus, improving social and spiritual connectedness may be a target in future HF QOL interventions.
A strength of this study is the consistent and deliberate integration of spirituality into an intervention for patients with HF. Previous research with HF patients indicates that spirituality is important to their lives17,18 and this study showed that although not all participants connected with the spirituality component, they thought it was important to include in the intervention. Second, this study used a mixed-methods approach, which allowed us to compare patients pre- and post-intervention and to gather rich participant feedback on the intervention. Knowledge of both will help improve the intervention.
There are also several limitations to consider. This was a pilot study conducted in one region with a relatively homogenous group of participants. Additionally, the sample was overrepresented by male patients with HF, who have been shown to report more mild-moderate depressive symptoms than female patients with HF, who tend to report more moderate-severe depressive symptoms.48 Given the small sample size and lack of control group, hypothesis tests comparing outcomes over time were limited and between groups testing could not be performed. In addition, missing 12-week data may have affected the results, given that healthier individuals may be more likely to complete the study. Finally, the phone calls added a social component to the intervention which could have influenced QOL. Future steps would be to test a revised intervention in a larger, more diverse sample, with adequate controls, and to make social connection a more explicit intervention component. It is also possible that a sample of patients with HF who admit to having more struggle with adjusting to their illness or who have more advanced illness may demonstrate greater need and benefit from this intervention. Additionally, this study used mail-based delivery of the intervention modules which was acceptable to the patients. However, as older adult cohorts become more comfortable with computer based technology (e.g., internet, smart phone apps), transfer of the modules to delivery via these formats will be indicated.
In summary, a spirituality-based intervention for patients with HF is feasible and acceptable. This psychospiritual intervention could be particularly beneficial for newly diagnosed patients or patients with HF having difficulty adjusting to their chronic illness. Future research should examine the relationships between spiritual connectedness and searching for meaning in relation to QOL in patients with HF. In addition, reducing the length of the intervention and modifying the spiritual components of this intervention to use a more meaning-based or existential approach may be beneficial. Finally, for some patients, supplementary religious components may be important.
Acknowledgements
We want to thank Megan Grigsby for her help with the qualitative analysis. This work was funded by: The US Veterans Administration Healthcare Agency CRICC Pilot Grant to Dr. Bekelman, the University of Colorado Denver Program in Palliative Care Research Pilot Grants Program to Dr. Masters, and the University of Connecticut Center for Health Intervention and Prevention Seed Grant to Dr. Park. This material is based upon work supported in part by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development HSR&D CDA 08-022 to Dr. Bekelman). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: A report from the American Heart Association. Circulation. 2015;131:00–00. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure. A meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Card. 2006;48(6):1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 3.Easton K, Coventry P, Lovell K, Carter LA, Deaton C. Prevalence and measurement of anxiety in samples of patients with heart failure: Meta-analysis. J Cardiovasc Nurs. 2015 doi: 10.1097/JCN.0000000000000265. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faller H, Stork S, Gelbrich G, Schowalter M, Ertl G, Angermann CE. Depressive symptoms in heart failure: Independent prognostic factor or marker of functional status? J Psychsom Res. 2015;78(6):569–572. doi: 10.1016/j.jpsychores.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 5.Suzuki T, Shiga T, Kuwahara K, et al. Impact of clustered depression and anxiety on mortality and rehospitalization in patients with heart failure. J Cardiol. 2014;64(6):456–62. doi: 10.1016/j.jjcc.2014.02.031. [DOI] [PubMed] [Google Scholar]
- 6.Fan H, Yu W, Zhang Q, et al. Depression after heart failure and risk of cardiovascular and all-cause mortality: A meta-analysis. Prev Med. 2014;63:36–42. doi: 10.1016/j.ypmed.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Riegel B, Lee CS, Dickson VV. Self care in patients with chronic heart failure. Nat Rev Cardiol. 2011;8(11):644–654. doi: 10.1038/nrcardio.2011.95. [DOI] [PubMed] [Google Scholar]
- 8.Kato N, Kinugawa K, Nakayama E, et al. Insufficient self-care is an independent risk factor for adverse clinical outcomes in Japanese patients with heart failure. Int Heart J. 2013;54:382–289. doi: 10.1536/ihj.54.382. [DOI] [PubMed] [Google Scholar]
- 9.Rustad JK, Stern TA, Hebert KA, Musselman DL. Diagnosis and treatment of depression in patients with congestive heart failure: A review of the literature. Prim Care Companion CNS Disord. 2013;15(4) doi: 10.4088/PCC.13r01511. PCC.13r01511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whalley B, Rees K, Davies P, et al. Psychological interventions for coronary heart disease. Cochrane Database Syst Rev. 2011;21(8):25–26. doi: 10.1002/14651858.CD002902.pub3. [DOI] [PubMed] [Google Scholar]
- 11.Bekelman DB, Havranek EP, Becker DM, et al. Symptoms, depression, and quality of life in patients with heart failure. J Card Fail. 2007;13(8):643–648. doi: 10.1016/j.cardfail.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Puchalski C, Ferrell B, Virani R, et al. Improving the quality of spiritual care as a dimension of palliative care: the report of the Consensus Conference. J Palliative Med. 2009;12:885–904. doi: 10.1089/jpm.2009.0142. [DOI] [PubMed] [Google Scholar]
- 13.Sulmasy DP. A biopsychosocial-spiritual model for the care of patients at the end of life. Gerontologist. 2002;42:24–33. doi: 10.1093/geront/42.suppl_3.24. [DOI] [PubMed] [Google Scholar]
- 14.WHOQOL Group The WHO quality of life assessment (WHOQOL) position paper from the World Health Organization. Soc Sci Med. 1995;41:1403–1409. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 15.American Academy of Hospice and Palliative Medicine; Center to Advance Palliative Care; Hospice and Palliative Nurses Association; Last Acts Partnership; National Hospice and Palliative Care Organization National Consensus Project for Quality Palliative Care: Clinical Practice Guidelines for quality palliative care, executive summary. J Palliative Med. 2004;7(5):611–27. doi: 10.1089/jpm.2004.7.611. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan MJ, Wood L, Terry J, et al. The Support, Education, and Research in Chronic Heart Failure Study (SEARCH): A mindfulness-based psychoeducational intervention improves depression and clinical symptoms in patients with chronic heart failure. Am Heart J. 2009;157(1):84–90. doi: 10.1016/j.ahj.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 17.Ross L, Austin J. Spiritual needs and spiritual support preferences in patients with end-stage heart failure and their carers: Implications for nurse managers. J Nurs Manag. 2015;23(1):87–95. doi: 10.1111/jonm.12087. [DOI] [PubMed] [Google Scholar]
- 18.Murray SA, Kendall M, Boyd K, Worth A, Benton TF. Exploring the spiritual needs of people dying of lung cancer or heart failure: a prospective qualitative interview study of patients and their carers. Palliative Med. 2004;18(1):39–45. doi: 10.1191/0269216304pm837oa. [DOI] [PubMed] [Google Scholar]
- 19.Murray SA, Kendall M, Grant E, Boyd K, Barclay S, Sheikh A. Patterns of social, psychological, and spiritual decline toward the end of life in lung cancer and heart failure. J Pain Symptom Manag. 2007;34(4):393–402. doi: 10.1016/j.jpainsymman.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 20.Park CL. Estimated longevity and changes in spirituality in the context of advanced congestive heart failure. Palliat Support Care. 2008;6(1):3–11. doi: 10.1017/S1478951508000023. [DOI] [PubMed] [Google Scholar]
- 21.Park CL, Lim H, Newlon M, Suresh DP, Bliss DE. Dimensions of religiousness and spirituality as predictors of well-being in advanced chronic heart failure patients. J Relig Health. 2014;53(2):579–590. doi: 10.1007/s10943-013-9714-1. [DOI] [PubMed] [Google Scholar]
- 22.Park CL, Malone MR, Suresh DP, Bliss D, Rosen RI. Coping, meaning in life, and quality of life in congestive heart failure patients. Qual Life Res. 2008;17:21–26. doi: 10.1007/s11136-007-9279-0. [DOI] [PubMed] [Google Scholar]
- 23.Park CL, Aldwin CM, Choun S, George L, Suresh DP, Bliss D. Spiritual peace predicts 5-year mortality in congestive heart failure patients. Health Psychol. 2015 doi: 10.1037/hea0000271. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Larsen KE, Vickers KS, Sampson S, Netzel P, Hayes SN. Depression in women with heart disease: The importance of social role performance and spirituality. J Clin Psychol Med S. 2006;13(1):39–48. [Google Scholar]
- 25.Salmoirago-Blotcher E, Crawford S, Tran C, Goldberg R, Rosenthal L, Ockene I. Spiritual well-being may buffer psychological distress in patients with implantable cardioverter defibrillators. J Evid Based Complementary Altern Med. 2012;17(3):148–154. doi: 10.1177/2156587212447627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park CL, Wortmann JH, Edmondson D. Religious struggle as a predictor of subsequent mental and physical well-being in advanced heart failure patients. J Behav Med. 2011;34(6):426–436. doi: 10.1007/s10865-011-9315-y. [DOI] [PubMed] [Google Scholar]
- 27.Westlake C, Dracup K. Role of spirituality in adjustment of patients with advanced heart failure. Prog Cardiovasc Nurs. 2001;16(3):119–125. doi: 10.1111/j.0889-7204.2001.00592.x. [DOI] [PubMed] [Google Scholar]
- 28.Steger K, Kashdan TB, Sullivan BA, Lorentz D. Understanding the search for meaning in life: Personality, cognitive style, and the dynamic between seeking and experiencing meaning. J Pers. 2008;76(2):199–228. doi: 10.1111/j.1467-6494.2007.00484.x. [DOI] [PubMed] [Google Scholar]
- 29.Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: A new health status measure for heart failure. J Am Coll Cardiol. 2000;35(5):1245–1255. doi: 10.1016/s0735-1097(00)00531-3. [DOI] [PubMed] [Google Scholar]
- 30.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Löwe B, Unützer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med Care. 2004;42:1194–1201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Steger MF, Frazier P, Oishi S, Kaler M. The Meaning in Life Questionnaire: Assessing the presence of and search for meaning in life. J Counsel Psychol. 2006;53:80–93. [Google Scholar]
- 33.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp) Ann Behav Med. 2002;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 34.Spertus JA, Peterson E, Conard MW, et al. Monitoring clinical changes in patients with heart failure: A comparison of methods. Am Heart J. 2005;150:707–715. doi: 10.1016/j.ahj.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 35.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 36.Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2nd ed. Sage Publications; Thousand Oaks: 2014. [Google Scholar]
- 37.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Earlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- 38.Gary RA, Cress ME, Higgins MK, Smith AL, Dunbar SB. A combined aerobic and resistance exercise program improves physical functional performance in patients with heart failure: A pilot study. J Cardiovasc Nurs. 2012;27(5):418–430. doi: 10.1097/JCN.0b013e31822ad3c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Delaney C, Barrere C, Helming M. The influence of a spirituality-based intervention on quality of life, depression, and anxiety in community-dwelling adults. J Holist Nurs. 2011;29(1):21–32. doi: 10.1177/0898010110378356. [DOI] [PubMed] [Google Scholar]
- 40.Warber SL, Ingerman S, Moura VL, et al. Healing the heart: A randomized pilot study of a spiritual retreat for depression in acute coronary syndrome patients. Explore. 2011;7:222–213. doi: 10.1016/j.explore.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 41.Breitbart W, Rosenfeld B, Gibson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: A pilot randomized controlled trial. Psycho-Oncology. 2010;19:21–28. doi: 10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frankl V. Man's search for meaning. Massachusetts; Beacon Press: 1969. [Google Scholar]
- 43.Cohen AB. Many forms of culture. Am Psychol. 2009;64:194–204. doi: 10.1037/a0015308. [DOI] [PubMed] [Google Scholar]
- 44.Masters KS, Hooker SA. Religiousness/spirituality, cardiovascular disease, and cancer: Cultural integration for health research and intervention. J Consult Clin Psychol. 2013;81:206–216. doi: 10.1037/a0030813. [DOI] [PubMed] [Google Scholar]
- 45.Khumalo IP, Wissing MP, Schutte L. Presence of meaning and search for meaning as mediators between spirituality and psychological well-being in a South African sample. J Psychol Afr. 2014;24(1):61–72. [Google Scholar]
- 46.Mulligan K, Mehta PA, Fteropoulli T, et al. Newly diagnosed heart failure: Change in quality of life, mood, and illness beliefs in the first 6 months after diagnosis. Br J Health Psychol. 2012;17:447–462. doi: 10.1111/j.2044-8287.2011.02047.x. [DOI] [PubMed] [Google Scholar]
- 47.Lee E. The impact of social and spiritual connectedness on the psychological well-being among older Americans. J Relig Spiritual Aging. 2014;26:300–319. [Google Scholar]
- 48.Kao C, Chen T, Cheng S, Lin W, Friedmann E, Thomas SA. Gender differences in the predictors of depression among patients with heart failure. Eur J Cardiovasc Nurs. 2014;13(4):320–328. doi: 10.1177/1474515113496493. [DOI] [PubMed] [Google Scholar]