Abstract
Background:
Cardiac rehabilitation (CR) programmes have been shown to improve patient outcomes, but vary widely in their components. The impact of Singapore’s CR programme on clinical outcomes is currently not known.
Objective:
To evaluate the effects of a community-based CR programme on important clinical parameters in patients with cardiovascular disease in Singapore.
Method:
A retrospective cohort study was conducted. Cardiovascular patients who had completed a hospital-based CR programme were included. Patients who continued with community-based CR (n = 94) during the period of 2009-2013 were compared with patients who received regular care (n = 157). Changes in clinical and physical examination parameters between baseline and one-year post follow-up were analyzed. Within-group differences were compared using the paired t-test, while multivariate linear regression was used to compare the changes in the various parameters between the intervention and control groups. The primary outcome measure was low density lipoprotein (LDL) levels.
Results:
Patients in the intervention group had significant lowering of LDL (2.5 to 2.2 mmol/L, p<0.01), while the control group’s LDL increased (2.2 to 2.4 mmol/L, p<0.01). The intervention group had greater improvements in LDL (-0.3 vs. +0.2 mmol/L, p<0.01), triglycerides (-0.1 vs. +0.1 mmol/L, p=0.01), total cholesterol (-0.3 vs. +0.3 mmol/L, p<0.01), fasting blood glucose (-0.5 vs. +0.3 mmol/L, p<0.01), systolic blood pressure (-3.2 vs. +5 mmHg, p<0.01) and diastolic blood pressure (-2.6 vs. +2.8 mmHg, p<0.01).
Conclusion:
The community-based CR programme in Singapore is associated with improvements in several cardiovascular clinical parameters and may be of benefit to cardiovascular patients.
Keywords: Community, Cardiovascular Disease, Cardiac Rehabilitation, Clinical Outcomes, Low density lipoprotein
Introduction
Cardiovascular disease (CVD) is the leading cause of death globally1. Half of the global burden of CVD is predicted to occur in the Asia-Pacific region, and this is likely to increase as a result of increasing prevalence of obesity and other risk factors2. Given the high prevalence of CVD and its associated morbidity and mortality, it is important that people with CVD, or who are at high cardiovascular risk, are detected early and managed appropriately.
One such intervention is cardiac rehabilitation (CR). CR refers to coordinated, multifaceted interventions designed to optimize a cardiac patient’s physical, psychological, and social functioning, in addition to stabilizing, slowing, or even reversing the progression of the underlying atherosclerotic processes, thereby reducing morbidity and mortality3. As such, CR provides an important avenue through which to deliver effective preventive care. The benefits of CR have been reviewed extensively in the literature in the Western countries, such as the United States. CR is associated with a reduction in mortality, hospital admissions and quality of life4, 5. Numerous other studies have demonstrated improvements in clinical parameters such as blood pressure (BP), total cholesterol (TC), low-density lipoprotein cholesterol (LDL) and triglycerides (TG)5-7.
CR programmes are traditionally located in the hospital setting, but alternative models such as community-based programmes, have been found to be similarly effective, and may have additional advantages such as lower costs and better compliance6-8. However, different CR programmes vary widely in the type and intensity of components involved, and are also influenced by additional differences between countries such as in economy, culture and standards of medical practice9.
Singapore also has her own unique drivers of CVD, such as her rapidly ageing population, the population’s lack of exercise and physical inactivity, as well as a multi-ethnic society which in turn affects CVD risk, due to possible differences in metabolic traits, such as insulin resistance10.To the best of our knowledge, studies evaluating the impact of CR programmes in Asia are currently lacking. Our study therefore aims to provide local supporting evidence for community-based CR by assessing participation in a community-based CR programme and its association with LDL and other clinical parameters in patients with CVD in Singapore.
Methods
A retrospective cohort study was conducted at the National Heart Centre, Singapore (NHCS), a national and regional referral centre for cardiovascular medicine, and the Singapore Heart Foundation (SHF). The SHF is a non-profit charitable organization that aims to promote heart health in Singapore, thereby preventing and reducing disability and death due to cardiovascular diseases and stroke, and is the only institution that provides a structured community-based CR programme in Singapore.
Study Subjects
Patients above the age of 21 who had previously been diagnosed with CVD were eligible for the study. Patients who were enrolled in the community-based CR programme at SHF from 2009 to 2013 were included in the intervention group. Patients were excluded if they did not complete one year of the programme due to withdrawal or loss to followup, or if they had previously participated in the programme for primary prevention. The control group comprised of NHCS patients who were not referred to the communitybased CR programme. All patients underwent phase two of CR. Regardless of participation in the programme, all patients continued to receive regular medical follow-up in the hospitals.
Ethical Issues
The study protocol was reviewed and approved by the institutional review boards of the National University of Singapore and NHCS, with a waiver for individual informed consent.
Cardiac Rehabilitation Interventions
The community-based CR programme at SHF is similar to hospital based CR in the local setting. The aim of community-based CR is the long term maintenance of structured, individualized exercise sessions and maintenance of access to relevant advice and support about various aspects of their care, such as cardiac, behavioural and psychological services.
The programme at SHF is supervised by a team of physiotherapists, dieticians and smoking cessation counsellors. Diet control and specific dietary advice would be given by a dietitian during one-to-one consultation sessions. Exercise sessions were supervised by physiotherapists with each session lasting 90 minutes, consisting of 20 minutes of warm-up, 60 minutes of aerobic exercises, and 10 minutes of cooldown stretching exercises. Patients were encouraged to attend at least three exercise sessions per week. Patients had to record their physical examination and six-minute walk test (6MWT) data in their exercise log which were collated into SHF electronic records.
Outcome Measures
The primary outcome measure of this study was LDL levels. Secondary outcomes include high-density lipoprotein (HDL), TC, TG, fasting blood glucose (FBG), total walking distance and maximum heart rate during the 6MWT, body mass index (BMI), abdominal circumference, systolic BP and diastolic BP.
Statistical Analysis
Baseline demographic data collected included gender, age, ethnicity, smoking status, BMI status and number of cardiovascular co-morbidities i.e. hypertension (HTN), Diabetes Mellitus (DM), and dyslipidemia. Clinical parameters collected included all outcome measures. Data was collected from the electronic records of SHF and NHCS.
Power and Sample Size Calculations programme version 3.1.2 was used to calculate the sample size for a study of a continuous response variable between independent intervention and control groups of patients in a 1:2 ratio. Sample size estimation was based on the hypothesis of this study that improvements in LDL levels will be at least that of a previous study by Kubilius et al, where the LDL mean difference between cardiovascular patients in the intervention and control groups was 1.1mmol/L7. Assuming the response within patients in the intervention group was normally distributed with standard deviation (SD) of 2.5 mmol/L, a minimum of 61 and 122 cardiovascular patients in the intervention and control groups respectively was required in order to reject the null hypothesis that the population mean between the two comparison groups are equal, with 80% power and type I error (α) less than 0.05.
Summary statistics were used to report demographic data and clinical parameters. The Chi-square test was used to check for associations between discrete variables, while the analysis of variance and Student’s t-test were used for continuous variables. The within-group difference in parameters between baseline and one-year post follow-up were compared using the paired t-test. Multivariate linear regression was used to compare the changes in the various parameters between the intervention and control groups while controlling for confounders. All analyses were carried out using STATA SE version 12.0 for Windows (StataCorp, College Station, TX, USA) at a 2-sided significance level of 5%.
Results
From 2009 to 2013, a total of 572 cardiovascular patients participated in the community-based CR programme (Figure 1). Of these, 197 subsequently withdrew from the study due to unspecified reasons and 6 passed away within the one-year follow up period. Another 238 patients were excluded from the study as they had previously participated in the programme for primary prevention. Of the 131 eligible patients, a further 37 were excluded due to incomplete data. Accordingly, a total of 94 patients were included in the intervention group. The control group was randomly selected from the 2009 to 2013 database from NHCS.
Figure 1.
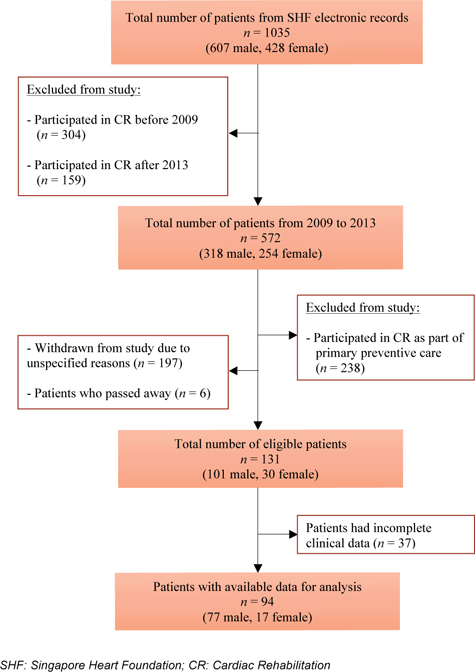
Flow Diagram of Cardiovascular Patients Recruited in Intervention Group
Baseline Demographics and Clinical Characteristics
Baseline demographics and clinical characteristics were generally comparable between the intervention and control group (Table 1). The proportion of patients who were smokers was larger in the control group (17.2% vs. 5.3%, p<0.01). The racial distribution (p=0.02) and number of cardiovascular comorbidities also differed (p=0.02) significantly between the two groups. The average age was approximately 60 years old in both groups. The majority of patients (84% and 77% in the intervention and control groups, respectively) were Chinese, reflecting the ethnicity distribution of the local population in Singapore. Most patients (72%) in the study had at least two of the three co-morbidities of HTN, DM or dyslipidemia. The different types of CVD in patients of both groups are summarised in Figure 2.
| Characteristics | Intervention Group (n = 94) | Control Group (n = 157) | p-value |
|---|---|---|---|
| Age (Years) | 59.6 (8.9) | 60.7 (9.7) | 0.36 |
| Gender | |||
| Male | 77 (81.9) | 131 (83.4) | 0.76 |
| Race | |||
| Chinese | 79 (84.0) | 121 (77.1) | 0.02 |
| Malay | 2 (2.1) | 15 (9.6) | |
| Indian | 6 (6.5) | 17 (10.8) | |
| Others | 7 (7.4) | 4 (2.5) | |
| Smoking Status | |||
| Yes | 5 (5.3) | 27 (17.2) | <0.01 |
| No | 89 (94.7) | 130 (82.8) | |
| Body Mass Index (kg/m2) | 24.4 (3.5) | 24.4 (3.8) | 0.9 |
| Body Mass Index Classificationa | |||
| Not Overweight | 35 (37.2) | 60 (28.2) | 0.68 |
| Overweight | 44 (46.8) | 66 (42.0) | |
| Obese | 15 (16.0) | 31 (19.7) | |
| Abdominal Circumference (cm) | 88.8 (9.1) | 88.0 (9.6) | 0.54 |
| Number of CVS co-morbiditiesb | |||
| 0 Total | 2 (2.1) | 10 (6.4) | 0.02 |
| 1 Total | 24 (25.5) | 45 (28.7) | |
| HTN | 2 (8.3) | 1 (2.2) | |
| DM | 1 (4.2) | 2 (4.4) | |
| Dyslipidemia | 21 (87.5) | 42 (93.4) | |
| 2 Total | 55 (58.5) | 64 (40.8) | |
| HTN + DM | 1 (1.8) | 1 (1.6) | |
| DM + Dyslipidemia | 4 (7.3) | 8 (12.5) | |
| HTN + Dyslipidemia | 50 (90.9) | 55 (85.9) | |
| 3 HTN + DM+ Dyslipidemia | 13 (13.9) | 38 (24.2) | |
Values are given as n (%) or mean ± SD.
CVS, Cardiovascular.
a Based on Ministry of Health, Singapore cut-off points of ≥23.0 kg/m2 as overweight and ≥27.5 kg/m2 as obese.
b Cardiovascular co-morbidities: Hypertension (HTN), Diabetes Mellitus (DM), Dyslipidemia.
Figure 2.
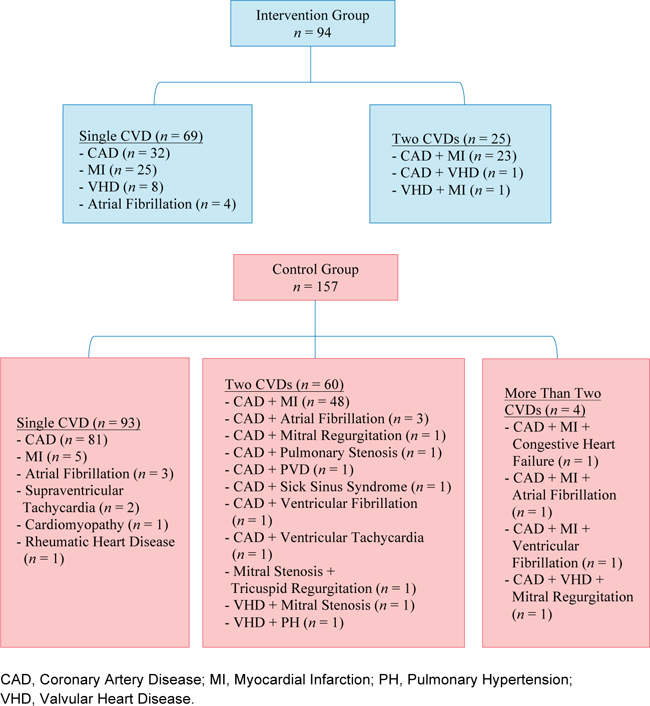
Different Types of cardiovascular diseases in patients of Intervention Group (top) and Control Group (bottom)
Outcome Measures
Changes in the primary outcome measure of LDL are shown in Figure 3, while changes in the secondary outcome measures over a year are summarised in Tables 2 and 3. At one year post follow-up, the intervention group showed small but statistically significant improvements in all components of the lipid panel, including the primary outcome measure of LDL (Δ: -0.3 mmol/L, CI: -0.4 to -0.2 mmol/L, p<0.01), TG (Δ: -0.1 mmol/L, CI: -0.2 to 0 mmol/L, p=0.03), and TC (Δ: -0.3 mmol/L, CI: -0.4 to -0.2 mmol/L, p<0.01), as well as in the FBG (Δ: -0.5 mmol/L, CI: -0.7 to -0.3 mmol/L, p<0.01). There were also improvements in systolic BP (Δ: -3.2 mmHg, CI: -6.2 to -0.3 mmHg, p=0.03), diastolic BP (Δ: -2.6 mmHg, CI: -4.3 to -0.8 mmHg, p=0.01), total walking distance (Δ: 36.9 m, 95% CI: 27.8 to 46.1 m, p<0.01) and maximum heart rate during the 6MWT (Δ: 3.6 beats/min, CI: 0.2 to 7.0 beats/min, p=0.04).
Figure 3.
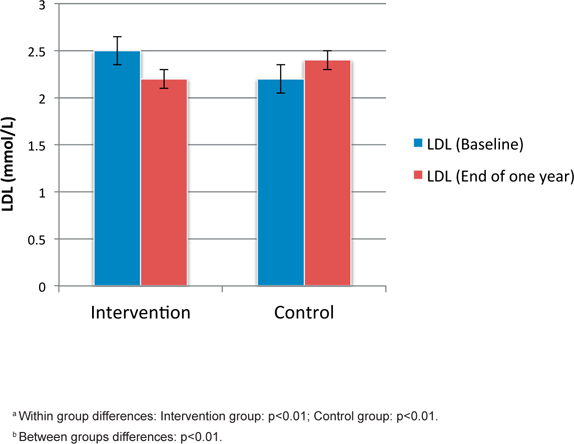
Changes in Primary Outcome Measure: Low Density Lipoprotein (LDL) Levels
| Measurements | Group | Baseline (95% CI) | End of one year (95% CI) | Difference (95% CI) | p-valuea | p-valueb | |
|---|---|---|---|---|---|---|---|
| Unadjusted | Adjustedc | ||||||
| HDL (mmol/L) | Intervention Control | 1.2 (1.2, 1.3) | 1.2 (1.1, 1.3) | 0.0 (0.0, 0.1) | 0.02 | 0.14 | <0.01 |
| 1.2 (1.1, 1.2) | 1.1 (1.1, 1.2) | 0.0 (0.0, 0.0) | 0.43 | ||||
| TG (mmol/L) | Intervention Control | 1.3 (1.2, 1.4) | 1.2 (1.1, 1.3) | -0.1 (-0.2, 0.0) | 0.03 | <0.01 | 0.01 |
| 1.2 (1.1, 1.3) | 1.3 (1.2, 1.4) | 0.1 (0.0, 0.2) | 0.03 | ||||
| TC (mmol/L) | Intervention Control | 4.3 (4.2, 4.5) | 4.0 (3.9, 4.2) | -0.3 (-0.4, -0.2) | <0.01 | <0.01 | <0.01 |
| 3.9 (3.8, 4.1) | 4.2 (4.0, 4.3) | 0.3 (0.1, 0.4) | <0.01 | ||||
| FBG (mmol/L) | Intervention Control | 6.1 (5.9, 6.4) | 5.6 (5.4, 5.9) | -0.5 (-0.7, -0.3) | <0.01 | <0.01 | <0.01 |
| 6.0 (5.8, 6.2) | 6.3 (6.1, 6.5) | 0.3 (0.2, 0.5) | <0.01 | ||||
HDL, High Density Lipoprotein; TG, Triglycerides; TC, Total Cholesterol; FBG, Fasting Blood Glucose.
a p value for statistical significance between baseline and 1-year post follow-up data measurement within group.
b p value for statistical significance between intervention and control group.
c Adjusted for race, smoking status and number of cardiovascular comorbidities.
| Measurements | Group | Baseline (95% CI) | End of one year (95% CI) | Difference (95% CI) | p-valuea | p-valueb | |
|---|---|---|---|---|---|---|---|
| Unadjusted | Adjustedc | ||||||
| BMI (kg/m2) | Intervention Control | 24.5 (23.7, 25.2) | 24.4 (23.8, 25.1) | 0.0 (-0.4, 0.3) | 0.89 | 0.19 | 0.20 |
| 24.4 (23.8, 25.0) | 24.6 (24.0, 25.2) | 0.2 (0.1, 0.3) | <0.01 | ||||
| Abdominal Circumference (cm) | Intervention Control | 88.8 (86.9, 90.6) | 89.4 (87.6, 91.3) | 0.7 (-0.2, 1.5) | 0.13 | 0.19 | 0.20 |
| 88.0 (86.5, 89.5) | 88.1 (86.6, 89.6) | 0.1 (-0.3, 0.5) | 0.59 | ||||
| Systolic BP (mmHg) | Intervention Control | 127.0 (124.2, 129.8) | 123.8 (121.6, 125.9) | -3.2 (-6.2, -0.3) | 0.03 | <0.01 | <0.01 |
| 115.7 (113.3, 118.1) | 120.7 (118.4, 123.0) | 5.0 (3.1, 6.8) | <0.01 | ||||
| Diastolic BP (mmHg) | Intervention Control | 73.7 (72.0, 75.4) | 71.1 (69.5, 72.8) | -2.6 (-4.3, -0.8) | 0.01 | <0.01 | <0.01 |
| 72.7 (71.2, 74.3) | 75.6 (74.3, 76.9) | 2.8 (1.7, 4.0) | <0.01 | ||||
| Resting HR (beats/min) | Intervention Control | 65.3 (63.2, 67.4) | 65.8 (63.7, 67.8) | 0.5 (-1.6, 2.6) | 0.64 | 0.09 | 0.12 |
| 70.4 (68.3, 72.4) | 73.4 (71.5, 75.3) | 3.0 (1.1, 4.9) | <0.01 | ||||
| Six-minute Walk Test Total Walking Distance (m) | Intervention Control | 522.2 (505.6, 538.8) | 559.2 (541.4, 576.9) | 36.9 (27.8, 46.1) | <0.01 | NA | NA |
| NA | NA | NA | NA | NA | NA | ||
| Maximum Heart Rate (beats/min) | Intervention Control | 105.0 (101.4, 108.6) | 108.6 (105.0, 112.3) | 3.6 (0.2, 7.0) | 0.04 | NA | NA |
| NA | NA | NA | NA | NA | NA | ||
BMI, Body Mass Index; BP, Blood Pressure; HR, Heart Rate; NA, Not Available.
a p value for statistical significance between baseline and 1-year post follow-up data measurement within group.
b p value for statistical significance between intervention and control group.
c Adjusted for race, smoking status and number of cardiovascular comorbidities.
In the control group, there was a statistically significant worsening of LDL (Δ: 0.2 mmol/L, CI: 0.1 to 0.3 mmol/L, p<0.01), TG (Δ: 0.1 mmol/L, CI: 0.0 to 0.2 mmol/L) (p=0.03), TC (Δ: 0.3 mmol/L, CI: 0.1 to 0.4 mmol/L, p<0.01), FBG (Δ: 0.3 mmol/LCI: 0.2 to 0.5 mmol/L, p<0.01). BMI (Δ: 0.2 mmHg, CI: 0.1 to 0.3 kg/m2, p<0.01), systolic BP (Δ: 5.0 mmHg, CI: 3.1 to 6.8 mmHg, p<0.01), diastolic BP (Δ: 2.8 mmHg, CI: 1.7 to 4.0 mmHg, p<0.01). Total walking distance and maximum heart rate in 6MWT were not available for the patients in the control group as 6MWTs were not conducted in the hospital setting.
When the two groups were compared, the intervention group showed greater improvement for the primary outcome measure of LDL. Mean LDL decreased from 2.5 mmol/L to 2.2 mmol/L in the intervention group, but increased from 2.2 mmol/L to 2.4 mmol/L in the control group (p<0.01). The intervention group also had greater improvements than the control group for the secondary outcome measures of TG (p=0.03), TC (p<0.01), FBG (p<0.01), systolic BP (p<0.01) and diastolic BP (p<0.01). These differences were still significant even after adjusting for race, smoking status and number of CVS comorbidities. There were no statistically significant differences between the two groups for the changes in the secondary outcomes of BMI, abdominal circumference and resting heart rate.
Discussion
This is the first study in the Asia-Pacific region to evaluate the impact of a community-based CR program in improving clinical parameters. There are several strengths to our study.
Firstly, unlike similar studies by Jackson et al and Richardson et al.6, 11, our study compared cardiovascular patients who have completed one year of a communitybased CR programme with a control group. The addition of a control group, and statistical adjustment for baseline characteristics that were different between the two groups, reduced bias owing to confounding by differences in these baseline characteristics between the two groups. Secondly, the number of patients included in the analyses exceeded the sample size required for the primary outcome measure, minimising the type II error rate. Thirdly, our study period of one year was sufficient, as suggested by a study by Morrin et al.12 on the impact of duration of a CR programme on coronary risk profile and health-related quality of life outcomes, which noted that significant improvements in lipid profile could already be observed at three months and six months.
The findings of this study suggest that participation in a community-based CR programme for a year was associated with improvements in the lipid and FBG profiles of cardiovascular patients, as well as in physical examination parameters such as systolic and diastolic BP, and results for the 6MWT. In addition, compared with controls, those who had undergone the programme also showed greater improvements in several parameters, namely LDL, TG, TC, FBG and systolic BP and diastolic BP.
While there was significant improvement in LDL levels from baseline in the intervention group, the improvement was only 0.3 mmol/L, which was less than what we have hypothesized. However, it is worth noting that our study participants had relatively lower LDL levels even at baseline, compared to that in the study by Kubilius et al., where the baseline LDL levels in the intervention and control groups were 3.7 ± 0.8 mmol/L and 3.0 ± 1.4 mmol/L respectively. Given that reductions in LDL, TC and FBG were also observed in previously conducted studies6, 7, 11, our study results provide support that community-based CR programmes are able to improve lipid profiles and FBG in cardiovascular patients.
We have chosen to use LDL as our primary outcome measure. This is in spite of the American College of Cardiology (ACC) / American Heart Association (AHA) Task Force on Practice Guidelines abandoning the longstanding principle of treating to specific LDL targets due to a lack of data based on randomized controlled trials with hard clinical outcomes to support a treat-totarget approach13. Instead, they advocated treatment based on providing an appropriate intensity of statin treatment after stratifying patients based on risk13. Despite this, there is an abundance of observational studies and other intervention trial data that has demonstrated that reduction in LDL is associated with favourable effects on reduction in coronary heart disease (CHD) events, especially in patients at high risk for CHD or those who have already manifested CHD14. Moreover, guidelines in other regions, such as the European and Canadian guidelines, still maintain lipid targets based on absolute risk15. Lifestyle modifications, which are major components of the CR programme, are also recommended in the ACC/AHA guidelines as the foundation of risk reduction13. Hence, we believe LDL-lowering is a reasonable surrogate marker for the programme’s effectiveness.
We believe the reduction in FBG shown in our study is also of clinical significance. Diabetes is recognised by the American Diabetes Association as an independent risk factor for CVD, and controlling single and especially multiple risk factors have substantial benefits in preventing or slowing CVD in people with diabetes16. Of note, there is evidence17 to suggest that coexistence of diabetes with hypertension conferred a 3.43-fold higher CVD risk. As such, our community-based CR programme may be of benefit to not just patients with CVD, but also diabetes patients as well, especially if they have concomitant hypertension.
Statistically significant improvements in both systolic and diastolic BP were also noted in our study, similar to that in a study done in the United Kingdom by Richardson et al.6. However, it is worth noting that BP in both groups of patients appear to be well controlled, even at baseline (Table 3), based on target ranges of 140 mmHg for systolic BP and 80mmHg for diastolic BP advocated by the latest guidelines from the Eight Joint National Committee18. Improvements in BP were also small, with a 3.2 point reduction in systolic BP in the intervention group. Further studies are needed to evaluate whether such a reduction is clinically significant, and whether there are improvements in clinical outcomes such as mortality, as well as whether such a community-based CR programme can achieve similar benefits in patients with more poorly controlled blood pressure.
Our study also found improvements in the results of the 6MWT in the intervention group, though we were not able to compare this with the control group. The 6MWT has been found to be a useful parameter that is reflective of activities of daily living in comparison to other walk tests19. Our results therefore suggest that the programme may improve daily functioning, an outcome likely to be highly relevant for patients.
There were limitations to the present study which should be considered when interpreting the findings. First, although we had a control group for comparison, we were not able to obtain a complete range of clinical parameters for comparison due to differences in monitoring regimes across institutions. For instance, the control group did not have data for the 6MWT as this was only performed at the SHF for the intervention group. Second, our study did not have data on key clinical outcomes such as mortality and hospital admissions, which would be relevant to both patients and health care policy makers. Third, we were unable to obtain data on the rate of participation in CR within the intervention group, even though it was recommended to attend three sessions a week. However, this would have been unlikely to affect our findings that the programme is beneficial, as lower participation would likely have caused the results to shift toward the null hypothesis and therefore reduced the chances of a falsepositive conclusion. Fourth, we were unable to obtain data regarding medication history, such as the doses of medications used. However, as all patients continued to receive usual care regardless of their assigned group, we assumed they received a similar level of care in terms of how their medications were titrated. Nevertheless, we acknowledge that other factors such as medication adherence could have contributed to residual confounding.
Conclusion
The results of this study suggest that our community-based CR programme in Singapore can improve various clinical and physical parameters in cardiovascular patients. Future prospective controlled studies are needed to confirm our findings, as well as to evaluate the effectiveness of the programme on important patient outcomes such as mortality and cost-effectiveness.
Footnotes
a Department of Pharmacy, Singapore General Hospital, Republic of Singapore,
b Department of Pharmacy, Faculty of Science, National University of Singapore, Republic of Singapore,
c Duke-NUS Medical School, Republic of Singapore,
d Heart Wellness Centre, Singapore Heart Foundation, Republic of Singapore,
e Department of Cardiology, National Heart Centre Singapore, Republic of Singapore.
Correspondence to and requests for reprints to be made to Yu Heng Kwan, MD-PhD Candidate, Program in Health Services and Systems Research, Duke-NUS Medical School. 8 College Road, Singapore 169857. Tel: +65 - 9023 1226; Fax: +65 - 6779 1554 Email: yuheng@u.duke.nus.edu Conflict of interest declaration: The authors declare no conflict of interest nor any sources of funding for this study.
© The Author(s) 2016. This article is published with open access by ASEAN Federation of Cardiology.
References
- 1.Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. linical practice guideline (update): adult sinusitis. Otolaryngology– head and neck surgery: Official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2015;152:S1–s39. doi: 10.1177/0194599815572097. [DOI] [PubMed] [Google Scholar]
- 2.Sasayama S. Heart disease in Asia. Circulation. 2008;118:2669–2671. doi: 10.1161/CIRCULATIONAHA.108.837054. [DOI] [PubMed] [Google Scholar]
- 3.Leon AS, Franklin BA, Costa F, et al. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005;111:369–376. doi: 10.1161/01.CIR.0000151788.08740.5C. [DOI] [PubMed] [Google Scholar]
- 4.Goel K, Lennon RJ, Tilbury RT, Squires RW, Thomas RJ. Impact of cardiac rehabilitation on mortality and cardiovascular events after percutaneous coronary intervention in the community. Circulation. 2011;123:2344–2352. doi: 10.1161/CIRCULATIONAHA.110.983536. [DOI] [PubMed] [Google Scholar]
- 5.Dalal HM, Doherty P, Taylor RS. Cardiac rehabilitation. BMJ (Clinical research ed) 2015;351:h5000. doi: 10.1136/bmj.h5000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richardson G, van Woerden HC, Morgan L, et al. Healthy hearts–a community-based primary prevention programme to reduce coronary heart disease. BMC cardiovascular disorders. 2008;8:1–8. doi: 10.1186/1471-2261-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kubilius R, Jasiukeviciene L, Grizas V, Kubiliene L, Jakubseviciene E, Vasiliauskas D. The impact of complex cardiac rehabilitation on manifestation of risk factors in patients with coronary heart disease. Medicina (Kaunas, Lithuania) 2012;48:166–173. [PubMed] [Google Scholar]
- 8.Mosleh SM, Bond CM, Lee AJ, Kiger A, Campbell NC. Effects of community based cardiac rehabilitation: Comparison with a hospital-based programme. European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology. 2015;14:108–116. doi: 10.1177/1474515113519362. [DOI] [PubMed] [Google Scholar]
- 9.Arena R. Exercise and Rehabilitation in Heart Failure, An Issue of Heart Failure Clinics: Elsevier; 2014 11 Dec 2014.
- 10.Meng Khoo C, Tai ES. Trends in the incidence and mortality of coronary heart disease in asian pacific region: the Singapore experience. Journal of atherosclerosis and thrombosis. 2014;21:S2–8. doi: 10.5551/jat.21_sup.1-s2. [DOI] [PubMed] [Google Scholar]
- 11.Jackson JL, Emery CF. Emotional distress, alexithymia, and coping as predictors of cardiac rehabilitation outcomes and attendance. Journal of cardiopulmonary rehabilitation and prevention. 2013;33:26–32. doi: 10.1097/HCR.0b013e318276864c. [DOI] [PubMed] [Google Scholar]
- 12.Morrin L, Black S, Reid R. Impact of duration in a cardiac rehabilitation program on coronary risk profile and healthrelated quality of life outcomes. Journal of cardiopulmonary rehabilitation. 2000;20:115–121. doi: 10.1097/00008483-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/ AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014;63:2889–2934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Hoogwerf BJ, Huang JC. Cardiovascular Disease Prevention 2012 [cited 2015 15 August]. Available from: http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/heart-disease-risk-reduction/.
- 15.Saraf S, Ray KK. New worldwide lipid guidelines. Current opinion in cardiology. 2015;30:447–453. doi: 10.1097/HCO.0000000000000184. [DOI] [PubMed] [Google Scholar]
- 16.American Diabetes Association. (8) Cardiovascular disease and risk management. Diabetes care. 2015;38:38–57. doi: 10.2337/dc15-S011. [DOI] [PubMed] [Google Scholar]
- 17.Qiu M, Shen W, Song X. Effects of prediabetes mellitus alone or plus hypertension on subsequent occurrence of cardiovascular disease and diabetes mellitus: longitudinal study. Hypertension. 2015;65:525–530. doi: 10.1161/HYPERTENSIONAHA.114.04632. [DOI] [PubMed] [Google Scholar]
- 18.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) Jama. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 19.Solway S, Brooks D, Lacasse Y. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest. 2001;119:256–270. doi: 10.1378/chest.119.1.256. [DOI] [PubMed] [Google Scholar]


