Abstract
This study assessed protective effects of a continuous introduction of safe instruments in terms of reduction of needle stick injuries. The retrospective study analyzed correlations between the increasing proportion of safe instruments and a reduction of the incidence of needle stick injuries linked to such instruments in a German university hospital over 5 years. Incidents declined about 17.6% from 80.3 incidents per 1000 employees to 66.2, associated with an increase in the proportions of injuries due to instruments without protective mechanisms such as scalpels or hypodermic needles by 12.2%. For injuries due to venipuncture cannulae in various surgical and internal medicine departments, there was a negative association between the proportion of safe instruments and the incidence of injuries. For injection needles, portacath needles, and lancets in selected internal medicine departments, the number of injuries also dropped during this study interval. However, there was no clear-cut association with the percentage of safe instruments. This observational study suggests a correlation between the implementation of use of safe instruments and the reduction of needle stick injuries in a case of a graduated implementation. However, the effects are much less pronounced than in previous interventional studies.
Keywords: needle stick injury, safe instrument, infection risk, prevention, occupational infection, implementation
Introduction
Along with contact and airborne transmission incidents, needle stick injuries are among the most frequent health hazards for professional health care workers [1], endangering about 35 million employees in the health sector every day [2]. In a broad sense, needle stick injuries are defined as penetrating injuries of the skin due to pointed or sharp instruments that are contaminated with potentially infectious materials from the patient such as blood or other body fluids irrespective of the presence of a bleeding wound [1]. The incidence of such injuries is estimated to be 3 million incidents per year worldwide [2]. Estimates of health care and general economic costs per needle stick injury vary from 500 euro [3] up to 1600 euro per incident [4]. Most injuries occur during medical procedures or in handling or reassembling of instruments [5].
Despite the frequency of needle stick injuries, professional health care workers frequently have inadequate knowledge about infection risks due to these injuries [6–8]. Needle stick injuries are often considered harmless and ignored owing to time pressure on the job [9, 10]. This pressure seems to be in part avoidable: a previous analysis indicated a reduction of needle stick injuries by 13% by organizational measures alone [11].
Ignorance of infectious disease risks also leads to such risky behavior as recapping of needles, which accounted for 9.3% of needle stick injuries in a Chinese assessment [10] and as many as 22% to 39% in a Georgian study [5]. Safety regulations for the appropriate disposal of contaminated needles were shown to be disobeyed by 28% of European students [12]. Wound disinfection and cleaning under streaming water were performed by as few as 57% and 62% of the injured, respectively, in a Chinese study [10].
Safe instruments with integrated protection mechanisms are considered to reduce needle stick injuries that arise from neglect and ignorance [13]. The security mechanism should be easy to activate (e.g., automatically or single-handedly), and no changes of daily routine procedure should be required [14]. Good acceptance among the employees and suitable training are required to optimize the protective potential of safe instruments [10, 15–17].
Several studies have shown significant protective effects of safe instruments, resulting in a reduction of needle stick injuries by 43% to 93% depending on the study [13, 17–26]. This wide variation depends on such factors as the kind of instrument replaced and the type of novel safe instrument used for replacement as well as the users’ professions and specializations. Automated safety procedures are more effective than manual or semi-automated ones; protection rates in the case of single-handed use are better than for systems requiring both hands [27]. In contrast, manually or semi-automatically operated systems offer more flexible use [15]. Health care professionals from internal medicine departments seem to derive more benefit from safe instruments than do surgeons or pathologists [13]. Acceptance of safe instruments among employees is usually good [13, 16].
Sudden shifts from the use of unsafe instruments to adoption of safe instruments in large health care facilities such as university hospitals are nevertheless exceptions. Usually, continuous shifts, with proportions of safe instruments increasing and proportions of unsafe instruments decreasing, will be the rule. Data from such a shift taking place from 2008 to 2012 at the University Hospital Rostock, Germany, were analyzed in the present study. The aim was to monitor the consequences of the increasing implementation of safe instruments as expressed by reduction of the incidence of needle stick injury at a German tertiary care hospital. Furthermore, we intended to record specific anatomical, temporal, and circumstantial aspects of the injuries to analyze whether a subset of personnel could derive more pronounced benefit from safe instruments.
Methods
Study design
A retrospective longitudinal assessment of needle stick injuries that were reported from 2005 to 2012 at the University Hospital Rostock was performed. Insurance reports as well as registration forms by infectious disease specialists were analyzed.
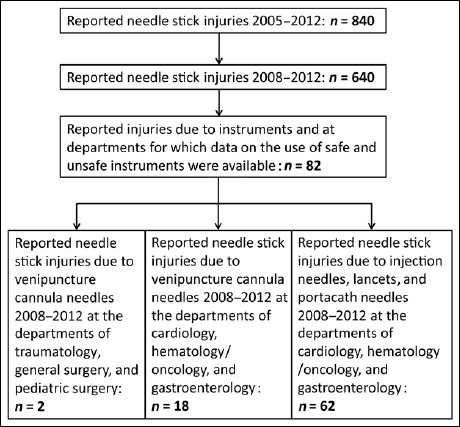
Only the period between 2008 and 2012 was included in the detailed assessment because there was a dramatic increase of reported needle stick injuries between 2005 and 2008. From 2005 to 2007, only low numbers of reported incidents were notified (Fig. 1), followed by an increase of reports between 2007 and 2008, suggesting a reporting bias. Indeed, the reporting procedures for needle stick injuries were changed between 2005 and 2008 in association with a large information campaign. Accordingly, an increase in health care workers’ awareness due to this campaign has to be expected, resulting in an increased readiness to report rather than a real increase in the number of incidents.
Fig. 1.
Distribution of needle stick injuries
Assessment of the study population and the modes of injury
The management of the University Hospital Rostock provided data on numbers and distributions of employees between 2005 and 2012 comprising profession, period of employment, and affiliation to departments of internal medicine, surgery, cardiac surgery, neurology, and anesthesiology/intensive care medicine. The assessed injured personnel were characterized according to the number of injuries, gender, age, profession, professional experience, and department. For injuries associated with professional activities, the parts of the body injured and the injuring instruments were recorded along with a complete analysis of the temporal distribution of the incidents throughout the month and week as well as by time of day and working hours.
Adoption of safe instruments
Safe instruments that were adopted at the University Hospital Rostock during the study interval beginning in 2008 and unsafe instruments that were still available are described in Table 1. The old, unsafe instruments were not replaced suddenly but rather in a slow process depending on existing stockpiles and the availability of the respective products.
Table 1.
Available safe and unsafe venipuncture cannulae, injection needles, portacath needles, and lancets between 2008 and 2012 at the University Hospital Rostock
| Instrument | Manufacturer (and model) | |
|---|---|---|
| Unsafe | Safe | |
| Lancet | Braun (“Solofix Blutlanzetten”) | Owen Mumford (“Unilet”) Sarstedt (“Safety-Lanzette”) |
| Injection needle | Becton Dickinson (“Normkanüle/Microlance”) Sarstedt (“Multifly-Kanüle”) | Becton Dickinson (“Eclipse-Kanüle”) Braun (“Hypodermic Needle-Pro”) |
| Portacath needle | Smiths Medical Ltd. (“Portnadel Gripper”) | Smiths Medical Ltd. (“Gripper Plus Safety”) |
| Venipuncture cannulae | Braun (“Vasofix”) Becton Dickenson (“Venflon Pro”) | Braun (“Vasofix safety”) |
Data on numbers of safe and unsafe instruments delivered from 2008 to the first half-year of 2012 were supplied by the central pharmaceutical facility of the hospital for major departments of internal medicine, i.e., the departments of cardiology, hematology/oncology, and gastroenterology, in which the majority of needle stick injuries occurred. For safe and unsafe venipuncture cannulae, delivery information was available for major departments of both internal medicine and surgery, i.e., the departments of traumatology, general surgery, pediatric surgery, cardiology, hematology/oncology, and gastroenterology. These data were analyzed for correlations with the number of injuries due to the respective kinds of instruments. Of note, the data sets did not indicate whether an injury occurred due to a safe or an unsafe instrument. Further, they did not allow attribution of employees to certain departments, so only absolute numbers of injuries but no yearly incidences per 1000 employees could be assessed. However, the numbers of employees in the departments of internal medicine and surgery remained stable during the study interval from 2008 to 2012.
A survey on compliance with protective procedures ran in parallel and may have biased the study. From the end of 2008 to the middle of 2009, a survey on compliance with protective procedures and medical consequences after needle stick injuries was conducted at the University Hospital Rostock [7]. This survey could have biased the study by additionally increasing the perception and reporting of such incidents. Being aware of this potential bias, we performed calculations omitting the year 2008 and the year 2009, respectively, in addition to the calculations covering the whole study period from 2008 to 2012.
Statistical assessment
Data on reported needle stick injuries and data on delivered safe and unsafe instruments from the central pharmaceutical facility were anonymously entered into a Microsoft Excel 2010 database and further analyzed using the statistical software IBM SPSS statistics 20.
The GraphPad Instat 3.06 software was used for assessments by linear regression of correlation between use of unsafe instruments and the incidence of injuries due to the respective instruments. ANOVA analysis was performed to confirm that the slope differed from zero. P values <0.05 were considered significant.
Ethics
Ethical clearance for the study was obtained from the ethics committee of the University Hospital Rostock (registration number A 2015-0079).
Results
Characterization of the study population
Between 2005 and 2012, 840 injuries were recorded, of which 640 were reported between 2008 and 2012. From the available data, a subset of 82 injuries (Fig. 1) could be further analyzed for correlations with the graduated implementation of the use of safe instruments.
The gender ratio of the injured was considerably skewed toward female sex, with 70.9% of the injured being female. This ratio reflects the general gender composition at the University Hospital Rostock. Between 2005 and 2012, the average proportion of female employees was 73.7%.
Most needle stick injuries happened in the surgical departments and the departments of internal medicine (Table 1). The numbers of employees in the departments of internal medicine and surgery from 2008 to 2012 were 366 ± 24 (standard deviation, SD) and 200 ± 5 (SD), respectively. The standard deviations for this period were thus <7%. For the overall assessment period since 2005, 350 ± 29 employees worked in internal medicine departments and 196 ± 7 employees in surgical departments.
The proportions of needle stick injuries that occurred at the departments of cardiology, hematology/oncology, and gastroenterology amounted to 22.6%, 18.4%, and 15.1% and, thus, in combination to 56.1% of registered incidents in internal medicine departments of the University Hospital Rostock during the study interval. One in six affected staff members reported repeated injuries. The mean age of staff members injured was 32.8 years in a left-shifted distribution. The most frequently affected professionals were nurses, medical doctors, and medical students in descending order, and younger professionals were more often injured than older ones (Table 2).
Table 2.
Characteristics of the injured
| Number of injuries (n = 698) | ||
| Single injury | n = 595 | 85.2% |
| Multiple injuries | n = 103 | 14.8% |
| • 2 Injuries | n = 78 | 11.2% |
| • 3 Injuries | n = 16 | 2.3% |
| • 4 Injuries | n = 6 | 0.9% |
| • 5 Injuries | n = 1 | 0.1% |
| • 6 Injuries | n = 2 | 0.3% |
| Gender (n = 838) | ||
| Male | n = 244 | 29.1% |
| Female | n = 594 | 70.9% |
| Age (n = 832) | ||
| Mean age of injured (±SD) | 32.8 (±10.1) years | |
| Median age of injured | 30.0 years | |
| Minimum/maximum age | 17/64 years | |
| Profession (n = 833) | ||
| Nurse | n = 329 | 39.5% |
| Medical doctor | n = 242 | 29.1% |
| Medical student | n = 211 | 25.3% |
| Medical technical assistant | n = 16 | 1.9% |
| Cleaning staff | n = 16 | 1.9% |
| Others | n = 19 | 2.3% |
| Professional experience in years (n = 554) | ||
| Up to 5 years | n = 277 | 50.0% |
| 6–10 years | n = 93 | 16.8% |
| 11–15 years | n = 50 | 9.0% |
| 15–20 years | n = 44 | 7.9% |
| 21–25 years | n = 38 | 6.9% |
| More than 25 years | n = 52 | 9.4% |
| Department in which the injured person worked (n = 813) | ||
| Surgical department | n = 234 | 28.8% |
| Internal medicine | n = 226 | 27.8% |
| Anesthesiology/intensive care medicine | n = 59 | 7.3% |
| Neurology | n = 48 | 5.9% |
| Orthopedics | n = 37 | 4.6% |
| Dermatology | n = 32 | 3.9% |
| Radiology/radiation therapy | n = 31 | 3.8% |
| Others | n = 146 | 18.0% |
Not all information was available for all data sets (n = 840). SD = standard deviation
Characterization of the modes of injury
The most frequent injury-associated professional activities were surgical procedures, cleaning activities, and the acquisition of blood: injection needles, hypodermic needles, and intravenous cannulae accounted for the highest number of injuries. Peripheral anatomical structures – the fingers with special emphasis to the digits I–III, the palm, and the forearm – were most frequently affected. Although the injuries were equally distributed during the month, their frequency was highest in the morning and during the first working hours on the job and was lower at the weekends. Details are given in Table 3.
Table 3.
Characteristics of the injuries
| Activity during the injury (n = 789) | ||
| Operation | n = 189 | 24.0% |
| Cleaning activity | n = 156 | 19.8% |
| Blood collection | n = 147 | 18.6% |
| Subcutaneous injection | n = 97 | 12.3% |
| Positioning of intravenous cannula | n = 4 | 6.8% |
| Others | n = 146 | 18.5% |
| Part of the body injured (n = 814) | ||
| Finger | n = 726 | 89.2% |
| Digit I | n = 203 | 28.0% |
| Digit II | n = 301 | 41.6% |
| Digit III | n = 123 | 18.5% |
| Digit IV | n = 55 | 7.6% |
| Digit V | n = 31 | 4.3% |
| Palm | n = 53 | 6.5% |
| Forearm | n = 15 | 1.8% |
| Back of the hands | n = 8 | 1.0% |
| Belly | n = 3 | 0.4% |
| Leg | n = 5 | 0.6% |
| Foot | n = 4 | 0.5% |
| Site of injury (n = 800) | ||
| Left body half | n = 480 | 60.0% |
| Right body half | n = 318 | 39.8% |
| Central | n = 2 | 0.3% |
| Injuring instrument (n = 798) | ||
| Injection needle | n = 394 | 49.4% |
| Hypodermic needle | n = 115 | 14.4% |
| Intravenous cannula | n = 69 | 8.6% |
| Scalpel | n = 63 | 7.9% |
| Butterfly cannula | n = 55 | 6.9% |
| Lancet | n = 32 | 4.0% |
| Portacath cannula | n = 12 | 1.5% |
| Others | n = 58 | 7.3% |
| Distribution of injuries throughout the month (n = 840) | ||
| 1st to 5th day | n = 136 | 16.2% |
| 6th to 10th day | n = 132 | 15.7% |
| 11th to 15th day | n = 147 | 17.5% |
| 16th to 20th day | n = 135 | 16.1% |
| 21st to 25th day | n = 133 | 15.8% |
| 26th day to end of the month | n = 157 | 18.7% |
| Distribution of injuries throughout the week (n = 840) | ||
| Monday | n = 166 | 19.8% |
| Tuesday | n = 149 | 17.7% |
| Wednesday | n = 151 | 18,0% |
| Thursday | n = 161 | 19.2% |
| Friday | n = 113 | 13.5% |
| Saturday | n = 45 | 5.4% |
| Sunday | n = 55 | 6.5% |
| Distribution of injuries by time (n = 832) | ||
| 00:00–05:59 a.m. | n = 15 | 1.8% |
| 06:00–08:59 a.m. | n = 158 | 19.0% |
| 09:00–11:59 a.m. | n = 259 | 31.1% |
| 12:00–02:59 p.m. | n = 193 | 23.2% |
| 03:00–05:59 p.m. | n = 109 | 13.1% |
| 06:00–11:59 p.m. | n = 98 | 11.8% |
| Distribution of injuries by working hours since the beginning of the working shift (n = 725) | ||
| 0–01:59 | n = 180 | 24.8% |
| 2–03:59 | n = 170 | 23.5% |
| 4–05:59 | n = 168 | 23.2% |
| 6–07:59 | n = 122 | 16.8% |
| 8–09:59 | n = 57 | 7.9% |
| 10–11:59 | n = 11 | 1.5% |
| ≥12 working hours | n = 17 | 2.3% |
Not all information was available for all data sets (n = 840)
Distribution of unsafe venipuncture cannulae and injuries due to these instruments at the University Hospital Rostock from 2008 to 2012
The percentage of unsafe venipuncture cannulae in use in the representative departments of traumatology, general surgery, pediatric surgery, cardiology, hematology/oncology, and gastroenterology dropped considerably from 2008 to 2010 and remained at a stable low level from 2010 to 2012 (Table 4). The frequency of needle stick injuries due to venipuncture cannulae in selected surgical and internal medicine departments of the University Hospital Rostock showed an analogous development (Table 4). Linear regression identified P values <0.05, suggesting a correlation with a slope different from zero (Table 5). A negative correlation between the percentage of purchased safe venipuncture cannulae and the incidence of injuries due to venipuncture cannulae was identified for the University Hospital Rostock. Considering the bias due to the needle stick survey from 2008/2009, the significance disappeared if the study year 2008 was omitted from the analysis (Table 5). The numbers of reported injuries between 2005 and 2007, when awareness of needle stick injuries was obviously low, resembled the result between 2010 and 2012 when the proportion of safe instruments was high (Table 4).
Table 4.
Distribution of safe and unsafe instruments in selected departments of the University Hospital Rostock and associated reported injuries
| Year | Safe instruments | Unsafe instruments | Injuries* | ||
|---|---|---|---|---|---|
| (Number) | (Percentage, %) | (Number) | (Percentage, %) | (Number) | |
| Proportions of distributed safe and unsafe venipuncture cannulae between 2008 and 2012 at departments of traumatology, general surgery, pediatric surgery, cardiology, hematology/oncology, and gastroenterology, and associated numbers of injuries due to the respective instruments at the respective departments | |||||
| 2005 | 0 | 0.0 | d.n.a. | 100.0 | 0 |
| 2006 | 0 | 0.0 | d.n.a. | 100.0 | 2 |
| 2007 | 0 | 0.0 | d.n.a. | 100.0 | 1 |
| 2008 | 1,922 | 10.4 | 16,513 | 89.6 | 9 |
| 2009 | 11,367 | 52.4 | 10,325 | 47.6 | 5 |
| 2010 | 17,577 | 86.5 | 2,750 | 13.5 | 2 |
| 2011 | 18,899 | 87.1 | 2,800 | 12.9 | 1 |
| 2012 | 9,650 | 84.3 | 1,800 | 15.7 | 3 |
| Proportions of distributed safe and unsafe venipuncture cannulae, injection needles, portacath needles, and lancets between 2008 and 2012 at the departments of cardiology, hematology/oncology, and gastroenterology, and associated number of injuries due to the respective instruments at the respective departments | |||||
| 2005 | 0 | 0.0 | d.n.a. | 100.0 | 6 |
| 2006 | 0 | 0.0 | d.n.a. | 100.0 | 9 |
| 2007 | 0 | 0.0 | d.n.a. | 100.0 | 9 |
| 2008 | 2,125 | 4.3 | 47,133 | 95.7 | 18 |
| 2009 | 18,865 | 32.2 | 39,663 | 67.8 | 29 |
| 2010 | 37,700 | 62.9 | 22,198 | 37.1 | 14 |
| 2011 | 54,814 | 78.8 | 14,768 | 21.2 | 6 |
| 2012† | 30,678 | 84.1 | 5,800 | 15.9 | 13 |
*Documentation did not allow for discrimination of injuries due to safe and unsafe instruments
†Delivery data were available for the first half of the year only d.n.a. = data not assessed
Table 5.
Correlation between the percentage of safe instruments used and the number of injuries based on linear regression beginning from the start of the implementation of use of safe instruments in 2008
| Assessment considering the study bias | Correlation coefficient (r) | r2 | P value | F value | |
|---|---|---|---|---|---|
| Percentage of used unsafe venipuncture cannulae and injuries due to venipuncture cannulae at selected surgical and internal medicine departments | 2008–2012 | –0.9808 | 0.9619 | 0.0032 | 75.23 |
| without 2009 | –0.9803 | 0.9609 | 0.0197 | 49.21 | |
| without 2008 | –0.9088 | 0.8259 | 0.0912 | 9.49 | |
| Percentage of used unsafe venipuncture cannula, injection needles, portacath needles, and lancets and injuries due to these instruments at selected internal medicine departments | 2008–2012 | –0.6489 | 0.4211 | 0.2361 | 2.18 |
| without 2009 | –0.7473 | 0.5584 | 0.2527 | 2.53 | |
| without 2008 | –0.9126 | 0.8329 | 0.0874 | 9.97 |
Distribution of unsafe venipuncture cannulae, injection needles, portacath needles, and lancets in internal medicine departments and injuries due to these instruments in internal medicine departments from 2008 to 2012
The percentage of unsafe venipuncture cannulae, injection needles, portacath needles, and lancets in internal medicine departments of the University Hospital Rostock dropped asymptotically during the whole study interval from 2008 to 2012 (Table 4). For these instruments, there was a pronounced increase of injury reports from 2008 to 2009 (Table 4), correlating well with a survey being conducted on the perception of needle stick injuries [7]. That survey showed particular high response rates from nonsurgical departments. Afterwards, there was a sharp decrease in reports from 2009 to 2010, followed by a steady state at about 10 reported injuries per year due to these instruments in the internal medicine departments assessed (Table 4). Again, this frequency of injuries resembled the situation from 2005 to 2007 when no safe instruments were in use but the awareness was still low. Correlation analysis between delivered safe instruments and associated reported injuries did not show any significant correlation for the whole study interval from 2008 to 2012 (Table 5), irrespective of the omission of the years 2008 or 2009 when the survey on the perception of needle stick injuries [7] was conducted.
Reduction of injuries and shift towards instruments without safety precautions
From 2008 to 2012, the total number of injuries was reduced by 17.6% from 80.3 incidents per 1000 employees to 66.2. For the years between these extremes, the incidences were 76.6, 65.1, and 62.8 per 1000 employees for 2009, 2010, and 2011, respectively. For instruments such as scalpels and hypodermic needles, for which no protective mechanisms were available, the relative proportion of incidents was increased by 12.2% during the study interval. For venipuncture cannulae, injection needles, portacath needles, and lancets, the proportion dropped similarly.
Discussion
The study was conducted to monitor the impact of the increasing implementation of the use of safe instruments at a German tertiary care hospital on the frequency of reported needle stick injuries over a 5-year period from 2008 to 2012. It suggested that the use of safe venipuncture cannulae reduced needle stick injuries due to these instruments. In a subgroup analysis monitoring the adoption of safe venipuncture cannulae, injection needles, portacath needles, and lancets specifically at internal medicine departments, the association between adoption of safe instruments and reduced needle stick injuries seemed considerably weaker. The results might have been influenced by a survey on the perception of needle stick injuries from 2008 to 2009 that showed particular high response rates from nonsurgical departments [7].
During the whole study period, a total of 840 injuries were recorded. With only 200 injuries, an unrealistically low reporting frequency was observed in the years 2005 to 2007, which led to the exclusion of this period from the assessment. Subsequently, reporting procedures were revised and a structured management workflow after needle stick injuries was implemented [7]. This resulted in an increased awareness among employees that was further supported by the increasing adoption of safe instruments since 2008.
The frequency of reported needle stick injuries decreased considerably from 2010 compared with the situation in 2008 and 2009. Within the period from 2008 to 2012, i.e., since the beginning of the implementation of the use of safe instruments and after the change of the reporting procedure for needle stick injuries at the University Hospital Rostock, there was a marked reduction in the total number of injuries by 17.6%. This reduction was considerably lower than found in other studies [13, 17–26]. However, one must keep in mind that the shift from use of unsafe to safe instruments had not yet been completed by 2012 during this real-life observational study, an important difference from previous interventional studies. Even the decrease by 17.6% suggests at least a mild to moderate effect of the adoption of safe instruments.
Injuries due to user error while handling yet-unfamiliar instruments may occur even when safe instruments are being introduced [10, 15, 16, 27]. Indeed, there were individual reports of injuries due to failure to activate the security mechanisms (data not shown), but the low number did not allow for a systematic assessment. Not surprisingly, there was an increase of 12.2% in the relative proportion of injuries due to instruments without safety mechanisms such as scalpels and hypodermic needles during the study interval.
Most injuries were reported by nursing staff (39.5%) and doctors (29.1%) in Rostock, similar to injury patterns reported by two recent Swiss studies [9, 28]. Also in line with previous literature reports from Germany [13, 29] and China [10], a majority of needle stick injuries in Rostock occurred on surgical wards (28.8%) and internal medicine wards (27.8%). However, this is in line with the size of the respective departments of the University Hospital Rostock.
In Rostock, the highest number of needle stick injuries occurred during surgical activities, i.e., when cutting or sewing, with 24% of reported incidents. Strikingly similar high percentages were reported from a Swiss hospital with 30% [28] and a Chinese hospital with 29.8% [10]. Causing nearly a half of the injuries, injection needles were the most frequent instrument of injury penetrating the skin of the employees from Rostock. A retrospective analysis at the University Hospital of Monterrey, Mexico, showed similar results during an assessment period from 2006 to 2011 with 59.1% of injuries due to injection needles, 10.7% due to hypodermic needles, and 8.8% due to lancets [30]. In a Chinese study, as many as 75% of needle stick injuries to nursing trainees were due to injection needles [10], and similar results were shown for Polish nurses in a study from 2005 [31].
The adoption of safe instruments can reduce the infection hazard for employees. This could be most important for injection needles, which provide a bigger reservoir for potentially infectious blood than do hypodermic needles. An American interventional study between 1998 and 2002 showed a reduction of needle stick injuries among the nursing staff by almost 75% [17]. Whereas in anglophone countries nurses largely perform intravenous measures [32, 33], such procedures are typically performed by medical doctors in Germany.
Achievement of optimum protection rates due to use of safe instruments requires adequate staff training, even in the case of automated protection systems [34]. With semi-automated or manually operated systems, training will increase the frequency of activation of the safety mechanisms [35]. Our data suggest that new and young personnel with low professional experience in hospitals are particularly affected by needle stick injuries. Accordingly, these professionals are particularly likely to benefit from training. However, the study does not answer the question whether the observed higher number of injuries in young and less-experienced employees is really due to less skilful work or due to the fact that unpopular and labor-intensive intravenous procedures are likely to be shifted to new coworkers who are usually low-ranking in the hospital hierarchy. In addition, older and professionally more experienced employees could have suffered from needle stick injuries but may have been less prone to report such incidents [7].
Not all kinds of safe instruments are well accepted by health care professionals. The market share of “blunt” hypodermic needles of only 3% is extremely low compared with 90% for safe intravenous catheters [36]. Furthermore, surgeons seem to be less likely to accept safe instruments than professionals from nonsurgical departments [37]. Previous estimations suggested that the use of available and well-accepted safe instruments could potentially avoid about one-third of reported needle stick injuries that occurred in risky medical procedures [38].
As a rarely analyzed feature, the study also focused on the anatomical and temporal distribution of needle stick injuries. The percentage of fingers affected was even higher than in a Chinese study, where injuries of the left digits I and II and the right digit II dominated with 64.3% of injuries [10]. The observed dominance of the left body half presumably results from a quantitative dominance of right-handed professionals who hold the injuring instrument in their right hand. The high frequency of injuries of fingers and hands stresses the importance of wearing gloves, which of course will not prevent injuries due to cutting and sticking but at least protect against careless touching of sharp blood-stained instruments. The markedly decreased frequency of injuries at the weekend coincides with a reduced number of staff and should therefore not be interpreted as a sign of decreased risk of injury. The high frequency of injuries during the first working hours of a shift coincides with the time when blood samples are usually collected, i.e., the time of the highest risk of exposure. An observed highest frequency of injuries during the first working hours and in the morning when risky activities are most frequent was also reported by Polish [31] and Mexican [30] study groups, suggesting a global phenomenon.
The study has a number of limitations. Only reported injuries could be assessed, and a possibly high number of unreported cases may have occurred. During the needle stick survey at the University Hospital Rostock from the end of 2008 to 2009, the documented rate of needle stick injuries was 62% among the survey participants [7]. This suggests a moderate reporting rate compared with other studies that suggested underreporting of between 30% and 90% of the cases [9, 10, 39, 40]. The documentation of injuries was characterized by varying completeness of the data and fluctuating quality. Unfortunately, only few protocols contained exact descriptions of how the accident occurred, e.g., due to failure of safety mechanisms or failure to activate the safety procedure. Further, the implementation of use of safe instruments had been a continuous process. Information was usually not available as to whether safe or unsafe instruments were being used when the accidents occurred. Thus, it was only possible to assess correlations with the proportions of the respective instruments distributed. All estimations were based on the numbers of safe and unsafe instruments distributed by the central pharmaceutical facility of the University Hospital Rostock. Further, exact data on these proportions could be provided only for some representative wards. Of note, the reporting rate prior to 2008 was evidently biased by low awareness. It remains unclear whether this awareness decreased again after the end of the needle stick survey in 2009 [7], making the real impact of safe instruments on the low number of reported injuries since 2010 uncertain.
Conclusion
In spite of potentially confounding effects, the study suggests that the implementation of the use of safe instruments reduces needle stick injuries. However, in case of graduated implementation, i.e., a continuous process of replacing unsafe instruments by safe ones, which will be the standard situation for most large hospitals, this reduction is considerably less pronounced than in previously described interventional studies. Training sessions should support the implementation of the use of safe instruments to achieve optimum results. Organizational improvements might further improve infection hazards. As demonstrated as early as in 1989, the employment of professional phlebotomists, who free overstrained doctors or nurses from time-consuming intravenous procedures, contributes to a reduction of needle stick injuries [41].
Funding Statement
Founding sources The authors report that there was no source of funding.
References
- 1.Hofmann F, Kralj N, Beie M: Needle stick injuries in health care – frequency, causes and preventive strategies. Gesundheitswesen 64, 259–266 (2002) [DOI] [PubMed] [Google Scholar]
- 2.Pruss-Ustun A, Rapiti E, Hutin Y: Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med 48, 482–490 (2005) [DOI] [PubMed] [Google Scholar]
- 3.Wittmann A: Kosten von Nadelstichverletzungen und wirtschaftlicher Nutzen neuer Sicherheitsprodukte. Prakt Arbeitsmed 5, 40-41 (2006) [Google Scholar]
- 4.Wagner-Ferrer D, Hartmann W: Kostenanalyse einer Nadelstichverletzung. Anästhesiologie und Intensivmedizin 47, 63–66 (2006) [Google Scholar]
- 5.Butsashvili M, Kamkamidze G, Kajala M, Morse DL, Triner W, DeHovitz J: Occupational exposure to body fluids among healthcare personnels in Georgia. Occup Med (Lond) 65, 1–7 (2012) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vandijck DM, Labeau SO, Blot SI: Prevention of needle-stick injuries among health care workers. Am J Infect Control 39, 347–348 (2011) [DOI] [PubMed] [Google Scholar]
- 7.Frickmann H, Reisinger E, Mittlmeier T, Schutt G, Podbielski A: Infektionsprophylaxe nach Nadelstichverletzung. Unfallchirurg 115, 708–716 (2012) [DOI] [PubMed] [Google Scholar]
- 8.Kuhn N, Wertli M: Needlestick-injuries among health care professionals: guidelines and reality. Praxis (Bern 1994) 100, 151–158 (2011) [DOI] [PubMed] [Google Scholar]
- 9.Voide C, Darling K, Kenfak-Foguena A, Erard V, Cavassini M, Lazor-Blanchet C: Underreporting of needlestick and sharps injuries among healthcare workers in a Swiss University Hospital. Swiss Med Wkly 142, w13523 (2012) [DOI] [PubMed] [Google Scholar]
- 10.Cheung K, Ching SSY, Chang KKP, Ho SC: Prevalence of and risk factors for needlestick and sharps injuries among nursing students in Hong Kong. Am J Infect Control 40, 997–1001 (2012) [DOI] [PubMed] [Google Scholar]
- 11.Wicker S, Jung J, Allwinn R, Gottschalk R, Rabenau HF: Prevalence and prevention of needlestick injuries among healthcare personnels in a German university hospital. Int Arch Occup Environ Health 81, 347–354 (2008) [DOI] [PubMed] [Google Scholar]
- 12.Salzer HUF, Hoenigl M, Kessler HH, Stigler FL, Raggam RB, Rippel KE, Langmann H, Sprenger M, Krause R: Lack of risk-awareness and reporting behavior towards HIV infection through needlestick injury among European medical students. Int J Hyg Environ Health 214, 407–410 (2011) [DOI] [PubMed] [Google Scholar]
- 13.Wicker S, Gottschalk R, Rabenau HF: Risk of needlestick injuries from an occupational medicine and virological viewpoint. Dtsch Arztebl Int 104, A3102-A3107 (2007) [Google Scholar]
- 14.Adams D, Elliott TS: Safety-engineered needle devices: evaluation prior to introduction is essential. J Hosp Infect 79, 174–175 (2011) [DOI] [PubMed] [Google Scholar]
- 15.Stankovic A: Protection against needlestick injuries: active or passive safety? MLO Med Lab Obs 43, 40/51 (2011) [PubMed] [Google Scholar]
- 16.Adams D, Elliott TS: Impact of safety needle devices on occupationally acquired needlestick injuries: a four-year prospective study. J Hosp Infect 64, 50–55 (2006) [DOI] [PubMed] [Google Scholar]
- 17.Sohn S, Eagan J, Sepkowitz KA, Zuccotti G: Effect of implementing safety-engineered devices on percutaneous injury epidemiology. Infect Control Hosp Epidemiol 25, 536-542 (2004) [DOI] [PubMed] [Google Scholar]
- 18.Orenstein R, Reynolds L, Karabaic M, Lamb A, Markowitz SM, Wong ES: Do protective devices prevent needlestick injuries among health care workers? Am J Infect Control 23, 344–351 (1995) [DOI] [PubMed] [Google Scholar]
- 19.Dale JC, Pruett SK, Maker MD: Accidental needlesticks in the phlebotomy service of the Department of Laboratory Medicine and Pathology at Mayo Clinic Rochester. Mayo Clin Proc 73, 611–615 (1998) [DOI] [PubMed] [Google Scholar]
- 20.Mendelsohn MH, Short LJ, Schechter CB, Meyers BR, Rodriguez M, Cohen S, Lozada J, DeCambre M, Hirschman SZ: Study of a needleless intermittent intravenous-access system for peripheral infusions: analysis of staff, patient and institutional outcomes. Infect Control Hosp Epidemiol 19, 401–406 (1998) [DOI] [PubMed] [Google Scholar]
- 21.Mendelson MH, Lin Chen BY, Solomon R, Bailey E, Kogan G, Goldbold J: Evaluation of a safety resheathable winged steel needle for prevention of percutaneous injuries associated with intravascular-access procedures among healthcare workers. Infect Control Hosp Epidemiol 24, 105–112 (2003) [DOI] [PubMed] [Google Scholar]
- 22.Müller-Barthelmeh R, Buchholz L, Nübling M, Häberle E: Qualitätssicherung bei Nadelschutztechniken. Interventionsstudie zur Senkung der Nadelstichverletzungen durch Instrumente mit Nadelschutztechnik. Arbeitsmedizin Sozialmedizin Umweltmedizin 41, 210–217 (2006) [Google Scholar]
- 23.Whitby M, McLaws ML, Slater K: Needlestick injuries in a major teaching hospital: the worthwhile effect of hospital-wide replacement of conventional hollow-bore needles. Am J Infect Control 36, 180–186 (2008) [DOI] [PubMed] [Google Scholar]
- 24.De Carli G, Puro V, Jagger J: Needlestick-prevention devices: we should already be there. J Hosp Infect 71, 183–184 (2009) [DOI] [PubMed] [Google Scholar]
- 25.Ruiz-Sternberg A, Velez-Van-Meerbeke A, Ruiz-Stern-berg J: Clinical acceptability and ease of use of a safety IV catheter system. Curr Med Res Opin 28, 1381–1387 (2012) [DOI] [PubMed] [Google Scholar]
- 26.Hoffmann C, Buchholz L, Schnitzler P: Reduction of needle stick injuries in healthcare personnel at a university hospital due using safety devices. J Occup Med Tox 8, 20 (2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tosini W, Ciotti C, Goyer F, Lolom I, L’Heriteau F, Abiteboul D, Pellissier G, Bouvet E: Needlestick injury rates according to different types of safety-engineered devices: results of a French multicenter study. Infect Control Hosp Epidemiol 31, 402–407 (2010) [DOI] [PubMed] [Google Scholar]
- 28.Colombo C, Masserey V, Ruef C: Incidence of needlestick injuries and other sharps exposures in Swiss acute care hospitals: results of a sentinel surveillance study. J Hosp Infect 77, 181–183 (2011) [DOI] [PubMed] [Google Scholar]
- 29.Himmelreich H, Rabenau HF, Rindermann M, Stephan C, Bickel M, Marzi I, Wicker S: The management of needle-stick injuries. Dtsch Arztebl Int 110, 61–67 (2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Camacho-Ortiz A, Diaz-Rodriguez X, Rodriguez-Lopez JM, Martinez-Palomares M, La Palomares-De Rosa A, Garza-Gonzalez E: A 5-year surveillance of occupational exposure to bloodborne pathogens in a university teaching hospital in Monterrey, Mexico. Am J Infect Control 41, e85-e88 (2013) [DOI] [PubMed] [Google Scholar]
- 31.Bilski B: Needlestick injuries in nurses – the Poznan study. Int J Occup Med Environ Health 18, 251-254 (2005) [PubMed] [Google Scholar]
- 32.Tintinalli J, Hayden S, Larson J: Emergency department phlebotomist: a failed experiment. Ann Emerg Med 44, 185–186 (2004) [DOI] [PubMed] [Google Scholar]
- 33.Witzel K, Kaminski C, Rauschhardt M, Parzeller M: Die venöse Blutentnahme im klinischen Alltag. Dtsch Med Wochenschr 132, 2495–2499 (2007) [DOI] [PubMed] [Google Scholar]
- 34.Adams D, Elliott TS: Needle protective devices. J Hosp Infect 65, 280 (2007) [DOI] [PubMed] [Google Scholar]
- 35.Alvarado-Ramy F, Beltrami EM, Short LJ, Srivastava PU, Henry K, Mendelson M, Gerberding JL, Delclos GL, Campbell S, Solomon R, Fahrner R, Culver DH, Bell D, Cardo DM, Chamberland ME: A comprehensive approach to percutaneous injury prevention during phlebotomy: results of a multicenter study, 1993–1995. Infect Control Hosp Epidemiol 24, 97–104 (2003) [DOI] [PubMed] [Google Scholar]
- 36.Perry JL, Pearson RD, Jagger J: Infected health care workers and patient safety: a double standard. Am J Infect Control 34, 313–319 (2006) [DOI] [PubMed] [Google Scholar]
- 37.Jagger J, Perry J, Gomaa A, Phillips EK: The impact of U.S. policies to protect healthcare workers from bloodborne pathogens: the critical role of safety-engineered devices. J Infect Public Health 1, 62–71 (2008) [DOI] [PubMed] [Google Scholar]
- 38.Wicker S, Ludwig AM, Gottschalk R, Rabenau HF: Needlestick injuries among healthcare personnels: occupational hazard or avoidable hazard? Wien Klin Wochenschr 120, 486–492 (2008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hofmann F, Wittmann A., Kralj N, Gasthaus K: Immunologischer und sicherheitstechnischer schutz vor HBV-,HCV-und HIV-Virusinfektionen. Anästhesiologie und Intensivmedizin 47, 37–66 (2006) [Google Scholar]
- 40.Au E, Gossage JA, Bailey SR: The reporting of needlestick injuries sustained in theatre by surgeons: are we underreporting? J Hosp Infect 70, 66–70 (2008) [DOI] [PubMed] [Google Scholar]
- 41.McGuff J, Popovsky MA: Needlestick injuries in blood collection staff. A retrospective analysis. Transfusion 29, 693–695 (1989) [DOI] [PubMed] [Google Scholar]


