Abstract
Background:
The advent of laparoscopic surgeries has proved to be beneficial for both patient and surgeon although increased morbidity may result from hemodynamic changes associated with laryngoscopy, intubation, and pneumoperitoneum (PNP).
Aim:
The present study was prospective, randomized, double-blind conducted to evaluate the efficacy of dexmdetomidine and fentanyl in attenuation of pressor responses to laryngoscopy, intubation, and PNP in laparoscopic cholecystectomy (LC).
Materials and Methods:
A total of 60 patients of 18–65 years, American Society of Anaesthesiologists Class I/II of either sex for elective LC, were included. The patients were divided into two groups of 30 patients each. Group I received dexmedetomidine and Group II Fentanyl loading 1 μg/kg over 15 min followed by maintenance 0.2 μg/kg/h throughout the PNP.
Measurements:
Heart rate (HR), systolic blood pressure, diastolic blood pressure, and mean arterial blood pressure (MAP) were recorded preoperatively, 15 min after infusion of study drug, 1 min after induction, 1 min after intubation, throughout the PNP, end of surgery, and until 60 min in postoperative period. Sedation score, visual analog scale score along with modified Alderete score applied in postanesthesia care unit.
Results:
Control of HR and MAP in Group I was better than in Group II during laryngoscopy, intubation and PNP. There was also smooth extubation, less sedation and better control of pain in Group I than in Group II.
Conclusion:
The present study demonstrates the benefits of dexmedetomidine over fentanyl in hemodynamic stability and analgesic quality in LC. Thus, it is establishing its utility over for attenuation of pressor response.
Keywords: Dexmedetomidine, fentanyl, laparoscopic cholecystectomy, pneumoperitoneum, pressor response
INTRODUCTION
Laparoscopic surgeries form an essence of today's surgical practice because of its magnification, dexterity, less cosmetic scar, less postoperative pain, and decreased hospital stay along with less morbidity and mortality.[1,2] Laparoscopic cholecystectomy (LC) has become the gold standard for gall bladder diseases.[3] It is termed as patient friendly surgery because of less postoperative pain, shorter hospitalization and faster functional recovery along with other advantages of laparoscopic procedures.[4]
Anesthetic maneuvers such as induction, laryngoscopy, tracheal intubation, and extubation involve sympathetic stimulation and autonomic reflex activity during general anesthesia.[5,6] In LC, initial Trendelenburg position, creation of pneumoperitoneum (PNP), systemic absorption of CO2, and reverse Trendelenburg position cause pathophysiological changes in various systems of the body leading to increase in plasma level of nor-epinephrine, epinephrine, and plasma renin activity.[7] All these factors together contribute to increase in heart rate (HR), mean arterial pressure (MAP), and increased systemic and pulmonary vascular resistance along with reduced cardiac output.[8] The hemodynamic changes predispose the myocardium in vulnerable patients to ischemic changes. Therefore, the basic need has been continuously felt in anesthesia practice for availability of drug that electively suppresses all hazardous responses to obnoxious stimuli with maximum safety margin.[9] Various agents such as opioid analgesics, benzodiazepines, beta blockers, calcium channel blockers, and vasodilators have been used with variable success.[6]
Alpha two agonists have potential benefit for use as they posses various properties such as hypnotic, sedative, anxiolytic, sympatholytic, and analgesic properties without producing significant respiratory depression. Opioids are also used to blunt the hemodynamic response to intubation and surgical stress responses, but they are associated with nausea, vomiting, and respiratory depression.[10]
The primary aim of the present study was, therefore, to evaluate and compare the effect of low dose infusion of dexmedetomidine and fentanyl in attenuation of pressor response to laryngoscopy, intubation, and PNP.
The secondary aims were to observe the effects on extubation time, sedation levels, postoperative analgesia, time to discharge from postanesthesia care unit (PACU), and occurrence of adverse effects.
MATERIALS AND METHODS
Study design: it was a prospective, randomized, double-blind study. The study protocol was approved by the Institutional Thesis and Ethics Committee and written informed consent was taken from each of the patients. Sixty American Society of Anaesthesiologists (ASA) Class I and II patients, aged 18–65 years and undergoing elective LC were randomly assigned to one of the two groups (each containing 30 patients): Group I (dexmedetomidine group) and Group II (fentanyl group). Patients with hypertension, morbid obesity, severe hepatic, renal, cardiac, and endocrine dysfunction were excluded from the study.
On arrival to operation theater, routine monitoring (electrocardiogram, pulse oximetry, noninvasive blood pressure) was started and baseline vital parameters such as HR, systolic blood pressure (SBP), diastolic blood pressure (DBP) and MAP, and arterial oxygen saturation (SpO2) were recorded. An intravenous (IV) line was secured and 10 ml/kg/h of ringer's lactate infusion was started before infusing any medication. IV injection midazolam 0.1 mg/kg was given 30 min before start of surgery. Study medication was prepared by an anesthesiologist who was blinded to the computerized generated randomization schedule in 50 ml syringe resulting in concentration of 5 µg/ml in both groups.
In Group I intravenous infusion of dexmedetomidine was started at a rate of 1 µg/kg followed by induction and then continuous infusion at the rate of 0.2 µg/kg throughout the surgery was given. In Group II, fentanyl was given as loading infusion at the rate of 1 µg/kg followed by infusion at the rate of 0.2 µg/kg. Induction was done 15 min after start of loading infusion with propofol (2 mg/kg). Endotracheal intubation was facilitated by vecuronium following “priming principle.” The priming dose of vecuronium (0.015 mg/kg) was given before propofol. Intubation was done after giving intubating dose of 0.05 mg/kg 6 min after giving the “priming dose.” Maintenance of anesthesia was done with O2 in N2O, isoflurane and intermittent bolus doses of vecuronium. PNP was created with peritoneal insufflation was done with CO2 (at the rate of 2 L/min). Intra-abdominal pressure (IAP) was maintained at 12–14 mmHg. EtCO2 was maintained between 35 and 40 mmHg by mechanical ventilation. Intraoperative hypertension was managed by nitroglycerine spray.
At the end of surgery, infusion of the study drug was stopped. Residual neuromuscular blockade was reversed by appropriate dose of neostigmine and glycopyrrolate followed by tracheal extubation. Time to tracheal extubation, time to respond to verbal commands, and Orientation time were noted. HR, SBP, DBP, MAP, and SpO2 were recorded throughout the surgery after infusion, 1 min after induction, 1 min after intubation, After PNP (at various intervals), end of PNP, end of surgery, and until 60 min after completion of surgery. Sedation in both groups was noted using Ramsay Sedation Score. Postoperative pain was evaluated in both the groups using visual analog scale (VAS) score. Modified Aldrete score was applied to decide about discharge the patients from postoperative care unit (PACU). Patients were observed for any adverse events in PACU.
Statistical analysis
The results obtained from the study have been presented in the tabulated manner. The results have been expressed in mean ± standard deviation. Comparison between groups performed with IBM SPSS 22 software (SPSS Inc., IBM, Chicago, IL, USA), unpaired t-test, Chi-square test, and P values. Blinding was opened at the end of the study.
RESULTS
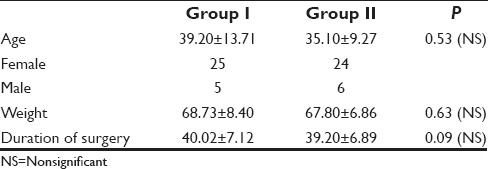
Demographic variables [Table 1] in terms of age, body weight, height, and gender along with ASA status (Class I/II) were comparable in between groups although was statistically significant higher females to male ratio and ASA I patients in study population among each. The mean duration of surgery in minutes was 40.02 ± 7.12 and 39.20 ± 6.89 in each group respectively [Table 1].
Table 1.
Demographic profile
Baseline HR (bpm) was comparable in both the groups, which was 78.01 ± 7.16 and 80.73 ± 9.23, respectively, in both the groups. After start of infusion of dexmedetomidine, HR decreased to 72.53 ± 4.89, 15 bpm in Group I. After induction, there was more decrease (67.43 ± 4.23) but it increased to 77.83 ± 6.57 after intubation. There was significant increase during PNP (80.18 ± 6.62), which returned to baseline at around 30 to 45 min after creation of PNP. In Group II, after start of infusion of fentanyl, HR decreased to 77.46 ± 1.65 beats/min. There was further decrease after induction to 75.07 ± 8.03 and increase after intubation (85 ± 6.3). After creation of PNP, HR remained above the baseline until the end of PNP. In both the groups during postoperative period HR was above baseline until 45 min which settled to baseline at around 60 min after completion of surgery [Graphs 1 and 2].
Graph 1.
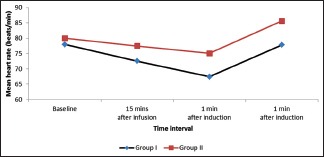
Variation of heart rate during laryngoscopy and intubation
Graph 2.
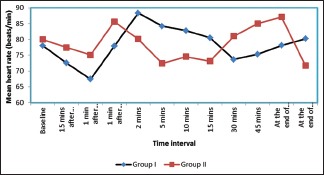
Variation of heart rate during surgery
The variation observed after laryngoscopy and intubation in our study is in consistence with a study conducted by Bajwa et al.[9] Talke et al.[11] showed that dexmedtomidine caused less increase in HRs and noradrenaline levels when administered at a dose of 0.8 µg/kg via IV infusion.
SBP (in mmHg) is comparable in both the groups with 130.50 ± 5.13 in Group I and 132.23 ± 7.09 in Group II. SBP decreased to 116.13 ± 4.11, 15 min after the infusion of dexmedetomidine which further decreased after induction (112.13 ± 4.34) followed by increase after intubation (122.13 ± 9.34). SBP remained lower than baseline throughout the PNP (119 ± 6) and end of surgery (121 ± 71). In Group II, SBP decreased after 15 after infusion of fentanyl to 128.00 ± 6.60. Further decrease occurred after induction to 121.96 ± 94, followed by increase after intubation to 137.00 ± 5.68. During PNP, there was decrease in value, though it remained above the baseline (133.42 ± 7.00) till the end of surgery. In postoperative period, initially, the value was above the baseline which returned to baseline at around 45 min after completion of the surgery in both the groups. Jain et al.,[12] concluded that an IV infusion of dexmedetomidine at 1 µg/kg recommended over fentanyl 2 µg/kg to attenuate the sympathetic response to laryngoscopy and endotracheal intubation with minimal side effects.
Baseline DBP (in mmHg) is 79.57 ± 5.26 in Group I which decreased to 71.56 ± 5.18 after starting the infusion of dexmedetomidine. There was further decrease after induction (69.46 ± 5.67) and increase after intubation to 75.53 ± 4.16 though values remained below the baseline. Throughout the PNP, DBP (74.35 ± 4.9) remained below baseline till end of surgery (77.53 ± 5.12). In Group II baseline DBP 82.51 ± 5.20 decreased after infusion of fentanyl to 79.56 ± 5.88. There was further decrease after induction to 69.46 ± 5.97 but increased to 75.53 ± 4.16 after intubation. There occurred increase after intubation. Values remained above the baseline throughout the surgery (84.86 ± 7.4). In postoperative period, DBP remained below the baseline in Group I and above the baseline in Group II which came to the baseline 60 min after completion of surgery.
Varma et al.[13] demonstrated effects of fentanyl 2 µg/kg and esmolol 2 µg/kg over attenuation of hemodynamic response to laryngoscopy and intubation.
Baseline MAP was 94.62 ± 4.45 and 96.31 ± 5.71, respectively, in both the groups. After infusion of dexmedetomidine, MAP decreased to 91.07 ± 5.27 and after induction it further decreased to 83.97 ± 4.95 but increased to 91.07 ± 5.27 after intubation. Values below baseline were noted throughout the PNP (92.5 ± 3.9) till end of the surgery 90.67 ± 5.17. In Group II, MAP decreased from the baseline (96.31 ± 5.71) to 90.28 ± 6.01, 15 min after infusion of fentanyl. There occurred reduction to 83.97 ± 4.95 after induction which increased to 91.07 ± 5.27 after intubation. MAP remained above baseline (102.23 ± 6.16) throughout the surgery till end of the surgery to 102.32 ± 6.14. In postoperative period, values remained below baseline in Group I and above the baseline till 60 min after completion of the surgery in Group II [Graph 3].
Graph 3.
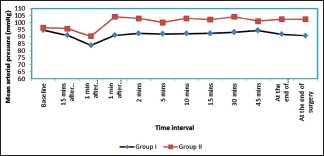
Variation of map during surgery
Ozkose et al.[14] observed decrease in MAP up to 20% and HR up to 15% after single dose of dexmedetomidine 1 µg/kg. Yildiz et al.[15] have concluded that a single dose of dexmedetomidine at 1 µg/kg prevented cardiovascular hemodynamic response and decreased the need for additional opioid during laryngoscopy and endotracheal intubation in elective minor surgery patients. Dahlgren and Messeter[16] have documented the attenuation of hemodynamic response to laryngoscopy and intubation by use of fentanyl in comparison to control group, though the dose required is much higher (5 µg/kg). Higher requirement of dose leads to various side effects which might over weigh the benefits.
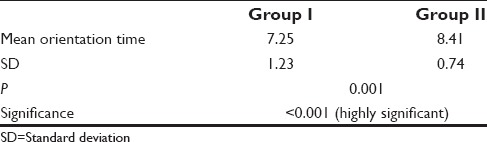
Time to extubation was comparable in both the groups. Orientation time was more in fentanyl group than in dexmedetomidine group. Time to respond to verbal commands was more in fentanyl group than in dexmedetomidine group. Rao[1] has concluded extubation to be smooth with minimal changes in hemodynamics. Immediate eye opening along with response to verbal commands indicates no residual effects of dexmedetomidine [Table 2].
Table 2.
Orientation time in Group I and Group II in minutes
Sedation score was comparable in both the groups. Rao[1] in his study has documented immediate eye opening and response to verbal commands, with no residual effects of dexmedetimidine. Alderete score in both the groups is not statistically significant. VAS score in PACU is higher in fentanyl group than in dexmedetomidine group. Helmy et al.[17] showed similar results in VAS score as our in postoperative period [Graph 4].
Graph 4.
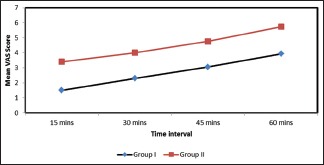
Visual analog scale score in Group I and Group II at 15 min, 30 min, 45 min, and 60 min after completion of surgery
DISCUSSION
Laryngoscopy and tracheal intubation are associated with sympathetic stimulation, which present in the form of hemodynamic changes such as rise in HR and blood pressure. These changes are usually transient, variable, and unpredictable which may or may not be tolerated by all the patients. Laparoscopic surgery requires creation of PNP, which is commonly done with insufflation with CO2. Elevated IAP after creation of PNP leads to rise in plasma level of norepiniphrine, epinephrine, and renin activity. Activation of Renin-angiotensin-aldosterone-system leads to various hemodynamic alterations such as decreased cardiac output, elevated arterial pressure and increased systemic/pulmonary vascular resistance. These physiological changes are of special concern to anaesthesiologists for safe and efficient management of the patient undergoing laparoscopic cholecystectomy. Various agents have been used to evaluate the safety of techniques and various drugs. Joris and Lamy documented release of vasopressin paralleled the time course of the increase in systemic vascular resistance after creation of PNP.[18]
In the study, we observed the effects of dexmedetomidine and fentanyl on attenuation of pressor response to laryngoscopy, intubation and PNP in LC. Dexmedetomidine is a highly selective α2 agonist. Hypotension is caused by activation of receptors in the brain and spinal cord level, inhibiting neuronal firing. Presynaptic activation of α2 adrenergic receptors inhibits release of noreponehprine and postsynaptic activation in the central nervous system inhibits sympathetic activity and, therefore, can decrease blood pressure and HR. Effects of hemodynamics are mediated by inhibition of central sympathetic outflow.[8]
Fentanyl on the other hand acts via opioid receptors, leading to obtundation of pressor response. At high doses, 6 µg/kg completely abolishes the pressor response but produces tissue accumulation and requirement of mechanical respiratory support. At low doses of 1–2 µg/kg, it attenuates arterial pressure and HR increase during laryngoscopy and intubation.[16]
In several study reports, infusion of dexmedetomidine has been used in range of 0.1 to 10 µg/kg.[8] There was smooth extubation and lesser orientation time by use of dexmedetomidine than fentanyl. Dexmedetomidine has shown better control of pain relief till 60 min in postoperative period than fentanyl, reducing postoperative analgesic requirements. Various side effects such as bradycardia and hypotension as associated with use of dexmedetomidine use can be counteracted by using slow infusion over 15–20 min and hypotension by adequate preloading of the patient.[8] In our study, no such adverse effect has been noted. Decrease in SpO2 as associated with fentanyl is prevented by proper monitoring and use of supplemented O2 therapy. Sedation in fentanyl was noted and patient taken care of by proper monitoring.
CONCLUSION
We have found better attenuation of pressor response by use of dexmedetomidine than by use of fentanyl along with better patient comfort and cooperation, both intra-operatively and postoperatively. But there are few limitations of our study. Study population as calculated at the start of our project was based on various previous studies and taken to be as 85%. We could have drawn more positive results had the power of study been taken to be as 90% or >90%. This would have been possible by inclusion of more number of patients, but we avoided, as it would increase the inclusion of population at risk. But still we recommend using of dexmedetomidine to attenuate pressor responses during laryngoscopy, intubation and while creating PNP in LC.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rao LN. A clinical study of dexmedetomidine for maintenance during general anaesthesia for laparoscopic surgeries. Int J Med Sci Clin Invent. 2015;2:681–7. [Google Scholar]
- 2.Srivastava VK, Nagle V, Agarwal S, Kumar D, Verma A, Kedia S. Comparative evaluation of esmolol and dexmedetomidine for attenuation of sympathomimetic response to laryngoscopy and intubation in neurosurgical patients. J Anaesthesiol Clin Pharmacol. 2015;31:186–90. doi: 10.4103/0970-9185.155146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Das M, Ray M, Mukherjee G. Haemodynmaic changes during laparoscopic cholecystectomy: Effect of clonidine premedication. Indian J Anaesth. 2007;51:205–10. [Google Scholar]
- 4.Amornyotin S. Anesthetic management of laparoscopic cholecystectomy. Int J Anesthesiol Res. 2013;1:3–7. [Google Scholar]
- 5.Chraemmer-Jørgensen B, Hertel S, Strøm J, Høilund-Carlsen PF, Bjerre-Jepsen K. Catecholamine response to laryngoscopy and intubation. The influence of three different drug combinations commonly used for induction of anaesthesia. Anaesthesia. 1992;47:750–6. doi: 10.1111/j.1365-2044.1992.tb03252.x. [DOI] [PubMed] [Google Scholar]
- 6.Manne GR, Upadhyay MR, Swadia V. Effects of low dose dexmedetomidine infusion on haemodynamic stress response, sedation and post-operative analgesia requirement in patients undergoing laparoscopic cholecystectomy. Indian J Anaesth. 2014;58:726–31. doi: 10.4103/0019-5049.147164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Leary E, Hubbard K, Tormey W, Cunningham AJ. Laparoscopic cholecystectomy: haemodynamic and neuroendocrine responses after pneumoperitoneum and changes in position. Br J Anaesth. 1996;76:640–4. doi: 10.1093/bja/76.5.640. [DOI] [PubMed] [Google Scholar]
- 8.Bhattacharjee DP, Nayek SK, Dawn S, Bandopadhyay G, Gupta K. Effects of dexmedetomidine in hemodynamics in patients undergoing laparoscopic cholecystectomy – A comparative study. J Anaesthesiol Clin Phamacol. 2010;29:45–8. [Google Scholar]
- 9.Bajwa SJ, Kaur J, Singh A, Parmar S, Singh G, Kulshrestha A, et al. Attenuation of pressor response and dose sparing of opioids and anaesthetics with pre-operative dexmedetomidine. Indian J Anaesth. 2012;56:123–8. doi: 10.4103/0019-5049.96303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prakash R, Kushwaha B, Kumar S. A comparative study of fentanyl and clonidine on hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy. Int J Sci Eng Res. 2014;5:1552–8. [Google Scholar]
- 11.Talke P, Chen R, Thomas B, Aggarwall A, Gottlieb A, Thorborg P, et al. The hemodynamic and adrenergic effects of perioperative dexmedetomidine infusion after vascular surgery. Anesth Analg. 2000;90:834–9. doi: 10.1097/00000539-200004000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Jain V, Chandak A, Ghosh A, Golhar M. Comparison of dexmedetomidine and fentanyl for attenuation of the hemodynamic response to laryngoscopy and tracheal intubation. Ain Shams J Anesthesiol. 2015;8:236–43. [Google Scholar]
- 13.Varma TA, Apranjit K, Uma R. A comparative study of efficacy of esmolol and fentanyl for attenuation of intubation response during laryngoscopy. J Evol Med Dent Sci. 2015;4:6778–86. [Google Scholar]
- 14.Ozkose Z, Demir FS, Pampal K, Yardim S. Hemodynamic and anesthetic advantages of dexmedetomidine, an alpha 2-agonist, for surgery in prone position. Tohoku J Exp Med. 2006;210:153–60. doi: 10.1620/tjem.210.153. [DOI] [PubMed] [Google Scholar]
- 15.Yildiz M, Tavlan A, Tuncer S, Reisli R, Yosunkaya A, Otelcioglu S. Effect of dexmedetomidine on haemodynamic responses to laryngoscopy and intubation: perioperative haemodynamics and anaesthetic requirements. Drugs R D. 2006;7:43–52. doi: 10.2165/00126839-200607010-00004. [DOI] [PubMed] [Google Scholar]
- 16.Dahlgren N, Messeter K. Treatment of stress response to laryngoscopy and intubation with fentanyl. Anaesthesia. 1981;36:1022–6. doi: 10.1111/j.1365-2044.1981.tb08676.x. [DOI] [PubMed] [Google Scholar]
- 17.Helmy N, Helmy J, El-Sakka A, Rafaat H. The hemodynamic and analgesic profile of dexmedetomidine against fentanyl in preeclamptic parturients undergoing cesarean section under general anesthesia. Ain Shams J Anesthesiol. 2015;8:183–8. [Google Scholar]
- 18.Joris J, Lamy M. Neuroendocrine changes during pneumoperitoneum for laparoscopic cholecystectomy. Br J Anaesth. 1993;70:A33. [Google Scholar]


