Abstract
Background:
Regional anesthesia using paravertebral block has been suggested as an ideal adjunct to general anesthesia for modified radical mastectomy. Paravertebral block is an effective management of peri-operative pain for Modified radical mastectomy, however, there are no established guidelines regarding what is the most suitable strategy when varying drugs and dosages between different groups.
Aim:
To evaluate the effectiveness of paravertebral block comparing the most frequently employed drugs in this procedure (bupivacaine vs ropivacaine).
Study Design:
Prospective randomized double blind study.
Methods:
A total 70 ASA I and II adult female patients undergoing Modified radical mastectomy under paravertebral block followed by general anesthesia were randomly divided into two groups. The first group was administered 0.375% Ropivacaine in a dose 0.25 ml /kg in paravertebral block. The second group was administered bupivacaine 0.375% in dose 0.25 ml /kg in paravertebral block. Standard induction technique followed. Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), were recorded pre block, post block 5 min, post block 10 min, at skin incision, post skin incision initially at 5 interval for first 15 min till one hour, and every 30 min till end of surgery. Post-operative visual analogue score for pain was recorded at 1 hr, 6 hr and 24 hr.
Statistical Analysis:
Chi-square test (Fisher's exact test) for qualitative variables. Independent sample t-test for quantitative data.
Results:
Ropivacaine and Bupivacaine had no difference in intraoperative analgesia as shown by intraoperative hemodynamic parameters. Bupivacaine got better post-operative VAS scores (P < 0.05) in mean and after first, 6 h and 24 h.
Keywords: Breast cancer, bupivacaine, modified radical mastectomy, paravertebral block, ropivacaine
INTRODUCTION
Advancement in diagnostic science has led to an increased frequency in the detection of cases of breast cancer. After diagnostic confirmation, the majority of these patients undergo definitive surgery, most commonly modified radical mastectomy (MRM) or lumpectomy with axillary dissection.
General anesthesia (GA) is currently the standard technique used for surgical treatment of breast cancer. GA alone cannot achieve adequate postoperative pain control.[1] Regional anesthesia using thoracic paravertebral block (TPVB) is an ideal alternative to GA for breast cancer surgery. Benefits include a prolonged postoperative pain relief, potential for early discharge and reduction in postoperative nausea and vomiting (PONV).[2]
TPVB provides superior analgesia for breast cancer surgery when used in conjunction with GA and reduces the severity of chronic pain after mastectomy.[3,4] In a study, continuous TPVB provides effective pain relief, significant opioid sparing, and also causes less painful restricted movement of the shoulder with very few side effects after breast cancer surgery.[5] The use of TPVB in breast surgery improves analgesia for up to 72 postoperative hours at rest and during movement and may reduce chronic postsurgical pain at 6 months.[6]
In another study, a paravertebral analgesia-based anesthetic reduced pain scores and opioid requirements and also reduced the doses of volatile anesthetics. Meta-analysis concluded that pain is reduced by about two points (on a 0–10 visual analog scale [VAS] score) and that opioid use is reduced by about 70% in the immediate postoperative 2 h.[7]
The aim of our study was to assess the efficacy of analgesia in TPVB with 0.375% ropivacaine and 0.375% bupivacaine to control postsurgical pain in women undergoing MRM.
MATERIALS AND METHODS
This prospective randomized study was carried out in seventy patients between the age of 18–60 years belonging to the American Society of Anesthesiologists (ASA) physical status I and II scheduled for MRM. The study was conducted during October 2014–December 2015 after obtaining approval from the Institute Ethics Committee. This trial was registered by the Central Trial Registry of India (www.ctri.nic.in) having the registration number CTRI/2015/01/008197. A written informed consent was obtained from all the patients before the day of surgery.
Sample size estimation
A sample size of 28 in each group was sufficient to depict a clinical difference of 1.5 points on the mean VAS assuming a standard deviation of 2 points, using two-tailed difference between mean VAS, a power of 80%, and a significance level of 5%. This was based on the assumption that the measurement of VAS is normally distributed. This number had been increased to 35 per group (total 70) to allow for a predicted dropout or withdrawal from the procedure of nearly 20%. Patients were randomly allocated by computer-generated random number into two groups:
Group 1 (n = 35) - Ropivacaine, 0.375% (0.25 mL/kg)
Group 2 (n = 35) - Bupivacaine, 0.375% (0.25 mL/kg)
Patients aged between 18 and 60 years, physical status ASA I and ASA II diagnosed breast cancer scheduled for MRM were included in the study. Patients with pre-existing respiratory diseases such as obstructive pulmonary disease, co-existing cardiovascular diseases, infection at the injection site, severe obesity (body mass index >35 kg/m2), psychiatric disorders, history of allergy, and bleeding diathesis were excluded from the study.
Patients were premedicated with alprazolam 0.25 mg on the night before and 2 h before the surgery. In the operation room, intravenous access was established and standard monitors were attached. Paravertebral block (PVB) was performed with patient sitting. Puncture site was cleaned and painted with antiseptic solution. A point 2.5 cm lateral to the midline was taken. The transverse process lies deep to the mark. The needle insertion point was infiltrated with local anesthetic. Tuohy's needle (18-gauge) was inserted perpendicular to the skin to contact transverse process at 2–4 cm depth. Then, the needle was manipulated to walk off the superior or inferior aspect of the transverse process, until loss of resistance to air could be elicited. Insertion was limited to <2 cm past the transverse process. Loss of resistance to the injection of air indicating that the needle tip had traversed the superior costo-transverse ligament into paravertebral space. After negative aspiration, local anesthetic 0 mL/kg was injected slowly over 2–3 min.
The drugs were prepared by an independent clinician not involved in the study. The anesthesiologist performing the block and observing the patient was blinded to the treatment group. Neither the patient nor the attending anesthesiologist who also collected the data was aware of the group allocation. Then, we waited for 5–10 min and accessed the block. A spirit-soaked swab was touched in the respective dermatomes and the patient was asked to count one, two, and three whenever she felt the cold sensation with eyes closed. If the block failed, the case was excluded from the study, but the failure rate was noted.
Then, the GA was induced with fentanyl 2 µg/kg and propofol 2–3 mg/kg followed by atracurium 0.5 mg/kg to facilitate the insertion of endotracheal tube of appropriate size. GA was maintained with isoflurane in 50% oxygen in 50% N2O, inhaled oxygen, end-tidal isoflurane, and carbon dioxide concentrations were monitored.
The data were collected by a third person who was not aware of the randomization. Baseline heart rate, systolic blood pressure (BP), diastolic BP, and SpO2 were recorded; then, preblock, postblock 5 min, postblock 10 min, at skin incision, postskin incision initially at 5 min interval for the first 15 min, then for every 15 min till 1 h, and every 30 min till the end of the surgery.
Heart rate and arterial BP were maintained within ± 20% of preoperative baseline. Boluses of injection fentanyl µg/kg intravenously were given if the heart rate and BP increased more than 20% of the baseline value. At the end of the surgery, residual neuromuscular blockade was antagonized with a mixture of neostigmine (2.5 mg) and glycopyrrolate (0.5 mg). The patient was transferred to postoperative recovery room.
Vitals and pain scores were noted at the end of 1, 6, and 24 h following reversal from GA. Postoperative analgesia was managed with intravenous infusion diclofenac 75 mg twice daily and paracetamol 1 g eight hourly. Rescue analgesia was provided with tramadol 50 mg in slow infusion with 100 ml of normal saline. Antiemetic ondansetron 4–8 mg was administered for nausea and vomiting. Incidence of any nausea or vomiting was noted in the first 24 h.
Statistical analysis
Descriptive statistics was used to describe the baseline characteristics. Dichotomous outcomes were compared by Fisher's exact test as applicable. Numerical data were expressed as mean and standard deviation. Qualitative data were expressed as frequency and percentage. Chi-square test (Fisher's exact test) was used to examine the relation between qualitative variables. For quantitative data, comparison between two groups was done using independent sample t-test. Comparison of repeated measures was done using ANOVA test for repeated measures. P <0.05 was considered significant. Analysis was the intention-to-treat, i.e., all patients who were randomized were included in the analysis, irrespective of the degree of compliance. Analysis was performed using SPSS software version 20.0 (IBM, SPSS-20 used for statistical analysis).
OBSERVATION AND RESULTS
The patients who accepted for the study were in the age group of 18–60 years. Both the groups were compared for significance in the difference of age distribution. The demographic data in both groups did not show any statistically significant difference [Table 1 and Figures 1–4].
Table 1.
Demographic data of patients in two groups
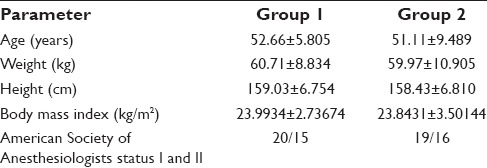
Figure 1.
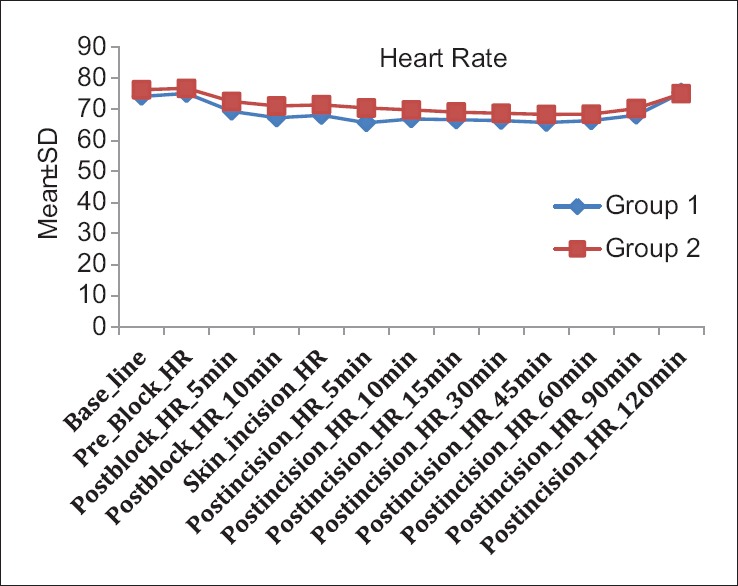
Comparison of heart rate. SD = Standard deviation, HR = Heart rate
Figure 4.
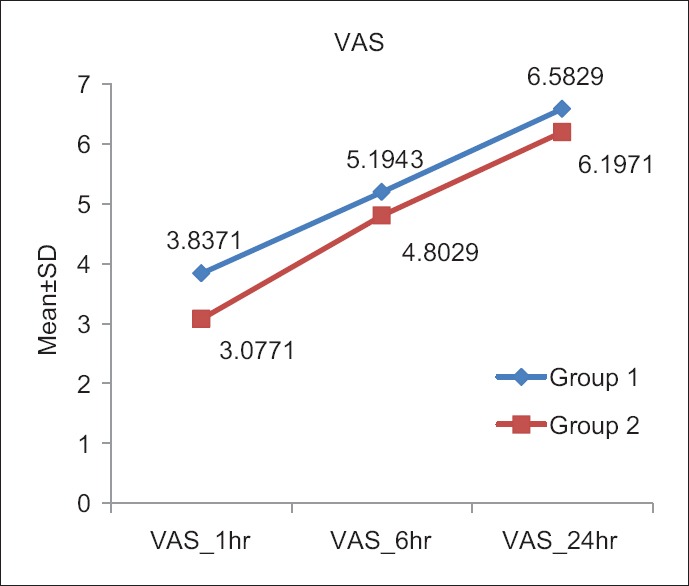
Comparison of visual analog scale score. VAS = Visual analog scale, SD = Standard deviation
Figure 2.
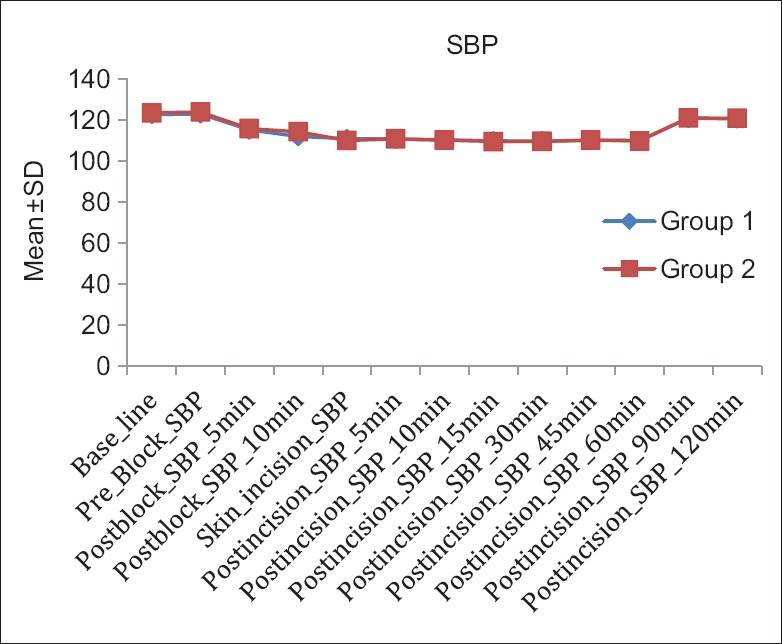
Comparison of systolic blood pressure. SBP = Systolic blood pressure, SD = Standard deviation
Figure 3.
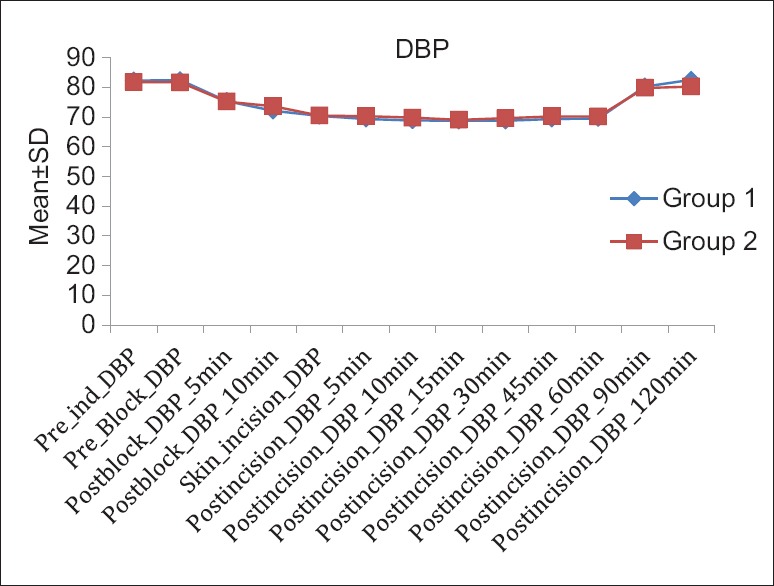
Comparison of diastolic blood pressure. DBP = Diastolic blood pressure, SD = Standard deviation
Both techniques provided acceptable postoperative analgesia as shown by the pain scores. Bupivacaine group got lower mean VAS value with a statistically significant difference, P = 0.006 (<0.05). Data was statistically significant difference between VAS 1, 6, and 24 h. Initial VAS scores were low in both the groups (3.8/3.07) with a peak of pain in 24 h (6.58/6.19). Eleven patients required tramadol as rescue drug (six with ropivacaine and five with bupivacaine), there were no differences in the requirements for rescue analgesia between the two groups (P > 0.05). There were no complications attributable to postoperative pain.
DISCUSSION
MRM produces severe discomfort and chronic pain syndrome that depend on the quality of pain relief. Appropriate analgesia can reduce this pain-related morbidity.
Bansal et al. observed PVB with GA which is associated with better postoperative analgesia, lower incidence of PONV, and better alertness score compared to GA with local infiltration.[8]
Kundra et al. concluded that lung functions are well preserved in patients undergoing MRM under GA supplemented with paravertebral or interpleural block which is as effective as PVB for postoperative pain relief. PVB has the added advantage of achieving a more complete block.[9]
Pusch et al. described a single injection of a high volume of bupivacaine into the thoracic paravertebral space and reported effective anesthesia for breast lump excisions as well as mastectomies with axillary clearance.[10]
The use of ropivacaine as a single injection into the TPVBs is increasingly being chosen. This local anesthetic agent has shown to be equally effective but less toxic than bupivacaine. Following accidental intravascular injection of bupivacaine during the induction of regional anesthesia, sudden cardiovascular collapse may result. The resultant malignant arrhythmia and ventricular fibrillation could be resistant to treatment with fatal consequence. On the other hand, clinical experience with ropivacaine showed that accidental intravenous administration resulted primarily in central nervous system complications that were easily treatable with minimal incidence of cardiac toxicity.
Greengrass et al. found that the average dose of 0.31 mL/kg of ropivacaine 1% injected into the paravertebral space at the T5 level elicited a spread of seven dermatomes.
The spread of ropivacaine as a single injection has not been previously evaluated. The spread of local anesthetic agent from the paravertebral space is known to be variable. Injected agents can extend laterally, superio-inferiorly, and even medially. Radiological studies examining the spread of single injections of radio-opaque dye into the thoracic paravertebral space showed two distinct patterns of distribution. These were classified as longitudinal and cloud-like distributions. A strong correlation between the volume of injection and the number of covered segments for the longitudinal group was reported (0.25 mL/kg) of the agent covering an average of six segments.[11]
PVB was observed as an effective method for post-MRM pain control. We decided to evaluate the most frequently employed local anesthetic (bupivacaine) with the more recently implanted anesthetic (ropivacaine) in two groups with single-shot PVB in patients undergoing MRM.
In our study, we have used 0.25 mL/kg of both drugs in T4 level and elicited a spread of average six dermatomes in both the groups with no significant difference.
Compared with bupivacaine, ropivacaine produces a greater sensorimotor differential block with the benefit of a shorter elimination half-life, with a possibly lower potential for accumulation. The risk of toxicity with ropivacaine is lower than that with bupivacaine.
Because of concerns of this potential bupivacaine toxicity, clinicians have turned to propose ropivacaine for TPVB as a safer option.
Clinical studies suggest that ropivacaine has a block profile very similar to that of bupivacaine, but with a marginal shorter duration when used for major peripheral and epidural block. In addition, the epidural studies also suggest that the degree of motor block produced by similar concentration is compared so that it may be possible to achieve a more consistent separation between sensory and motor block when the agent is used for pain relief.[12]
It is a fact that higher levels of block are obtained at an increasing concentration of anesthetic. On the other hand, a higher volume of anesthetic is supposed to block more intercostal nerves, compensating a lower concentration. Lower concentration is supposed to produce a more differential block with more sensory.
In our study, hemodynamic parameters remained stable at all times in most of the patients both intraoperatively and postoperatively. Five episodes of hypotension were reported in the study, of which two episodes were seen with ropivacaine and three episodes with bupivacaine. There was no intraoperative requirement of rescue analgesia (fentanyl). Cardiovascular changes were similar in both ropivacaine and bupivacaine groups with no significant difference.
These results are in accordance with the previous studies by McGlade et al. where they found that cardiovascular changes were similar in ropivacaine and bupivacaine in lumbar epidural for lower limb orthopedic surgery.[13]
Wood and Rubin compared epidural 1% ropivacaine and 0.75% bupivacaine for lower abdominal gynecological surgery and found that cardiovascular changes are similar for both drugs.[14]
Regarding the need for rescue analgesia in postoperative period, both analgesics obtained similar results. However, mean VAS score value with bupivacaine was better than those of ropivacaine (P < 0.05) as also seen after 1, 6, and 24 h postoperatively [Figure 4]. The differences are small, but show the importance of duration of action. Bupivacaine is longer acting than ropivacaine.
In our results, first-hour values were significantly lower (3.83/3.07) in comparison to post 6 h values (5.19/4.80) which could be explained because of the accumulation of residual analgesic given during the surgery.
After 6 h surgery, the mean VAS score for bupivacaine is 4.80 compared to mean VAS of 5.19 ropivacaine with statistical significance difference. That could be explained by longer duration of action of bupivacaine.
Fibla et al. compared PVB with bupivacaine 0.5% versus ropivacaine 0.2% in postoperative thoracotomy and found that both provided acceptable postoperative analgesia as shown by pain score. Bupivacaine group got lower mean VAS value with a statistically significant difference.[15]
Brown et al. compared 0.5% ropivacaine and 0.5% bupivacaine for epidural anesthesia in patients undergoing lower extremity surgery and found 0.5% ropivacaine and bupivacaine to be clinically similar in both sensory and motor blocking characteristic, with the exception that bupivacaine produced a blockade of slightly longer duration.[16]
Brockway et al. compared extradural ropivacaine and bupivacaine and found that ropivacaine produced shorter duration of block than bupivacaine.[17]
Tuttle et al. compared abdominal relaxation produced by epidural 0.75% ropivacaine and 0.75% bupivacaine in gynecological surgery and found that sensory block by ropivacaine is shorter than bupivacaine. Almost 1.4% of the patients had vomiting in Group 1 as compared to 1.05% in Group 2. Two patients (0.7%) had respiratory depression in each group while no cases of shivering were reported in both the groups.[18]
Regarding literature, TPVB is mainly performed by continuous infusion of the anesthetic. In our management, we employed bolus. We believe that this facilitates postoperative management of the patients. In our institute, post-MRM patients are managed in the ward. And, an important part of the feasibility of this policy is the multimodal pain approach.
We believe that TPVB bolus facilitates postoperative care, and monitoring is simplified. Consequently, this policy could be more suitably adapted to patients in surgical wards avoiding highly monitored Intensive Care Unit. The multimodal treatment including the TPVB alternated with intravenous fentanyl intraoperatively and tramadol postoperatively as rescue drug provides effective analgesia after MRM surgery.
There are recent interests in the utilization of ultrasound technologies in thoracic paravertebral punctures. Pace et al. conducted a retrospective study on the routine use of a single injection and transverse in-plane ultrasound-guided technique for TPVB in patients undergoing mastectomy with immediate breast reconstruction which is associated with very few complications.[19]
CONCLUSION
Based on the findings of our study, we can arrive at the conclusion that patients received satisfactory perioperative analgesia with single-shot PVB. Ropivacaine and bupivacaine had no difference in intraoperative analgesia as shown by intraoperative hemodynamic parameters.
Bupivacaine got better postoperative VAS scores (P < 0.05) in mean and after 1, 6, and 24 h, however the two groups had no difference in the requirement for rescue analgesia. No toxicity was observed. Higher concentrations and volumes of local anesthetics could be used to obtain better VAS scores.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cohen AM, Schaeffer N, Chen ZY, Wood WC. Early discharge after modified radical mastectomy. Am J Surg. 1986;151:465–6. doi: 10.1016/0002-9610(86)90104-2. [DOI] [PubMed] [Google Scholar]
- 2.Richardson J, Sabanathan S. Thoracic paravertebral analgesia. Acta Anaesthesiol Scand. 1995;39:1005–15. doi: 10.1111/j.1399-6576.1995.tb04219.x. [DOI] [PubMed] [Google Scholar]
- 3.Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: A meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105:842–52. doi: 10.1093/bja/aeq265. [DOI] [PubMed] [Google Scholar]
- 4.Karmakar MK, Samy W, Li JW, Lee A, Chan WC, Chen PP, et al. Thoracic paravertebral block and its effects on chronic pain and health-related quality of life after modified radical mastectomy. Reg Anesth Pain Med. 2014;39:289–98. doi: 10.1097/AAP.0000000000000113. [DOI] [PubMed] [Google Scholar]
- 5.Abdel-Halim JM. Continuous thoracic paravertebral block: An adjunct to general anaesthesia in major breast surgery. Egypt J Anaesth. 2011;27:83–7. [Google Scholar]
- 6.Terkawi AS, Tsang S, Sessler DI, Terkawi RS, Nunemaker MS, Durieux ME, et al. Improving analgesic efficacy and safety of thoracic paravertebral block for breast surgery: A mixed-effects meta-analysis. Pain Physician. 2015;18:E757–80. [PubMed] [Google Scholar]
- 7.Wu J, Buggy D, Fleischmann E, Parra-Sanchez I, Treschan T, Kurz A, et al. Thoracic paravertebral regional anesthesia improves analgesia after breast cancer surgery: A randomized controlled multicentre clinical trial. Can J Anaesth. 2015;62:241–51. doi: 10.1007/s12630-014-0285-8. [DOI] [PubMed] [Google Scholar]
- 8.Bansal P, Saxena KN, Taneja B, Sareen B. A comparative randomized study of paravertebral block versus wound infiltration of bupivacaine in modified radical mastectomy. J Anaesthesiol Clin Pharmacol. 2012;28:76–80. doi: 10.4103/0970-9185.92449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kundra P, Varadharajan R, Yuvaraj K, Vinayagam S. Comparison of paravertebral and interpleural block in patients undergoing modified radical mastectomy. J Anaesthesiol Clin Pharmacol. 2013;29:459–64. doi: 10.4103/0970-9185.119133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pusch F, Freitag H, Weinstabl C, Obwegeser R, Huber E, Wildling E. Single-injection paravertebral block compared to general anaesthesia in breast surgery. Acta Anaesthesiol Scand. 1999;43:770–4. doi: 10.1034/j.1399-6576.1999.430714.x. [DOI] [PubMed] [Google Scholar]
- 11.Greengrass R, O’Brien F, Lyerly K, Hardman D, Gleason D, D’Ercole F, et al. Paravertebral block for breast cancer surgery. Can J Anaesth. 1996;43:858–61. doi: 10.1007/BF03013039. [DOI] [PubMed] [Google Scholar]
- 12.Hickey R, Hoffman J, Ramamurthy S. A comparison of ropivacaine 0.5% and bupivacaine 0.5% for brachial plexus block. Anesthesiology. 1991;74:639–42. doi: 10.1097/00000542-199104000-00002. [DOI] [PubMed] [Google Scholar]
- 13.McGlade DP, Kalpokas MV, Mooney PH, Buckland MR, Vallipuram SK, Hendrata MV, et al. Comparison of 0.5% ropivacaine and 0.5% bupivacaine in lumbar epidural anaesthesia for lower limb orthopaedic surgery. Anaesth Intensive Care. 1997;25:262–6. doi: 10.1177/0310057X9702500310. [DOI] [PubMed] [Google Scholar]
- 14.Wood MB, Rubin AP. A comparison of epidural 1% ropivacaine and 0.75% bupivacaine for lower abdominal gynecologic surgery. Anesth Analg. 1993;76:1274–8. doi: 10.1213/00000539-199376060-00015. [DOI] [PubMed] [Google Scholar]
- 15.Fibla JJ, Molins L, Mier JM, Sierra A, Vidal G. Comparative analysis of analgesic quality in the postoperative of thoracotomy: Paravertebral block with bupivacaine 0.5% vs ropivacaine 0.2% Eur J Cardiothorac Surg. 2008;33:430–4. doi: 10.1016/j.ejcts.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Brown DL, Carpenter RL, Thompson GE. Comparison of 0.5% ropivacaine and 0.5% bupivacaine for epidural anesthesia in patients undergoing lower-extremity surgery. Anesthesiology. 1990;72:633–6. doi: 10.1097/00000542-199004000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Brockway MS, Bannister J, McClure JH, McKeown D, Wildsmith JA. Comparison of extradural ropivacaine and bupivacaine. Br J Anaesth. 1991;66:31–7. doi: 10.1093/bja/66.1.31. [DOI] [PubMed] [Google Scholar]
- 18.Tuttle AA, Katz JA, Bridenbaugh PO, Quinlan R, Knarr D. A double-blind comparison of the abdominal wall relaxation produced by epidural 0.75% ropivacaine and 0.75% bupivacaine in gynecologic surgery. Reg Anesth. 1995;20:515–20. [PubMed] [Google Scholar]
- 19.Pace MM, Sharma B, Anderson-Dam J, Fleischmann K, Warren L, Stefanovich P. Ultrasound-guided thoracic paravertebral blockade: A retrospective study of the incidence of complications. Anesth Analg. 2016;122:1186–91. doi: 10.1213/ANE.0000000000001117. [DOI] [PubMed] [Google Scholar]


