Abstract
Objectives
This study examined three competing mechanisms in the link between educational attainment and health among young adults: (a) a health behavior mechanism; (b) a psychosocial stressor mechanism; and (c) a health insurance mechanism. The central research question was the pervasiveness and specificity of these mechanisms in the link between low educational attainment and health outcomes during young adulthood.
Study design
A prospective longitudinal study was conducted with 808 men and women followed to age 33 in the United States.
Methods
Health outcomes included major depressive disorder, obesity, chronic health conditions, and self-rated health. The focal predictor was educational attainment at age 21. The roles of the health behavior mechanism (heavy episodic drinking, cigarette smoking, and meeting physical activity guidelines), the psychosocial stressor mechanism (stressful life events, perceived financial stress, and lack of control at work), and having health insurance (either through their employer or union or via family members) in the link between education and varying health outcomes were assessed using path analyses.
Results
Lack of health insurance emerged as a statistically significant explanatory factor underlying the association of education with depression and self-rated health. Health behaviors, specifically smoking and physical activity, were statistically significant intervening factors for obesity and self-rated health.
Conclusions
The processes linking educational attainment to health inequalities begin unfolding during young adulthood. The salience of different mechanisms is specific to a health outcome rather than pervasive across multiple health outcomes. Public health policies with a broad spectrum of components, particularly focusing on smoking, physical activity, and lack of health insurance, are recommended to promote educational equalities in multiple health outcomes among young adults.
Keywords: health inequalities, education, young adults, health behaviors, psychosocial distress, health insurance
Introduction
Disparities according to educational level have been consistently documented1–4 for a wide array of health outcomes, including physical health conditions such as diabetes and heart disease5,6; mental health7,8; and self-rated general health status.9 However, it is unclear why educational attainment is inversely related to health.1,2 Prior studies to date have suggested that at least three behavioral and psychosocial factors should be considered as possible mechanisms: (a) health risk behaviors, such as substance use and low physical activity6,10–13; (b) psychosocial stressors, such as stressful life events, financial distress, and unfavorable work conditions10,14,15; and (c) lack of access,16 particularly to health care.6
Conceptual discussion of the role of these possible factors linking education and health,17 and empirical findings1,10 regarding the magnitude of the role played by these factors, has been inconsistent. Some have contended that such intervening factors might not account for the association between education and health at all, a contention consistent with a “fundamental cause” approach to the link between education and health.17,18 Adding to the confusion, empirical findings regarding each possible factor have been mixed. For example, in a cross-sectional sample of individuals aged 19–95, health risk behaviors, arguably one of the most widely examined mechanisms,12 were found to explain 50% of the association between education and physical impairment.11 Yet in another study, Lundborg19 reported that in a U.S. sample aged 25–74, the associations of education with self-assessed health and number of chronic conditions were virtually unaffected, even after adjusting for a similar list of health risk behaviors. Similarly, health insurance, another possible intervening factor, has been consistently linked to educational attainment20 and varying health outcomes.21 However, findings from studies explicitly examining the role of health insurance in the link between education and health have been inconclusive. In fact, some reports suggested that the role of health insurance might be insubstantial in the link between education and health.10,19 Further clarification of the role of health insurance in disparities in health outcomes is particularly important given its prominence in the current policy debate.
Such mixed findings demand further inquiries in this topic area. First, prior studies have primarily focused on a single domain of health outcome.2 This limits the ability to draw a more definite conclusion about the pervasive versus specific role of different explanatory mechanisms, particularly when varying conclusions arise across studies. The present study examined multiple mechanisms and health measures to reduce the possibility that differential conclusions might arise simply due to differences in study samples or analysis strategies by examining multiple mechanisms and multiple health outcomes in a single sample using a single analysis strategy.
Second, most relevant studies have examined middle-aged or older age groups; relatively few studies have focused on young adults.14 Young adulthood is a critical period for preventive public health efforts,14,22 because (a) the prevalence of important health problems—including physical health problems like obesity and mental health problems like depression—is substantial by the 30s23; (b) health trajectories that portend worsening health problems are established during this developmental period24; and (c) health disparities start widening at this age, including disparities by education.22
Finally, because most studies used cross-sectional data,1 there is a need for prospective longitudinal data that can establish temporal sequencing among involved variables,1,2 which would allay concerns about social selection or drift (i.e., preexisting health problems impair an individual’s ability to achieve higher levels of education).
The present study sought to address these gaps. Specifically, the present study capitalized on a rich trove of information in a contemporary longitudinal sample of young adults and tested the pervasiveness and specificity of the role of health risk behaviors, psychosocial stressors, and access to health insurance as explanatory mechanisms for educational inequalities in depression, obesity, number of chronic health conditions, and self-rated health status. Clarifying mechanisms in the link between education and health can provide concrete and practical intervention targets for public health efforts1,10 involving the target group.
Methods
Sample
Data were from the Seattle Social Development Project (SSDP), a panel study examining an extensive range of behavioral, mental, and physical health outcomes. In September 1985, 18 elementary schools in Seattle, Wash., were identified that overrepresented students from disadvantaged neighborhoods. All fifth-grade students (N = 1,053) in these schools were invited to join the panel study. From this initial sampling pool, 808 students (77%) consented to participate in the SSDP longitudinal study. Fifty-one percent of these participants were male. The sample was ethnically diverse (47% European American, 26% African American, 22% Asian American, and 5% Native American). Fifty-two percent of study participants were eligible for the National School Lunch/School Breakfast program between the ages of 10 and 13. The median household income in the 1990 wave of data collection was estimated to be $25,000. The SSDP sample is more ethnically diverse and economically disadvantaged than the U.S general population. According to the 1990 census,25 about 80% of the U.S. population was European American, about 12% was African American, about 3% was Asian and Pacific Islander, and about 1% was American Indian, Eskimo, and Aleut. According to the same source, the median household income in the 1990 was $29,943 in the United States. SSDP followed these participants from age 10 to 18 in annual increments (except for age 17 due to funding restrictions), and then every 3 years from age 21 to 33 (for more information, see Hawkins et al.26). Analyses presented here used all data from childhood or adolescence (age 10 to 18) and focused on adult data collected at ages 21, 30, and 33. Sample retention rates have been consistently high (92% at age 33).
Measures
Outcomes: mental and physical health status measures (age 33)
Major depression was assessed using the Diagnostic Interview Schedule for DSM-IV27 (1 = meeting the diagnostic threshold in the past year, 0 = otherwise). Obesity was defined as having body mass index (BMI) ≥ 30 (1 = yes, 0 = no). Number of chronic health conditions was a sum measure of 15 self-reported chronic health conditions such as arthritis, glaucoma, and high cholesterol. Self-rated health, a valid and reliable measure of general well-being,28 was assessed by asking: “How would you describe your general health?” (1 = excellent to 4 = poor).
Focal predictor: low educational attainment (age 21)
Participants who did not graduate from high school by age 21 were coded 1 (including those with a GED); all other participants were coded 0. Individuals with a GED have been reported to be more comparable to those without a high school diploma rather than those with a high school diploma with regard to health status.29–31 Accordingly, participants with a GED were grouped with high school dropouts for the analysis. It has been also shown that completion of a degree, rather than an additional year of schooling, is associated with improvement in health,2,32 although this association remains debatable.4 Because the majority of participants at the age 21 survey had not completed a postsecondary degree, and high school completion remains an important marker in an individual’s educational career and has been shown to have long-term impacts on various life outcomes,33–35 educational attainment was operationalized as previously described.
Pathway measures
Health behaviors (at age 30) included: (a) heavy episodic drinking, i.e., the number of times of having five or more drinks in a row during the past month; (b) cigarette smoking, i.e., the number of times of smoking during the past month (ranging from 1 = not at all to 5 = about a pack a day or more); and (c) meeting physical activity guidelines (1 = yes, 0 = no).
Psychosocial stressors included: (a) stressful life events (at age 30), i.e., a count of five stressful life events occurring during the past year, such as getting fired or laid off; (b) perceived financial distress (at age 33), i.e., having serious financial problems during the year prior (1 = yes, 0 = no); and (c) lack of control at work (at age 30), i.e., the average of four items indicating the degree of discretion that a participant had in his or her job.
Being covered by health insurance (at age 33) indicated whether or not a participant had health insurance either through their employer or union or via family members (1 = yes, 0 = no).
Covariates
Analyses were also adjusted for potential confounding factors explaining educational inequalities in health.
Baseline health status during childhood1,2 included symptoms of psychopathology as assessed by the internalizing (e.g., affective disorder and anxiety problems) and externalizing (e.g., conduct problems) scales of the Achenbach Child Behavior Checklist, completed by teachers when participants were aged 10–1436 (not available for later adolescence); being overweight and having physical problems, such as headaches, eye problems, or rashes or other skin problems, also reported by teachers at ages 10–14 as a part of the Achenbach Child Behavior Checklist; and use of alcohol, tobacco, and cannabis measured at ages 13–18 (the earliest age at which all substance use measures were available).
Low socioeconomic status during childhood (SES)26,27 was indicated by ever living in a household in which the household-size-adjusted income was in the lowest 25% of the study sample or having parents with fewer than 12 years of education (1 = yes, 0 = no) during late childhood and adolescence (ages 10–16). Building on the cumulative risk literature,37 participants who were ever in the lowest 25% of household income (adjusted for household size) or lived with parents who had fewer than 12 years of education were coded 1; otherwise they were coded 0.
Achievement scores at age 10 were included as a proxy for an individual’s cognitive ability.38,39 Achievement scores were measured using reading, language, and math subsets of the California Achievement Test, a widely used standardized achievement battery.40
Other sociodemographic factors included participants’ gender (1 = male; 0 = female) and a dichotomous variable indicating race (1 = Caucasian American; 0 = other).
Plan of analysis
We first examined relationships between educational attainment and health outcomes with covariates but without any mechanism factors. We then tested the hypothesized mechanisms in the link between education and health outcomes using path analysis. Path analysis, a type of structural equation modeling, is designed to estimate linear effects of multiple predictors on an outcome of interest and assess intervening mechanisms.41 The main focus of the present study was on the intervening mechanisms between educational attainment and health measures, and a path analysis is well suited to this task.1,2
Reflecting distributional properties of health measures, probit regression was estimated for major depression and obesity. Ordered probit regression was estimated for number of chronic health conditions. Prediction of the self-rated health measure was estimated using linear regression; its skewness (SPSS skew index = .362) and kurtosis (SPSS kurtosis index = .051) were acceptable, based on guidelines in the relevant literature.42 Probit regression coefficients give the change in the z-score or probit index for a 1-unit change in the predictor. As recommended for path models with categorical variables, bootstrap standard errors and confidence intervals were calculated.43 All analyses were performed in Mplus version 7.1. Pathway variables that were not continuous were modeled using probit regression for dichotomous variables and ordered probit regression for ordered variables with more than two levels.
Consistent with recommended guidelines, we considered multiple fit indexes to evaluate whether a model adequately fit the data (CFI ≥ .95,44 RMSEA ≤ .06,44 and WRMR ≤ 1.045). A nonsignificant chi-square value indicates a hypothesized model is an excellent fit to the data; however, large sample sizes often return statistically significant chi-square test results.46 Of the original sample of 808 participants, 87% had available data for the final analysis. Missing data were handled with full information maximum likelihood, a recommended method to handle missingness.47
Results
Educational disparities in health during young adulthood (main effect)
In general, results from models adjusted for covariates (but without mediators) indicated that low educational attainment was significantly associated with higher levels of health problems. Those with low educational attainment had a higher probability of meeting the diagnostic threshold for major depression (b = .68, p < .05), having more chronic health conditions (b = .32, p < .05), and reporting less favorable health status (b = .21, p < .05). Low educational attainment was not, however, associated with obesity (b = .21, p = .21). In general, these findings suggest that health disparities based on educational attainment might be present during young adulthood.
Evaluation of the hypothesized mechanisms
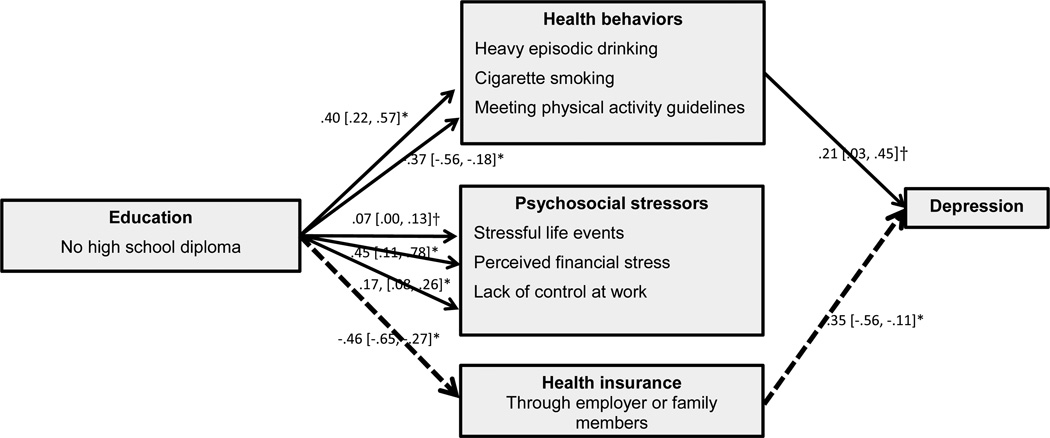
Figure 1 presents unstandardized coefficients from the models testing three competing domains of mechanisms hypothesized to link low educational attainment at age 21 with major depression at age 33. Aside from heavy episodic drinking, low educational attainment was associated with all hypothesized mechanisms. Of these potential mechanisms, indirect tests indicated that only health insurance coverage through an individual’s employer or union or via family members is a statistically significant explanatory factor underlying the link between low educational attainment and major depression at age 33 (b = .16, p < .05). Because the substantive association of low educational attainment at age 21 with the intervening mechanisms was the same across all health measures, it is not discussed with regard to the other three health measures.
Figure 1.
Estimated model of explanatory mechanisms underlying the association of education at age 21 with depression at age 33 (estimate, [bootstrap 95% CI]).
Note. The model fit the data reasonably well: CFI = .93, RMSEA = .04, WRMR = .56, χ2 (21) = 47.09, p = .001). Dashed lines represent statistically indirect effect of education on depression via a hypothesized intervening factor. Paths from covariates to main variables are not presented but are discussed in the text. All paths adjusted for baseline health status during childhood, childhood low SES, and cognitive ability.
*p < .05
†p < .10
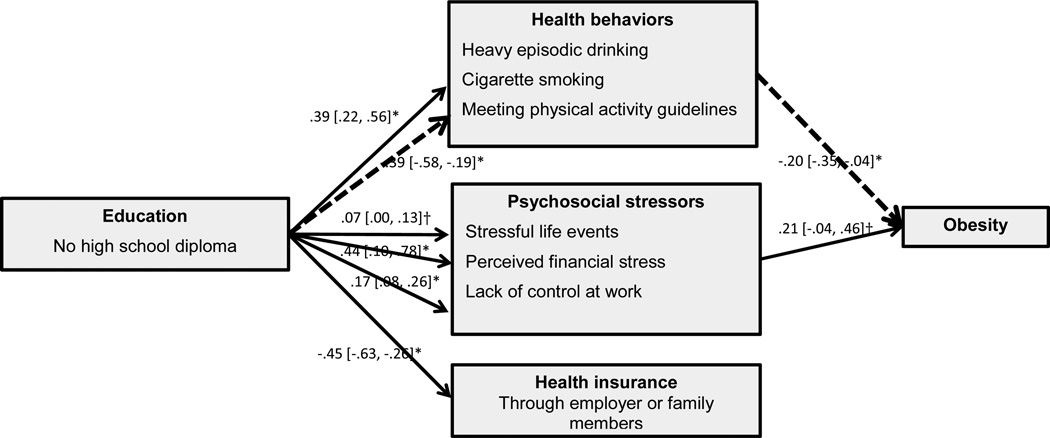
As shown in Figure 2, a different factor emerged as a significant mechanism in the link between low educational attainment at age 21 and BMI at age 33. Indirect tests suggested that low educational attainment affects a young adult’s probability of meeting physical activity guidelines, which in turn affects probability of being obese (b = .08, p < .05). Although not shown, it is noteworthy that teacher reports of participants’ being overweight at ages 10–14 remained a statistically significant predictor of BMI scores at age 33, beyond the hypothesized mechanisms and other covariates (b = .60, p < .05).
Figure 2.
Estimated model of explanatory mechanisms underlying the association of education at age 21 with obesity at age 33 (estimate, [bootstrap 95% CI]).
Note. The model fit the data reasonably well: CFI = .95, RMSEA = .04, WRMR = .58, χ2 (21) = 49.99, p < .001). Dashed lines represent statistically indirect effect of education on depression via a hypothesized intervening factor. Paths from covariates to main variables are not presented but are discussed in the text. All paths adjusted for baseline health status during childhood, childhood low SES, and cognitive ability.
*p < .05
†p < .10
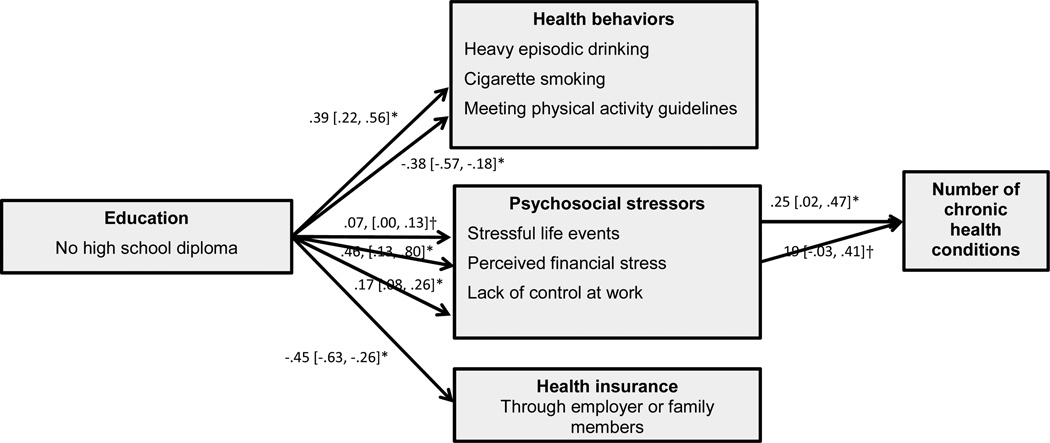
Figure 3 shows results from the path model examining mechanisms linking low educational attainment at age 21 with number of chronic health conditions at age 33. Number of stressful life events and perceived (increased) financial strain were associated with increased number of chronic health conditions, although accompanying indirect tests indicated that these effects cannot be traced back to educational attainment in young adulthood (b = .02, p =.17 and b = .09, p = .15, respectively). Teacher report of students’ being overweight (b = .13, p < .05) and having physical problems (b = .35, p < .05) at ages 10–14 were also predictive of number of chronic health conditions.
Figure 3.
Estimated model of explanatory mechanisms underlying the association of education at age 21 with number of chronic diseases at age 33 (estimate, [bootstrap 95% CI]).
Note. The model fit the data reasonably well: CFI = .93, RMSEA = .04, WRMR = .54, χ2 (21) = 45.37, p = .002). Dashed lines represent statistically indirect effect of education on depression via a hypothesized intervening factor. Paths from covariates to main variables are not presented but are discussed in the text. All paths adjusted for baseline health status during childhood, childhood low SES, and cognitive ability.
*p < .05
†p < .10
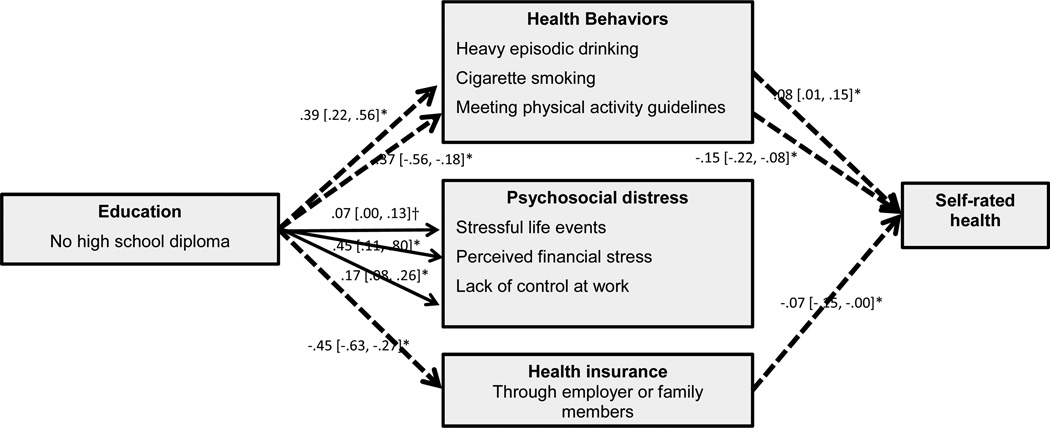
Our final model, shown in Figure 4, concerns the mechanisms linking education and self-rated health status at age 33. Indirect tests showed that low educational attainment at age 21 predicted cigarette smoking (b = .03, p < .05), not meeting physical activity guidelines (b = .06, p < .05), and not having health insurance at the trend level (b = .03, p < .10), which in turn predicted a less favorable self-evaluation of health at age 33. Teacher reports of students’ overweight status at ages 10–14 was associated with less favorable self-evaluation of health at a trend level (b = .06, p < .05).
Figure 4.
Estimated model of explanatory mechanisms underlying the association of education at age 21 with self-rated poor health status at age 33 (estimate, [bootstrap 95% CI]).
Note. The model fit the data reasonably well: CFI = .94, RMSEA = .04, WRMR = .54, χ2 (21) = 44.69, p = .002). Dashed lines represent statistically indirect effect of education on depression via a hypothesized intervening factor. Paths from covariates to main variables are not presented but are discussed in the text. All paths adjusted for baseline health status during childhood, childhood low SES, and cognitive ability.
*p < .05
†p < .10
Of note, when a direct path from low educational attainment at age 21 to each health measure was added, all direct path coefficients were statistically nonsignificant. As such, all the models presented here did not include the direct paths from low educational attainment at age 21 to each health outcome measure.
Discussion
A robust body of literature has consistently documented that low educational attainment is a major contributor to the disparity between being healthy and unhealthy. What warrants further inquiry are the pathways by which lower educational attainment is associated with increased susceptibility to health problems among young adults. Results from this longitudinal study indicate that educational inequalities in health begin unfolding during young adulthood. Regarding our question of the pervasiveness or specificity of the role of hypothesized mechanisms in the link between lower educational attainment and health outcomes, different explanatory mechanisms were evident for different health measures.
Regarding depression, not having a high school diploma was associated with a higher probability of not being insured either through their employer or union or via family members, which in turn was associated with a greater risk of depression at age 33. This finding is in line with a prior study focusing on depression in young adulthood,48 which also suggested that lack of health insurance may be an important explanatory mechanism for increased depression. This finding is also consistent with prior studies reporting a protective effect of health insurance on mental health including depression.49,50 On the other hand, this finding appears to be in contrast to other studies reporting that health insurance is not related to depression.51 This study by Jacobs and colleagues,51 however, focused on women and used different measures to assess depression. The difference in findings may stem from differences in sample characteristics and measures. It is worth noting that as part of the recent implementation of the Patient Protection and Affordable Care Act in the United States, the Mental Health Parity and Addiction Equity Act of 2008 has been substantially expanded.52 It will be important to assess if this recent expansion lessens disparities among young adults given increased access to insurance coverage for behavioral and mental health services. Such information may help clarify mixed evidence regarding the impact of health insurance on mental health.
Psychosocial stressors did not emerge as a statistically significant explanatory factor underlying the link between educational attainment and any health outcome at age 33. One possible explanation is that this intervening factor might be more salient among individuals who hold a relatively advantaged socioeconomic position that is not as well represented in our sample. For example, Krueger and Chang53 reported that the impact of perceived stress on mortality is exacerbated among individuals in the higher SES group relative to low- or middle-SES groups. Examining the extent to which this interplay between psychosocial stress and SES occurs may be a fruitful direction in future studies. It is important to note that these findings do not indicate that psychosocial stressors play no role in shaping young adults’ health. Rather, statistically nonsignificant indirect tests suggested that effects of psychosocial stressors on health outcomes, which were evident for chronic health conditions in our study, cannot be traced back to young adults’ education. As is often discussed in the literature, psychosocial stress can challenge an individual’s biological system, resulting in a range of physical health symptoms.54 Our findings suggest that this process might be observable during young adulthood, although psychosocial stressors do not explain the association between education and health among young adults.
In line with previous studies,6,13,14 health behaviors—particularly cigarette smoking and meeting physical activity guidelines—emerged as statistically significant explanatory factors underlying the association between education and self-perceived health status. However, heavy episodic drinking at age 30 was neither predicted by low educational attainment nor predictive of any health outcomes. It is plausible that the role of heavy episodic drinking in the association between education and health becomes evident later in life, and that harmful drinking during young adulthood, a normative peak age for harmful drinking,55 might not be predictive of later health. Testing the role of drinking behaviors in the link between education and health outcomes at a later point in life may be another fruitful direction for future studies.
Finally, it is noteworthy that a measure assessing teachers’ observations of whether a child is overweight or has other physical problems at ages 10–14 was a statistically significant predictor for obesity and number of chronic health conditions. Consistent with prior studies,56 this finding supports research showing that childhood health conditions have long-lasting effects on health status in young adulthood.
We note three limitations of our study. First, most of the measures were derived from respondent self-reports, with the exception of two teacher-reported measures and obesity. Respondents’ report of their health risk behaviors in particular might be underreported due to social desirability. However, it is noteworthy that cigarette smoking, arguably the most highly stigmatized health behavior,57 showed predictive capacity in the present study, which lends confidence to our findings. Second, our health insurance variable was operationalized to indicate whether an individual was covered either through their employer or union or via a family member. The intent behind this approach was to minimize possible variation across varying health insurance policies. More detailed information about health insurance policies was not available in the SSDP data. Third, it should be acknowledged that the study sample was not nationally representative and generalization of findings should be conducted with caution. These findings should be interpreted in the context of the study sample, which was ethnically diverse and originally from economically challenged backgrounds in Seattle.
The current study made four main contributions to research on the link between education and health outcomes. First, it examined multiple pathways and multiple health outcomes. These analyses were intended to help clarify the pervasiveness or specificity of the role of different mediating factors across varying health outcome measures. Findings can inform efforts to develop effective public health interventions targeting educational disparities in health outcomes. Second, the study findings suggest that different explanatory mechanisms were evident for different health measures. This finding might provide preliminary empirical support for how the fundamental cause approach17,18 might operate in a sample of individuals with more disadvantaged backgrounds. This approach suggests that intervening factors, and certainly a single intervening factor, cannot account for the association between education and health. Because the SSDP sample was originally from high-crime neighborhoods, the SSDP sample represents a group of people who are socioeconomically disadvantaged relative to national samples. Our findings suggest that the fundamental cause might be more evident among those with economically disadvantaged backgrounds. Third, our study contributed to a better understanding of young adulthood, which may hold particular promise for prevention of later health problems that often take a more serious form and require more costly treatment plans.22–24 Fourth, our study capitalized on prospective longitudinal data to better clarify the association between education and later health measures. Specifically, these data can help address the alternative explanation of social selection or drift (i.e., that preexisting health problems impair an individual’s ability to achieve a higher level of education) by (a) specifying a hypothesized temporal order of variables of interest, particularly between education and health outcomes; and (b) adjusting for indicators of health status during childhood.
The current study highlights the need to prevent high school dropout and clarifies the importance of this goal from a public health perspective. Findings also suggest that the salience of different explanatory mechanisms is often specific to a few health outcomes rather than pervasive across many types of health outcomes, which may necessitate a broad spectrum of intervention program components to promote educational equalities in a wide range of health outcomes among young adults. Public health policies with a broad spectrum of components, particularly focusing on smoking, physical activity, and lack of health insurance, are recommended to promote educational equalities in multiple health outcomes among young adults. Finally, findings remind us that there are many public health prevention points during the life course, including childhood and adolescence when an individual’s educational attainment and baseline health status are shaped and young adulthood when health disparities start widening.
Table 1.
Descriptive statistics of the study variables
| Variable (metric or range) | M or % |
|---|---|
| Educational attainment, age 21 | |
| No high school diploma (1 = yes), age 21 | 18.70 |
| Health outcomes | |
| Major depression (1 = yes), age 33 | 10.00 |
| Obesity (1 = yes), age 33 | 34.00 |
| Number of chronic health conditions, age 33 | |
| 0 | 77.10 |
| 1 | 19.00 |
| 2 | 2.70 |
| 3 | 0.70 |
| 4 | 0.10 |
| Self-rated general health, age 33 | 2.05 |
| Mediators | |
| Health behaviors | |
| Heavy episodic drinking, age 30 | 0.58 |
| Cigarette smoking, age 30 | 1.78 |
| Meeting physical activity guidelines, age 30 | 38.30 |
| Psychosocial stressors | |
| Stressful life events, age 30 | 0.32 |
| Perceived financial distress, age 33 | 6.00 |
| Lack of control at work, age 30 | |
| Health insurance covered (1 = yes) | 66.10 |
| Covariates | |
| Baseline symptoms of psychopathology, ages 10–12 | |
| Internalizing problems (z-score), ages 10–12 | 0.01 |
| Externalizing behavior problems (z-score), ages 10–12 | 0.02 |
| Low child and adolescent SES (1 = yes), ages 10–16 | 19.00 |
| Baseline substance use, ages 13–18 | 0.00 |
| Caucasian American (1 = yes) | 47.20 |
| Sex (1 = male) | 51.00 |
Note. SES, socioeconomic status.
Highlights.
The processes of educational health inequalities are already unfolding during young adulthood.
Different explanatory mechanisms were evident for different health measures.
Having a health insurance accounted for the link between education and depression.
Health behaviors explained educational disparities in self-perceived health status.
Psychosocial stressors did not emerge as a statistically significant explanatory factor.
Acknowledgments
Funding: This research was supported by grant 1R01AA016960-03 from the National Institute on Alcohol Abuse and Alcoholism and grants 5R01DA021426-11, 1R01DA033956-01, and 1R01DA024411-05-07 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. The funding agencies played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit this article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing interests: None declared.
Ethical approval: All study procedures were approved by the Human Subjects Review Committee of the University of Washington.
Contributor Information
Jungeun Olivia Lee, Email: lee363@usc.edu.
Rick Kosterman, Email: rickk@uw.edu.
Tiffany M. Jones, Email: MA.
Todd I. Herrenkohl, Email: tih@uw.edu.
Isaac C. Rhew, Email: rhew@uw.edu.
Richard F. Catalano, Email: catalano@uw.edu.
J. David Hawkins, Email: jdh@uw.edu.
References
- 1.Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 2.Kawachi I, Adler NE, Dow WH. Money, schooling, and health: mechanisms and causal evidence. Ann NY Acad Sci. 2010;1186:56–68. doi: 10.1111/j.1749-6632.2009.05340.x. [DOI] [PubMed] [Google Scholar]
- 3.Delva J, O’Malley PA, Johnston LD. Racial/ethnic and socioeconomic status differences in overweight and health-related behaviors among American students: national trends 1986–2003. J Adolesc Health. 2006;39:536–545. doi: 10.1016/j.jadohealth.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Mirowsky J, Ross CE. Education, social status, and health. New York: Aldine De Gruyter; 2003. [Google Scholar]
- 5.Russell LM. Reducing disparities in life expectancy: what factors matter? 2011 Available from: http://www.iom.edu/~/media/Files/Activity%20Files/SelectPops/HealthDisparities/2011-FEB-24/Commissioned%20Paper%20by%20Lesley%20Russell.pdf. [Google Scholar]
- 6.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 7.Lorant V, Croux C, Weich S, Deliege D, Mackenbach J, Ansseau M. Depression and socioeconomic risk factors: 7-year longitudinal population study. Br J Psychiatry. 2007;190:293–298. doi: 10.1192/bjp.bp.105.020040. [DOI] [PubMed] [Google Scholar]
- 8.Lee JO, Herrenkohl TI, Kosterman R, Small CM, Hawkins JD. Educational inequalities in the co-occurrence of mental health and substance use problems, and its adult socioeconomic consequences: a longitudinal study of young adults in a community sample. Public Health. 2013;127:745–753. doi: 10.1016/j.puhe.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schiller JS, Lucas JW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2011. Vital Health Stat. 2012;10:256. [PubMed] [Google Scholar]
- 10.Ettner SL, Grzywacz JG. Socioeconomic status and health among Californians: an examination of multiple pathways. Am J Public Health. 2003;93:441–444. doi: 10.2105/ajph.93.3.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ross CE, Mirowsky J. The interaction of personal and parental education on health. Soc Sci Med. 2011;72:591–599. doi: 10.1016/j.socscimed.2010.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farrell P, Fuchs VR. Schooling and health: the cigarette connection. Cambridge: National Bureau of Economic Research; 1981. [DOI] [PubMed] [Google Scholar]
- 14.Karmakar SD, Breslin FC. The role of educational level and job characteristics on the health of young adults. Soc Sci Med. 2008;66:2011–2022. doi: 10.1016/j.socscimed.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 15.Rainisch BKW, Upchurch DM. Sociodemographic correlates of allostatic load among a national sample of adolescents: findings from the National Health and Nutrition Examination Survey, 1999–2008. J Adolesc Health. 2013;53:506–511. doi: 10.1016/j.jadohealth.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ross CE, Mirowsky J. Does medical insurance contribute to socioeconomic differentials in health? Milbank Q. 2000;78:291–321. doi: 10.1111/1468-0009.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Freese J, Lutfey K. Fundamental causality: challenges of an animating concept for medical sociology. In: Pescosolido BA, Martin JK, McLeod JD, Rogers A, editors. Handbook of the sociology of health, illness, and healing. New York: Springer; 2011. pp. 67–81. [Google Scholar]
- 18.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;35:80–94. [PubMed] [Google Scholar]
- 19.Lundborg P. The health returns to schooling—what can we learn from twins? J Popul Econ. 2008;26:673–701. [Google Scholar]
- 20.Centers for Disease Control and Prevention. CDC health disparities and inequalities report, United States, 2013. MMWR. 2013;62:3. [PubMed] [Google Scholar]
- 21.Freeman JD, Kadiyala S, Bell JF, Martin DP. The causal effect of health insurance on utilization and outcomes in adults: a systematic review of US studies. Med Care. 2008;46:1023–1032. doi: 10.1097/MLR.0b013e318185c913. [DOI] [PubMed] [Google Scholar]
- 22.Pampel FC, Mollborn S, Lawrence EM. Life course transitions in early adulthood and SES disparities in tobacco use. Soc Sci Res. 2014;43:45–59. doi: 10.1016/j.ssresearch.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kubzansky LD, Martin LT, Buka SL. Early manifestations of personality and adult health: a life course perspective. Health Psychol. 2009;28:364–372. doi: 10.1037/a0014428. [DOI] [PubMed] [Google Scholar]
- 24.Hertzman C, Power C. A life course approach to health and human development. In: Heymann J, Hertzman C, Barer ML, Evans RG, editors. Healthier societies: from analysis to action. New York: Oxford University Press; 2006. pp. 83–106. [Google Scholar]
- 25.Bureau of the Census. Census Questionnaire Content, 1990 CQC-4. Washington, DC: U.S. Department of Commerce; 1992. We asked … you told us. race. [Google Scholar]
- 26.Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Effects of social development intervention in childhood fifteen years later. Arch Pediatr Adolesc Med. 2008;162:1133–1141. doi: 10.1001/archpedi.162.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robins L, Helzer JE, Croghan J, Williams JBW, Spitzer RL. NIMH Diagnostic Interview Schedule. Version III. Rockville: National Institute of Mental Health; 1981. [Google Scholar]
- 28.Lima-Costa MF, Cesar CC, Chor D, Proietti FA. Self-rated health compared with objectively measured health status as a tool for mortality risk screening in older adults: 10-year follow-up of the Bambui Cohort Study of Aging. Am J Epidemiol. 2012;175:228–235. doi: 10.1093/aje/kwr290. [DOI] [PubMed] [Google Scholar]
- 29.Liu SY, Chavan NR, Glymour MM. Type of high-school credentials and older age ADL and IADL limitations: is the GED credential equivalent to a diploma? Gerontologist. 2013;53:326–333. doi: 10.1093/geront/gns077. [DOI] [PubMed] [Google Scholar]
- 30.Zajacova A. Health in working-aged Americans: adults with high school equivalency diploma are similar to dropouts, not high school graduates. Am J Public Health. 2012;102:S284–S290. doi: 10.2105/AJPH.2011.300524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zajacova A, Everett BG. The nonequivalent health of high school equivalents. Soc Sci Q. 2014;95:221–238. doi: 10.1111/ssqu.12039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dickson M, Smith S. What determines the return to education: an extra year or a hurdle cleared? Econ Educ Rev. 2011;30:1167–1176. [Google Scholar]
- 33.Kenkel D, Lillard D, Mathios A. The roles of high school completion and GED receipt in smoking and obesity. J Labor Econ. 2006;24:635–660. [Google Scholar]
- 34.Laird J, Lew S, DeBell M, Chapman C. Dropout rates in the United States: 2002 and 2003. NCES 2006-062. Washington, DC: Department of Education; 2006. [Google Scholar]
- 35.Natsuaki MN, Ge XJ, Wenk E. Continuity and changes in the developmental trajectories of criminal career: examining the roles of timing of first arrest and high school graduation. J Youth Adolesc. 2008;37:431–444. [Google Scholar]
- 36.Achenbach TM. CBCL 4–18: YSR and TRF profiles. Burlington: University of Vermont Press; 1991. [Google Scholar]
- 37.Appleyard K, Egeland B, van Dulmen MHM, Sroufe LA. When more is not better: the role of cumulative risk in child behavior outcomes. J Child Psychol Psychiatry. 2005;46:235–245. doi: 10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- 38.Heckman JJ, Stixrud J, Urzua S. The effects of cognitive and noncognitive abilities on labor market outcomes and social behavior. J Labor Econ. 2006;24:411–482. [Google Scholar]
- 39.Farkas G. Cognitive skills and noncognitive traits and behaviors in stratification processes. Annu Rev Sociol. 2003;29:541–562. [Google Scholar]
- 40.Wardrop JL. Review of the California Achievement Tests, Forms E and F. In: Conoley JC, Kramer J, editors. The tenth mental measurement yearbook. Lincoln: University of Nebraska Press; 1989. pp. 128–133. [Google Scholar]
- 41.Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- 42.Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 2011. [Google Scholar]
- 43.Muthén B. Applications of causally defined direct and indirect effects in mediation analysis using SEM in Mplus. 2011 Available from: https://www.statmodel.com/download/causalmediation.pdf. [Google Scholar]
- 44.Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Model. 1999;6:1–55. [Google Scholar]
- 45.Yu CY. Unpublished doctoral dissertation. Los Angeles: University of California, Los Angeles; 2002. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes. [Google Scholar]
- 46.Wang J, Wang X. Structural equation modeling: applications using Mplus. Chichester: Wiley; 2012. [Google Scholar]
- 47.Schlomer GL, Bauman S, Card NA. Best practices for missing data management in counseling psychology. J Couns Psychol. 2010;57:1–10. doi: 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- 48.Zimmerman FJ, Katon W. Socioeconomic status, depression disparities, and financial strain: what lies behind the income-depression relationship? Health Econ. 2005;14:1197–1215. doi: 10.1002/hec.1011. [DOI] [PubMed] [Google Scholar]
- 49.Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, et al. The Oregon experiment — effects of Medicaid on clinical outcomes. New Engl J Med. 2013;368:1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Snowden LR. Health and mental health policies’ role in better understanding and closing African American-White American disparities in treatment access and quality of care. Am Psychol. 2012;67:524–531. doi: 10.1037/a0030054. [DOI] [PubMed] [Google Scholar]
- 51.Jacobs AW, Hill TD, Burdette AM. Health insurance status and symptoms of psychological distress among low-income urban women. Soc Ment Health. 2015;5:1–15. [Google Scholar]
- 52.Mechanic D. Seizing opportunities under the Affordable Care Act for transforming the mental and behavioral health system. Health Aff. 2012;31:376–382. doi: 10.1377/hlthaff.2011.0623. [DOI] [PubMed] [Google Scholar]
- 53.Krueger PM, Chang VW. Being poor and coping with stress: health behaviors and the risk of death. Am J Public Health. 2008;98:889–896. doi: 10.2105/AJPH.2007.114454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Scott KM, Von Korff M, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, et al. Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Arch Gen Psychiatr. 2011;68:838–844. doi: 10.1001/archgenpsychiatry.2011.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bachman JG, O’Malley PM, Schulenberg JE, Johnston LD, Bryant AL, Merline AC. The decline of substance use in young adulthood. Mahwah, NJ: Lawrence Erlbaum; 2002. [Google Scholar]
- 56.Haas S. Trajectories of functional health: the ‘long arm’ of childhood health and socioeconomic factors. Soc Sci Med. 2008;66:849–861. doi: 10.1016/j.socscimed.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 57.Stuber J, Galea S, Link BG. Smoking and the emergence of a stigmatized social status. Soc Sci Med. 2008;67:420–430. doi: 10.1016/j.socscimed.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]