Abstract
Purpose:
To hypothesize a new theory based on soft tissue reference points on lateral profile photographs (LPPs) for determining the vertical dimension of occlusion (VDO), as there is need to explore for simple strategies.
Materials and Methods:
Fifty-three participants in the age range of 20–27 years who met the inclusion criteria were recruited. LPPs were taken for all participants using standard protocol and duplicate copies obtained, on which five soft tissue reference points, nasion (Stn), subnasale (Stsn), porion (Stp), gnathion (Stgn), and gonion (Stg) (Stg prenoted on the face) were marked and joined to form angles; distance between Stsn and Stgn was considered as VDO in LPP (VDO-LP). The angle formed between Stn-Stsn-Stgn and Stn-Stsn-Stg; Stp-Stg-Stgn and Stp-Stg-Stsn was correlated; two simple linear regression models were developed to predict Stn-Stsn-Stgn and Stp-Stg-Stgn using Stn-Stsn-Stg and Stp-Stg-Stsn as independent variables. Using the formulae, VDO-LP predicted was constructed and correlated with the actual values.
Results:
The angle Stn-Stsn-Stgn had a statistically significant moderate positive correlation with Stn-Stsn-Stg (r = 0.57, P < 0.001) and angle Stp-Stg-Stgn, a significant strong positive correlation with Stp-Stg-Stsn (r = 0.81, P < 0.001). Using simple linear regression analysis, the following formulae were obtained: Stn-Stsn-Stgn (in degrees) = 0.776 Stn-Stsn-Stg (in degrees) +79.01 and Stp-Stg-Stgn (in degrees) =1.331 Stp-Stg-Stsn (in degrees) +10.2. The predicted and actual VDO-LP values were in strong positive correlation with a coefficient of 0.8.
Conclusion:
With the use of simple landmarks on LPP, it is possible to reconstruct the lost facial dimensions during prosthetic replacement of lost teeth.
Keywords: Dental occlusion, photography, soft tissue, vertical dimension
INTRODUCTION
Vertical dimension of occlusion (VDO) has been defined as the lower facial height measured between two points when the maxillary and mandibular teeth are intercuspated. Thus, it is the vertical position of the mandible in relation to maxilla when the occluding members are in contact.[1] In our routine practice, to determine the VDO, many measures are employed.[2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17] They include “divine proportions” by Leonardo da Vinci, proportional face measurements such as the distance from eyebrow to ala, eyebrow to hair line, and horizontal distance between the pupils. Determining vertical dimension at rest and positioning VDO to establish 2–3 mm of interocclusal rest space (IRS) may also be utilized. Using profile scales, application of mechanical recording devices in the mouth or on the head, methods based on swallowing, bite force, phonetic assessment of closest speaking space, facial esthetics, preextraction records, intraoral measurements, and those based on cephalometric, telemetric, and magnetic methods are other standard ones. However, since none of these procedures can assure a correct and precise determination of VDO in partially and fully edentulous people, using several methods to reach a conclusion is most commonly practiced currently. Approached differently, when dentists sometimes alter the VDO, and despite considering the factors such as esthetics, occlusal relationship corrections, allowance for restorations, space, and prosthetic convenience, there is a risk of instability following the increase/decrease in VDO.[18,19,20] Altered state of closure (overclosed/open) and sufficiency (insufficient/excessive) can cause clinical consequences such as compromised esthetics, diminished masticatory function, angular cheilitis, altered phonetics, and encroachment of the IRS during speech and pain in the edentulous ridges.[21] Thus, there is a need to explore new strategies to estimate the lost VDO. This study was performed to investigate the application of formulae derived from lateral profile photographs (LPPs) of fully dentulous persons for determining the VDO in partially and totally edentulous patients.
MATERIALS AND METHODS
Ethical clearance for the study was obtained from the Institutional Ethical Committee. The inclusion criteria for the selection of participants were age range of 20–27 years with full complement of teeth, well-balanced face, Class I skeletal, molar and canine relationship, and no acute or previous temporomandibular disorder. Individuals who were orthodontically treated previously and those with facial asymmetries were excluded from the study.
Lateral profile photography
Lateral profiles of all the recruited participants were made following standards of extraoral photography.[22] Participants were instructed to stand straight with their head in a natural position, looking into the mirror hung on the wall at their eye level. After confirming that the line drawn from the outer canthus of the eye and upper edge of the ear was parallel to the floor, photographs were taken from a distance of 5 feet.
Soft tissue reference points
Figure 1 displays points considered in this study:
Figure 1.
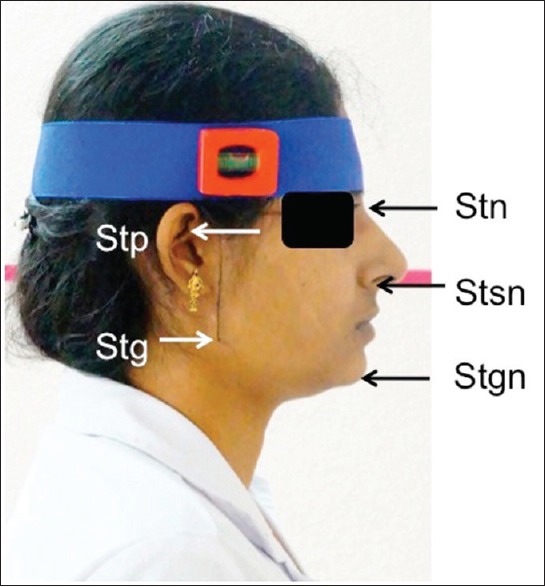
Lateral profile photograph of participant with five reference points
Skin nasion (Stn): The deepest point in the concavity formed in the frontonasal region
Skin subnasale (Stsn): The point where the lowest border of the nose meets the outer contour of the upper lip
Point corresponding to porion (Stp): The most superiorly positioned point on the external opening of the auditory meatus
Gonion (Stg): A point on the curvature of the angle of the mandible formed by the posterior ramus and the inferior border of the mandible
Skin gnathion (Stgn): The point where the anterior curve in the outline of the chin merges into the body of the mandible.
Procedure
To mark the point Stg correctly on the mobile soft tissue, a line connecting the outer canthus of the eye and upper edge of the ear was drawn. The gonion was palpated by the left-hand thumb. Without leaving the finger from the face, a perpendicular line was drawn using a set square from the line drawn on the face half way to the tip of the thumb and was extended to the lower border of the mandible after leaving the finger. The standardized LPP was made when the participants were in occlusion and duplicates obtained on which all the above-mentioned soft tissue reference points were marked. Figure 2 shows how those points were joined so as to form the following angles:
Figure 2.
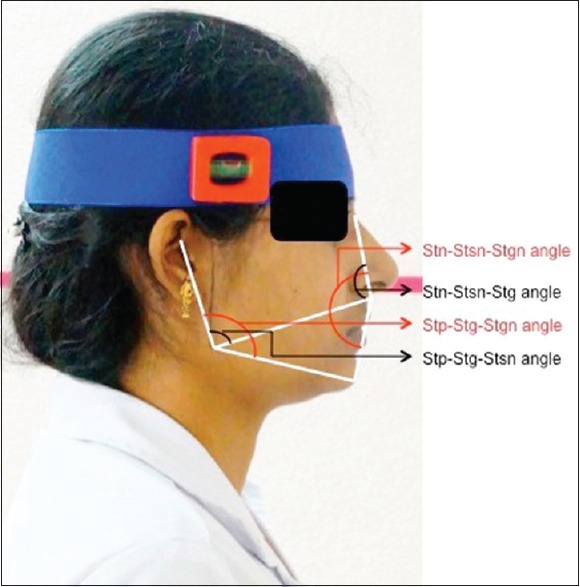
Lateral profile photograph with four angles formed with the reference points
Stn-Stsn-Stgn angle: Formed by joining soft tissue landmarks nasion, subnasale, and gnathion
Stn-Stsn-Stg angle: Formed by joining soft tissue landmarks nasion, subnasale, and gonion
Stp-Stg-Stgn angle: Formed by joining soft tissue landmarks porion, gonion, and gnathion
Stp-Stg-Stsn angle: Formed by joining soft tissue landmarks porion, gonion, and subnasale.
Vertical dimension of occlusion determination on lateral photographs
For all the LPPs, the distance between the two marked points, Stsn and Stgn, was measured as VDO-LP.
Sample size determination
Based on the findings of our pilot study done on 10 potential participants (not included in the main study), with the level of significance set at 0.05, power of 80%, a minimal sample size of 28 was determined.
Reproducibility of angles and vertical dimension of occlusion-lateral photograph in lateral profile photographs
For the above 10 participants, LPPs were made by two investigators (DV and KK) on two occasions following the same procedure described in Figure 2. The angles and VDO-LP were measured on the duplicates obtained and tested for intra- and inter-rater reliabilities (cite reliability coefficients).
Statistical analysis
All statistical analyses were performed using SPSS 17.0 software (version 17.0, SPSS, Chicago, IL, USA). Cohen's kappa was employed to measure the reliability of the obtained data (both intra- and inter-rater). The normality of the data was tested using Shapiro–Wilk test. The correlations between the angles, Stn-Stsn-Stg and Stn-Stsn-Stgn; Stp-Stg-Stsn and Stp-Stg-Stgn were determined using Pearson correlation test. For predicting Stn-Stsn-Stgn and Stp-Stg-Stgn angles from Stn-Stsn-Stg and Stp-Stg-Stsn, respectively, simple linear regression analysis was carried out. The predicted angles were transferred on to the LPP and VDO constructed on the photograph. The actual and predicted VDO-LP values were again correlated using Pearson correlation test.
RESULTS
Descriptive analysis
A total of 53 participants were recruited. The mean age of the participants was 22.4 (range of 20–27 years). The mean values for Stn-Stsn-Stgn and Stn-Stsn-Stg were 160.4 ± 5.03 (range from 149 to 170) and 104.8 ± 3.7 (range from 98 to 115), respectively. The mean values for the Stp-Stg-Stgn and Stp-Stg-Stsn angles were 129.13 ± 6.74 (range from 114 to 147) and 89.3 ± 4.08 (range from 80 to 103), respectively. The mean VDO-LP was 38.43 ± 3.52 with a range between 32 and 45 mm.
Correlations
The intra- and inter-rater reliabilities of the lateral profile analysis (determination of angles and VDO) were found to be 0.98 and 0.97, respectively. The correlation (r) between the Stn-Stsn-Stgn and Stn-Stsn-Stg angles was statistically significant and moderately positive (r = 0.57, P < 0.001***) with a determination coefficient (r2) of 0.32 [Figure 3]. The correlation between Stp-Stg-Stgn and Stp-Stg-Stsn was statistically strong and positive (r = 0.81, P < 0.001***), with a determination coefficient of r2 = 0.65 [Figure 4]. Linear regression equations to predict Stn-Stsn-Stgn and Stp-Stg-Stgn were determined using Stn-Stsn-Stg and Stp-Stg-Stsn angles as predictors. The equations determined were calculated as, y = a + bx, where y is the dependent variable, Stn-Stsn-Stgn/Stp-Stg-Stgn, x is the independent variable, Stn-Stsn-Stg/Stp-Stg-Stsn, a is the y-intercept, and b is the slope of regression. By calculation for the prediction of Stn-Stsn-Stgn, the equation was y = 0.776x + 79.01; Stn-Stsn-Stgn (in degrees) = 0.776 Stn-Stsn-Stg (in degrees) +79.01. For the prediction of Stp-Stg-Stgn, the equation was y = 1.331x + 10.2; Stp-Stg-Stgn (in degrees) =1.331 Stp-Stg-Stsn (in degrees) +10.2. Applying these new equations, the Stn-Stsn-Stgn and Stp-Stg-Stgn were predicted and transferred on to the LP, as shown in Figure 5, to predict VDO-LP (VDO on the LP using predicted angles). The predicted and actual VDO-LP for all the participants were again correlated which gave a strong positive correlation coefficient of 0.8 (r2 = 0.64).
Figure 3.
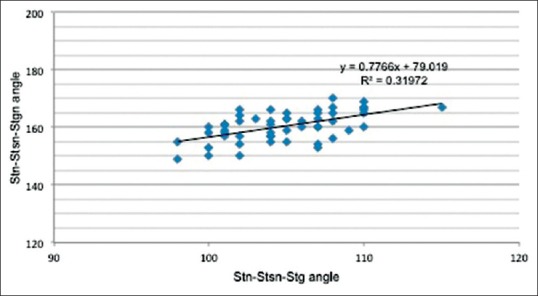
Correlation of Stn-Stsn-Stg and Stn-Stsn-Stgn angles
Figure 4.
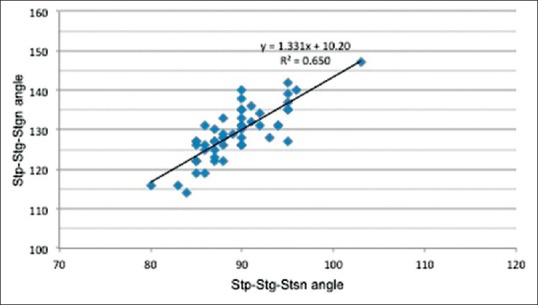
Correlation of Stp-Stg-Stsn and Stp-Stg-Stgn angles
Figure 5.
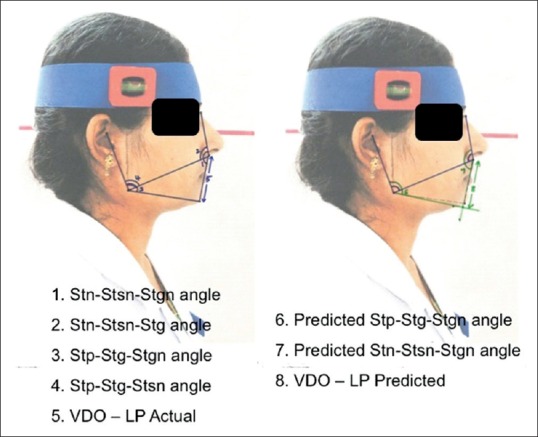
Scanned copy of lateral profile photograph showing prediction of vertical dimension of occlusion
DISCUSSION
The VDO is a range, better described as the comfort zone, which leads to the best harmony of the musculoskeletal determinants. It is the result of musculoskeletal balance during growth; the muscle organization clearly related to the skeletal morphology which influences the facial morphology. Thus, anatomic features, physiologic needs, craniofacial growth, neuromuscular control, and environmental factors together play a role in establishing VDO.[4,11] The accurate determination of VDO forms a critical part of recording the jaw relation and the preciseness in estimating the lost dimension can give an idea for the practitioner to understand the direction of treatment. Many methods to determine the lost VDO that depend on either muscular activity or the skeletal morphology are reported in the literature.[2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17] However, as the facial morphology is easier and simpler to assess than these methods, this study was planned to correlate the facial angles formed by joining five landmarks, to predict one from another so as to calculate the VDO.
The clinical consequences frequently proposed when VDO is not properly recorded are compromised esthetics resulting from changes in facial appearance, diminished masticatory function, altered phonetics, and pain at the teeth or edentulous ridges. In addition, some patients describe a feeling of not having space in their mouth, a sensation akin to “oral claustrophobia.”[21] Thus, reestablishment of height is important as this significantly compromises function, facial aesthetics, and stomatognathic system which affect the patient's quality of life.[14]
The old pioneering method described by Niswonger, determination of VDO by evaluating IRS, is still in usage though debated by many, whereas mechanical recording devices placed on the mouth or on the head cause the mandibular muscles to be tensed which can bias the recordings. Then, cephalometrics has been the trend with attempts to propose efficient method since it uses specific and predetermined points of bone.[11,12,13,14,16,17] Although there are many studies on cephalometrics, there are variations among them, which can be ascribed not only for individual variations but also to picture deformations, superposition of structures, and inaccuracy of tracing.[11] In spite of imperfections with cephalometrics, this method was further studied with the hope that this additionally helps the practitioner to understand the direction of treatment concerning the lower facial height in occlusion. Trial to frame regression equations, using cephalometrics, found this more interesting and specifically related to the patient.[16] However, simple regressions were not so accurate when compared to the multiple linear regressions. Thus, the intention of this study was to go for a simpler method by the usage of certain landmarks in cephalometrics which can also be marked on the LPP, so as to attempt easy prediction of lost dimensions. The present study findings contradicted the misconception that the reference points on soft tissue are unstable and cannot be defined. It also proved that simple regressions were able to predict the VDO using facial angles on the photographs, thus avoiding complex multiple regression equations.
Directly studying a new method on edentulous patients will have the limitation of lacking a real standard against which to compare the results. Hence, this study was planned on dentulous subjects so as to apply those formulae for the edentulous patients in the contemporary population. In edentulous condition, among the five reference points considered, only one landmark, Stgn, will be missing which can be constructed at the intersection of the two predicted angles Stp-Stg-Stgn and Stn-Stsn-Stgn. The distance between Stn to Stsn clinically (VDO clinically) can be calculated by using the formula X1/X2 = Y1/Y2; X1 = Y1/Y2 × X2, where X1 is the distance between Stsn and Stgn and X2 is the distance between Stn and Stsn clinically, whereas Y1 is the distance between Stsn and Stgn, Y2 is the distance between Stn and Stsn on LPP.
The major drawback of this study is that the sample consisted mostly of females, and another being the applicability of the present findings to other ethnic groups which demand further studies based on the same methodology in different populations. This study facilitated determination of the lower facial height, aiding in the construction of full or partial prosthesis, and those with extensive prosthetic rehabilitation. The formulae obtained in this study can be further studied by applying them for edentulous patients, so as to know the clinical applicability of the derived formulae. Developing software to calculate the dimensions directly in computer can also be a futuristic trend.
CONCLUSION
As revealed in this study, with the use of four simple reference landmarks on an LPP, it is possible to construct a fifth point and construct the lost facial dimensions easily. This method based on photographs is easy, clinically feasible, cost-effective, and avoids common problems with cephalograms. Thus, profile photographs can be a viable alternative for the determination of VDO during prosthetic replacements.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.The glossary of prosthodontic terms. J Prosthet Dent. 2005;94:10–92. doi: 10.1016/j.prosdent.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 2.Sakar O, Sülün T, Kurt H, Gençel B. Reliability and comparison of two facial measurements to detect changes of occlusal vertical dimension in complete denture wearers. Gerodontology. 2011;28:205–8. doi: 10.1111/j.1741-2358.2009.00353.x. [DOI] [PubMed] [Google Scholar]
- 3.Rizzatti A, Ceruti P, Mussano F, Erovigni F, Preti G. A new clinical method for evaluating the closest speaking space in dentulous and edentulous subjects: A pilot study. Int J Prosthodont. 2007;20:259–62. [PubMed] [Google Scholar]
- 4.LoSchiavo M, Madhav S, Whyman R. Determination of vertical dimension by hydraulic intraoral jack. J Oral Rehabil. 1988;15:393–9. doi: 10.1111/j.1365-2842.1988.tb00174.x. [DOI] [PubMed] [Google Scholar]
- 5.Millet C, Jeannin C, Vincent B, Malquarti G. Report on the determination of occlusal vertical dimension and centric relation using swallowing in edentulous patients. J Oral Rehabil. 2003;30:1118–22. doi: 10.1046/j.1365-2842.2003.01201.x. [DOI] [PubMed] [Google Scholar]
- 6.Nagpal A, Parkash H, Bhargava A, Chittaranjan B. Reliability of different facial measurements for determination of vertical dimension of occlusion in edentulous using accepted facial dimensions recorded from dentulous subjects. J Indian Prosthodont Soc. 2014;14:233–42. doi: 10.1007/s13191-013-0315-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chawla C, Parkash H, Duggal R. Facial measurements as a means of determination of vertical dimension. J Indian Prosthodont Soc. 2000;11:33–41. [Google Scholar]
- 8.Sheppard IM, Sheppard SM. Classic article – Vertical dimension measurements. J Prosthet Dent. 2006;95:175–80. doi: 10.1016/j.prosdent.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 9.Burnett CA, Clifford TJ. Closest speaking space during the production of sibilant sounds and its value in establishing the vertical dimension of occlusion. J Dent Res. 1993;72:964–7. doi: 10.1177/00220345930720061201. [DOI] [PubMed] [Google Scholar]
- 10.Bissasu M. Pre-extraction records for complete denture fabrication: A literature review. J Prosthet Dent. 2004;91:55–8. doi: 10.1016/j.prosdent.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Orthlieb JD, Laurent M, Laplanche O. Cephalometric estimation of vertical dimension of occlusion. J Oral Rehabil. 2000;27:802–7. doi: 10.1046/j.1365-2842.2000.00592.x. [DOI] [PubMed] [Google Scholar]
- 12.Brzoza D, Barrera N, Contasti G, Hernández A. Predicting vertical dimension with cephalograms, for edentulous patients. Gerodontology. 2005;22:98–103. doi: 10.1111/j.1741-2358.2005.00060.x. [DOI] [PubMed] [Google Scholar]
- 13.Strajnic L, Stanisic-Sinobad D, Markovic D, Stojanovic L. Cephalometric indicators of the vertical dimension of occlusion. Coll Antropol. 2008;32:535–41. [PubMed] [Google Scholar]
- 14.Tavano KT, Seraidarian PI, de Oliveira DD, Jansen WC. Determination of vertical dimension of occlusion in dentate patients by cephalometric analysis – Pilot study. Gerodontology. 2012;29:e297–305. doi: 10.1111/j.1741-2358.2011.00469.x. [DOI] [PubMed] [Google Scholar]
- 15.Ladda R, Bhandari AJ, Kasat VO, Angadi GS. A new technique to determine vertical dimension of occlusion from anthropometric measurements of fingers. Indian J Dent Res. 2013;24:316–20. doi: 10.4103/0970-9290.117993. [DOI] [PubMed] [Google Scholar]
- 16.Yamashita S, Shimizu M, Katada H. A Newly Proposed Method to Predict Optimum Occlusal Vertical Dimension. J Prosthodont. 2015;24:287–90. doi: 10.1111/jopr.12223. [DOI] [PubMed] [Google Scholar]
- 17.Zielak JC, Gulin Neto D, da Cunha LF, Deliberador TM, Giovanini AF. Cephalometric approach to the occlusal vertical dimension reestablishment. Case Rep Dent 2014. 2014 doi: 10.1155/2014/920840. 920840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kois JC, Phillips KM. Occlusal vertical dimension: Alteration concerns. Compend Contin Educ Dent. 1997;18:1169–74. 1176-7. [PubMed] [Google Scholar]
- 19.Abduo J, Lyons K. Clinical considerations for increasing occlusal vertical dimension: A review. Aust Dent J. 2012;57:2–10. doi: 10.1111/j.1834-7819.2011.01640.x. [DOI] [PubMed] [Google Scholar]
- 20.Gross MD, Nissan J, Ormianer Z, Dvori S, Shifman A. The effect of increasing occlusal vertical dimension on face height. Int J Prosthodont. 2002;15:353–7. [PubMed] [Google Scholar]
- 21.Koka S. Vertical dimension of occlusion. Int J Prosthodont. 2007;20:342. [PubMed] [Google Scholar]
- 22.Anic-Milosevic S, Slaj M, Lapter-Varga M. Basic principles for taking extraoral photographs. Acta Stomatol Croat. 2005;39:201–4. [Google Scholar]


