Abstract
Background and Aims:
Early extubation is a desirable goal after general anesthesia. Very few studies have compared the effect of bispectral index (BIS) monitoring versus standard end-tidal anesthetic gas (ETAG) concentration monitoring on tracheal extubation time for halothane-based anesthesia. The aim of this study was to compare the effect of BIS versus ETAG-guided anesthesia on time to tracheal extubation for halothane-based anesthesia in general surgical setting.
Methods:
This was a randomized, controlled double-blind study. Sixty patients with the American Society of Anesthesiologists physical status Class 1 or 2, receiving halothane-based general anesthesia were randomized to BIS-guided (n = 30) and ETAG-guided anesthesia (n = 30). Time to tracheal extubation was measured. In BIS group, BIS value was kept between 40 and 60 while in ETAG group; ETAG value was kept between 0.7 and 1.3 minimum alveolar concentration. The two groups were compared using Student's t-test, and P < 0.05 was considered statistically significant. Data were processed and analyzed using SPSS version 17 software.
Results:
Mean time to tracheal extubation was significantly longer in BIS group (9.63 ± 3.02 min) as compared to ETAG group (5.29 ± 1.51 min), mean difference 4.34 min with 95% confidence interval (3.106, 5.982) (P < 0.05).
Conclusion:
In our study, the extubation time was significantly longer in BIS-guided anesthesia as compared to ETAG-guided anesthesia. ETAG monitoring promotes earlier extubation of patients as compared to BIS monitoring during halothane anesthesia.
Keywords: Airway extubation, bispectral index monitor, end-tidal anesthetic gas concentration, general anesthesia, halothane
INTRODUCTION
In this era of newer inhalational anesthetic agents, halothane is still in use in developing countries, due to its low cost, compatibility of halothane vaporizer with all kinds of anesthesia workstations and even Boyle's apparatus.[1] The low incidence of hepatitis is to be weighed against the cost-effectiveness of the drug. For such reasons, complete replacement of halothane with other costlier volatile agents from developing nations including India may not be possible or appropriate.[2] A recent survey studying anesthesia practice in our country showed significant use of halothane.[3] Early tracheal extubation after general anesthesia is a desirable goal as it is associated with decreased Intensive Care Unit (ICU) length of stay (LOS), hospital LOS, and thus, the potential for improved recovery and decreased resource utilization. While intraoperative anesthetic techniques have evolved to emphasize fast track recovery,[4] the role of brain monitoring in extubation has not been well studied. Bispectral index (BIS) monitoring has been used to monitor the depth of anesthesia[5] and might also permit improved accuracy of titration of anesthetic doses to individual patient requirement; therefore, may have relevance regarding reducing recovery time. The widely accepted concept of minimum alveolar concentration (MAC) has led to the use of end-tidal anesthetic gas (ETAG) concentration as a way to monitor the level of unconsciousness induced by inhaled anesthetics. Unlike BIS which provides EEG-based measures of brain activity, the ETAG criteria are related to brain activity through concentration of anesthetic expired in lungs assuming it is in equilibrium with brain concentration. That BIS- and ETAG-based criteria are comparable for monitoring the level of consciousness under general anesthesia have been demonstrated by B-Unaware and BAG-RECALL Trials. They reported no difference in awareness incidence with anesthetic protocol based on BIS (range 40–60) and anesthetic protocol based on ETAG concentration (MAC range 0.7–1.3).[6,7] Yet, the efficacy of these two monitoring modalities for achieving earlier tracheal extubation has not been unequivocally established.[8] Very few studies have compared the effect of BIS versus ETAG monitoring on tracheal extubation time after anesthesia in general surgical patients under halothane anesthesia. Thus, our present study investigates the effect of BIS versus ETAG monitoring on time to tracheal extubation in general surgical patients receiving halothane and nitrous oxide-based anesthesia.
METHODS
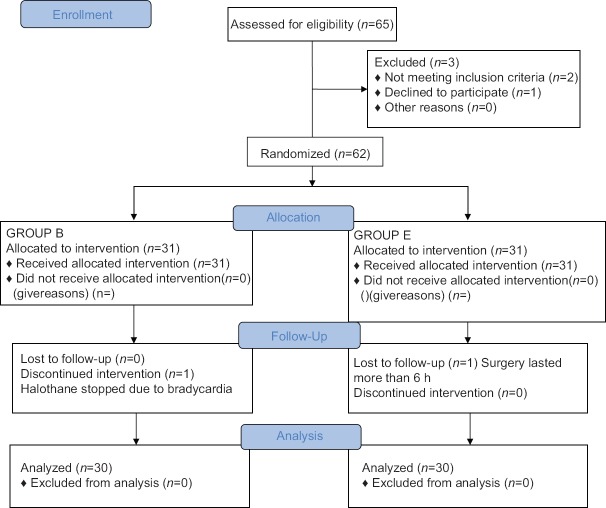
The study was conducted at the Department of Anesthesiology of our college after due permission from the Institutional Ethical Committee and written informed patient consent. It was a randomized controlled double-blind study. Sixty-two patients with the American Society of Anesthesiologists physical status Class 1 or 2 receiving halothane (fluothane (200 ml), Nicholas Piramal India Ltd.) based general anesthesia were randomized to BIS (n = 31) or ETAG (n = 31) guided anesthesia protocols using computerized random number table. Patients refusing for participation in the study, psychiatric patients, chronic users of psychoactive medication, patients with known or suspected electroencephalographic abnormality (e.g., epilepsy, previous brain surgery), patients with deranged liver function, conduction abnormalities or lost in follow-up due to operation time exceeding 6 h or change of anesthetic plan were excluded from study [Figure 1].
Figure 1.
Consort 2010 flow diagram
On arrival in the operation theater, patient's weight, fasting status, consent, and preanesthetic record were checked. Patients were put on the standard monitoring using Ultraview SL 2700 monitor (Spacelabs Healthcare, Issaquah, Washington) comprising body temperature, noninvasive blood pressure, pulse oximetry (SpO2), end-tidal carbon dioxide, heart rate, and electrocardiography, and baseline readings were recorded.
BIS monitoring was initiated using “Quatro” BIS sensor (Aspect Medical System, Newton, Massachusetts) and the patient's awake BIS was recorded. The Spacelabs Healthcare 91482 BISx™ module acquires real-time electroencephalography data and processes it into a BIS number. The MAC values of nitrous oxide and halothane are considered to be additive; therefore, we have taken total MAC as a measure of ETAG concentration. The Spacelabs Healthcare 91518 multigas sidestream analyzer was used to measure ETAG also displaying MAC of the inhalational anesthetic agents in which nitrous oxide is taken into account in the MAC calculations by module. The vaporizer used was Blease Datum L® series halothane vaporizer. The anesthesiologists caring for patients in the ETAG group were using a monitor configuration that omitted BIS number [Figure 2] while those caring for the patients in BIS group were using a monitor that had no MAC value displayed [Figure 3]. Thus, they were blinded to MAC value in BIS group and BIS value in ETAG group. The anesthesiologists were also unaware that extubation time was the endpoint of the study. In BIS group, an audible alarm was set to indicate when the BIS value exceeded 60 or fell below 40. In ETAG group, an audible alarm was set to indicate when the ETAG concentration was outside the range of 0.7 MAC to 1.3 MAC.
Figure 2.
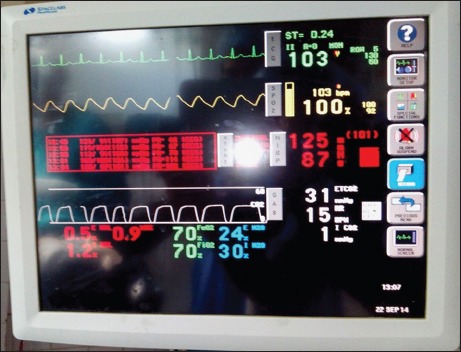
Monitor configuration in end-tidal anesthetic gas group
Figure 3.
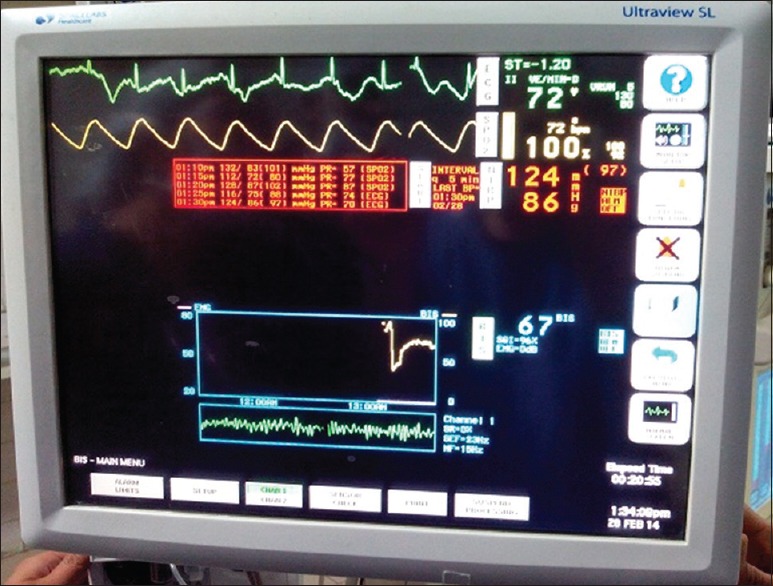
Monitor configuration in bispectral group
Patients were premedicated with intravenous glycopyrrolate (4 µg/kg) and nalbuphine (0.2 mg/kg). Induction was achieved with propofol (2 mg/kg), and intubation was facilitated with rocuronium (0.8 mg/kg) intravenously. Anesthesia was maintained with 60% of nitrous oxide in oxygen and halothane titrated according to respective group protocol along with rocuronium (0.15 mg/kg) as required. Halothane was titrated to maintain a BIS value of 40–60 in BIS group and 0.7–1.3 MAC in ETAG group. All hemodynamic parameters were recorded at 5 min interval until the patient was shifted from the operating room. After the last skin suture, all the anesthetic agents were stopped and after the onset of spontaneous respiration, residual neuromuscular blockade was reversed with neostigmine (0.05 mg/kg) and glycopyrrolate (0.01 mg/kg). Extubation was done when (a) patient followed verbal command, (b) had a sustained head lift for 5 s, and (c) maintained adequate SpO2.
Patient characteristics and variables such as type and duration of surgery and duration of anesthesia (time from induction to skin closure) were documented. The time between anesthetic discontinuation and tracheal extubation was recorded as tracheal extubation time as primary outcome. Any intraoperative or immediate postoperative complication was recorded and managed.
The sample size was calculated assuming a difference of 3 min in time to tracheal extubation in BIS and ETAG group in a recent systematic review,[9] α error of 0.05, and a β error of 0.05 (power of 0.95). Thirty patients per group would be needed to show a significant difference between BIS and ETAG groups. The two groups were compared using Student's t-test, and P < 0.05 was considered statistically significant. Data were processed and analyzed using SPSS Statistics for Windows, version 17.0 (Chicago: SPSS Inc.).
RESULTS
Thirty patients were analyzed in each group, one patient in BIS group was excluded due to change in anesthetic plan as he developed bradycardia and one in ETAG group was excluded as surgery lasted for more than 6 h. The groups were well-matched regarding age, weight, gender, and the American Society of Anesthesiologists status [Table 1]. Type of surgery in our study mainly comprised open cholecystectomy and abdominal hysterectomy. Both groups were comparable regarding type and duration of surgery. The mean duration of anesthesia in BIS group was 1.36 ± 0.35 h while that in ETAG group, it was 1.39 ± 0.32 h [Table 2]. Mean baseline BIS value was 98 and it decreased to <40 after induction. BIS value in Group B was maintained between 40 and 60 during surgery. Whereas in group E mean MAC value increased from 0 to 0.7 after induction and was maintained between 0.7 and 1.3 during surgery. After stopping all anesthetic agents, the values of BIS and MAC returned near to baseline in at the time of extubation [Figure 4]. All hemodynamic parameters remained within normal limits (20% of baseline) throughout the course of anesthesia.
Table 1.
Demographic profile of patients
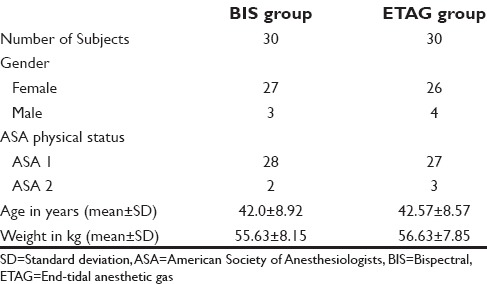
Table 2.
Mean duration of surgery and anesthesia and extubation time in bispectral and end-tidal anesthetic gas group
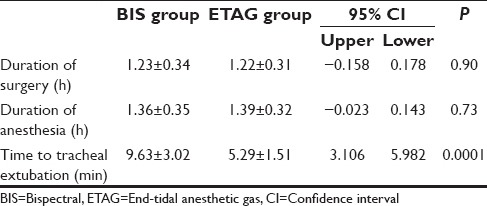
Figure 4.
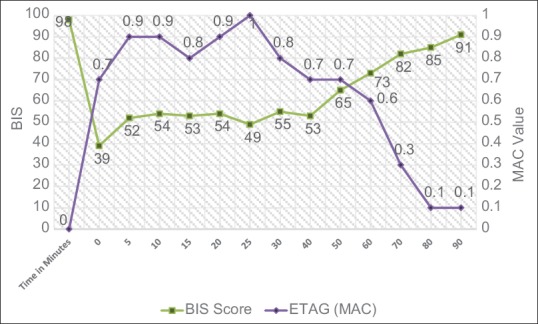
Intraoperative mean bispectral and end-tidal anesthetic gas values in the two study groups
In our study, mean time to tracheal extubation in BIS group was found to be 4.34 min longer than ETAG group with a 95% of confidence interval range of 3.106, 5.982, and P < 0.0001. It was 9.63 ± 3.02 min in BIS group as compared to 5.29 ± 1.51 min in ETAG group. All the patients were extubated in the operating room, and no significant complication was noted during perioperative period in any patient.
DISCUSSION
MAC is commonly used for the titration of volatile anesthetics in clinical practice. MAC value describes mainly the immobilizing potency of the anesthetic agent. To obtain more complete concentration-response curves for the hypnotic effects of various volatile anesthetics, EEG-derived BIS is more specific.
Since the majority of the world's population live in developing countries, halothane remains the most commonly used inhalation anesthetic agent across the world.[2,10] Thus, in our study, we compared the time to tracheal extubation into two groups of patients receiving either BIS- or ETAG-guided titration protocol for halothane-based general anesthesia.
In our study, we found that in general surgical patients, the mean extubation time was significantly prolonged when BIS monitoring was used as compared to ETAG monitoring to titrate halothane. However, Persec et al. performed similar study with sevoflurane and observed a significantly shorter extubation time (17.5 min vs. 75 min, P < 0.001) in the BIS-guided group as compared to ETAG group.[11] On the contrary, Villafranca et al. performed a study in fast-track cardiac surgery using sevoflurane or desflurane. They concluded that compared with management based on ETAG, anesthetic management based on BIS guidance does not strongly increase the probability of earlier tracheal extubation.[12] In another study, authors concluded that the use of intraoperative BIS monitoring during cardiac surgery did not change the time to extubation, ICU LOS, or hospital LOS.[13]
By observing these and other similar studies, we can say that BIS guidance may promote faster recovery if sevoflurane, isoflurane, or desflurane is used, although evidence is equivocal. However, the question is does BIS-guided anesthesia promote faster recovery with halothane too?
In since halothane is still a part of the majority of anesthesia protocols due to its cost-effectiveness at many centers; thus, we have considered halothane for maintenance in our study. Equal MAC of various volatile anesthetic agents may produce different BIS values. Gupta et al. found that at equi-MAC sevoflurane produces lower BIS values as compared to isoflurane, reflecting an agent-specific effect and a deficiency in BIS algorithm for certain agents and their interplay.[14] The effect of halothane on EEG is different from other inhalational agents. Schwab et al. studied the effect of sevoflurane and halothane on BIS values. They concluded that sevoflurane causes a greater decrease in BIS values as compared to halothane at equal MAC multiples. They found that mean BIS value was 54 ± 7 with halothane as compared to 34 ± 6 with sevoflurane at 1 MAC.[15]
A study compared BIS value using halothane and isoflurane at equipotent concentration (1 MAC) and at a reproducible measure of anesthetic effect (awakening). The authors observed that movement to stimulus (as measured by MAC), is a crude measure of the immobilizing effect of anesthesia. The BIS is designed to reflect consciousness and memory formation rather than movement suppression. They also observed that the ratio of MAC-awake to MAC is greater for halothane (MAC-awake/MAC for halothane is 0.5 and for isoflurane 0.4). Halothane has a greater immobilizing effect. They concluded that at equipotent concentrations of halothane and isoflurane BIS valves were significantly greater with halothane and that BIS must be interpreted with caution when using halothane.[16]
Similarly, Bharti and Devrajan compared the BIS values produced by isoflurane and halothane at equal end-tidal MAC concentrations and found that at equi-MAC end-tidal concentrations isoflurane produces lower BIS values than halothane. The BIS values were 54.2 ± 3.7 and 42.4 ± 5.8 at 1 MAC in halothane and isoflurane groups, respectively. They inferred that the BIS values for volatile anesthetics may be drug specific.[17]
Murrell et al. studied the effect of halothane, isoflurane, sevoflurane, and desflurane on the electroencephalogram of the rat. They concluded that halothane causes significantly less depression of cortical activity than the newer inhalant agents at equivalent multiples of MAC and that halothane has a fundamentally different mechanism of action than the other inhalant agents. These studies explain the prolongation of extubation time in BIS-guided group in our study when compared to ETAG group.[18]
However, there are certain limitations of our study. First, the observations cannot be generalized to all types of surgeries and anesthesia protocols. Second, other factors affecting recovery after general anesthesia such as body mass index, blood loss, temperature fluid, and electrolyte balance were not taken into consideration for this study.
We conclude that when halothane is being used, ETAG monitoring promotes earlier extubation of patients as compared to BIS monitoring. Therefore, the added cost of BIS-based protocol to facilitate early extubation in halothane-based anesthesia may not be justified.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Habibollahi P, Mahboobi N, Esmaeili S, Safari S, Dabbagh A, Alavian SM. Halothane-induced hepatitis: A forgotten issue in developing countries: Halothane-induced hepatitis. Hepat Mon. 2011;11:3–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Mahboobi N, Esmaeili S, Safari S, Habibollahi P, Dabbagh A, Alavian SM. Halothane: How should it be used in a developing country? East Mediterr Health J. 2012;18:159–64. doi: 10.26719/2012.18.2.159. [DOI] [PubMed] [Google Scholar]
- 3.Nagella AB, Ravishankar M, Hemanth Kumar VR. Anaesthesia practice and reproductive outcomes: Facts unveiled. Indian J Anaesth. 2015;59:706–14. doi: 10.4103/0019-5049.170028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Monk TG, Saini V, Weldon BC, Sigl JC. Anesthetic management and one-year mortality after noncardiac surgery. Anesth Analg. 2005;100:4–10. doi: 10.1213/01.ANE.0000147519.82841.5E. [DOI] [PubMed] [Google Scholar]
- 5.Johansen JW, Sebel PS. Development and clinical application of electroencephalographic bispectrum monitoring. Anesthesiology. 2000;93:1336–44. doi: 10.1097/00000542-200011000-00029. [DOI] [PubMed] [Google Scholar]
- 6.Avidan MS, Zhang L, Burnside BA, Finkel KJ, Searleman AC, Selvidge JA, et al. Anesthesia awareness and the bispectral index. N Engl J Med. 2008;358:1097–108. doi: 10.1056/NEJMoa0707361. [DOI] [PubMed] [Google Scholar]
- 7.Avidan MS, Jacobsohn E, Glick D, Burnside BA, Zhang L, Villafranca A, et al. Prevention of intraoperative awareness in a high-risk surgical population. N Engl J Med. 2011;365:591–600. doi: 10.1056/NEJMoa1100403. [DOI] [PubMed] [Google Scholar]
- 8.Boztug N, Bigat Z, Akyuz M, Demir S, Ertok E. Does using the bispectral index (BIS) during craniotomy affect the quality of recovery? J Neurosurg Anesthesiol. 2006;18:1–4. doi: 10.1097/01.ana.0000188028.80960.dd. [DOI] [PubMed] [Google Scholar]
- 9.Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2014;6:CD003843. doi: 10.1002/14651858.CD003843.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Totonidis S. A role for trichloroethylene in developing nation anaesthesia. Kathmandu Univ Med J (KUMJ) 2005;3:181–90. [PubMed] [Google Scholar]
- 11.Persec J, Persec Z, Kopljar M, Sojcic N, Husedzinovic I. Effect of bispectral index monitoring on extubation time and analgesic consumption in abdominal surgery: A randomised clinical trial. Swiss Med Wkly. 2012;142:w13689. doi: 10.4414/smw.2012.13689. [DOI] [PubMed] [Google Scholar]
- 12.Villafranca A, Thomson IA, Grocott HP, Avidan MS, Kahn S, Jacobsohn E. The impact of bispectral index versus end-tidal anesthetic concentration-guided anesthesia on time to tracheal extubation in fast-track cardiac surgery. Anesth Analg. 2013;116:541–8. doi: 10.1213/ANE.0b013e31827b117e. [DOI] [PubMed] [Google Scholar]
- 13.Vance JL, Shanks AM, Woodrum DT. Intraoperative bispectral index monitoring and time to extubation after cardiac surgery: Secondary analysis of a randomized controlled trial. BMC Anesthesiol. 2014;14:79. doi: 10.1186/1471-2253-14-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta M, Shri I, Sakia P, Govil D. Comparison of equi-minimum alveolar concentration of sevoflurane and isoflurane on bispectral index values during both wash in and wash out phases: A prospective randomised study. Indian J Anaesth. 2015;59:79–84. doi: 10.4103/0019-5049.151363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schwab HS, Seeberger MD, Eger EI 2nd, Kindler CH, Filipovic M. Sevoflurane decreases bispectral index values more than does halothane at equal MAC multiples. Anesth Analg. 2004;99:1723–7. doi: 10.1213/01.ANE.0000136467.47996.70. [DOI] [PubMed] [Google Scholar]
- 16.Davidson AJ, Czarnecki C. The bispectral index in children: Comparing isoflurane and halothane. Br J Anaesth. 2004;92:14–7. doi: 10.1093/bja/aeh011. [DOI] [PubMed] [Google Scholar]
- 17.Bharti N, Devrajan J. Comparison of bispectral index values produced by isoflurane and halothane at equal end-tidal MAC concentrations. Indian J Anaesth. 2007;51:401–4. [Google Scholar]
- 18.Murrell JC, Waters D, Johnson CB. Comparative effects of halothane, isoflurane, sevoflurane and desflurane on the electroencephalogram of the rat. Lab Anim. 2008;42:161–70. doi: 10.1258/la.2007.06019e. [DOI] [PubMed] [Google Scholar]