Case Report
A 59-year-old woman with newly diagnosed, treatment-naïve hepatitis C presented with right upper quadrant abdominal pain. One day prior, she underwent transjugular liver biopsy to evaluate for cirrhosis. Physical exam revealed stable vital signs, jaundice, scleral icterus, and guarding to right upper quadrant palpation. Liver function tests were consistent, with total bilirubin 11.2 mg/dL, AST 354 U/L, ALT 209 U/L, PT 15.2, and INR 1.2. Hemoglobin was 8.9 g/dL, decreased from baseline of 15 g/dL. Abdominal computed tomography showed a large soft tissue density extending the entire length of the common bile duct (Figure 1). ERCP was performed, finding a dilated CBD greater than 2.5 cm with multiple large, amorphous filling defects (Figure 2). Repeated balloon sweeps revealed blood clots (Figure 3), and a nasobiliary tube was left in place for flushing. Despite this, the patient developed hemorrhagic shock. She underwent angiography, revealing distal hepatic artery laceration and subsequent coil embolization achieved hemostasis. After procedure, hemoglobin and vital signs stabilized. However, on hospital day 12, she again developed severe right upper quadrant pain. Abdominal ultrasound revealed an enlarged gallbladder with a thickened wall and a positive Murphy’s sign. HIDA scan showed nonvisualization of the gallbladder, consistent with blockage of the cystic duct. She underwent laparoscopic cholecystectomy, confirming hemocholecystitis, with a tense gallbladder filled with blood. Histopathology was consistent with cholecystitis (Figure 4). She did well postoperatively and is without any residual clinical sequelae greater than one year later.
Figure 1.
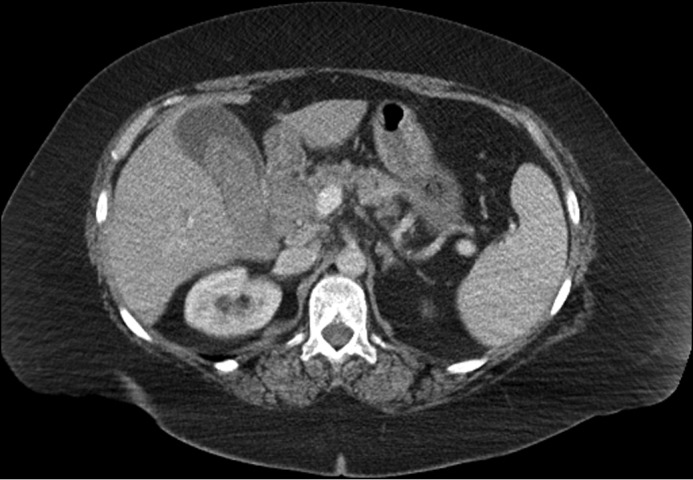
Abdominal computed tomography, interpreted as a large soft tissue density extending along the entire length of the common bile duct, which is mildly enlarged, and soft tissue density within the gallbladder.
Figure 2.

ERCP demonstrating a markedly dilated CBD/CHD, 36 mm in diameter, with multiple large, lucent filling defects within the extrahepatic bile ducts, confirmed to be blood clots on balloon and basket sweeps. The intrahepatic bile ducts are moderately dilated.
Figure 3.
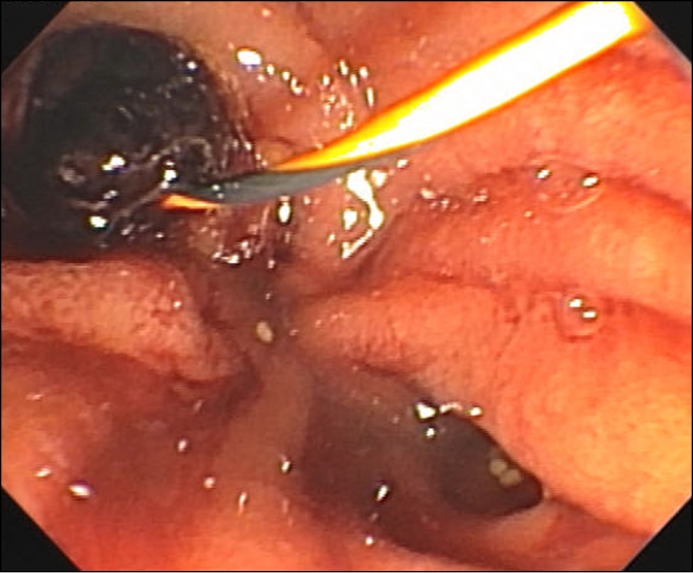
ERCP revealing blood clots at the papilla.
Figure 4.
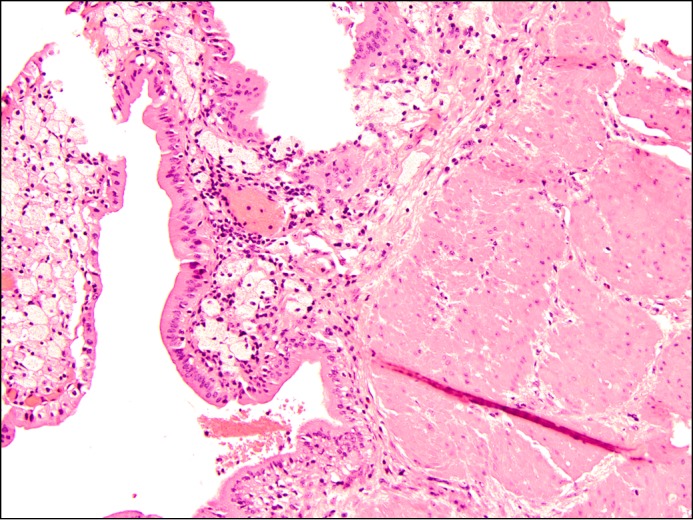
Microscopic examination of the gallbladder demonstrates epithelium with chronic inflammation consistent with chronic cholecystitis (at 40x). During the surgery, it was noted that the gallbladder was filled with blood, but due to rupture of the gallbladder during surgery, no evidence of hemorrhage was identified grossly.
Hemobilia is a rare complication of liver biopsy with an incidence less than 1%, occurring immediately or within 1 week after biopsy.1 Classic clinical presentation with Quincke’s triad (right upper quadrant pain, jaundice, and gastrointestinal hemorrhage) occurs in only 20% of patients with hemobilia.2 Resultant biliary obstruction requires ERCP with sphincterotomy and clot extraction. While half of cases reach hemostasis spontaneously, the remaining cases require embolization.2 Hemocholecystitis following liver biopsy is even more uncommon, with only a few cases reported in the literature.3 When right upper quadrant pain worsens despite proper treatment of hemobilia, hemocholecystitis should be suspected and can be confirmed with a HIDA scan. Without prompt diagnosis, gallbladder perforation can occur in 2%–15% of hemocholecystitis cases as a result of gangrenous cholecystitis.4 Treatment involves early cholecystectomy.
Disclosures
Author contributions: KA Suchniak-Mussari and BA Foreman wrote the manuscript. A. Sharma reviewed and edited the manuscript and obtained the figures. T. Shah contributed the pathology specimen images and description. CE Dye reviewed the manuscript and figures. KA Suchniak-Mussari is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Previous Presentation: This case report was presented at the ACG Annual Scientific Meeting, October 16-21, 2015; Honolulu, Hawaii.
References
- 1.Zhou HB. Hemobilia and other complications caused by percutaneous ultrasound-guided liver biopsy. World J Gastroenterol. 2014; 20(13):3712–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marynissen T, Maleux G, Heye S, et al. Transcatheter arterial embolization for iatrogenic hemobilia is a safe and effective procedure: case series and review of the literature. Eur J Gastroenterol Hepatol. 2012; 24(8):905–9. [DOI] [PubMed] [Google Scholar]
- 3.Edden Y, St Hilaire H, Benkov K, Harris MT. Percutaneous liver biopsy complicated by hemobilia-associated acute cholecystitis. World J Gastroenterol. 2006; 12(27):4435–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plerhoples TA, Lau JN. Hemobilia from transjugular liver biopsy resulting in gallbladder rupture. Dig Dis Sci. 2013; 58(3):630–3. [DOI] [PubMed] [Google Scholar]


