Abstract
Background: Knowledge about the travel-associated risks of hepatitis A and B, and the extent of pre-travel health-advice being sought may vary between countries.
Methods: An online survey was undertaken to assess the awareness, advice-seeking behaviour, rates of vaccination against hepatitis A and B and adherence rates in Australia, Finland, Germany, Norway, Sweden, the UK and Canada between August and October 2014. Individuals aged 18–65 years were screened for eligibility based on: travel to hepatitis A and B endemic countries within the past 3 years, awareness of hepatitis A, and/or combined hepatitis A&B vaccines; awareness of their self-reported vaccination status and if vaccinated, vaccination within the last 3 years. Awareness and receipt of the vaccines, sources of advice, reasons for non-vaccination, adherence to recommended doses and the value of immunization reminders were analysed.
Results: Of 27 386 screened travellers, 19 817 (72%) were aware of monovalent hepatitis A or combined A&B vaccines. Of these 13 857 (70%) had sought advice from a healthcare provider (HCP) regarding combined hepatitis A&B or monovalent hepatitis A vaccination, and 9328 (67%) were vaccinated. Of 5225 individuals eligible for the main survey (recently vaccinated = 3576; unvaccinated = 1649), 27% (841/3111) and 37% (174/465) of vaccinated travellers had adhered to the 3-dose combined hepatitis A&B or 2-dose monovalent hepatitis A vaccination schedules, respectively. Of travellers partially vaccinated against combined hepatitis A&B or hepatitis A, 84% and 61%, respectively, believed that they had received the recommended number of doses.
Conclusions: HCPs remain the main source of pre-travel health advice. The majority of travellers who received monovalent hepatitis A or combined hepatitis A&B vaccines did not complete the recommended course. These findings highlight the need for further training of HCPs and the provision of reminder services to improve traveller awareness and adherence to vaccination schedules.
Keywords: Travel, vaccination, hepatitis A, hepatitis B, healthcare providers, adherence, awareness
Introduction
Hepatitis A virus (HAV), which is transmitted through the faecal–oral route, causes mild-to-severe liver disease.1 Hepatitis B virus (HBV) is transmitted through sexual or blood-borne routes, or vertically from mother to infant and may lead to chronic liver disease if left untreated.2 Hepatitis A is highly endemic in parts of Africa, Asia and central and South America1,3 with endemicity in many countries shifting from younger to older age groups.4 Hepatitis B is highly endemic in Africa, parts of South America, Eastern Europe, Eastern Mediterranean, South-East Asia, China and parts of the Pacific Islands.2,5
Unvaccinated travellers from low-prevalence countries are at increased risk of hepatitis A and B infection whilst travelling to highly endemic regions for HAV and HBV.6,7 Vaccination against HAV and HBV, with two or three doses of the monovalent vaccines, respectively, or three doses of the combined hepatitis A&B vaccine is recommended by the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) for travellers to endemic areas.8,9 In 2014, about 1.1 billion people travelled abroad.10 Despite undertaking high-risk activities, travellers are often unaware of the potential risk factors for hepatitis A1 and B2 during travel.11–15
Consequently, travellers to regions with high HAV and HBV endemicity may not seek pre-travel health advice or follow recommended vaccination schedules.8,16–18 As awareness may vary between countries, an online survey was conducted to assess awareness of hepatitis A and B vaccines among travellers, differences in pre-travel consulting practices and accessibility of vaccination reminder systems in seven countries.
Methodology
Study Design and Setting
An online survey of 15–20 minutes duration was conducted between August and October 2014 in seven countries: Australia, Canada, Finland, Germany, Norway, Sweden and the United Kingdom (UK). Respondents were recruited through online panels to meet a specific target sample size for each country (Supplementary Material Table S1). The online panels consisted of pre-recruited individuals who had previously agreed to participate in online market research surveys. For this study, an invitation was sent via e-mail and eligibility was assessed using a screening questionnaire.
Questionnaire Design
The survey comprised two questionnaires. The screening questionnaire assessed the eligibility criteria: age, travel history, destinations, number of international trips in the past 3 years, the purpose of their most recent travel, awareness of hepatitis vaccine, sources of healthcare advice and health-related information to assist in hepatitis vaccination decision making and status. As delivery of health services, including pre-travel advice, differs by included country, we included primary care providers and family doctors, practice nurses, walk-in clinic doctors, travel clinic doctors or nurses, pharmacists, Public Health Unit health providers and other specialist doctors in our definition of healthcare provider (HCP).
Upon their responses, the following individuals were eligible to participate in the main questionnaire: individuals aged 18–65 years, residents of the selected countries, travellers to hepatitis A endemic countries in Africa, Asia and South and Central America (defined by the WHO1) in the past 3 years, awareness of hepatitis vaccines, knowledge of their vaccination history with hepatitis A or hepatitis A&B vaccines and if vaccinated, had received it within the last 3 years for non-job-related reasons.
The main questionnaire contained closed and open-ended questions and aimed to determine knowledge gaps in the facilitators and barriers to travellers’ vaccination and an understanding of the awareness level of travel-related risks and protective measures, as in previous studies.19–22 Eligible respondents were asked additional questions related to: awareness of disease severity, knowledge of activities that potentially increase hepatitis A or B risk and whether they had undertaken these activities on previous trips to the selected destinations over the past 3 years using a series of Likert scale agree statements (Supplementary material Text 1).
Vaccinated individuals were asked to report the type of vaccination received (hepatitis A, B, or A&B), adherence (number of doses) and time and primary reason of vaccination. Questions regarding reminder services for vaccination were included. Reasons for non-vaccination prior to travel were collected from unvaccinated individuals. Demographic data included age, gender, country of residence, marital status and highest level of formal education.
Ethical approval was provided by Bellberry Limited in Australia and Quorum Review in Canada, Finland, Germany, Norway, Sweden and UK.
Statistical Analysis
Two datasets are presented: screening and main survey data. For the main questionnaire, a composite score for knowledge of risk activities that could expose a traveller to hepatitis infection was calculated. The following scores were assigned: 0 points = correctly identified all risks, 1–3 points = incorrectly identified some risks. A score was also given for the awareness level of hepatitis A and B risk: 0= complete awareness; 1–3 = moderate level; 4 = very low level.
Aggregate data were analysed overall and at individual country level and by advice-seeking behaviours, vaccination status and schedule adherence (vaccinated only). Elements of the initial analysis were designed before study start; however, much of the analysis was post-hoc. A code frame was developed and applied to the verbatim responses for each open-ended question. Data were analysed using IBM Statistical Package for the Social Sciences (SPSS) and IBM SPSS Data Collection.
Results
Screening Questionnaire
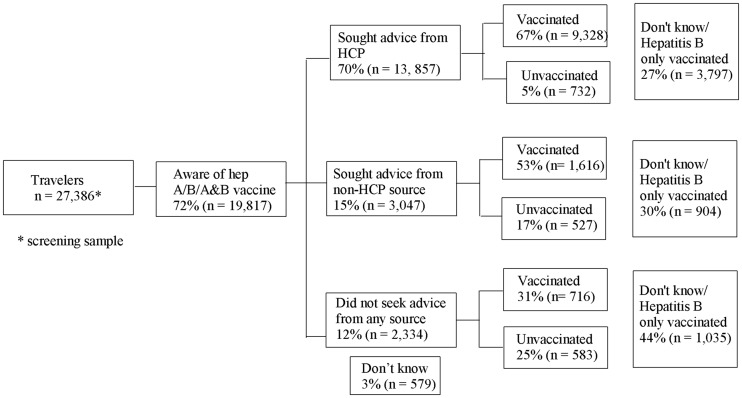
Overall, 27 386 participants aged 18–65 years who had travelled to a hepatitis A or B endemic country in the past 3 years were screened. Of these, 19 817 (72%) were aware of hepatitis A, B or A&B vaccines, 11 660 (59%) reported being vaccinated against hepatitis A or hepatitis A&B; 1842 (9%) were unvaccinated against hepatitis A and 5736 (29%) did not know their vaccination status or had only been vaccinated against hepatitis B (Figure 1).
Figure 1.
Flow diagram of screened individuals and their vaccine awareness, vaccination status and pre-travel health seeking* behaviours. *Sought advice or health information regarding hepatitis A or hepatitis A&B vaccination decision making.
Advice-Seeking Behaviour
Of the 19 817 participants who were aware of hepatitis A, B or A&B vaccines, 70% (n = 13 857) had previously consulted an HCP to help them decide whether to have a hepatitis A or hepatitis A&B vaccine. Advice-seeking was highest in Canada (78%; 2662/3399) and lowest in Sweden (58%; 986/1706) (Table 1). An additional 15% (3047) had sought information only from non-HCPs, 12% (2334) did not seek any advice and 3% (579) did not know if they had sought any advice.
Table 1.
Vaccine uptake of participants by source of advice and by country of residence (N* = 27 386)
| AUS | CAN | FIN | GER | NOR | SWE | UK | Global | ||
|---|---|---|---|---|---|---|---|---|---|
| Aware of hepatitis A/B/A&B | n | 4875/ | 3399/ | 1608/ | 4042/ | 909/ | 1706/ | 3278/ | 19 817/ |
| N | 7226 | 4309 | 1761 | 5022 | 1374 | 2212 | 5442 | 27 386 | |
| (%) | (67%) | (79%) | (91%) | (80%) | (66%) | (77%) | (59%) | (72%) | |
| Sought advice from any HCP | n* | 3470 | 2662 | 1061 | 2755 | 636 | 986 | 2287 | 13 857 |
| (%*) | (71%) | (78%) | (66%) | (68%) | (70%) | (58%) | (70%) | (70%) | |
| Percentage (%) of vaccinated participants by source of HCP advice (N = 9328) | |||||||||
| Primary care providers | 80 | 74 | 40 | 89 | 44 | 17 | 69 | 68 | |
| Travel clinic doctor/nurse | 22 | 35 | 16 | 8 | 32 | 60 | 27 | 26 | |
| Pamphlet/poster in doctor’s waiting room | 15 | 15 | 21 | 16 | 10 | 15 | 15 | 16 | |
| Pharmacist | 13 | 11 | 5 | 12 | 3 | 4 | 13 | 10 | |
| Public Health Unit | 6 | 9 | 24 | 9 | 33 | 8 | 4 | 10 | |
| Pamphlet/poster in pharmacy | 8 | 6 | 11 | 9 | 8 | 6 | 8 | 8 | |
| Walk-in clinic doctor | 12 | 7 | 6 | 3 | 2 | 9 | 11 | 8 | |
| Practice nurse | 3 | 2 | 25 | 1 | 8 | 10 | 18 | 8 | |
| Sought information from non-HCP sources only | n* | 617 | 383 | 428 | 507 | 144 | 507 | 461 | 3047 |
| (%*) | (13%) | (11%) | (27%) | (13%) | (16%) | (30%) | (14%) | (15%) | |
| Percentage (%) of vaccinated participants by source of non-HCP advice (N = 1616) | |||||||||
| Travel related websites | 31 | 45 | 70 | 22 | 35 | 62 | 30 | 45 | |
| Family/friends/colleagues | 42 | 30 | 32 | 40 | 47 | 43 | 36 | 38 | |
| Travel or guide book | 13 | 13 | 27 | 16 | 19 | 12 | 12 | 16 | |
| Pamphlet/poster in doctor’s waiting room | 13 | 8 | 10 | 26 | 7 | 12 | 18 | 14 | |
| Advised by travel agency | 6 | 7 | 15 | 9 | 17 | 9 | 10 | 10 | |
| Pamphlet/poster in pharmacy | 11 | 5 | 7 | 14 | 0 | 7 | 13 | 9 | |
| Ad seen on TV | 4 | 23 | 9 | 4 | 5 | 10 | 4 | 9 | |
| General health websites | 2 | 1 | 7 | 4 | 7 | 2 | 11 | 5 | |
| Discussion with an educator | 11 | 4 | 1 | 5 | 5 | 2 | 8 | 5 | |
N* = total number screened participants.
N = total number screened by country.
n = number of participants who were aware of hepatitis A/B/A&B.
(%) = percentage of participants who were aware of hepatitis A/B/A&B.
n* = number of vaccinated and unvaccinated participants who sought advice from HCP or non-HCP source.
(%*) = percentage of vaccinated and unvaccinated participants who sought advice from HCP or non-HCP source.
HCP = healthcare provider.
Note: the percentages under HCP and non-HCP sources are not mutually exclusive.
Of the vaccinated participants, 9328 (80%) had sought advice from an HCP, 1616 (14%) from a non-HCP and 716 (6%) did not seek any advice. Of the unvaccinated, 732 (40%) had sought advice from an HCP, 527 (29%) from a non-HCP and 583 (32%) did not seek any advice (Figure 1). The vaccination rate of travellers who sought advice from HCPs, non-HCPs and did not seek any advice was 67% (9328/13 857), 53% (1616/3047) and 31% (716/2334), respectively.
Among vaccinated travellers, primary care providers (68%; 6305/9328) were the most consulted HCP sources; the percentage was highest in Germany (89%; 1600/1795). Travel-related websites (45%; 735/1616) were the most consulted non-HCP sources; the percentage was highest in Finland (70%; 226/324). Individuals who sought advice from HCPs also consulted non-HCP sources, e.g. travel websites (35%; 3239/9328) and family/friends (33%; 3077/9328) (Table 1). The vaccination rate of travellers who sought advice from any source was the highest for travel clinics (80%; 2445/3050) and online advertisements (71%; 17/24) (Table 2). The percentages were highest in Finland for travel clinics (95%; 148/156) and online advertisements (88%; 7/8). Among vaccinated travellers consulting HCPs, large differences existed between countries: 89 and 8% consulted primary care providers and travel clinics, respectively, in Germany compared with 17 and 60% in Sweden (Table 1).
Table 2.
Vaccination rate by sources of informationa among vaccinated participants
| Category | HCP (%) | Non-HCP (%) | Category | HCP (%) | Non-HCP (%) |
|---|---|---|---|---|---|
| Primary care providers | 65 | – | Family/friends/colleagues | 67 | 49 |
| Walk in clinic doctor | 63 | – | Travel or guide book | 72 | 56 |
| Practice nurse | 70 | – | General health websites | 67 | 63 |
| Travel clinic doctor or nurse | 80 | – | Discussion with an educator | 59 | 56 |
| Pharmacist | 66 | – | Online discussion | 63 | 70 |
| Public Health Unit | 72 | – | Advertisement seen online | 61 | 71 |
| Pamphlet/poster in pharmacy | 60 | 49 | Advised by travel agency | 70 | 66 |
| Pamphlet/poster in doctor’s waiting room | 65 | 47 | Advertisement seen on TV | 71 | 48 |
| Travel-related websites | 73 | 61 | Information on radio | 49 | 67 |
HCP, healthcare provider.
Base varies according to how many people sought advice from each source.
aFor non-HCP sources, proportion of vaccinated is reported for both HCP sources and those reporting non-HCP sources only (multiple sources of information could have been sought by participant).
Note: the percentages under HCP and non-HCP sources are not mutually exclusive.
Lack of information about vaccination schedules (63%; 1041/1649), previous visits to the country (17%; 277/1649), cost (12%; 199/1649), lack of time (11%; 188/1649) and safety concerns (12%; 206/1649) were the main reasons for not getting vaccinated. The most common reason for non-vaccination across countries was lack of information (Table 3).
Table 3.
The main reasons for not getting vaccinated by proportion of unvaccinated participants by country of residence
| Reason | Australia (N=344) % | Canada (N=320) % | Finland (N=103) % | Germany (N=440) % | Norway (N=58) % | Sweden (N=82) % | United Kingdom (N=302) % | Global (N= 1649) % |
|---|---|---|---|---|---|---|---|---|
| Cost | 9 | 14 | 17 | 14 | 7 | 15 | 10 | 12 |
| Lack of information | 68 | 61 | 62 | 58 | 72 | 57 | 67 | 63 |
| Require reminder | 4 | 2 | 3 | 5 | 2 | 1 | 2 | 3 |
| Safety | 10 | 14 | 8 | 15 | 14 | 18 | 10 | 12 |
| Lack of time | 6 | 18 | 16 | 12 | 9 | 13 | 9 | 11 |
| Othersa | 40 | 32 | 38 | 35 | 38 | 29 | 33 | 35 |
N = number of unvaccinated travellers.
% = percentage of travellers under each category.
aFor example: “I have travelled to that country before”, “It’s my home country/country of birth”, “needle fear”, etc.
Note: the percentages within each country are not mutually exclusive.
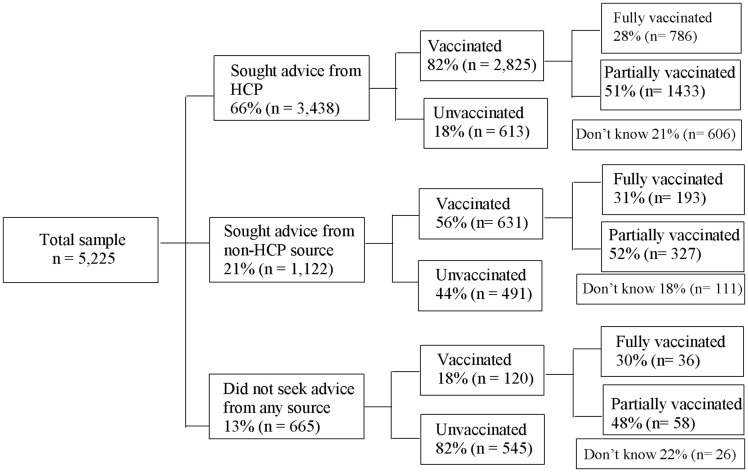
Recently Vaccinated Participants—Main Questionnaire
Of the 5225 participants in the main questionnaire, 3576 had been vaccinated in the past 3 years for the purpose of non-job-related travel, and completed additional questions about demography and adherence rates. A total of 1649 unvaccinated travellers also completed these additional questions (Figure 2). Of these (vaccinated & unvaccinated) respondents, 66% (3438) sought advice from HCPs, 21% (1122) sought advice from non-HCPs and 13% (665) did not seek any advice related to hepatitis vaccination. The rate of advice-seeking was high (83%; 862/1041) in travellers to highly endemic regions.
Figure 2.
Flow diagram of individuals eligible for the main questionnaire, by vaccination status, pre-travel health seeking* and adherence**. *Sought advice or health information regarding hepatitis A or hepatitis A&B vaccination decision making. **Defined as self-reported adherence to the recommended doses including a 2-dose monovalent hepatitis A vaccine schedule and a 3-dose combined hepatitis A&B vaccine schedule.
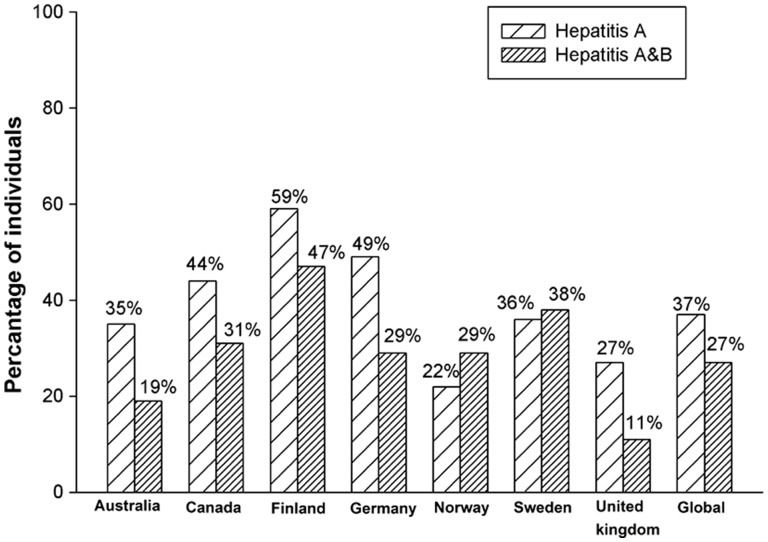
Of vaccinated respondents, 13% (465/3576) were vaccinated against hepatitis A, and 87% (3111/3576) were vaccinated against both hepatitis A and B (Table 4). Overall self-reported adherence to recommended doses was 37% (174/465) for hepatitis A and 27% (841/3111) for hepatitis A&B. Finland had the highest adherence rate for both hepatitis A (59%; 30/51) and hepatitis A&B (47%; 138/296) vaccinations (Figure 3). Adherence rate for hepatitis A vaccination was high in adults aged 51–60 years (52%; 42/81) and for hepatitis A&B in adults aged 41–50 years (31%; 200/641).
Table 4.
Demographic details of the individuals participating in the main study (N = 5225)
| Characteristics | n (%) |
|---|---|
| Age group (years) | |
| 18–30 | 1177 (23) |
| 31–40 | 1180 (23) |
| 41–50 | 1129 (22) |
| 51–60 | 1178 (23) |
| 61–65 | 561 (11) |
| Mean age | |
| All respondents | 43 years |
| Gender | |
| Male | 2235 (43) |
| Female | 2990 (57) |
| Marital status | |
| Live with a spouse or partner | 3666 (70) |
| Region visited most recently | |
| Africa | 1216 (23) |
| Asia | 3219 (62) |
| Central America | 386 (7) |
| South America | 404 (8) |
| Highest level of formal education | |
| Secondary school/Some high school | 346 (7) |
| High school | 911 (17) |
| Technical/trade school/community college | 1033 (20) |
| Some community college/University but did not finish | 542 (10) |
| University degree (eg: Bachelor’s) | 1706 (33) |
| Post graduate degree (eg: Master’s or Ph.D) | 687 (13) |
| Number of children per household | |
| 0 | 3384 (65) |
| 1 | 915 (18) |
| 2 | 727 (14) |
| >3 | 199 (4) |
| Employment status | |
| Employed full-time | 3247 (62) |
| Employed part-time | 852 (16) |
| Not employed | 1126 (22) |
N = number of individuals included in the main survey.
n = number of individuals in each category.
% = percentage of individuals in each category.
Figure 3.
Adherence* to hepatitis A and hepatitis A&B vaccination schedules, by country of residence. *Defined as self-reported adherence to the recommended doses including a 2-dose monovalent hepatitis A vaccine schedule and a 3-dose combined hepatitis A&B vaccine schedule.
Lack of information about vaccination schedules (36%; 662/1818), lack of time (28%; 504/1818) and need for reminders (24%; 428/1818) were the main reasons for partial adherence to vaccination. Of the travellers partially vaccinated against hepatitis A and hepatitis A&B, 61% (135/221) and 84% (1,348/1597), respectively, believed that they had received the recommended number of doses.
The most commonly offered services to remind respondents to get all vaccine doses were vaccination card/booklet and follow-up appointment scheduled at the time of first dose, used by 53% and 45% of the 3576 vaccinated individuals, respectively.
Of all travellers included in the main analysis from each country, the percentage of travellers who were aware of the risk factors (Supplementary Material Table S2) ranged from 10% in Norway (hepatitis A) to 50% in Canada (hepatitis B). The overall level of risk awareness of hepatitis A and B was low among travellers visiting friends and relatives (VFRs) with only 103/764 (13%) and 173/764 (23%) of individuals aware of hepatitis A and B risks, respectively (Table 5). Of the 764 VFRs, 63% were vaccinated; and 63% had sought pre-travel advice from an HCP (Table 5). Adherence rates of VFR travellers for hepatitis A and A&B vaccination were 32% (27/85) and 18% (71/394), respectively. Travellers for volunteer work and school/university/college students had high vaccination rates (93% [115/123] and 91% [61/67], respectively). Adherence rates for hepatitis A and A&B vaccination were 44% (4/9) and 46% (24/52), respectively, among students and 50% (4/8) and 30% (32/107) among volunteers (Table 5).
Table 5.
Health seeking, vaccination and risk awareness among the participants included in the main surveya
| Sought advice from HCP | Hepatitis vaccination rate | Adherence rate hepatitis A | Adherence rate hepatitis A&B | Completely aware of risks for hepatitis A | Completely aware of risks for hepatitis B | |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Total | 5225 (66) | 5225 (68) | 465 (37) | 3111 (27) | 5225 (19) | 5225 (28) |
| Visiting friends/family in my home country | 764 (63) | 764 (63) | 85 (32) | 394 (18) | 764 (13) | 764 (23) |
| Holiday/travelling | 4054 (65) | 4054 (68) | 340 (38) | 2430 (28) | 4054 (19) | 4054 (30) |
| Medical/dental treatment | 30 (60) | 30 (63) | 9 (22) | 10 (40) | 30 (17) | 30 (17) |
| Religious pilgrimage | 33 (70) | 33 (70) | 2 (100) | 21 (14) | 33 (12) | 33 (18) |
| Volunteer work | 123 (84) | 123 (93) | 8 (50) | 107 (30) | 123 (29) | 123 (30) |
| School/university/college trip | 67 (76) | 67 (91) | 9 (44) | 52 (46) | 67 (12) | 67 (21) |
aPeople travelling for work not included in main survey.
n = number of individuals in each category.
% = percentage of individuals in each category.
HCP = healthcare provider.
Note: travellers with a risk score of 0 were considered completely aware of risks for hepatitis A/B.
Discussion
The majority of travellers from the mentioned seven countries had consulted an HCP to help in their hepatitis A or A&B vaccination decision making. However, adherence rates to hepatitis A or A&B vaccination schedules were low. Our data confirm that findings from earlier studies that HCPs, mainly primary care providers, are the most commonly sought source of pre-travel advice.19,20 Nevertheless, previous studies have shown that travellers do not seek adequate health advice regarding HAV and HBV vaccination before travelling.21–24
Vaccination rates were highest when travellers consulted an HCP (67%), compared with non-HCP sources (53%). Of those who did not seek advice from any source for their hepatitis A or A&B vaccination decision making, 31% reported prior vaccination. Although the advice rate sought from primary care providers was higher than travel clinics, the proportion of vaccinated participants was higher among those who sought advice from travel clinics than primary care providers. Lack of information (63%) was the most common factor for non-vaccination. These findings complement recently published hepatitis A and B traveller vaccination data from another Internet-based survey of respondents participating in the National Health and Wellness Survey in France, Germany, Italy, Spain and UK.18 This study showed that frequent travellers had 2.3–2.4 times the odds of being vaccinated relative to non-travellers, and odds of vaccination were 2.5–3.1 times higher among travellers to endemic areas relative to other travellers.18
We observed differences in health-seeking and prevention behaviour between different traveller types. Indeed, as previously found,25 VFRs have an overall lower level of risk awareness, consult less and have lower vaccination and adherence rates, whereas high proportions of school/university/college students (91%) and volunteer workers (94%) are vaccinated. These differences may be attributed to the vaccination advice provided by employers or schools particularly as school students might be vaccinated independently of their risk knowledge.
Overall, the adherence rate was sub-optimal for both hepatitis A and B, but higher for the 2-dose hepatitis A schedule (37%) than for the 3-dose combined hepatitis A&B vaccine (27%). Lack of time (28%) and need for reminder services (24%) were important reasons for non-adherence. We found that travellers would benefit from reminder services to improve their adherence to vaccination schedules.
HCPs have an important role in educating travellers about the risks of HAV and HBV infection and encouraging vaccination.21 HCPs were the key information source for travellers in all surveyed countries. It is therefore important that they keep up-to-date with guidelines to enable the provision of appropriate travel education and facilitate vaccination adherence.24,26–28
A European study showed that due to a lack of understanding of potential travel risks, many individuals travelling within the region wrongly believe that no medical advice or vaccination is required.29 In addition, advice given by HCPs may vary and primary care providers, the main source of advice, may not have specific training in travel medicine. With the increase in travel worldwide, there is a growing need to better support generalist practitioners, by ensuring their access to travel medicine continuing medical education programs, which have been shown to be an effective strategy in improving overall knowledge of travel vaccination practices.30,31
Adhering to recommended vaccination schedules ensures long-term protection for present and future trips.32 Introducing reminder services could help increase adherence rates among travellers, with post-introduction research to evaluate their effectiveness in improving vaccination uptake and adherence.
This study has some limitations. Selection bias could arise because only individuals with internet access (e.g. younger people, those who are able to afford internet, literate and more educated) would have taken the survey. Recall bias may have arisen due to the self-reported nature of the survey. Most cross-sectional studies of travel vaccination rely on self-reported vaccination status and self-report is often the only available information in a pre-travel consultation to assess vaccination history and schedule completeness. Furthermore, country-specific variables, such as cultural and economic factors, were not taken into consideration which might have affected the travellers’ behaviour towards accessing pre-travel advice and vaccination. Finally, the hepatitis A vaccination course was considered incomplete if the booster was not reported by the respondents. However, data suggest that the effectiveness and duration of immunity induced by the booster dose is not impacted from delays of up to at least 6 years after the primary dose.33 It is possible that some participants intended to complete their course but had yet to do so at time of interview.
Conclusion
Travel risk knowledge, behaviour and attitudes can contribute to exposure to vaccine-preventable infectious diseases, including hepatitis A and B. Awareness, pre-travel consulting practices, information seeking and vaccination uptake among travellers differ by country. The low vaccination and adherence rates for both hepatitis A and hepatitis A&B vaccines in our study highlight the need for HCPs to be updated with new tools to improve travellers’ awareness, and to introduce systems that remind travellers to seek advice and obtain recommended vaccinations prior to travel. These measures would improve risk knowledge and adherence and potentially reduce the disease burden among travellers.
Supplementary Data
Supplementary data are available at JTM online.
Funding
This study was supported by GlaxoSmithKline Biologicals SA. GlaxoSmithKline Biologicals SA was involved in all stages of the study conduct and analysis; and paid all costs associated with developing and publishing the manuscript.
Acknowledgements
We thank Varshini Sreenivas (employed by GSK Vaccines) for drafting this manuscript, Julia Donnelly (freelance medical writer c/o GSK Vaccines) and Petronela M. Petrar (XPE Pharma & Sciences c/o GSK Vaccines) for language editing, and Lakshmi Hariharan (employed by GSK Vaccines) and Angeles Ceregido (XPE Pharma & Sciences c/o GSK Vaccines) for assisting with publication management and editorial assistance.
Conflicts of interest
Anita Heywood reports personal fees from the GSK group of companies and has also received investigator grant funding from the GSK group of companies and from Sanofi Pasteur for activities outside the submitted work. Hans Nothdurft reports personal honoraria from the GSK group of companies. Dominique Tessier has received honoraria from the GSK group of companies for participation in this study and for advisory board participation in 2014 outside of the submitted work. Melissa Moodley has no conflict of interest to disclose. Lars Rombo reports fees for lectures from GSK group of companies, Sanofi-Pasteur and Valneva. Cinzia Marano and Laurence De Moerlooze are employees of the GSK group of companies. Laurence De Moerlooze owns restricted shares from the GSK group of companies.
References
- 1.WHO. Hepatitis A Fact sheet 2016. http://www.who.int/mediacentre/factsheets/fs328/en/ (3 March 2016, date last accessed).
- 2.WHO. Hepatitis B Fact sheet 2016. http://www.who.int/mediacentre/factsheets/fs204/en/ (3 March 2016, date last accessed).
- 3.Jacobsen KH, Wiersma ST. Hepatitis A virus seroprevalence by age and world region, 1990 and 2005. Vaccine 2010; 28: 6653–7. [DOI] [PubMed] [Google Scholar]
- 4.Melhem NM, Jaffa M, Zaatari M. et al. The changing pattern of hepatitis A in Lebanese adults. Int J Infect Dis 2015; 30: 87–90. [DOI] [PubMed] [Google Scholar]
- 5.Ott JJ, Stevens GA, Groeger J, Wiersma ST. Global epidemiology of hepatitis B virus infection: new estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine 2012; 30: 2212–9. [DOI] [PubMed] [Google Scholar]
- 6.Wu D, Guo CY. Epidemiology and prevention of hepatitis A in travelers. J Travel Med 2013; 20: 394–9. [DOI] [PubMed] [Google Scholar]
- 7.Keystone JS. Travel-related hepatitis B: risk factors and prevention using an accelerated vaccination schedule. Am J Med 2005; 118: 63S–8S. [DOI] [PubMed] [Google Scholar]
- 8.WHO. International Travel and Health, Vaccine-preventable diseases and vaccines, 2015. http://www.who.int/ith/ITH_chapter_6.pdf?ua=1 (3 March 2016, date last accessed).
- 9.CDC. Travelers' Health. http://wwwnc.cdc.gov/travel/ (3 March 2016, date last accessed).
- 10.World Tourism Organization. Press Release, 2015. http://media.unwto.org/press-release/2015-01-27/over-11-billion-tourists-travelled-abroad-2014 (3 March 2016, date last accessed).
- 11.Spira AM. A review of combined hepatitis A and hepatitis B vaccination for travelers. Clin Ther 2003; 25: 2337–51. [DOI] [PubMed] [Google Scholar]
- 12.Streeton CL, Zwar N. Risk of exposure to hepatitis B and other blood-borne viruses among Australians who travel abroad. J Travel Med 2006; 13: 345–50. [DOI] [PubMed] [Google Scholar]
- 13.Leggat PA, Zwar NA, Hudson BJ. Hepatitis B risks and immunisation coverage amongst Australians travelling to southeast Asia and east Asia. Travel Med Infect Dis 2009; 7: 344–9. [DOI] [PubMed] [Google Scholar]
- 14.Mulhall BP, Hu M, Thompson M. et al. Planned sexual behaviour of young Australian visitors to Thailand. Med J Aust 1993; 158: 530–5. [DOI] [PubMed] [Google Scholar]
- 15.Zuckerman JN, Steffen R. Risks of hepatitis B in travelers as compared to immunization status. J Travel Med 2000; 7: 170–4. [DOI] [PubMed] [Google Scholar]
- 16.CDC. Yellow Book, Chapter 2. The pre-travel consultation, 2016. http://wwwnc.cdc.gov/travel/yellowbook/2016/the-pre-travel-consultation/the-pre-travel-consultation (3 March 2016, date last accessed).
- 17.Baer A, Libassi L, Lloyd JK. et al. Risk factors for infections in international travelers: an analysis of travel-related notifiable communicable diseases. Travel Med Infect Dis 2014; 12: 525–33. [DOI] [PubMed] [Google Scholar]
- 18.Pedersini R, Marano C, De Moerlooze L. et al. HAV & HBV vaccination among travellers participating in the National Health and Wellness Survey in five European countries. Travel Med Infect Dis 2016; 14: 221–32. [DOI] [PubMed] [Google Scholar]
- 19.Heywood AE, Watkins RE, Iamsirithaworn S. et al. A cross-sectional study of pre-travel health-seeking practices among travelers departing Sydney and Bangkok airports. BMC Public Health 2012; 12: 321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walz A, Tschudi P, Badertscher N, Hatz C. Pre travel advice—a study among Swiss general practitioners. Ther Umsch 2013; 70: 313–7. [DOI] [PubMed] [Google Scholar]
- 21.Herbinger KH, Nothdurft HD, Prymula R. Online survey: knowledge about risks, prevention and consequences of infections with HBV among travellers from four European countries. Curr Med Res Opin 2011; 27: 489–96. [DOI] [PubMed] [Google Scholar]
- 22.Zwar N, Streeton CL. Pretravel advice and hepatitis A immunization among Australian travelers. J Travel Med 2007; 14: 31–6. [DOI] [PubMed] [Google Scholar]
- 23.Hamer DH, Connor BA. Travel health knowledge, attitudes and practices among United States travelers. J Travel Med 2004; 11: 23–6. [DOI] [PubMed] [Google Scholar]
- 24.Liu SJ, Sharapov U, Klevens M. Patient awareness of need for hepatitis a vaccination (prophylaxis) before international travel. J Travel Med 2015; 22: 174–8. [DOI] [PubMed] [Google Scholar]
- 25.Leder K, Tong S, Weld L. et al. Illness in travelers visiting friends and relatives: a review of the GeoSentinel Surveillance Network. Clin Infect Dis 2006; 43: 1185–93. [DOI] [PubMed] [Google Scholar]
- 26.Stockwell MS, Hofstetter AM, DuRivage N. et al. Text message reminders for second dose of influenza vaccine: a randomized controlled trial. Pediatrics 2015; 135: e83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aigbogun NW, Hawker JI, Stewart A. Interventions to increase influenza vaccination rates in children with high-risk conditions—a systematic review. Vaccine 2015; 33: 759–70. [DOI] [PubMed] [Google Scholar]
- 28.Taubitz W, Menckhoff S, Nothdurft HD. A recall system improves vaccination compliance. A post card to combat lagging immunization rates. MMW Fortschr Med 2006; 148: 40. [PubMed] [Google Scholar]
- 29.Nothdurft HD, Dahlgren AL, Gallagher EA. et al. The risk of acquiring hepatitis A and B among travelers in selected Eastern and Southern Europe and non-European Mediterranean countries: review and consensus statement on hepatitis A and B vaccination. J Travel Med 2007; 14: 181–7. [DOI] [PubMed] [Google Scholar]
- 30.Kogelman L, Barnett ED, Chen LH. et al. Knowledge, attitudes, and practices of US practitioners who provide pre-travel advice. J Travel Med 2014; 21: 104–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Streit JA, Marano C, Beekmann SE. et al. Travel and tropical medicine practice among infectious disease practitioners. J Travel Med 2012; 19: 92–5. [DOI] [PubMed] [Google Scholar]
- 32.Leder K, Chen LH, Wilson ME. Aggregate travel vs. single trip assessment: arguments for cumulative risk analysis. Vaccine 2012; 30: 2600–4. [DOI] [PubMed] [Google Scholar]
- 33.Ott JJ, Wiersma ST. Single-dose administration of inactivated hepatitis A vaccination in the context of hepatitis A vaccine recommendations. Int J Infect Dis 2013; 17: e939–44. [DOI] [PubMed] [Google Scholar]