Abstract
Purpose:
The purpose of this study was to evaluate and compare the flexural strength and microhardness of provisional restorative materials fabricated utilizing rapid prototyping (RP), Computer Assisted Designing and Computer Assisted Milling (CAD-CAM) and conventional method.
Materials and Methods:
Twenty specimens of dimensions 25 mm × 2 mm × 2 mm (ADA-ANSI specification #27) were fabricated each using: (1) Three dimensional (3D) printed light-cured micro-hybrid filled composite by RP resin group, (2) a milled polymethyl methacrylate (CH) using CAD-CAM (CC resin group), and (3) a conventionally fabricated heat activated polymerized CH resin group. Flexural strength and microhardness were measured and values obtained were evaluated.
Results:
The measured mean flexural strength values (MegaPascals) were 79.54 (RP resin group), 104.20 (CC resin group), and 95.58 (CH resin group). The measured mean microhardness values (Knoop hardness number) were 32.77 (RP resin group), 25.33 (CC resin group), and 27.36 (CH resin group). The analysis of variance (ANOVA) test shows that there is statistically significant difference in the flexural strength values of the three groups (P < 0.05). According to the pairwise comparison of Tukey's honest significant difference (HSD) test, flexural strength values of CC resin group and CH resin group were higher and statistically significant than those of the RP resin group (P < 0.05). However, there was no significant difference between flexural strength values of CC resin and CH resin group (P = 0.64). The difference in microhardness values of the three groups was statistically significant according to ANOVA as well as the intergroup comparison done using the Tukey's HSD (post hoc) test (P < 0.05).
Conclusions:
CC-based CH had the highest flexural strength whereas RP-based 3D printed and light cured micro-hybrid filled composite had the highest microhardness.
Keywords: Computer-Assisted Designing and Computer-Assisted Milling, provisionals, rapid prototyping
INTRODUCTION
Provisional fixed dental prostheses (FDPs) are an integral part of fixed prosthodontics and dental implantology. The provisional FDPs must satisfy the requirements of pulpal protection, periodontal health, occlusal compatibility, maintaining tooth position, protection against fracture, resistance to functional loads, resistance to removal forces, maintaining inter-abutment alignment, be easily contourable, color stable, and have sufficient translucency. The uses of a provisional FDP are diagnostic purpose when the functional, occlusal and esthetic parameters are to be developed to identify an optimum treatment outcome before the completion of the definitive prosthesis, providing a template for defining tooth contour, esthetics, proximal contacts, and occlusion. It can also provide an important tool for the psychological management of patients until the final restorations are cemented.[1]
Conventionally, various methods and materials have been introduced to provide a provisional restoration that is esthetic, easy to fabricate, most importantly having a high strength and hardness. These materials for the fabrication of single and multiple unit provisional restorations are mostly resin based. They differ with regard to the method of polymerization, filler composition, and monomer type.[2] These materials include[3] poly(methyl methacrylate) (PMMA), poly (ethyl methacrylate), polyvinyl(ethylmethacrylate), bisphenol A gycidyl methacrylate, bis-acryl resin composites, urethane di-methacrylate resins, etc.
Computer-Assisted Designing and Computer-Assisted Milling (CAD-CAM) was first used in dentistry in the 1970s. CAD-CAM (CC) has now become a well-accepted technology in most modern dental laboratories and for some enterprising clinicians at the chairside.[4] CC, i.e., subtractive technologies have emerged during the recent years for various applications including provisional restorations fabricated by milling the resin-based blanks which are cured under optimal conditions. Not only do they exhibit increased mechanical strength and prevent porosity within the restorations but also have reduced the chairside time.
In addition to subtractive methods, additive manufacturing is also an emerging technology. Additive manufacturing is defined by the American Society for Testing and Materials as the process of joining materials to make objects from three dimensional (3D) model data, usually layer upon layer, as opposed to subtractive manufacturing methodologies. In principle, the process works by taking a 3D computer file and creating a series of cross-sectional slices. Each slice is then printed one on top of the other to create the 3D objects. While using this technology for resins, a concentrated beam of ultraviolet (UV) light is focused onto the surface of a platform filled with liquid photopolymer and as the light beam draws the object onto the surface of the liquid, each time a layer of resin is polymerized. One attractive feature of this process is that there is no wastage of the material. Traditionally additive manufacturing processes were first used in the 1980s to manufacture prototypes, models, and casting patterns. Thus, it has its origins in rapid prototyping (RP), which is the name given to the rapid production of models using additive layer manufacturing.[4]
RP is being used in dentistry for a range of dental specialties, including oral and maxillofacial prosthodontics and dental implantology. It is used to fabricate physical models, surgical guides, extraoral maxillofacial prostheses, and recently in fixed Prosthodontics for long-term provisional FDPs. It is claimed by the manufacturers to have better mechanical properties and esthetics compared to its conventionally fabricated counterparts which need to be further verified.
In choosing a provisional restorative resin material, the clinicians select a product based on factors that include clinically desirability, adequate working time, ease of mix and repair, biocompatibility with the pulp and soft tissue, dimensional stability during and after fabrication, shade selection, and color stability.[5] Understanding the mechanical properties is necessary to evaluate these newer technologies that are coming to the market, verify the manufacturers' claims and further compared with conventional ones to obtain an optimum material and a suitable technique for long-term provisional FDPs. Thus, various mechanical properties such as flexural strength, hardness, impact strength, and color stability become extremely important. The flexural strength and microhardness of provisional materials are important, particularly when the patient must use the provisional restoration for an extended period, when the patient exhibits parafunctional habits or when long-span prostheses are planned.[6]
Most of the studies on flexural strength and microhardness of provisional restorative materials which have been done so far are comparing different commercial materials and/or those materials with reinforcements such as polyethylene, glass, nylon, and carbon. There is a scarcity of literature on determination of properties of provisional restorative materials fabricated by those utilizing the recent technologies of CC and RP.
Thus, in this study, mechanical properties such as flexural strength and microhardness of different provisional restorative materials used to fabricate provisional FDPs utilizing the following methods will be evaluated:
Conventional method using heat activated PMMA
CC milling of PMMA blanks (subtractive method)
RP a visible light cure Microhybrid filled composite resin (3D printing and additive method).
MATERIALS AND METHODS
Twenty specimens of each group of dimensions, 25 mm × 2 mm × 2 mm (ADA-ANSI specification #27)[6] were fabricated using each of the above-mentioned fabrication processes. To fabricate the samples for the CC resin group and the RP resin group, the specimens were designed as per the dimensions using the CAD software and computer file in STL (stereolithography/standard tessellation language) format was prepared and kept ready to be utilized by the respective units for milling and 3D printing.
PREPARATION OF SPECIMENS
Conventional heat activated resin specimens
In order to prepare the final specimens for polymethyl methacrylate (CH) group, the intermediate specimens were prepared with pattern resin (GC Corporation, Japan) in the machined brass mold. Further, these pattern resin specimens were invested in conventional flasks and the conventional PMMA test specimens were fabricated using the compression molding technique.
Computer-Assisted Designing and Computer-Assisted Milling specimens
In this study, Ceramill TEMP (AmannGirrbach, AG, Austria) PMMA resin blanks (100% by weight, polymethylmethacrylate) were used to fabricate specimens for the CC group. The computer file in STL format was transferred to Ceramill Mind (CAD program), and the specimens were transferred to the milling unit. The specimens were milled in two prepolymerized PMMA blanks (Ceramill TEMP) of the shade A2. Conventional cutters, trimmers were used for finishing and polishing within the milling machine.
Rapid prototyping (three dimensional printing) specimens
Envision TEC's E-Dent 100 is a light-cured micro-hybrid filled dental crown and bridge material for long-term temporization. Provisionals are photopolymerized on a voxel by voxel basis within the liquid resin. EnvisionTECs Perfactory® 4 Standard 3D Printer was used to fabricate the RP (3D printing) specimens. In principle, the process works by using a 3D computer file and creating a series of cross-sectional slices. Each slice is printed one on top of the other to create the 3D object. The process is repeated to form the entire layer of specimen, until the specimens as designed are produced.
TESTING OF SPECIMENS
Flexural strength determination
A Universal Testing Machine (Star Testing System, India. Model No. STS 248) was utilized for this study and a three-point loading system was used for the application of load and all the sixty specimens of the three groups were subjected to the three-point bending test. The load was applied at a crosshead speed of 3 mm/min, over a distance of 20 mm, the loading was continued till fracture occurred and the breaking load was noted. These breaking load values were converted to flexural strength (σ) using the following formula:
σ =3FL/2bd2,
where,
σ = Flexural strength
F = Load (force) at the fracture point
L = length of the support span
b = Width of specimen
d = Thickness of the specimen
The flexural strength values obtained were in MegaPascals (MPa) by the software, provided along with the machine.
Microhardness testing
The fractured specimens were used to determine the surface hardness. The fractured specimens were embedded in acrylic resin for the same as a measure to secure the specimens in place for microhardness testing. A microhardness tester (Reichert Austria, Serial No. 363798) was utilized for the same. Surface hardness was determined by loading each specimen for 15 s with a force of 50 g, after mounting it on the microhardness tester. A rhomboid-shaped indentation was obtained on each specimen and its image was transferred to the computer monitor with the help of a microscope present along with the microhardness tester. The longest diagonal of the diamond indentation was marked and Vickers hardness number was calculated with the help of the software. It was then converted to Knoop hardness number (KHN) with the help of the software itself.
Statistical analysis
Data obtained were compiled on MS-Excel sheet. Mean and standard deviation (SD) readings were calculated. Statistical tests were performed using SPSS Software Version 17.0 (Chicago, IL, USA). Intergroup comparison of flexural strength and microhardness values was done using one-way analysis of variance (ANOVA) and pairwise post hoc comparison was done using Tukey's honest significant difference (HSD) post hoc test. P < 0.05 was considered to be statistically significant.
RESULTS
The flexural strength and microhardness were recorded for each specimen. This raw data of the values obtained were compiled on MS-Excel sheet to get the mean and SD. The data were then statistically analyzed.
The mean and SDs were determined for the three groups: CH resin, CC resin, and RP resin [Table 1]. P value was set as statistically significant at P = 0.05. Intergroup comparison was done using one-way ANOVA [Table 2]. The pairwise comparison was done using Tukey's HSD post hoc test [Table 3]. The results were analyzed using software package SPSS Version 17.0 (Chicago, IL, USA).
Table 1.
Mean and standard deviation values of flexural strength and microhardness of the three groups
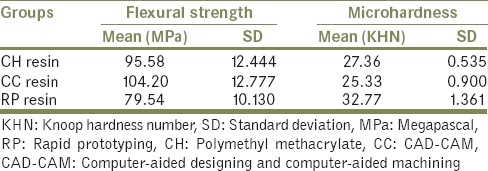
Table 2.
Intergroup comparison of flexural strength and microhardness using one-way analysis of variance
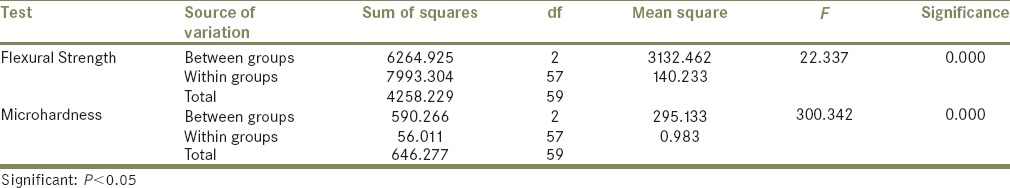
Table 3.
Pairwise comparison using Tukey's honest significant difference test (post hoc)
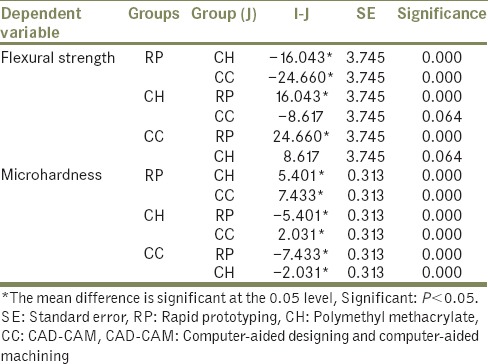
The mean flexural strength values in CC resin group (104.20 MPa) were higher compared to the specimens of CH resin group (95.58 MPa) and RP resin group (79.54 MPa). The ANOVA Test shows that there is statistically significant difference in the flexural strength values of the three groups (P < 0.05). However, according to the pairwise comparison of Tukey's HSD test, flexural strength values of CC resin group and CH resin group were higher and statistically significant than those of the RP resin group (P < 0.05). However, there was no significant difference between flexural strength values of CC resin and CH resin group (P = 0.64).
RP resin group showed the highest microhardness values at the surface (32.76 KHN) followed by CH resin group (27.37 KHN) and CC resin group (25.33 KHN). The difference in microhardness values of the three groups was statistically significant according to ANOVA as well as the intergroup comparison done using the Tukey's HSD (post hoc) test (P < 0.05).
DISCUSSION
Provisional FDPs are essential components of fixed prosthodontic treatment. Provisional restorations must satisfy biologic, esthetic, and mechanical requirements such as resistance to functional loads, resistance to removal forces, and maintenance of abutment alignment.[7] There are a number of materials available for provisional FDPs. The majority of these materials can fit into two main categories based on their composition: (1) Methyl methacrylate resins and (2) composite resins.[2,3,7] Traditional methyl methacrylate type resins are mono-functional low molecular weight, linear molecules that exhibit decreased strength and rigidity whereas composite resins are di-functional and capable of cross-linking with another monomer chain imparting strength and toughness to the material.[6] There is not a single material or method that has been found to be useful in all clinical situations, so it is important to know the properties of the material in order to know the limitations and indications/contraindications for their clinical use for extended periods of time. One such property is flexural strength and the other is microhardness.[6]
If the provisional FDPs are expected to function for extended periods of time or when additional therapy is required before completion of definitive treatment viz. during the prosthetic phase of dental implants and reconstructive procedures, while evaluation of a change in vertical dimension, for orthodontic stabilization, in case of assessing the results of periodontal and endodontic therapies and in cases of bruxism, the improved mechanical properties play an important role.[8,9,10]
In case of prosthetic phase of dental implants, longer treatment times and the necessity for addressing tissue contour issues before definitive treatment dictate techniques that would provide more durability. Management involving indirect fabrication of acrylic resin provisional restorations for increased polymerization and reinforcement can be done with assorted types of methods and materials.[1]
Heat-activated acrylic resin is inherently stronger, has greater stability, and is more resistant to polymer breakdown than autopolymerized resin.[8] It also has the advantages of color stability, maintenance of surface finish, and resistance to wear.[8] Provisional restorations fabricated from heat-processed acrylic resin can function satisfactorily for extended periods of time.[11]
Rekow[12] reviewed the CC systems used in dentistry and proposed its use for provisionalization. Manufacturing under industrial conditions permits high-density polymer-based restorations which offer favorable mechanical behavior and biocompatibility.[13] These CC restorations also reduce the chair side time of the patient.[14] In addition, according to Rocca et al.,[15] it is over the last two decades that the CC technique has evolved. Hardware has become less expensive, software is easier to use, fabrication is faster, and the milled restorations are more accurate in terms of anatomic form, marginal fit, and occlusal/interproximal contacts. Thus, the CC approach is becoming more popular for the fabrication of tooth-colored indirect restorations.[15]
Moreover, the location, shape, and extension of the pontics over the soft tissue of the residual ridge could be determined virtually. In addition, in situations where a fracture of the provisional restoration occurs, the dataset will be available for a second milling process. Furthermore, the shape of the restoration can be simulated for the fabrication of the definitive prosthesis. The customized provisional restoration could be scanned after a prolonged clinical acceptance and digitally transferred into a definitive restoration. This facilitates the precise transfer of the contour of the provisional into a definitive restoration and in turn will result in higher predictability for the definitive restorations.[13]
CC milling of PMMA blanks (subtractive method) has been used for the fabrication of provisional FDPs since past few years.[16] However, RP (3D printing and additive method) is an emerging technology for the same. It basically produces solid layers using a concentrated UV light beam that moves on a photosensitive liquid polymer resin placed on a platform. As the first layer is polymerized, the platform is lowered a few microns and the next layer is cured. This process is repeated until the whole solid object is completed. The object is then rinsed with a solvent and placed in a UV oven to thoroughly cure the resin.[17]
RP (3D printing) has been used in the past for various applications viz. fabrication of maxillofacial prosthesis,[17,18] making complete dentures,[19] crowns, bridges and/or copings/resin patterns for the same[20] and making dental casts models,[17,21,22,23] surgical templates for guided surgery of implants,[17,24] and fabrication of patterns for Cast Partial Dentures (CPD),[4,17,20,25,26,27,28,29,30] and post and core.[22] But, apart from these, there is little literature on its application for provisional FDPs.
Provisional FDPs should resist wear to help maintain the position of prepared teeth and meet the esthetic needs of the patient. Microhardness can be used as an indicator of density, and it can be hypothesized that a denser material would be more resistant to wear and surface deterioration. Resins without fillers such as PMMA are also more prone to wear however absence of fillers and absence of polarity due to the mono-functional nature of the molecules render them more color stable.[31] The surface hardness of a material is a complex mechanical property affected by several other properties, including strength, proportional limit, ductility, malleability, and resistance to abrasion and cutting. However, surface hardness alone is not an indicator of overall rigidity and strength and cannot predict the clinical behavior of long-span prostheses as quoted by Diaz-Arnold et al.[5] Apart from that higher the hardness value, denser the material and lesser is the tendency to absorb bacterial plaque.[32]
In case of long term use of provisional FDPs such as in full mouth rehabilitation, in unforeseen events such as laboratory delays, nonavailability of patient, and in the restorative phase of implant therapy, the strength of a material can be a determinant of how well these requirements are met. Flexural strength, also known as transverse strength, is a measurement of the strength of a bar (supported at each end) under a static load. The flexural strength test is a combination of tensile and compressive strength tests and includes elements of proportional limit and elastic modulus measurements. The flexural strength of provisional materials is important, particularly when the patient must use the provisional restoration for an extended period, when the patient exhibits parafunctional habits or when a long span prosthesis is planned.[6] Strength is also said to be particularly critical for anterior fixed partial dentures because fracture can cause embarrassment and inconvenience for the patient.[33]
Thus, keeping in mind the long-term FDPs, this study was done to evaluate the effect of manufacturing technique and material of provisional FDPs on mechanical properties like flexural strength and hardness, which were fabricated using:
Conventional indirect method using heat activated PMMA
CC milling of PMMA blanks (subtractive method)
RP of micro-hybrid filled visible light-cured composite resin (3D printing and additive method).
The results of this study indicated that the mean flexural strength values of CC resin group (104.2 MPa) were the highest, followed by the specimens of CH resin group (95.58 MPa) and RP resin group (79.54 MPa), respectively. Flexural strength values of CC resin group and CH resin group were higher and statistically significant than those of the RP resin group (P < 0.05). However, there was no statistically significant difference between flexural strength values of CC resin and CH resin group (P = 0.64).
The material used for CC milling in this study, Ceramill TEMP, is a cross-linked polymer of PMMA resin. The cross-linking consists of methacrylic acid ester-based polymers. According to Edelhoff et al.,[14] these high-density polymers based on highly cross-linked resins are manufactured in an industrial process, thus, exhibiting superior qualities. These findings are similar to the research conducted by Alt et al.,[34] who investigated the influence of fabrication method, storage condition, and use of different materials, on the fracture strength of provisional 3-unit FDPs using CC technologies and resin-based blanks cured under optimal conditions. They concluded that CC specimens exhibited increased mechanical strength and had less porosity within the restoration. Thus, it can be proposed that it was due to these optimal curing conditions, the CC specimens showed the highest flexural strength in this study.
A product made by RP is influenced by the technique of fabrication utilized. The technique can cause shrinkage of the specimen during building, postcuring and due to minimal thickness of layers. In addition, data conversion and manipulation while formatting into an STL format could also result in some changes.[23] Therefore, it can be postulated that RP resin group has lesser flexural strength than CC resin group.
Conventional methacrylate resins are mono-functional, low-molecular weight, and linear molecules that exhibit decreased strength and rigidity. In addition, if they are not polymerized under pressure, air bubbles will be trapped and decrease their strength. The strength of the material, polymerization shrinkage, and other properties also depend on the residual monomer content.[35] Moreover, the conventional heat activated specimens were made by the same operator according to the manufacturers' instructions, but the samples were prepared at different time intervals. Therefore, operator related variations and absence of cross-linking in the conventional heat activated resin could have led to lesser flexural strength values in these specimens when compared to the CC resin specimens.
Haselton et al.,[6] who compared the flexural strength of five PMMA-based and eight bis-acryl-based provisional restorative materials after conditioning in artificial saliva, had contradictory findings. They concluded that the highest flexural strength values were found among bis-acryl type material. There was no correlation between the flexural strength of different provisional restorative materials when immersed in artificial saliva. However, some bis-acryl resins reported lesser strength than PMMA.[6]
Apart from flexural strength, the microhardness of provisional FDPs was evaluated in this study. The RP resin group showed the highest microhardness values at the surface (32.8 KHN) followed by CH resin group (27.5 KHN) and CC resin group (25.6 KHN). The difference in microhardness of the three groups was statistically significant (P < 0.05).
The composite resins contain multifunctional cross-linked monomers and other inorganic fillers which are said to increase the hardness of these resins compared to PMMA.[31]
The findings of this study were also similar to the result obtained by Diaz-Arnold et al.[5] who found out that all composite resin materials exhibited superior microhardness over the traditional methyl methacrylate resins throughout a 14-day interval of investigation. According to them, these resins contain inorganic fillers to increase their resistance to abrasion and decrease polymerization shrinkage in comparison to PMMA material used in the other groups.
In India, the CC and 3D printed temporization are being used and the economics is improving with the passage of time, making these technologies relevant in present time and age.
CONCLUSION
Within the limitations of this in vitro study, and on the basis of the results obtained, it can be concluded that:
CC resin group specimens exhibited highest flexural strength values followed by CH resin group and RP resin group
The flexural strength values of all the groups were higher than minimal acceptable flexural strength of provisional FDP materials which is 50 MPa, according to ADA-ANSI specification #27
RP resin group exhibited highest microhardness values followed by CH resin group and CC resin group.
It may be further concluded that:
When the strength of the provisional FDPs is a prime concern in long term and long span conditions, provisional FDPs fabricated by CC milling of the PMMA blanks may be used
In situations which advocate maintenance of vertical dimension and wear resistance, provisional FDPs fabricated using RP (3D printed) of a visible light cured micro-hybrid filled composite may be considered
CC and RP showed the highest flexural strength and microhardness values, respectively. However, heat activated PMMA may be a comparable option to the newer techniques and materials.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Burns DR, Beck DA, Nelson SK. Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: Report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J Prosthet Dent. 2003;90:474–97. doi: 10.1016/s0022-3913(03)00259-2. [DOI] [PubMed] [Google Scholar]
- 2.Gratton DG, Aquilino SA. Interim restorations. Dent Clin North Am. 2004;48:487–97. doi: 10.1016/j.cden.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 3.Shillinburg HT, Hobo S, Whitsett LD, Jacobi R, Brackett SE. Fundamentals of Fixed Prosthodontics. 4th ed. Chicago, IL: Quintessence Publishing Co; 1997. pp. 225–56. [Google Scholar]
- 4.van Noort R. The future of dental devices is digital. Dent Mater. 2012;28:3–12. doi: 10.1016/j.dental.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 5.Diaz-Arnold AM, Dunne JT, Jones AH. Microhardness of provisional fixed prosthodontic materials. J Prosthet Dent. 1999;82:525–8. doi: 10.1016/s0022-3913(99)70050-8. [DOI] [PubMed] [Google Scholar]
- 6.Haselton DR, Diaz-Arnold AM, Vargas MA. Flexural strength of provisional crown and fixed partial denture resins. J Prosthet Dent. 2002;87:225–8. doi: 10.1067/mpr.2002.121406. [DOI] [PubMed] [Google Scholar]
- 7.Rosenstiel SF, Land MF, Fujimoto J. Contemporary Fixed Prosthodontics. 4th ed. St. Louis: Mosby Elsevier Inc; 2007. pp. 466–505. [Google Scholar]
- 8.Binkley CJ, Irvin PT. Reinforced heat-processed acrylic resin provisional restorations. J Prosthet Dent. 1987;57:689–93. doi: 10.1016/0022-3913(87)90364-7. [DOI] [PubMed] [Google Scholar]
- 9.Sen D, Göller G, Issever H. The effect of two polishing pastes on the surface roughness of bis-acryl composite and methacrylate-based resins. J Prosthet Dent. 2002;88:527–32. doi: 10.1067/mpr.2002.129335. [DOI] [PubMed] [Google Scholar]
- 10.Hamza TA, Rosenstiel SF, El-Hosary MM, Ibraheem RM. Fracture resistance of fiber-reinforced PMMA interim fixed partial dentures. J Prosthodont. 2006;15:223–8. doi: 10.1111/j.1532-849X.2006.00110.x. [DOI] [PubMed] [Google Scholar]
- 11.Davidoff SR. Heat-processed acrylic resin provisional restorations: An in-office procedure. J Prosthet Dent. 1982;48:673–5. doi: 10.1016/s0022-3913(82)80026-7. [DOI] [PubMed] [Google Scholar]
- 12.Rekow ED. Dental CAD/CAM systems: A 20-year success story. J Am Dent Assoc. 2006;137:5S–6S. doi: 10.14219/jada.archive.2006.0396. [DOI] [PubMed] [Google Scholar]
- 13.Güth JF, Almeida E, Silva JS, Beuer FF, Edelhoff D. Enhancing the predictability of complex rehabilitation with a removable CAD/CAM-fabricated long-term provisional prosthesis: A clinical report. J Prosthet Dent. 2012;107:1–6. doi: 10.1016/S0022-3913(11)00171-5. [DOI] [PubMed] [Google Scholar]
- 14.Edelhoff D, Beuer F, Schweiger J, Brix O, Stimmelmayr M, Guth JF. CAD/CAM-generated high-density polymer restorations for the pretreatment of complex cases: A case report. Quintessence Int. 2012;43:457–67. [PubMed] [Google Scholar]
- 15.Rocca GT, Bonnafous F, Rizcalla N, Krejci I. A technique to improve the esthetic aspects of CAD/CAM composite resin restorations. J Prosthet Dent. 2010;104:273–5. doi: 10.1016/S0022-3913(10)60138-2. [DOI] [PubMed] [Google Scholar]
- 16.Lin WS, Harris BT, Ozdemir E, Morton D. Maxillary rehabilitation with a CAD/CAM-fabricated, long-term interim and anatomic contour definitive prosthesis with a digital workflow: A clinical report. J Prosthet Dent. 2013;110:1–7. doi: 10.1016/S0022-3913(13)00127-3. [DOI] [PubMed] [Google Scholar]
- 17.Abduo J, Lyons K, Bennamoun M. Trends in computer-aided manufacturing in prosthodontics: A review of the available streams. Int J Dent 2014. 2014 doi: 10.1155/2014/783948. 783948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiao T, Zhu C, Dong X, Gu X. Rehabilitation of maxillectomy defects with obturator prostheses fabricated using computer-aided design and rapid prototyping: A pilot study. Int J Prosthodont. 2014;27:480–6. doi: 10.11607/ijp.3733. [DOI] [PubMed] [Google Scholar]
- 19.Katase H, Kanazawa M, Inokoshi M, Minakuchi S. Face simulation system for complete dentures by applying rapid prototyping. J Prosthet Dent. 2013;109:353–60. doi: 10.1016/S0022-3913(13)60316-9. [DOI] [PubMed] [Google Scholar]
- 20.Sun J, Zhang FQ. The application of rapid prototyping in prosthodontics. J Prosthodont. 2012;21:641–4. doi: 10.1111/j.1532-849X.2012.00888.x. [DOI] [PubMed] [Google Scholar]
- 21.Soares PV, de Almeida Milito G, Pereira FA, Reis BR, Soares CJ, de Sousa Menezes M, et al. Rapid prototyping and 3D-virtual models for operative dentistry education in Brazil. J Dent Educ. 2013;77:358–63. [PubMed] [Google Scholar]
- 22.Lee JH. Accelerated techniques for a post and core and a crown restoration with intraoral digital scanners and CAD/CAM and rapid prototyping. J Prosthet Dent. 2014;112:1024–9. doi: 10.1016/j.prosdent.2014.04.019. [DOI] [PubMed] [Google Scholar]
- 23.Hazeveld A, Huddleston Slater JJ, Ren Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am J Orthod Dentofacial Orthop. 2014;145:108–15. doi: 10.1016/j.ajodo.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 24.Park JM, Yi TK, Koak JY, Kim SK, Park EJ, Heo SJ. Comparison of five-axis milling and rapid prototyping for implant surgical templates. Int J Oral Maxillofac Implants. 2014;29:374–83. doi: 10.11607/jomi.3265. [DOI] [PubMed] [Google Scholar]
- 25.Eggbeer D, Bibb R, Williams R. The computer-aided design and rapid prototyping fabrication of removable partial denture frameworks. Proc Inst Mech Eng H. 2005;219:195–202. doi: 10.1243/095441105X9372. [DOI] [PubMed] [Google Scholar]
- 26.Bibb RJ, Eggbeer D, Williams RJ, Woodward A. Trial fitting of a removable partial denture framework made using computer-aided design and rapid prototyping techniques. Proc Inst Mech Eng H. 2006;220:793–7. doi: 10.1243/09544119JEIM62. [DOI] [PubMed] [Google Scholar]
- 27.Williams RJ, Bibb R, Eggbeer D, Collis J. Use of CAD/CAM technology to fabricate a removable partial denture framework. J Prosthet Dent. 2006;96:96–9. doi: 10.1016/j.prosdent.2006.05.029. [DOI] [PubMed] [Google Scholar]
- 28.Lee MY, Chang CC, Ku YC. New layer-based imaging and rapid prototyping techniques for computer-aided design and manufacture of custom dental restoration. J Med Eng Technol. 2008;32:83–90. doi: 10.1080/03091900600836642. [DOI] [PubMed] [Google Scholar]
- 29.Bhambhani R, Bhattacharya J, Sen SK. Digitization and its futuristic approach in prosthodontics. J Indian Prosthodont Soc. 2013;13:165–74. doi: 10.1007/s13191-012-0181-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lima JM, Anami LC, Araujo RM, Pavanelli CA. Removable partial dentures: Use of rapid prototyping. J Prosthodont. 2014;23:588–91. doi: 10.1111/jopr.12154. [DOI] [PubMed] [Google Scholar]
- 31.Gujjari AK, Bhatnagar VM, Basavaraju RM. Color stability and flexural strength of poly (methyl methacrylate) and bis-acrylic composite based provisional crown and bridge auto-polymerizing resins exposed to beverages and food dye: An in vitro study. Indian J Dent Res. 2013;24:172–7. doi: 10.4103/0970-9290.116672. [DOI] [PubMed] [Google Scholar]
- 32.Donovan TE, Hurst RG, Campagni WV. Physical properties of acrylic resin polymerized by four different techniques. J Prosthet Dent. 1985;54:522–4. doi: 10.1016/0022-3913(85)90425-1. [DOI] [PubMed] [Google Scholar]
- 33.Gegauff AG, Pryor HG. Fracture toughness of provisional resins for fixed prosthodontics. J Prosthet Dent. 1987;58:23–9. doi: 10.1016/s0022-3913(87)80137-3. [DOI] [PubMed] [Google Scholar]
- 34.Alt V, Hannig M, Wöstmann B, Balkenhol M. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent Mater. 2011;27:339–47. doi: 10.1016/j.dental.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 35.Yanikoğlu ND. Flexural strength of temporary restorative materials stored in different solutions. Open J Stomatol. 2014;4:291–8. [Google Scholar]


