Abstract
Background:
The present study was undertaken to compare and evaluate the efficacy of intravenous (IV) fentanyl and lignocaine airway nebulization and a combination of both in attenuating the hemodynamic response to laryngoscopy and tracheal intubation.
Materials and Methods:
Ninety-six patients of either sex aged between 18 and 65 years of age, belonging to the American Society of Anesthesiologists (ASA) health status Classes I and II, undergoing elective surgery requiring general anesthesia with endotracheal intubation were included in the study. Patients were randomly divided into three groups. Group F received IV fentanyl 2 μg/kg, Group L received nebulization with 3 mg/kg of 4% lignocaine, and Group FL received both nebulization with 3 mg/kg of 4% lignocaine and IV fentanyl 2 μg/kg before intubation. Hemodynamic parameters were noted before and immediately after induction, 1 min after intubation, and every minute after intubation for 10 min.
Results:
Hemodynamic response to laryngoscopy and intubation was not completely abolished in any of the groups. Nebulized lignocaine was least effective in attenuating hemodynamic response to intubation, and hemodynamic parameters were significantly high after intubation as compared to other groups. Fentanyl alone or in combination with nebulized lignocaine was most effective, and Group F and Group FL were comparable. The maximum increase in mean blood pressure after intubation from baseline in Groups F, L, and FL was 7.4%, 14.6%, and 5.4%, respectively.
Conclusion:
In our study, IV fentanyl 2 μg/kg administered 5 min before induction was found to be the most effective in attenuating the hemodynamic response. There was no advantage to the use of nebulized lignocaine in attenuating the hemodynamic response to laryngoscopy and intubation.
Keywords: Fentanyl, hemodynamic response, intubation, laryngoscopy, lignocaine, nebulization
INTRODUCTION
Laryngoscopy and tracheal intubation after induction of anesthesia generate pressure and sympathoadrenal responses which are thought to be somatovisceral reflexes caused by the stimulation of epipharynx and laryngopharynx.[1] Laryngoscopy alone generates essentially the same pressor response as done by laryngoscopy followed by intubation.[2] It starts within 5 s, reaches a peak in 1–2 min, and returns to baseline within 5 min.[3] These responses result in increased circulatory catecholamines, heart rate (HR), blood pressure, myocardial oxygen demand, and dysrhythmias. The rise in HR and blood pressure is usually transient, variable, and unpredictable. Average increase in HR has been reported to be 23 beats and increase in blood pressure by 53/54 mmHg and decrease in the left ventricular ejection fraction by approximately 20%.[4,5] Although such a response would likely be tolerated by healthy patients, these changes may be associated with myocardial ischemia and cerebral hemorrhage in those with a significant coronary artery or cerebrovascular diseases.[6]
Several techniques have been tried in an effort to attenuate adverse hemodynamic responses to intubation. Commonly used techniques include increasing the depth of anesthesia by heavy premedication, potent narcotics such as fentanyl[7] and inhalational anesthetic agents.[8] Others include intravenous (IV) and topical lignocaine, clonidine, calcium channel blockers, sodium nitroprusside, beta-adrenergic blockers, and magnesium sulfate but none is ideal.
Topical anesthesia of the upper airway has been shown to attenuate the hemodynamic responses during laryngoscopy and intubation, and a combination of topical anesthetics with opioids may be useful. Our objective was to find a simple and safe method for diminishing the incidence and severity of cardiovascular reaction to laryngoscopy and tracheal intubation which would be of clinical importance in anesthetic practice, particularly in patients with intracranial pathology and decreased myocardial reserve. As the circulatory changes are thought to be somatovisceral reflexes that are triggered by the stimulation of proprioceptors at the epipharynx and laryngopharynx, it was hypothesized that topical anesthesia of airway alone or in combination with other techniques may be useful in attenuating these reflexes. This study was designed as a prospective, blind, randomized controlled study to compare and evaluate the efficacy of IV fentanyl and lignocaine airway nebulization and a combination of both in attenuating the hemodynamic response to laryngoscopy and tracheal intubation.
MATERIALS AND METHODS
After approval by the Hospital Ethics Committee, this prospective randomized, double-blind study was conducted in 96 normotensive, the American Society of Anesthesiologists (ASA) physical status Class I and II patients of either sex in the age group of 18–65 years. A written informed consent was taken from patients scheduled for elective surgery in the supine position under general anesthesia with tracheal intubation and controlled ventilation. They were randomly divided into three groups each containing 32 patients according to computer generated numbers: Group F-nebulization with 0.075 ml/kg normal saline and IV fentanyl 2 μg/kg (diluted to 3cc with normal saline); Group L-nebulization with 3 mg/kg (0.075 ml/kg) of 4% lignocaine and IV normal saline 3cc; Group FL-nebulization with 3 mg/kg (0.075 ml/kg) of 4% lignocaine and IV fentanyl 2 μg/kg (diluted to 3cc with normal saline).
Patients with the following conditions were excluded from the study: refusal or inability to understand the procedure, allergy to any of the study drugs, smoker, body mass index (BMI) >30, modified Mallampati Class III or IV, history of respiratory distress, gastroesophageal reflux, neurological, cardiovascular, cerebrovascular, respiratory, hepatic or renal diseases, and anticipated difficult airway.
All selected patients underwent a thorough preanesthetic checkup. All patients fasted overnight and received oral alprazolam 0.5 mg the night before surgery.
In the preoperative holding area standard monitoring, including noninvasive blood pressure, HR, oxygen saturation (SpO2), and electrocardiography (ECG) lead II was instituted and recorded at predetermined intervals. IV access was secured. Ringer's lactate 10 ml/kg/h was administered until the completion of the study. Midazolam 20 μg/kg was administered IV. After 5 min, baseline hemodynamic parameters including HR, systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MBP), rate pressure product (RPP), ECG lead II, and SpO2 were recorded.
The patients, according to the allotted group, received either 0.075 ml/kg normal saline or 3 mg/kg of 4% lignocaine via a face mask and cirrus nebulizer with O2 at the rate of 8 L/min. Nebulization was done until the complete utilization of drug (approximately 10–15 min.). The hemodynamic parameters were noted at 5 min intervals during nebulization.
The patients were then brought to the operation theater and monitoring reinstituted. The patients, according to the allotted groups, received IV fentanyl 2 μg/kg diluted to 3cc with normal saline or IV normal saline 3cc and given slowly. The hemodynamic parameters were recorded 5 min after IV study drugs.
The anesthetist who prepared the drugs was aware of the groups assigned, but the hemodynamic parameters were noted by another anesthetist who was unaware of the group allocation.
Patients were supine and in sniffing position. Anesthesia was induced with propofol IV (2–2.5 mg/kg) until the loss of verbal response followed by vecuronium 0.1 mg/kg. Intermittent positive pressure ventilation was performed with N2O 66% in O2 with isoflurane 0.6% at a flow rate of 6 L/min. via a face mask. Three minutes later, laryngoscopy using Macintosh blade size 3 and tracheal intubation using cuffed tracheal tube size 7 mm (in females), and size 8 mm (in males) was performed by an experienced anesthetist. Duration of laryngoscopy and intubation till cuff inflation was noted. Hemodynamic parameters were noted before and immediately after induction, 1 min after intubation, and every minute after intubation for 10 min. During this period, the patient was left undisturbed. Adverse events, if any, were noted. Any coughing/bucking by the patient was recorded.
Anesthesia was maintained with 66% N2O in O2 and isoflurane 0.6%. Ventilatory parameters were TV = 10 ml/kg, I: E = 1:2, RR = 12 breaths/min, and EtCO2 = 30–35 mmHg.
Patients in whom the Cormack and Lehane grade were 3 or 4, duration of laryngoscopy and intubation >30 s, unexpected difficulty in ventilation or intubation, laryngospasm or bronchospasm occurrence or in whom the time span from completion of nebulization to intubation >20 min were excluded from the study.
To detect a difference of 10 mmHg in MBP between standard and study group for alpha = 0.05 and power = 80%, the minimum number of cases required were 32 in each group. Patients excluded from the study were re-randomized.
Demographic data such as age, sex, height, weight, and BMI were also noted.
Data are expressed as mean ± standard deviation for quantitative information and in percentage and numbers for categorical variations. The results were subjected to statistical analysis using ANOVA for overall differences. Student's t-test was applied to observe the difference between two groups. P < 0.05 was taken as statistically significant. Analysis of the statistical data obtained from the study was carried out by statistical programming software Statistical Package for the Social Sciences (SPSS) Statistics version 19.0.0 (SPSS Inc., Chicago, Illinois, USA).
RESULTS
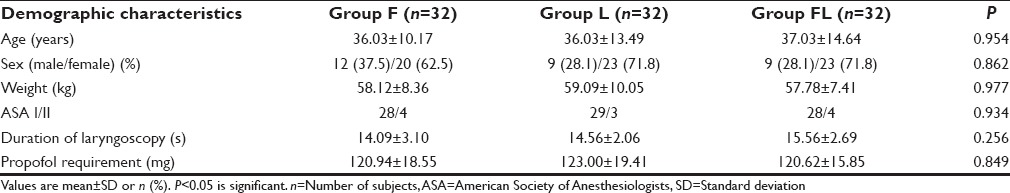
Age, sex, weight, ASA Physical status, duration of laryngoscopy, and propofol consumption were comparable in the three groups [Table 1].
Table 1.
Demographic characteristics
Baseline hemodynamic parameters were comparable in all the groups.
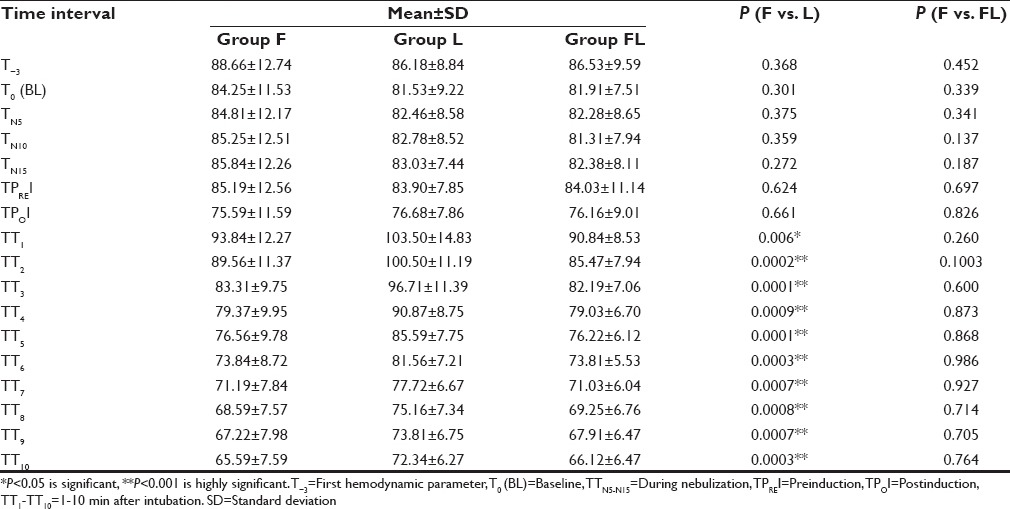
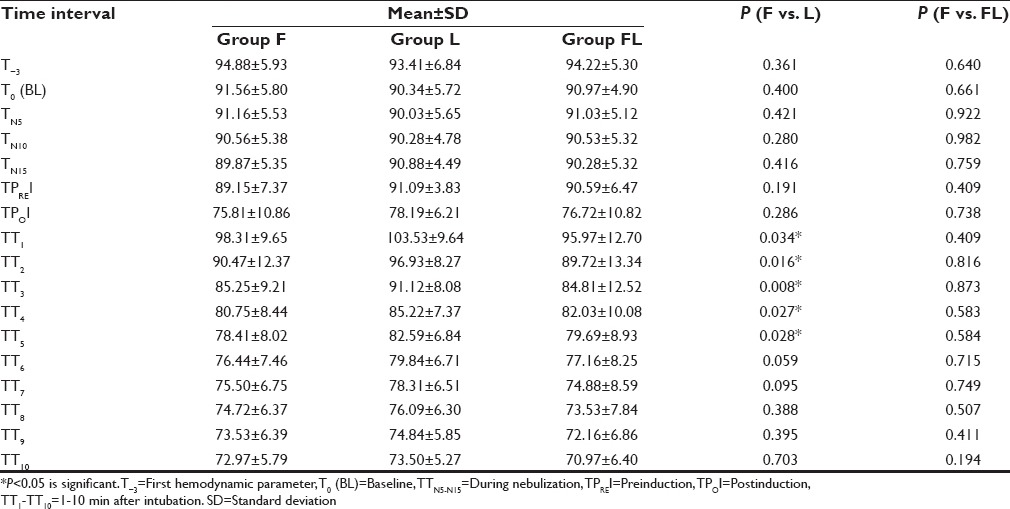
Among the groups, the maximum increase in HR was seen in Group L 1 min after intubation [Graph 1]. When HR at different time intervals in Group F was compared with Group L and FL, it was found to be significantly high in Group L 1 min after intubation (TT1) and remained increased till study period (TT10), whereas in group FL there was no significant difference [Table 2].
Graph 1.
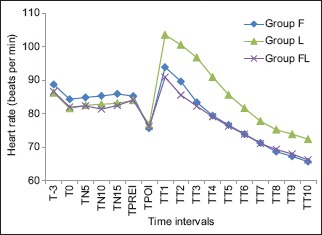
Intergroup comparison of heart rate (T–3 – First hemodynamic parameter, T0 – Baseline, TTN5–N15 – During nebulization, TPREI – Preinduction, TPOI – Post induction, TT1 to TT10 – 1–10 min after intubation)
Table 2.
Intergroup comparison of heart rate
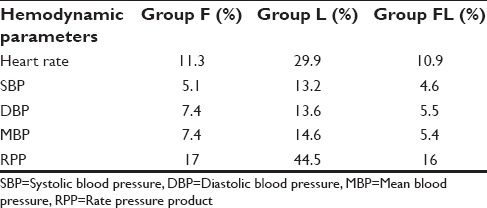
Among the groups, MBP was maximally increased after intubation in Group L [Graph 2].
Graph 2.
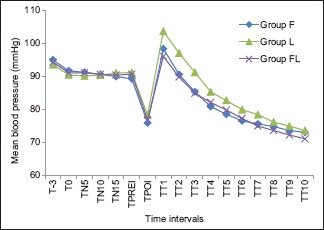
Intergroup comparison of mean blood pressure (T–3 – First hemodynamic parameter, T0 – Baseline, TTN5–N15 – During nebulization, TPREI – Preinduction, TPOI – Post induction, TT1 to TT10 – 1–10 min after intubation)
MBP was significantly high in Group L from 1 to 5 min after intubation (TT1 to TT5) when compared with Group F. MBP at all the time intervals were comparable in Group FL and Group F [Table 3].
Table 3.
Intergroup comparison of mean blood pressure
On comparing SBP, DBP, and RPP in Group F with Group L at different time intervals, SBP was significantly high from 1 min after intubation (TT1) to 10 min (TT10), DBP from TT1 to TT2 and RPP from TT1 to TT10 in group L. SBP, DBP, and RPP were comparable in group F and group FL at all time intervals.
The maximum increase in hemodynamic parameters in all the groups was observed at 1 min after intubation (TT1). Group L showed significantly greater increase in all the hemodynamic parameters when compared with Group F and FL. Group F and Group FL were comparable [Table 4].
Table 4.
Maximum increase in hemodynamic parameters from baseline (%)
Coughing was not observed in any patient at the time of laryngoscopy and intubation. ECG was within normal limits in all the patients studied during the study period. No episodes of dysrhythmias in any patient were observed. No patient required atropine or vasopressor. SpO2 was >95% in the patients during the study period. No other adverse effects were seen during the study period.
DISCUSSION
Hemodynamic response to laryngoscopy and intubation was not completely abolished in any of the groups. Fentanyl alone or in combination with nebulized lignocaine was most effective in blunting the postintubation increase in both HR and blood pressures among the groups, but both of them were comparable.
Dahlgren and Messeter,[9] Ezike and Nwosu[10] and Hoda and Khan,[11] Parida et al.,[12] Mireskandari et al.,[13] Malde and Sarode[14] also found IV fentanyl effective in blunting hemodynamic response to intubation. Hoda and Khan[11] in a double-blind study, studied the effect of one MAC sevoflurane with or without fentanyl on hemodynamic response to laryngoscopy and intubation. They showed a maximum increase after intubation in HR and SBP of 15% and 6%, respectively, in group receiving IV fentanyl 2 µg/kg with sevoflurane. These findings were comparable to our study in which maximum rise in HR and SBP was 11.3% and 5.1%, respectively. Kautto,[15] Black et al.,[16] and Kay et al.[17] have shown complete attenuation of the hemodynamic response to intubation by IV fentanyl. Our study shows blunting but not complete attenuation of the hemodynamic response to intubation. This may be due to a higher dose of fentanyl (5–6 µg/kg) used in these studies, unlike our study in which we used 2 µg/kg.
Nebulized lignocaine was found least effective in all the groups, and all the hemodynamic parameters were significantly increased after intubation when compared with other groups. Combining nebulized lignocaine and IV fentanyl was found most effective, but it did not reach the significant level when compared with IV fentanyl alone. Therefore, nebulization with lignocaine did not offer any additional advantage in attenuating hemodynamic response.
Our study has shown nebulized lignocaine as least effective in attenuating hemodynamic response to intubation. This probably may be due to several reasons. Laryngoscopy and intubation are a two part process, each contributing to the hemodynamic response independently. Pressure by laryngoscope blade not only on the mucous membrane but also to the submucosal deep proprioceptors is responsible for these reactions which cannot be blocked by topical anesthesia.[18] The inhalation method provides inadequate anesthesia of trachea. A major part of the drug is lost to air and in patient's mouth during nebulization which is supported by findings of Chinn et al.,[19] who demonstrated that up to 60% of lignocaine dose can be lost via nebulized route. In addition, it has been suggested that nebulized lignocaine may partially inhibit the vagus afferent which by itself may result in unopposed sympathetic outflow with consequent increase in HR and blood pressure.[20] These results were consistent with the studies done by Laurito et al.,[2] Venus et al.,[21] Bunting et al.,[22] Mostafa et al.,[23] and Williams et al.[24] Contrary to our findings, Sklar et al.[25] and Abd El-Hamid et al.[26] found nebulized lignocaine effective in attenuating hemodynamic response to intubation. Meng et al.[27] found topical lidocaine and ropivacaine effective in reducing hemodynamic responses during intubation and ropivacaine better at inhibiting hemodynamic changes at emergence in hypertensive patients when compared with lidocaine.
CONCLUSION
In our study, IV fentanyl 2 μg/kg administered 5 min before induction was found to be the most effective in attenuating the hemodynamic response. It is a part of the routine anesthesia regimen and was found to be a safe and effective method in attenuating the hemodynamic response to laryngoscopy and intubation. There was no advantage to the use of nebulized lignocaine in attenuating the hemodynamic response to laryngoscopy and intubation. Therefore, it should not be used alone for this purpose.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hassan HG, el-Sharkawy TY, Renck H, Mansour G, Fouda A. Hemodynamic and catecholamine responses to laryngoscopy with vs. without endotracheal intubation. Acta Anaesthesiol Scand. 1991;35:442–7. doi: 10.1111/j.1399-6576.1991.tb03325.x. [DOI] [PubMed] [Google Scholar]
- 2.Laurito CE, Baughman VL, Becker GL, Polek WV, Riegler FX, VadeBoncouer TR. Effects of aerosolized and/or intravenous lidocaine on hemodynamic responses to laryngoscopy and intubation in outpatients. Anesth Analg. 1988;67:389–92. [PubMed] [Google Scholar]
- 3.Henderson J. Airway management in the adult. In: Miller RD, editor. Miller's Anesthesia. 7th ed. Philadelphia: Elsevier Churchill Livingstone; 2010. pp. 1573–610. [Google Scholar]
- 4.King BD, Harris LC, Jr, Greifenstein FE, Elder JD, Jr, Dripps RD. Reflex circulatory responses to direct laryngoscopy and tracheal intubation performed during general anesthesia. Anesthesiology. 1951;12:556–66. doi: 10.1097/00000542-195109000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Ng WS. Pathological effects of tracheal intubation. In: Latto IP, Rosen M, editors. Difficulties in Tracheal Intubation. London: Bailliere Tindall; 1985. p. 14. [Google Scholar]
- 6.Roy WL, Edelist G, Gilbert B. Myocardial ischemia during non-cardiac surgical procedures in patients with coronary-artery disease. Anesthesiology. 1979;51:393–7. doi: 10.1097/00000542-197911000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Stoelting R. Opioid agonist and antagonist. In: Stoelting RK, Hiller SC, editors. Pharmacology and physiology in anesthetic practice. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2006. pp. 87–122. [Google Scholar]
- 8.Hamill JF, Bedford RF, Weaver DC, Colohan AR. Lidocaine before endotracheal intubation: Intravenous or laryngotracheal? Anesthesiology. 1981;55:578–81. doi: 10.1097/00000542-198111000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Dahlgren N, Messeter K. Treatment of stress response to laryngoscopy and intubation with fentanyl. Anaesthesia. 1981;36:1022–6. doi: 10.1111/j.1365-2044.1981.tb08676.x. [DOI] [PubMed] [Google Scholar]
- 10.Ezike HA, Nwosu AD. Comparison of the relative efficacy of fentanyl premedication and repeat dose propofol in attenuating cardiovascular response to endotracheal intubation. Niger Med J. 2010;51:18–22. [Google Scholar]
- 11.Hoda A, Khan FA. Effect of one minimum alveolar concentration sevoflurane with and without fentanyl on hemodynamic response to laryngoscopy and tracheal intubation. J Anaesthesiol Clin Pharmacol. 2011;27:522–6. doi: 10.4103/0970-9185.86599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parida S, Ashraf NC, Mathew JS, Mishra SK, Badhe AS. Attenuation of the haemodynamic responses to tracheal intubation with gabapentin, fentanyl and a combination of both: A randomised controlled trial. Indian J Anaesth. 2015;59:306–11. doi: 10.4103/0019-5049.156885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mireskandari SM, Abulahrar N, Darabi ME, Rahimi I, Haji-Mohamadi F, Movafegh A. Comparison of the effect of fentanyl, sufentanil, alfentanil and remifentanil on cardiovascular response to tracheal intubation in children. Iran J Pediatr. 2011;21:173–80. [PMC free article] [PubMed] [Google Scholar]
- 14.Malde A, Sarode V. Attenuation of the hemodynamic response to endotracheal intubation: Fentanyl versus lignocaine. Internet J Anesthesiol. 2006;12:1. [Google Scholar]
- 15.Kautto UM. Attenuation of the circulatory response to laryngoscopy and intubation by fentanyl. Acta Anaesthesiol Scand. 1982;26:217–21. doi: 10.1111/j.1399-6576.1982.tb01757.x. [DOI] [PubMed] [Google Scholar]
- 16.Black TE, Kay B, Healy TE. Reducing the haemodynamic responses to laryngoscopy and intubation. A comparison of alfentanil with fentanyl. Anaesthesia. 1984;39:883–7. doi: 10.1111/j.1365-2044.1984.tb06575.x. [DOI] [PubMed] [Google Scholar]
- 17.Kay B, Healy TE, Bolder PM. Blocking the circulatory responses to tracheal intubation. A comparison of fentanyl and nalbuphine. Anaesthesia. 1985;40:960–3. doi: 10.1111/j.1365-2044.1985.tb10550.x. [DOI] [PubMed] [Google Scholar]
- 18.Barton S, Williams JD. Glossopharyngeal nerve block. Arch Otolaryngol. 1971;93:186–8. doi: 10.1001/archotol.1971.00770060272014. [DOI] [PubMed] [Google Scholar]
- 19.Chinn WM, Zavala DC, Ambre J. Plasma levels of lidocaine following nebulized aerosol administration. Chest. 1977;71:346–8. doi: 10.1378/chest.71.3.346. [DOI] [PubMed] [Google Scholar]
- 20.Mador MJ. Effect of nebulized lidocaine on ventilatory response to CO2 in healthy subjects. J Appl Physiol. 1993;74:1419–24. doi: 10.1152/jappl.1993.74.3.1419. [DOI] [PubMed] [Google Scholar]
- 21.Venus B, Polassani V, Pham CG. Effects of aerosolized lidocaine on circulatory responses to laryngoscopy and tracheal intubation. Crit Care Med. 1984;12:391–4. doi: 10.1097/00003246-198404000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Bunting HE, Kelly MC, Milligan KR. Effect of nebulized lignocaine on airway irritation and haemodynamic changes during induction of anaesthesia with desflurane. Br J Anaesth. 1995;75:631–3. doi: 10.1093/bja/75.5.631. [DOI] [PubMed] [Google Scholar]
- 23.Mostafa SM, Murthy BV, Barrett PJ, McHugh P. Comparison of the effects of topical lignocaine spray applied before or after induction of anaesthesia on the pressor response to direct laryngoscopy and intubation. Eur J Anaesthesiol. 1999;16:7–10. doi: 10.1046/j.1365-2346.1999.00410.x. [DOI] [PubMed] [Google Scholar]
- 24.Williams KA, Barker GL, Harwood RJ, Woodall NM. Combined nebulization and spray-as-you-go topical local anaesthesia of the airway. Br J Anaesth. 2005;95:549–53. doi: 10.1093/bja/aei202. [DOI] [PubMed] [Google Scholar]
- 25.Sklar BZ, Lurie S, Ezri T, Krichelli D, Savir I, Soroker D. Lidocaine inhalation attenuates the circulatory response to laryngoscopy and endotracheal intubation. J Clin Anesth. 1992;4:382–5. doi: 10.1016/0952-8180(92)90160-3. [DOI] [PubMed] [Google Scholar]
- 26.Abd El-Hamid AM, Hasan AM, Abd El-Fattah MH, Shehata A. Lidocaine Nebulizer reduce response to endotracheal intubation and the need for postoperative analgesia after nasal operations. J Am Sci. 2013;9:287–91. [Google Scholar]
- 27.Meng YF, Cui GX, Gao W, Li ZW. Local airway anesthesia attenuates hemodynamic responses to intubation and extubation in hypertensive surgical patients. Med Sci Monit. 2014;20:1518–24. doi: 10.12659/MSM.890703. [DOI] [PMC free article] [PubMed] [Google Scholar]


