Abstract
Human monocytic ehrlichiosis can manifest as a disease causing multi-organ failure. Rarely, it can cause secondary hemophagocytic lymphohistiocytosis (HLH). Early diagnosis and initiation of treatment for both ehrlichiosis and HLH is lifesaving. Therefore, clinical suspicion of HLH must remain high in the setting of an ehrlichiosis infection.
Keywords: Ehrlichiosis, Hemophagocytic Lymphohistiocytosis
Human monocytic ehrlichiosis1 (HME), caused by Ehrlichia chaffeensis, is an uncommon tick-borne infection endemic to parts of the United States. Although HME typically presents as a mild-moderate illness it can cause severe multi-organ failure, primarily in immunosuppressed individuals (1). Rarely, HME can cause secondary hemophagocytic lymphohistiocytosis2 (HLH). Here, we present a case of an immunocompetent middle-aged woman who developed severe multi-organ failure and meningoencephalitis due to E. chaffeensis infection that was complicated by HLH.
A 41-year-old woman with no significant past medical history was transferred to our institution with 1 week of fevers, malaise, and progressively worsening mental status. Her husband reported a recent camping trip in northern Illinois during which she sustained a tick bite. At the referring hospital, she was found to have distributive shock, acute kidney injury, and encephalopathy. She underwent lumbar puncture showing 144 white blood cells with 71% neutrophils and a negative Gram stain. Broad spectrum antibiotics including doxycycline were started prior to transfer.
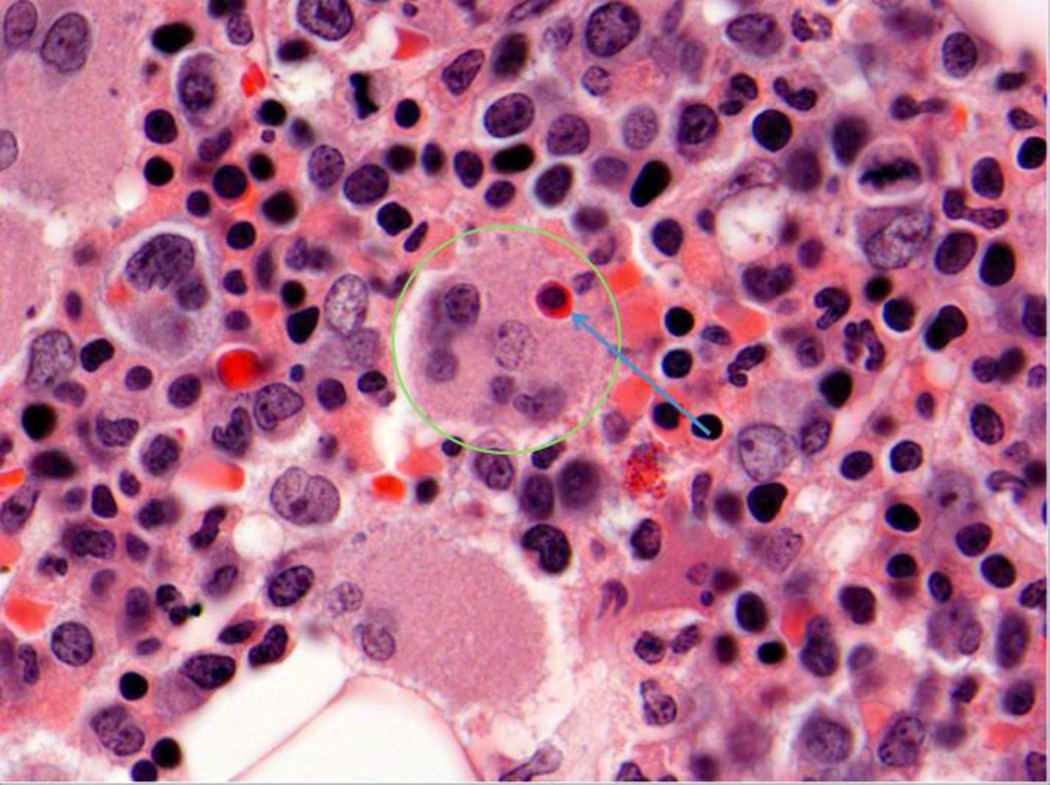
On arrival to our institution, she was spontaneously awake but not responsive. Physical examination revealed petechiae over the eyelids. Notable laboratory findings are summarized in Table 1. Evaluation of a bone marrow aspirate demonstrated a hypercellular bone marrow and increased histiocytes with hemophagocytosis as seen in Figure 1.
Table 1.
Laboratory evaluation
| Laboratory test | Patient’s value on admission |
Patient’s value on day 14 |
Institutional reference range |
|---|---|---|---|
| Hemoglobin | 8.4 g/dL | 7.0 g/dL | 11.6 – 15.4 g/dL |
| Platelet count | 27 k/uL | 131 k/uL | 140 – 390 k/uL |
| White blood cell count | 4.2 k/uL | 8.1 k/uL | 3.5 – 10.5 k/uL |
| White blood cell differential* | 67%N, 19%L, 14%M | Not rechecked | |
| D-dimer | 3465 ng/mL | 1987 ng/mL | 0 – 230 ng/mL |
| Fibrinogen | 156 mg/dL | 371 mg/dL | 200 – 393 mg/dL |
| Lactate dehydrogenase | 3137 unit/L | 440 unit/L | 0 – 271 unit/L |
| Aspartate transaminase | 464 unit/L | 18 unit/L | 0 – 39 unit/L |
| Alanine transaminase | 138 unit/L | 24 unit/L | 0 – 52 unit/L |
| Alkaline phosphatase | 246 unit/L | 139 unit/L | 34 – 104 unit/L |
| Total bilirubin | 3.2 mg/dL | 0.8 mg/dL | 0 – 1.0 mg/dL |
| Prothrombin time | 9.2 s | 11.8 s | 9.2 – 13.0 s |
| Ferritin | 13,257 ng/mL | 577 ng/mL | 11 – 307 ng/mL |
| Triglycerides | 829 mg/dL | Not rechecked | < 100 mg/dL |
| NK Cell (%) | 2 % | Not rechecked | 4–25% |
| NK Cell (abs.) | < 20 cells/uL | Not rechecked | 70–760 cells/uL |
Neutrophils = N, Lymphocytes = L, Monocytes = M
Figure 1.
Section of bone marrow core biopsy demonstrating hemophagocytosis. A histiocyte (green circle), characterized by indistinct nuclear borders and eosinophilic cytoplasm, can be seen englufing an erythoid/RBC precursor (blue arrow).
The patient’s clinical and laboratory findings met 6 of the 8 the criteria (diagnostic) for HLH with fevers > 38.5 °C, peripheral blood cytopenias, hypertriglyceridemia, hemophagocytosis in the bone marrow, elevated ferritin, and decreased NK cell activity. Treatment was initiated with prednisone (1 mg/kg) and intravenous immunoglobulin (IVIG, 500 mg/kg) for 3 days (2). Laboratory markers including ferritin, lactate dehydrogenase, and transaminase levels decreased rapidly with treatment.
During her course, the patient remained severely encephalopathic. EEG demonstrated severe encephalopathy without focal seizures, and MRI of the brain revealed diffuse T2/flair enhancement consistent with encephalitis.
Additional results included serum antibody titers for E. chaffeensis: IgG > 1:1024 and IgM = 1:20. Titers of Rickettsia rickettsii were IgG > 1:1024 and IgM < 1:20. The Rickettsia IgG sent from the referring hospital was similarly elevated at 1:512, suggesting previous exposure to Rickettsia. Cerebrospinal fluid from repeat lumbar puncture returned positive for E. chaffeensis by DNA PCR, confirming the diagnosis of Ehrlichia meningoencephalitis.
The patient completed a 14-day course of doxycycline. Several days after completing the antibiotic course, her encephalopathy resolved. Her course was complicated by severe critical illness myopathy; she was discharged to a rehabilitation facility.
E. chaffeensis is an obligate intracellular bacterium transmitted by the lone star tick Amblyomma americanum. It is endemic to parts of the United States including the southern regions extending north to Illinois and the upper Midwest.
HME can be fatal in immunocompetent patients and manifests as a multisystem disease, with 42% of cases requiring hospitalization and a case-fatality rate of 3% (3). Early diagnosis is essential, as prognosis worsens if treatment with doxycycline is delayed. HME should be considered in patients who report tick exposure. Specific laboratory tests for HME include DNA PCR and acute and convalescent antibody assays. In the largest case series to date published by Otrock et al. in 2015, less than half of their patients had cerebrospinal fluid studies positive for E. chaffeensis (4).
HME is rarely a cause of secondary HLH. Otrock et al. identified 5 cases of adult HLH secondary to E. chaffeensis infection of 76 HLH cases reviewed. In our patient, therapy with prednisone and IVIG for 3 days (2) resulted in rapid improvement in inflammatory markers. Treatment of HLH in addition to doxycycline therapy proved lifesaving in this case.
Acknowledgments
Disclosures:
Dr. Singer receives grant support from the National Heart, Lung, and Blood Institute of the National Institutes of Health under K08 HL128867 and the Parker B. Francis Research Opportunity Award.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Human monocytic ehrlichiosis (HME)
Hemophagocytic lymphohistiocytosis (HLH)
References
- 1.Yachoui R. Multiorgan failure related to human monocytic ehrlichiosis. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2013-008716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.La Rosee P. Treatment of hemophagocytic lymphohistiocytosis in adults. Hematology Am Soc Hematol Educ Program. 2015;2015:190–196. doi: 10.1182/asheducation-2015.1.190. [DOI] [PubMed] [Google Scholar]
- 3.Ismail N, Bloch KC, McBride JW. Human ehrlichiosis and anaplasmosis. Clin Lab Med. 2010;30(1):261–292. doi: 10.1016/j.cll.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Otrock ZK, Gonzalez MD, Eby CS. Ehrlichia-Induced Hemophagocytic Lymphohistiocytosis: A Case Series and Review of Literature. Blood Cells Mol Dis. 2015;55(3):191–193. doi: 10.1016/j.bcmd.2015.06.009. [DOI] [PubMed] [Google Scholar]