Abstract
Objective. To assess benefits of mindfulness meditation and cognitive behavioral therapy (CBT)-based intervention for opioid-treated chronic low back pain (CLBP).
Design. 26-week parallel-arm pilot randomized controlled trial (Intervention and Usual Care versus Usual Care alone).
Setting. Outpatient.
Subjects. Adults with CLBP, prescribed ≥30 mg/day of morphine-equivalent dose (MED) for at least 3 months.
Methods. The intervention comprised eight weekly group sessions (meditation and CLBP-specific CBT components) and 30 minutes/day, 6 days/week of at-home practice. Outcome measures were collected at baseline, 8, and 26 weeks: primary-pain severity (Brief Pain Inventory) and function/disability (Oswestry Disability Index); secondary-pain acceptance, opioid dose, pain sensitivity to thermal stimuli, and serum pain-sensitive biomarkers (Interferon-γ; Tumor Necrosis Factor-α; Interleukins 1ß and 6; C-reactive Protein).
Results. Thirty-five (21 experimental, 14 control) participants were enrolled and completed the study. They were 51.8 ± 9.7 years old, 80% female, with severe CLBP-related disability (66.7 ± 11.4), moderate pain severity (5.8 ± 1.4), and taking 148.3 ± 129.2 mg/day of MED. Results of the intention-to-treat analysis showed that, compared with controls, the meditation-CBT group reduced pain severity ratings during the study (P = 0.045), with between-group difference in score change reaching 1 point at 26 weeks (95% Confidence Interval: 0.2,1.9; Cohen’s d = 0.86), and decreased pain sensitivity to thermal stimuli (P < 0.05), without adverse events. Exploratory analyses suggested a relationship between the extent of meditation practice and the magnitude of intervention benefits.
Conclusions. Meditation-CBT intervention reduced pain severity and sensitivity to experimental thermal pain stimuli in patients with opioid-treated CLBP.
Keywords: Chronic Low Back Pain, Mindfulness Meditation, Cognitive Behavioral Therapy, Long-Term Opioid Therapy
Introduction
Chronic low back pain (CLBP) is common, disabling, costly, and often refractory to currently employed treatments [1–3]. It is the leading non-cancer chronic pain condition for which long-term opioids are prescribed [4]. Although long-term opioids can be helpful, their use is controversial. They are often only marginally effective for chronic pain, and can cause dose-dependent harm including death, hyperalgesia, and addiction [5–8]. These observations highlight the need for alternative treatment modalities, especially for patients affected by refractory CLBP, requiring opioid therapy. Multimodal approaches, including those that incorporate complementary and integrative health approaches (e.g., mind-body modalities) are a recommended strategy for chronic pain, and are of high interest to patients with CLBP [9,10].
Mindfulness meditation (“meditation”) is a safe mind-body modality used to train non-judgmental awareness and attention to present-moment experience (e.g., emotions, thoughts, or bodily sensations such as pain). Originally developed over three decades ago for mitigating chronic pain and stress [11], Mindfulness-Based Stress Reduction has become the most common meditation program used for improving health and well-being in clinical settings [12]. With expert opinions indicating that effectiveness can be enhanced by combining meditation with specialized, evidence-based strategies targeting the specific condition in question [13], “targeted” programs have emerged, many of them combining meditation and elements of other cognitive behavioral therapies (CBT) [14–17]. The combination of meditation and CBT is especially of interest for treating CLBP as CBT is already a component of the prevailing “standard of care” for this condition, and the addition of meditation to CBT may have added benefit [13], even for those with treatment-refractory pain, such as opioid-treated CLBP.
Research shows that meditation-based interventions can improve many medical and mental health problems, including poor sleep, anxiety, depression, and stress reactivity [18]. These symptoms are all common in patients with opioid-treated CLBP and known to affect treatment outcomes in chronic pain [2,18–21]. Meditation has also been related to positive changes in the neural activity in several brain areas involved in adaptive stress, affect, and pain regulation [22,23], and both meditation and CBT have been shown to improve pain coping [24–26]. The beneficial effects of meditation practice can be sustained over time [27].
Although meditation is frequently utilized by patients and clinicians to help alleviate the severity of CLBP and its sequelae, scientific evidence on its efficacy is limited and inconclusive in CLBP, and scarce in opioid-treated chronic pain [14,18,20,28–30]. Only one randomized controlled trial (RCT, N = 115) evaluated the benefits of a meditation-based intervention (Mindfulness-Oriented Recovery Enhancement) among patients with opioid-treated chronic pain conditions, showing both decreased pain severity and desire for opioids at 3 months in the intervention, compared with an active control group [14]. This RCT included patients who reported taking opioid medications on at least 5 days per week, however, the daily opioid dose was not assessed in this trial. Clinical experience and research evidence indicate the medical complexity (e.g., due to co-occurring multiple chronic conditions, especially mental health problems, and opioid-related adverse effects) tend to be opioid dose-dependent [4–7,19]. Therefore, it is important to measure the effects of an intervention in patients treated with moderate-to-high daily doses of opioids, as their therapeutic needs may differ from those who are treated with lower opioid doses, and to evaluate the effects of an intervention on the daily opioid dose in this patient population.
To address this gap, we conducted a pilot RCT (N = 35) to evaluate feasibility, acceptability, safety, and potential efficacy of a targeted meditation-CBT intervention in this patient population. We hypothesized meditation-CBT would safely improve CLBP-related outcomes. This article focuses on the efficacy-related results.
Methods
Trial Design
This pilot study was a two parallel-arm 26-week RCT assessing experience with and effects of a meditation-CBT intervention, “Mindfulness for Chronic Pain,” among patients with CLBP under long-term treatment with daily opioids. Detailed results on the feasibility, accessibility and safety will be presented elsewhere; briefly, the study methods, including the intervention, were found to be feasible, acceptable, and safe (unpublished data, 2015). All participants received usual care for CLBP throughout the study. Those randomly assigned to a control group (N = 14) were eligible to receive the intervention after they completed the study (wait-list control group). Those randomly assigned to a meditation-CBT group (N = 21) received the intervention in addition to their usual care. All participants were evaluated prior to the start of the intervention (baseline), immediately post-intervention (8 weeks), and 18 weeks post-intervention (26 weeks). The study was approved by the University of Wisconsin-Madison (UW) Health Sciences Institutional Review Board and registered with ClinicalTrials.gov. Informed consent was obtained prior to study enrollment.
Participants
Potential participants were adults treated with long-term opioids for CLBP. The methods for participant identification were detailed elsewhere [31]. Briefly, potential participants were identified through the search of the University’s Department of Family Medicine and Community Health electronic health record electronic health record (EHR) data for active patients (who were then sent a letter with an opt-out card), or were referred to the study by their clinicians or a self-referral, using the contact information from the study brochures mailed to the clinicians. Eligibility was determined by self-report, by phone. Eligible participants were at least 21 years old, fluent in English, reported having daily CLBP (lumbosacral area pain or “sciatica” leg pain) that had been treated by a clinician with daily opioid therapy (at least 30 mg/day of morphine-equivalent dose, MED) for at least 3 months, and had the ability to feel thermal sensations in both hands (required for pain sensitivity testing). Ineligibility was due to one or more of the following factors: prior experience with mindfulness meditation training or practice; inability to consent for or reliably participate in study activities; diagnoses of borderline personality, bipolar, or delusional disorders; or current pregnancy. Eligible and interested prospective participants were scheduled for an enrollment meeting.
Interventions
Usual care for CLBP and opioid therapy management was provided to all participants by their regular clinicians. Usual care includes pharmacotherapy, safety, and treatment progress monitoring, treatment agreements, and referral to specialty care, including physical therapy, and complementary therapies for pain and/or mental health [7–10].
Experimental group participants also underwent a manualized training in the meditation-CBT intervention (2 hours per week for 8 weeks), with each session focusing on a specific topic building on previous topics: Session 1—defining mindfulness meditation and auto-pilot, and understanding the relationship between auto-pilot and pain; Session 2—understanding triggers of auto-pilot reactions to pain and stressors, impact of our interpretation of events on thoughts, feelings, and behaviors; Session 3—bringing mindfulness into daily living; Session 4—maintaining mindfulness in challenging pain situations and staying present; Session 5—understanding acceptance and change, and its relation to perception of pain, using mindfulness as a way to cope; Session 6—understanding the connection between thoughts, pain, and auto-pilot reactions to pain; identifying unhealthy thought patterns (e.g., pain catastrophizing); Session 7—reducing vulnerability to pain-triggered auto-pilot reactions; understanding the importance of self-care and balance in life; Session 8—using mindfulness to support life balance; creating a support network; identifying barriers to seeking help. The mindfulness techniques taught during the intervention had a specific therapeutic focus and complemented each other to provide a well-rounded curriculum for learning how to apply mindfulness to coping with challenges associated with chronic pain. Breath meditations and the brief “pain wave surfing” exercise, adapted from the existing “urge surfing” technique [16,17], provided practice in bringing attention to the breath, with a non-judgmental awareness of pain experience, without becoming engaged in catastrophizing, rumination, or other negative thinking about it. Similarly, body scan meditations and mindful movement (walking or stretching) provided practice in interoceptive awareness of pain while engaging in present-moment acceptance and non-judgment of this experience. SABER (Stop, Acknowledge, Breathe, Expand, Respond) mini-meditation, encouraged to use in the context of a challenging pain or other stressful situation, enabled mindful awareness of sensations, emotions, and thoughts, and facilitated a healthy, mindful response to the situation instead of relying on a habitual, often maladaptive, reaction. Lovingkindness meditation enabled practice of kindness and non-judgmental acceptance of self and one's chronic pain. In addition to the weekly sessions, participants were encouraged to practice formal mindfulness meditation (e.g., breath meditation, body scan meditation) at least 6 days per week for at least 30 minutes per day and to engage in daily, brief mindfulness practices through the duration of the study.
The meditation-CBT intervention was led by two psychologists experienced with pain patients (JS, SM), both with over 20 years of personal meditation practice and over 10 years of meditation teaching experience.
Study Procedures and Settings
The enrollment meeting for eligible, interested individuals and the in-person study assessments took place at the UW Clinical Research Unit (CRU) and were conducted by the research coordinator. At the initial meeting, participants were first enrolled, and then completed baseline data collection, before being randomized. Participants in the experimental arm were then scheduled for the intervention, and controls were reminded about being able to receive the intervention after their study completion. Participants received a financial renumeration for their effort to complete the assessments (up to $180) and for travel to attend the intervention sessions (up to $80 in gasoline cards).
Outcome Measures
Details of measures related to feasibility, acceptability, and safety will be described elsewhere. Efficacy-related data were obtained at baseline, 8 weeks, and 26 weeks. Outcome measures were selected based on existing recommendations, including IMMPACT guidelines, for efficacy trials in chronic pain and CLBP [32–35], with pain intensity and CLBP-specific function ratings serving as primary outcomes. During each assessment session, three types of measures were collected: 1) self-reports of pain, function, general psychological and physical health, medication and other substance use; 2) biomarkers (urine specimens for toxicology testing; venous blood for biomarkers); and 3) pain psychophysics.
Self-Reported Measures
Pain intensity was assessed using the four-item pain severity subscale from the validated Brief Pain Inventory [36], inquiring about “current” and past-week “average, worst and least” pain severity, rated on a 11-point Numerical Rating Scale (NRS; 0 = no pain, 10 = “pain as bad as you can imagine”). The NRS is reliable and valid in CLBP [37], with its “minimal important change” (MIC) determined as a 1-point between-group difference [33,34]. An average of the four ratings was used for analyses as recommended for pilot studies [38].
Physical function (disability) was measured using the 10-item validated Oswestry Disability Index (ODI) [39]. The ODI is reliable, responsive to change [35,40], with its total score (0–100) reflecting the percent of CLBP-related disability “today.” A 4- to 10-point score reduction constitutes its MIC [33,34].
Daily opioid dose of prescription-based opioids (both legitimately prescribed and illicitly obtained) for “the past 28 days” were collected via self-report and verified against medication bottle information (medication name, strength per unit, number of units taken per day), using the Timeline Followback (TLFB) method, a validated, reliable measure of daily substance use [41,42]. Doses of all opioids were converted to a MED (mg/day), by multiplying daily dose of a given opioid by the published conversion factors, as described elsewhere [31].
Psychological health was assessed by 1) the 20-item Chronic Pain Acceptance Questionnaire (CPAQ), which is valid and reliable in chronic pain, and measures the propensity toward an acceptance pain-coping (the composite score ranges from 0–120 points, with higher scores = better pain acceptance) [43,44]; 2) the 15-item Mindful Attention Awareness Scale (MAAS) [45], which appears valid and reliable in chronic pain [46], and measures the degree of mindfulness (the composite score is calculated as the average score of all responses, with higher value = higher degree of mindfulness or ability to focus on present-moment experiences); and 3) the 10-item Perceived Stress Scale (PSS) [47–49], which has good reliability and validity, and measures the severity of perceived stress in the “past month” (the composite score ranges from 0 to 40, with higher score = greater perceived stress).
Additional questions on demographics, and duration of back pain and opioid therapy, and home practice of mindfulness meditation were also included.
Biomarkers
To assess the potential biological effects of the intervention, serum levels of C-reactive protein (CRP) and four pain-related, inflammatory cytokines were determined. CRP level was measured by the UW Hospital Laboratory using the nephelometry method (Dimension Vista System, Siemens Healthcare Diagnostics, Inc., Marburg, Germany). Cytokine concentrations were determined in duplicate by multi-array with an electrochemiluminescence platform (Meso Scale Discovery, Gaithersburg, MD). The panel included interleukin-1beta (IL-1ß), tumor necrosis factor-alpha (TNFα), interleukin-6 (IL-6), and interferon-gamma (IFN-γ). The lower limits of cytokine detection were: 0.1, 0.1, 0.2, and 0.4 pg/mL, respectively.
Pain Psychophysical Testing
Pain sensitivity to thermal stimuli was assessed using previously described psychophysical procedures [50,51]. Thermal stimuli were applied to the thenar eminence of the right hand using a Medoc TSA-2001 Thermal Sensory Analyzer with a 900 mm2 Peltier thermode (Medoc Advanced Medical Systems, Ltd., Ramat Yishai, Israel). Participants were randomly presented seven temperatures, each one for 8 seconds, with 1 minute separating each stimulus, ranging from 43 to 49ºC in 1ºC increments. Each temperature was presented twice for a total of 14 stimuli. The baseline temperature for heat testing was 32ºC and the temperature increased at a rate of 8ºC per second. Each stimulus was rated on two separate, validated 0–20 category-ratio scales assessing pain intensity and unpleasantness [52]. Standardized instructions were given to all participants prior to pain sensitivity testing. Participants were not directed to meditate or to utilize any particular coping techniques during psychophysical pain testing.
Other
Participants’ weights and heights were measured at study entry and enabled calculation of a body mass index (BMI), defined as weight (kg)/squared height (m2). For participants in the experimental arm, data on mindfulness meditation practice at home were collected from the participant-completed logs, detailing practice minutes/day and number of practice days/week; these data enabled a calculation of weekly minutes of formal practice. Participants were asked to log their practice minutes daily during the intervention, then log the average weekly values during the follow-up period.
Sample Size and Randomization
The goal was to enroll 10–25 participants per arm (1:1 ratio) to a total of 20–50 participants within the allotted recruitment period prior to the intervention start date. Therefore, 52 randomization envelopes were prepared by a study statistician using the Minitab® Version 12 software and placed in sealed envelopes, blind to the researchers and participants. Envelopes were opened by participants in consecutive order after the completion of baseline assessments.
Blinding
Participants, intervention instructors, and outcome assessors were not blinded to the group assignment.
Statistical Methods
The data were double-entered and managed using the RedCap™ (version 5.1.1) electronic secure database hosted at our institution. Analyses were carried out using the IBM SPSS Statistics (version 21) and R (version 2.15.1) programs. Descriptive statistics summarized the variables and their change at all time points. A two-tailed test, with P < 0.05 was considered statistically significant. Due to the pilot nature of this study, no correction for multiple comparisons was applied.
Primary Analyses
To assess efficacy of the intervention on self-reported and biomarker outcomes, a repeated measures analysis (linear mixed model) evaluated longitudinal between-group effects, using an intention-to-treat (ITT) approach. A “difference score” (score change of a given outcome measure from baseline to the follow-up assessment) was used to account for potential differences between the groups on baseline measures. The linear mixed model included “participant” as a random effect, and produced estimates and 95% confidence intervals (CIs) of the between-group contrasts at each follow-up time point; Cohen’s d additionally assessed the magnitude of effect size for between-group comparisons of longitudinal change. Given the range of thermal stimuli used for pain sensitivity testing, differences in sensitivity were evaluated by estimating and comparing the slope of the relationship between pain ratings and stimuli temperatures for each group using a linear mixed model with a quadratic effect included for temperature, an effect for time, and random effects for subject. The rationale for selecting this model was based on our aim to compare the groups on their overall pain sensitivity rather than sensitivity to individual temperatures, and on the anticipated shape of the curve representing the relationship between pain ratings and stimulus intensity (i.e., temperature). A random quadratic model was fit for each subject and the marginal treatment effects were compared. Maximum likelihood models were fit via the R software package lme4 [53,54], and P values were based on a likelihood ratio test. Post hoc comparisons were carried out at each time point (i.e., 8 and 26 weeks) using a similar approach with a random effect for subject.
Secondary Analyses
Within-group change from baseline to a follow-up assessment was evaluated using estimates and 95% CIs. Comparisons between the groups at a given time point on “difference scores” were carried out using nonparametric Wilcoxon tests for independent samples.
Exploratory analyses assessed the relationship between the changes in outcome measures (pain severity, disability, daily opioid dose) and explanatory variables using a bivariate Spearman correlational analysis and the potential “dose-response” effects of the intervention. To assess the latter, participants were categorized as either “consistent” meditators (≥150 minutes/week of formal meditation practice during at least 2/3 of the study) or “inconsistent” meditators <150 minutes/week of practice during at least 2/3 of the study); the cut off of 150 minutes/week was chosen as it represented over 80% of the recommended weekly practice. Comparison of outcomes between consistent and inconsistent meditators and the controls were conducted using the Mann-Whitney-Wilcoxon Test for independent samples, and within-group comparisons (i.e., change from baseline) were conducted using the related-samples Wilcoxon Signed Rank Test.
Results
Participant Recruitment and Flow
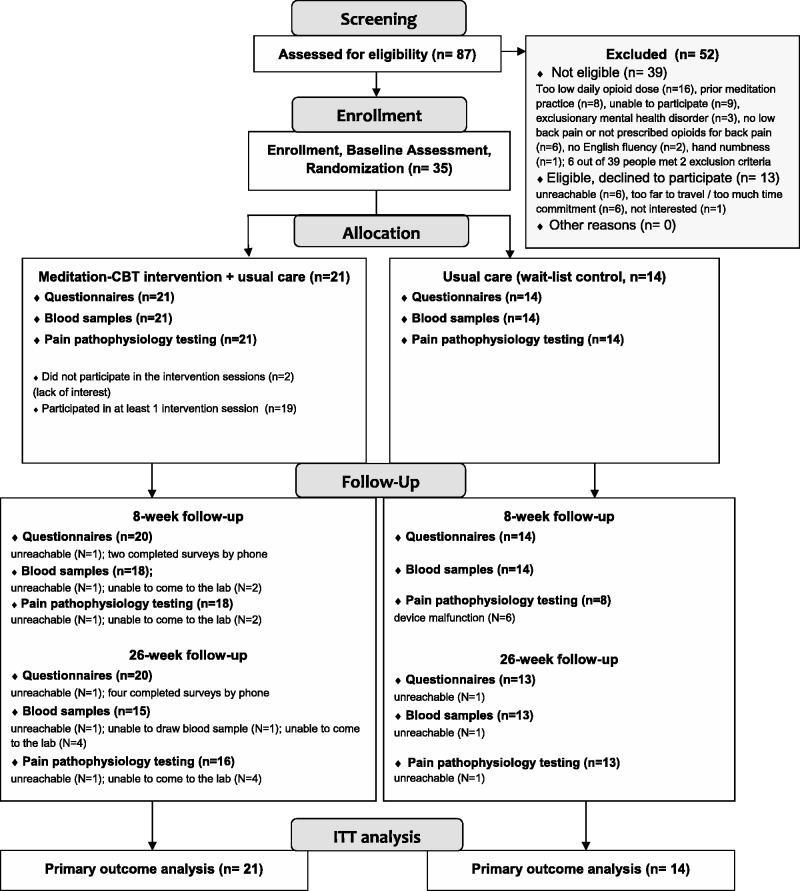
Screening of the EHR database identified 264 potential participants who were then sent an invitation letter with an opt-out card. Forty additional individuals were acquired by patient or clinician referral. Of the total 304 potential participants, 134 opted out (53 by mail, 81 by phone), 84 were unreachable, and 87 were screened. Among the screened adults, 39 were ineligible, 13 were eligible but declined participation, and 35 were eligible and enrolled: 21 in the meditation-CBT and 14 in the control group (Figure 1); this unequal randomization was explained by the fact that 52 randomization envelopes were prepared, but only 35 participants were enrolled during the allotted recruitment/enrollment timeframe (10 weeks, January to March 2013) prior to the study intervention start date in March 2013. No participant withdrew from the study. They all provided baseline and at least one set of follow-up data on primary outcomes. Therefore, primary outcome data from all 35 participants were analyzed (Figure 1). Only anticipated, mild and self-limited mild side effects were reported by the participants.
Figure 1.
Study flow diagram.
Baseline Characteristics
Baseline socio-demographic characteristics of the sample have been presented in detail elsewhere [31]. Briefly, participants were on average 51.8 ± 9.7 years old, predominantly white women. Approximately one-third were unemployed. The majority was receiving disability-related benefits from the Social Security Administration and had an individual annual income not exceeding $15,000 [31]. They reported low back pain for 14.2 ± 10.1 years and were treated with opioid therapy for 7.9 ± 5.7 years [31]. On average, their BMI (33.8 ± 10.8 kg/m2) was in the obese category. The two groups did not differ at baseline on these above factors (P > 0.05).
As shown in Table 1, participants at baseline rated their pain severity at 5.8 ± 1.4 points and all endorsed severe, crippling, or bed-bound back pain-related disability (ODI score: 66.7 ± 11.4). This persistent pain was present despite high, on average, daily dose of opioid therapy (148.3 ± 129.2 mg/day of MED; median: 105.1). At baseline, the meditation-CBT group endorsed more severe pain, a higher degree of mindfulness, and lower perceived stress than controls (P < 0.05). Baseline CRP and cytokine levels (Table 1) and pain sensitivity measures (intensity and unpleasantness ratings to thermal stimuli) did not differ between the groups (P > 0.05).
Table 1.
Baseline clinical characteristics of the sample (N = 35) by group status: self-reported and biomarker outcomes
| Variable | Total (N = 35) | Meditation-CBT group (N = 21) | Control group (N = 14) | P value1 |
|---|---|---|---|---|
| Self-reported outcomes | ||||
| Pain Intensity (Brief Pain Inventory), averaged pain score2 | ||||
| mean (SD) | 5.8 (1.4) | 6.3 (1.2) | 4.9 (1.1) | 0.001 |
| median (25–75%) | 5.5 (5.0; 6.5) | 6.3 (5.5; 7.4) | 5.0 (4.4; 5.3) | |
| Physical Function (Oswestry Disability Index), total score | ||||
| mean (SD) | 66.7 (11.4) | 68.1 (9.3) | 64.5 (14.1) | 0.434 |
| median (25–75%) | 68.0 (58.0; 74.0) | 68.0 (61.1; 78.0) | 67.0 (50.8; 73.5) | |
| Opioid Dose (morphine-equivalent dose), mg/day | ||||
| mean (SD) | 148.3 (129.2) | 166.9 (153.7) | 120.3 (76.9) | 0.654 |
| median (25–75%) | 105.1 (43.3; 210.0) | 105.1 (52.0; 246.1) | 120.8 (35.3; 197.3) | |
| Pain Acceptance (Chronic Pain Acceptance Questionnaire), total score | ||||
| mean (SD) | 54.8 (19.0) | 56.2 (19.4) | 52.6 (18.9) | 0.778 |
| median (25–75%) | 56.0 (47.0; 65.0) | 56.0 (45.0; 66.0) | 54.5 (42.5; 65.5) | |
| Degree of Mindfulness (Mindful Attention and Awareness Scale), total score | ||||
| mean (SD) | 4.3 (0.9) | 4.7 (0.8) | 3.7 (0.9) | 0.002 |
| median (25–75%) | 4.4 (3.5; 5.1) | 4.9 (4.1; 5.2) | 4.0 (3.0; 4.5) | |
| Perceived Stress (Perceived Stress Scale), total score | ||||
| mean (SD) | 18.9 (8.1) | 16.4 (7.9) | 22.6 (7.1) | 0.020 |
| median (25–75%) | 18.0 (14.0; 25.0) | 16.0 (10.5; 22.5) | 22.0 (18.8; 26.5) | |
| Biomarkers | ||||
| Interleukin-1ß, pg/mL | ||||
| mean (SD) | 0.4 (1.2) | 0.6 (1.5) | 0.1 (0.1) | 0.293 |
| median (25–75%) | 0.1 (0.1; 0.2) | 0.1 (0.1; 0.2) | 0.1 (0.1; 0.1) | |
| Interleukin-6, pg/mL | ||||
| mean (SD) | 2.5 (2.9) | 3.0 (3.5) | 1.8 (1.3) | 0.434 |
| median (25–75%) | 1.8 (0.9; 3.2) | 2.0 (1.0; 3.5) | 1.6 (0.6; 2.9) | |
| Interferon-γ, pg/mL | ||||
| mean (SD) | 10.0 (6.3) | 10.4 (7.1) | 9.4 (5.1) | 0.702 |
| median (25–75%) | 9.4 (5.3; 11.7) | 9.7 (5.2; 13.1) | 9.4 (5.1; 11.1) | |
| Tumor Necrosis Factor-α, pg/mL | ||||
| mean (SD) | 5.6 (4.3) | 5.0 (2.3) | 6.4 (6.2) | 1.000 |
| median (25–75%) | 5.0 (3.2; 6.7) | 5.0 (3.6; 6.3) | 4.7 (2.4; 7.7) | |
| C-Reactive Protein, mg/dL | ||||
| mean (SD) | 1.3 (2.2) | 1.8 (2.6) | 0.5 (0.7) | 0.278 |
| median (25–75%) | 1.0 (0.00; 1.0) | 1.0 (0.00; 2.0) | 0.00 (0.00; 1.0) | |
1P < 0.05 (Mann-Whitney-Wilcoxon Test for between-group comparisons).
2Average of “usual, worst, least, and current” pain ratings.
Primary Analyses—Between-Group Differences over Time
ITT repeated measures analysis evaluated longitudinal changes in outcomes, providing information on the efficacy of the intervention.
Self-Reported Outcome Measures
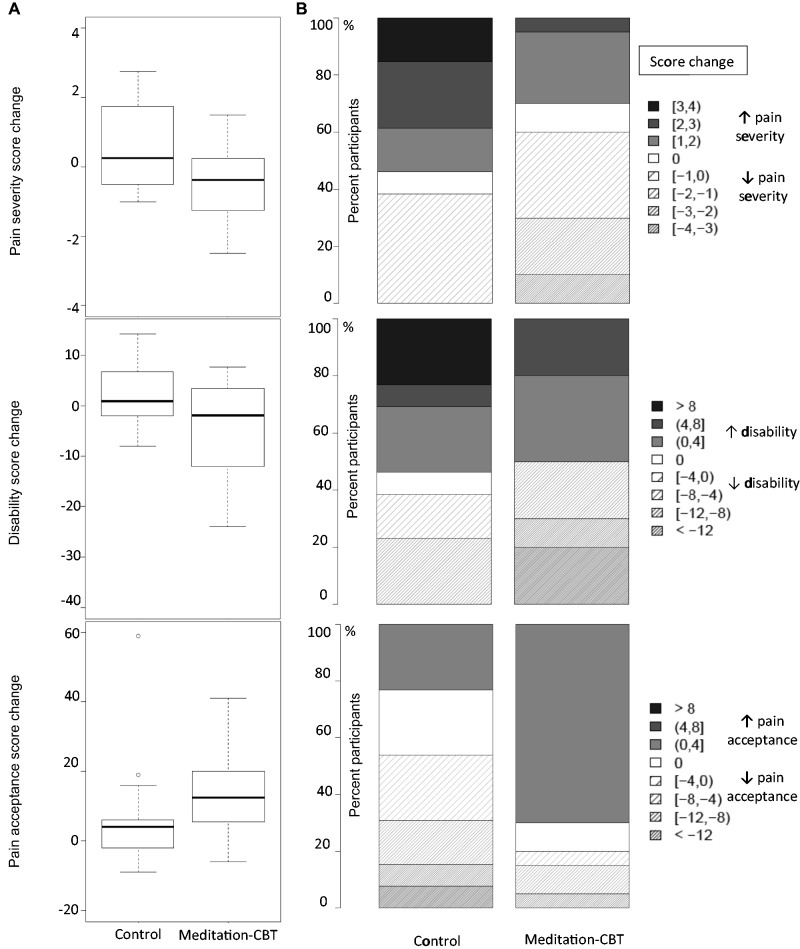
Self-reported outcome measures (Table 2 ): Compared with controls, the meditation-CBT improved the averaged pain ratings across the study (P = 0.045; Figure 2 ); on average, the meditation-CBT reduced the pain score by 8% at both 8 and 26 weeks, while the pain scores in the control group increased by 8% at 8 weeks and 10% at 26 weeks, compared with baseline. The between-group difference in score change reached 1 point at 26 weeks (95% CI: 0.2, 1.9; Cohen’s d = 0.86). No other statistically significant between-group differences were noted over time (P > 0.05) in self-reported measures, although the between-group changes in physical function and pain acceptance scores trended in the hypothesized direction (Figure 2).
Table 2.
Findings from outcome analyses comparing the change in self-reported and biomarker measures between the meditation-CBT and control groups
| Control group compared with meditation-CBT group | P value (repeated measures analysis) | |
|---|---|---|
| Self-reported outcomes | ||
| Brief Pain Inventory, averaged pain | ||
| baseline to 8 weeks, mean (95% CI), n = 34 | 0.9 (0.01; 1.7) | 0.045 |
| Cohen’s d | 0.69 | |
| baseline to 26 weeks, mean (95% CI), n = 33 | 1.03 (0.2; 1.9) | |
| Cohen’s d | 0.86 | |
| Oswestry Disability Index, total score | ||
| baseline to 8 weeks, mean (95% CI), n = 34 | 1.9 (−5.5; 9.3) | 0.209 |
| Cohen’s d | 0.15 | |
| baseline to 26 weeks, mean (95% CI), n = 33 | 6.5 (−1.0; 14.0) | |
| Cohen’s d | 0.68 | |
| Morphine Equivalent Dose, mg per day | ||
| baseline to 8 weeks, mean (95% CI), n = 34 | 5.7 (−34.3; 45.7) | 0.842 |
| Cohen’s d | 0.16 | |
| baseline to 26 weeks, mean (95% CI), n = 33 | 9.9 (−30.3; 50.1) | |
| Cohen’s d | −0.03 | |
| Chronic Pain Acceptance Questionnaire, total score | ||
| baseline to 8 weeks, mean (95% CI), n = 34 | −2.7 (−13.0; 7.6) | 0.471 |
| Cohen’s d | −0.24 | |
| baseline to 26 weeks, mean (95% CI), n = 33 | −5.3 (−15.7; 5.0) | |
| Cohen’s d | −0.42 | |
| Mindful Attention and Awareness Scale, total score | ||
| baseline to 8 weeks, mean (95% CI), n = 34 | 0.3 (−0.2; 0.9) | 0.479 |
| Cohen’s d | 0.45 | |
| baseline to 26 weeks, mean (95% CI), n = 32 | 0.1 (−0.4; 0.7) | |
| Cohen’s d | 0.19 | |
| Perceived Stress Scale, total score | ||
| baseline to 8 weeks, mean (95% CI), n = 34 | −0.4 (−5.2; 4.4) | 0.986 |
| Cohen’s d | -0.06 | |
| baseline to 26 weeks, mean (95% CI), n = 33 | −0.03 (−4.9; 4.8) | |
| Cohen’s d | −0.05 | |
| Biomarkers | ||
| Interleukin-1ß, pg/mL | ||
| baseline to 8 weeks, mean (95% CI), n = 32 | −0.3 (−0.8; 0.2) | 0.196 |
| Cohen’s d | −0.51 | |
| baseline to 26 weeks, mean (95% CI), n = 28 | −0.04 (−0.6; 0.5) | |
| Cohen’s d | 0.05 | |
| Interleukin-6, pg/mL | ||
| baseline to 8 weeks, mean (95% CI), n = 32 | 1.2 (−0.4; 2.7) | 0.126 |
| Cohen’s d | 0.53 | |
| baseline to 26 weeks, mean (95% CI), n = 28 | 0.2 (−1.3; 1.8) | |
| Cohen’s d | −0.47 | |
| Interferon-γ, pg/mL | ||
| baseline to 8 weeks, mean (95% CI), n = 32 | −1.1 (−6.6; 4.4) | 0.717 |
| Cohen’s d | −0.16 | |
| baseline to 26 weeks, mean (95% CI), n = 28 | −2.1 (-8.0; 3.7) | |
| Cohen’s d | −0.33 | |
| Tumor Necrosis Factor-α, pg/mL | ||
| baseline to 8 weeks, mean (95% CI), n = 32 | 2.6 (−3.2; 8.4) | 0.400 |
| Cohen’s d | 0.34 | |
| baseline to 26 weeks, mean (95% CI), n = 28 | 3.3 (−2.5; 9.2) | |
| Cohen’s d | 0.38 | |
| C-Reactive Protein, mg/dL | ||
| baseline to 8 weeks, mean (95% CI), n = 32 | 1.0 (−0.3; 2.2) | 0.220 |
| Cohen’s d | 0.48 | |
| baseline to 26 weeks, mean (95% CI), n = 28 | 0.8 (−0.4; 2.1) | |
| Cohen’s d | 0.34 | |
Results for between-group difference in change from baseline to 8- or 26-week follow-up are presented as mean (95% Confidence Interval, CI) and Cohen’s d effect size. P value refers to the results of repeated measures analysis (linear mixed model), comparing the change in outcomes between the groups from baseline through 26 weeks.
Figure 2.
Change in pain severity, disability, and pain acceptance ratings from baseline to 26 weeks by group status (N = 35): (A) Box-plot presentation. (B) Percentage of participants reporting a given score change.
Biomarker Profile
Biomarker profile (Table 2): Repeated measures analysis did not indicate statistically significant between-group differences in CRP or cytokine levels over time.
Pain Psychophysical Testing
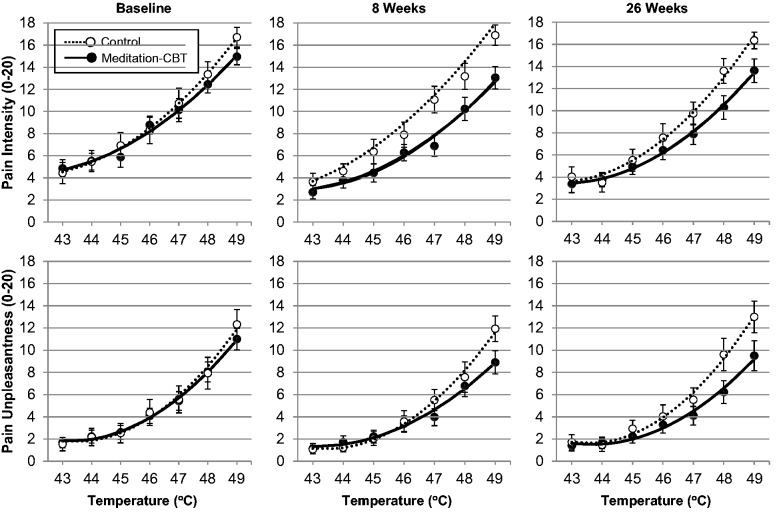
One participant in the meditation-CBT arm declined the pain sensitivity testing at all time points. The remaining 34 participants provided baseline pain sensitivity data; among them, 22 participants (15 meditation-CBT, seven control) completed both follow-up testing, and 11 (four meditation-CBT, seven control) completed either the 8- or 26-week testing (Figure 1). Using a linear mixed model, the overall test of treatment effect for intensity at any follow-up was statistically significant (P = 0.0011). For unpleasantness, the overall test of treatment effect at any follow-up was statistically significant (P < 0.0001). As shown in Figure 3, a significant difference in the slopes of the quadratic functions estimating the relationship between stimulus intensity (temperature) and pain ratings was found at 8 weeks between the two groups for both pain intensity (P = 0.024) and unpleasantness (P = 0.003). The difference indicated reduced pain sensitivity in the meditation-CBT group. The benefit conveyed by the slopes was maintained at 26 weeks, with significant differences between groups still evident for both pain intensity (P = 0.049) and unpleasantness (P = 0.028).
Figure 3.
Comparison of average pain intensity and unpleasantness ratings of thermal stimuli between meditation-CBT (N = 20) and control (N = 14) participants at baseline, 8, and 26 weeks. The lines represent the average estimate of quadratic function for the relationship between stimulus temperatures and pain ratings; the markers represent the average pain rating at each temperature with error bars for the standard error of the mean (SEM). Significant differences between the groups for the slope of the quadratic function were observed for pain intensity and unpleasantness ratings at both 8 and 26 weeks (P < 0.05).
Secondary Analyses—Within-Group Change over Time
To help explain findings of the outcome analyses, a longitudinal within-group change from baseline to each of the two follow-up assessments was evaluated for self-reported and biomarker measures (Table 3). Compared with baseline, both groups showed improvements in pain acceptance ratings at 26 weeks (increase by 14.7 points [95% CI: 8.1, 21.2] in the meditation-CBT, and by 9.3 points [95% CI: 1.3, 17.4] in the control group). The CRP levels in the meditation-CBT group, but not controls, were lower at 8 weeks (-0.9 mg/dL, 95% CI: -1.7, -0.1). No other statistically significant longitudinal within-group changes were noted.
Table 3.
Findings from secondary analyses (linear mixed model) evaluating longitudinal change (Δ) within each group from baseline to 8- and 26-week follow-up in self-reported and biomarker measures
| Variable | Meditation-CBT N = 21 | Control group N = 14 |
|---|---|---|
| Self-reported outcomes | ||
| Pain Intensity (Brief Pain Inventory), averaged pain score | ||
| baseline to 8 weeks, mean (95% CI) | −0.5 (−1. 1; 0.03) | 0.4 (−0.3; 1.0) |
| baseline to 26 weeks, mean (95% CI) | −0.5 (−1.1; 0.02) | 0.5 (−0.2; 1.2) |
| Physical Function (Oswestry Disability Index), total score | ||
| baseline to 8 weeks, mean (95% CI) | −2.4 (−7.2; 2.3) | −0.6 (−6.2; 5.1) |
| baseline to 26 weeks, mean (95% CI) | −5.0 (−9.7; −0.2) | 1.6 (−4.3; 7.4) |
| Morphine Equivalent Dose, mg per day | ||
| baseline to 8 weeks, mean (95% CI) | −7.1 (−32.5; 18.3) | −1.4 (−32.3; 29.5) |
| baseline to 26 weeks, mean (95% CI) | −10.1 (−35.5; 15.2) | −0.2 (−31.4; 30.9) |
| Chronic Pain Acceptance Questionnaire, total score | ||
| baseline to 8 weeks, mean (95% CI) | 5.9 (−0.6; 12.4) | 3.2 (−4.7; 11.2) |
| baseline to 26 weeks, mean (95% CI) | 14.7 (8.1; 21.2) | 9.321 (1.3; 17.4) |
| Mindful Attention and Awareness Scale, total score | ||
| baseline to 8 weeks, mean (95% CI) | 0.04 (−0.3; 0.4) | 0.4 (−0.1; 0.8) |
| baseline to 26 weeks, mean (95% CI) | 0.1 (−0.3; 0.5) | 0.3 (−0.2; 0.7) |
| Perceived Stress Scale, total score | ||
| baseline to 8 weeks, mean (95% CI) | 0.6 (−2.5; 3.6) | 0.2 (−3.5; 3.9) |
| baseline to 26 weeks, mean (95% CI) | −1.7 (−4.8; 1.3) | −1.8 (−5.6; 2.0) |
| Biomarkers | ||
| Interleukin-1ß, pg/mL | ||
| baseline to 8 weeks, mean (95% CI), | 0.3 (−0.1; 0.6) | −0.02 (−0.4; 0.4) |
| (N) | (18) | (14) |
| baseline to 26 weeks, mean (95% CI), | 0.2 (−0.2; 0.5) | 0.1 (−0.3; 0.5) |
| (N) | (15) | (13) |
| Interleukin-6, pg/mL | ||
| baseline to 8 weeks, mean (95% CI), | −0.8 (−1.8; 0.2) | 0.3 (−0.8; 1.5) |
| (N) | (18) | (14) |
| baseline to 26 weeks, mean (95% CI), | −0.3 (−1.4; 0.7) | −0.1 (−1.3; 1.1) |
| (N) | (15) | (13) |
| Interferon-γ, pg/mL | ||
| baseline to 8 weeks, mean (95% CI), | 1.3 (−2.3, 4.9) | 0.2 (−3.9; 4.3) |
| (N) | (18) | (14) |
| baseline to 26 weeks, mean (95% CI), | 1.6 (−2.4; 5.6) | −0.5 (−4.8; 3.7) |
| (N) | (15) | (13) |
| Tumor Necrosis Factor-α, pg/mL | ||
| baseline to 8 weeks, mean (95% CI), | 0.03 (−3.8; 3.8) | 2.6 (−1.8; 7.0) |
| (N) | (18) | (14) |
| baseline to 26 weeks, mean (95% CI). | 0.0005 (−3.8; 3.8) | 3.3 (−1.1; 7.8) |
| (N) | (15) | (13) |
| C−Reactive Protein, mg/dL | ||
| baseline to 8 weeks, mean (95% CI), | −0.9 (−1.7;−0.1) | 0.1 (−0.9; 1.0) |
| (N) | (18) | (14) |
| baseline to 26 weeks, mean (95% CI), | −0.7 (−1.6; 0.1) | 0.1 (−0.9; 1.0) |
| (N) | (15) | (13) |
Results are presented as mean difference score (95% confidence interval, CI).
Exploratory Analyses
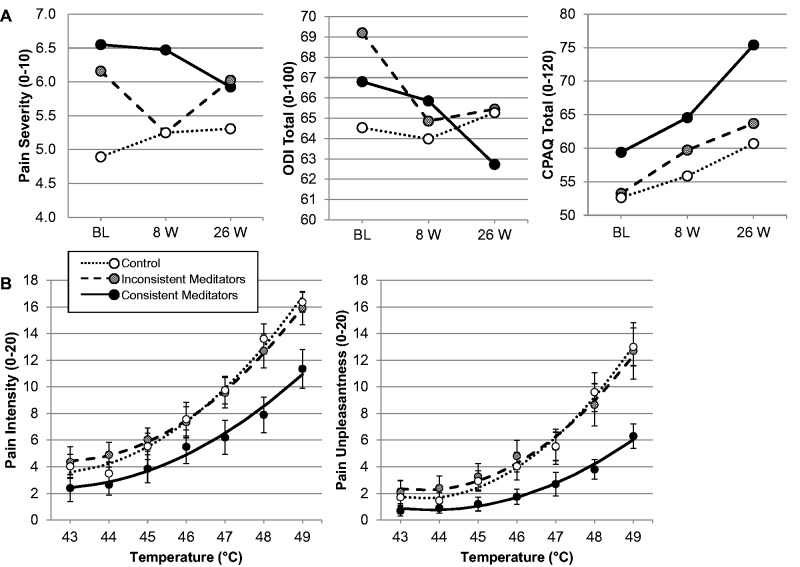
“Dose-response:” Nineteen out of 21 experimental participants attended at least one intervention session (mean 4.7 ± 2.8 among all experimental participants); all experimental participants provided data on home-based formal meditation practice during weeks 1–8, and 20 provided data on their practice during weeks 9–26. Experimental participants as a group engaged in 164.0 ± 122.1 minutes/week of practice on average during the study (weeks 1–26). However, when categorized by the practice amount/consistency, “consistent” meditators (N = 10) reported 256.2 ± 102.7 minutes/week, while “inconsistent” ones (N = 11) reported only 71.7 ± 44.8 minutes/week of practice; these two groups of did not differ though in their attendance in the intervention sessions (P ≥ 0.05).
To evaluate the possible influence of the extent and the consistency of formal meditation practice, change in outcome measures was compared between consistent and inconsistent meditators, and the controls (Figure 4). There were no statistically significant differences in the change in self-reported and biomarker measures between the consistent and inconsistent meditators at 8 and 26 weeks (Mann-Whitney U test). However, when compared with controls, the consistent meditators had a greater decrease in pain ratings (P = 0.026) at 26 weeks. The inconsistent meditators showed a transient improvement in pain severity ratings only at 8 weeks relative to controls (P = 0.038; Figure 4A). Despite the illustrated differences between consistent meditators and the other two groups on the physical function and pain acceptance scores (portrayed in Figure 4A), and on the sensitivity data (Figure 4B), the between-group comparisons of the scores and the slopes of the quadratic regressions between thermal stimulus intensity and both pain intensity and unpleasantness ratings, respectively, were not significantly different between groups (P ≥ 0.05).
Figure 4.
Comparison between consistent and inconsistent meditators, and control group participants. (A) Self-reported outcomes: change over time in pain severity, disability (ODI), and pain acceptance (CPAQ) ratings for 10 consistent and 11 inconsistent meditators, and 14 controls; outcomes collected at baseline (BL), 8 weeks (8 W), and 26 weeks (26 W). (B) Pain sensitivity measures: average ratings of pain intensity and unpleasantness to thermal stimuli at 26 weeks for 10 consistent and 10 inconsistent meditators, and 14 controls. Average estimate of quadratic function for the relationship between stimulus temperature and rating is included; error bars represent the standard error of the mean.
Spearman correlations: At 8 weeks, the reduction in disability correlated with a reduction in perceived stress (r = 0.76; P < 0.001) and increased mindfulness (r = -0.56; P = 0.010) in the meditation-CBT group. In the control group, only one correlation was of marginal significance at 8 weeks (between changes in disability and stress scores, r = 0.52; P = 0.057). At 26 weeks, no statistically significant correlations were found between main and explanatory outcome measures in either group.
Discussion
Our 26-week pilot RCT indicates efficacy of the meditation-CBT intervention, when delivered as an adjunct to usual care, for reducing pain severity ratings and sensitivity to experimental nociceptive stimuli. A potential dose-response relationship between amount and consistency of meditation practice and the intervention benefits was also observed.
The statistically significant reduction in the severity of pain symptoms is encouraging and suggests meditation-CBT may offer benefits extending beyond the effects of each modality alone. This finding concurs with a RCT of a similar intervention for 115 patients with opioid-treated chronic pain, Mindfulness-Oriented Recovery Enhancement (MORE) [14]. This RCT found that MORE decreased pain severity (P = 0.038) and interference (P = 0.003) at a 3-month follow-up as compared with an active control [14]. Interestingly, the average reduction in pain severity by 0.67 points in the MORE group was similar to that noted in our study. When assessed as separate modalities, a meta-analysis by Veehoff et al. found evidence for a small effect of acceptance-based interventions, e.g., Mindfulness-Based Stress Reduction, for reducing pain (standardized mean difference [SMD] = 0.37; 95% CI: 0.20, 0.53) [25]. Likewise, the Agency for Healthcare Research and Quality’s meta-analysis found moderate strength of evidence for small effect of mindfulness interventions for decreasing pain when compared with a nonspecific active control (SMD = 0.33; 95% CI: 0.03, 0.62) and low strength of evidence for “no effect” when compared with a specific active control [18]. Although CBT is considered a standard of care therapy in CLBP, it is supported by relatively limited empirical evidence [10]. A 2010 Cochrane Collaboration review [55] found moderate quality evidence that a “combined behavioral therapy,” such as CBT, when compared with usual care, was effective for pain relief in the short-term (SMD = -0.60; 95% CI: -0.97, -0.22), but not in the long-term or for improving functional status in CLBP, conclusions consistent with those of a recent systematic review [56]. Evidence on positive effects of CBT for opioid-treated populations is even more limited but promising [10,14,55–57]. When combined, meditation and CBT could capitalize on gains attributable to each modality and safely achieve additive effects [25], which may persist long-term with continued meditation practice [27].
There is very limited research on the long-term effects of opioids in chronic non-cancer pain [8,58–60]. However, some studies suggest long-term opioid therapy may worsen pain [61] and disability [62]. Our study participants were, on average, treated with high-dose opioids at baseline; yet, they reported substantial daily pain and severe physical disability, which may indicate a lack of efficacy of opioids as well as hyperalgesia. Therefore, opioid dose reduction could potentially improve outcomes, especially if opioid-induced hyperalgesia played a role. Although we did not find a statistically significant decrease in the use of opioid medications during this study, it is plausible that a significant opioid dose reduction could be found with a longer follow-up period or larger sample size. Reduced desire for opioids, noted by Garland et al. in an RCT of the MORE intervention for opioid-treated chronic pain [14], and discontinuation of opioid therapy by four participants with opioid-treated chronic pain after the CBP intervention in a small pre-post clinical trial (N = 22) [57], lend support to such hypothesis. Decreased reliance on and use of opioids by chronic pain patients could reduce the dose-dependent risk of opioid therapy and lessen a societal problem of prescription opioid abuse [59,61]. Development and testing of new, non-opioid therapies, such as meditation-CBT intervention, is critical to safely improve outcomes in this population.
Psychophysical measures of pain sensitivity take a step beyond self-report to begin addressing potential mechanisms underlying efficacy of meditation-CBT in this population. Current perspectives on the mechanisms of chronic pain, particularly in conditions without clear peripheral pathology, suggest that chronic pain symptoms can be maintained by a combination of augmented processing and reduced descending regulation of sensory information [63]. However, it is currently unknown whether reductions in neural sensitivity translate into improved clinical outcomes. Our findings of decreased pain sensitivity to noxious thermal stimuli, observed at 8 and maintained at 26 weeks, suggest the meditation-CBT intervention reduced CNS sensitivity and hyperalgesia, concomitant with improved clinical outcomes among opioid-treated CLBP patients. These findings are consistent with previous research demonstrating improved pain sensitivity and regulation with meditation [23,64–66], and extend them to opioid-treated chronic pain patients. Future studies, incorporating more direct measures of central sensitivity and/or pain modulation as well as clinical measures are needed to better evaluate the effects of this intervention.
Although the improvements in physical function, pain acceptance, and the inflammatory biomarker profile (including CRP) did not reach a statistical significance, they tended to favor the meditation-CBT group (small-to-moderate Cohen’s d effect sizes). Our findings suggested the improvements in pain acceptance (as measured by the CPAQ) rather than changes in the mindfulness scores (as assessed by the MAAS) contributed to treatment efficacy. This is consistent with the goals of meditation-based interventions, which target adaptive pain coping [67]. Though these results provide promise, they should be considered tentative, requiring further testing in future, larger studies.
Limitations, Generalizability
Lack of blinding of participants and the study personnel, and self-selection of participants to the study of meditation-based intervention may have introduced bias. A “placebo effect” could favor positive outcomes in the meditation-CBT group, and the experimental design would have benefited from an active comparison group. The design did not permit untangling of the specific (i.e., meditation-CBT components) versus non-specific (e.g., placebo, therapist contact, peer-group support) effects of the intervention. However, the change in multiple domains of outcomes was well aligned with the hypothesized effects of the meditation-CBT intervention. Moreover, the magnitude of change was related to the “dose” of at-home meditation practice, suggesting that the intervention enactment influenced outcomes. This hypothesis is supported by qualitative comments from participants (authors’ unpublished data), and—indirectly—by the unfavorable natural history and poor treatment effects of “usual care” in chronic back pain [68,69]. Small sample size, combined with the above limitations, preclude drawing final conclusions about the full scope of intervention’s effects on outcomes in opioid-treated CLBP.
Future Directions
Development of new effective therapies is critically needed for patients with opioid-treated CLBP, which is often refractory to existing treatments and considered one of the most challenging conditions in clinical practice [68,70]. Findings of this pilot RCT, favoring the meditation-CBT over control group, call for further evaluation of the meditation-CBT intervention. Future studies are needed to better understand effects and mechanisms of action of meditation and/or CBT as therapies for opioid-treated CLBP, and to evaluate new modes of intervention delivery beyond a traditional in-person approach that can limit treatment access/engagement among patients affected by physical disability. These pilot-level data offer promise that the positive effects of meditation-CBT on clinical outcomes may translate into a reduced need for and use of opioid analgesics, a hypothesis that should be tested by future long-term trials.
Conclusions
Mindfulness meditation and CBT-based interventions have the potential to safely reduce pain severity and sensitivity in patients with opioid-treated CLBP. With substantial and growing interest of chronic pain patients in meditation and other integrative and complementary health modalities, more research is needed so that these interventions, if proven effective, can gain coverage by health care plans and be more available to patients.
Funding sources: Dr. Zgierska’s work was supported by the K23AA017508 from the National Institutes of Health (NIH) National Institute on Alcohol Abuse and Alcoholism (NIAAA), and funds from the University of Wisconsin-Madison. The project was also supported by the Clinical and Translational Science Award (CTSA) program through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427.
Disclosure and conflicts of interest: The authors have no conflicts of interest to disclose. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- 1.Martin BI, Turner JA, Mirza SK, et al. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997-2006. Spine 2009;34(19):2077–84. [DOI] [PubMed] [Google Scholar]
- 2.Gore M, Sadosky A, Stacey BR, Tai KS, Leslie D. The burden of chronic low back pain: Clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine 2012;37(11):E668–77. [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services. Healthy People 2020, 2020 Topics and objectives: Arthritis, osteoporosis, and chronic back conditions. Updated 2015. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=3 (accessed November 2015).
- 4.Dillie KS, Fleming MF, Mundt MP, French MT. Quality of life associated with daily opioid therapy in a primary care chronic pain sample. J Am Board Fam Med 2008;21(2):108–17. [DOI] [PubMed] [Google Scholar]
- 5.Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med 2011;171(7):686–91. [DOI] [PubMed] [Google Scholar]
- 6.Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: A cohort study. Ann Intern Med 2010;152(2):85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chou R, Ballantyne JC, Fanciullo GJ, Fine PG, Miaskowski C. Research gaps on use of opioids for chronic noncancer pain: Findings from a review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guideline. J Pain 2009;10(2):147–59. [DOI] [PubMed] [Google Scholar]
- 8.Manchikanti L, Abdi S, Atluri S, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part I—evidence assessment. Pain Physician 2012;15(3 suppl):S1–65. [PubMed] [Google Scholar]
- 9.National Center for Complementary and Alternative Medicine. Third Strategic Plan 2011-2015: Exploring the science of complementary and alternative medicine. 2011. Available at: http://nccam.nih.gov/sites/nccam.nih.gov/files/NCCAM_SP_508.pdf (accessed November 2015).
- 10.Reese C, Mittag O. Psychological interventions in the rehabilitation of patients with chronic low back pain: Evidence and recommendations from systematic reviews and guidelines. Int J Rehabil Res 2013;36(1):6–12. [DOI] [PubMed] [Google Scholar]
- 11.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen Hosp Psychiatry 1982;4(1):33–47. [DOI] [PubMed] [Google Scholar]
- 12.Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin Psychol Sci Prac 2003;10:125–43. [Google Scholar]
- 13.Fjorback LO, Arendt M, Ornbol E, Fink P, Walach H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy: A systematic review of randomized controlled trials. Acta Psychiatr Scand 2011;124(2):102–19. [DOI] [PubMed] [Google Scholar]
- 14.Garland EL, Manusov EG, Froeliger B, et al. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: Results from an early-stage randomized controlled trial. J Consult Clin Psychol 2014;82(3):448–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Segal ZV, Williams JM, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York: Guilford Publications; 2002. [Google Scholar]
- 16.Zgierska A, Rabago D, Zuelsdorff M, et al. Mindfulness meditation for alcohol relapse prevention: A feasibility pilot study. J Addict Med 2008;2(3):165–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bowen S, Chawla N, Marlatt A. Mindfulness-Based Relapse Prevention for Addictive Behaviors: A Clinician's Guide. New York: Guilford Press; 2010. [Google Scholar]
- 18.Goyal M, Singh S, Sibinga EMS, et al. Meditation Programs for Psychological Stress and Well-Being. Comparative Effectiveness Review No. 124. (Prepared by Johns Hopkins University Evidence-based Practice Center under Contract No. 290-2007-10061–I.) AHRQ Publication No. 13(14)-EHC116-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2014. Available at: http://www.effectivehealthcare.ahrq.gov/ehc/products/375/1830/Meditation-report-140110.pdf (accessed November 2015). [Google Scholar]
- 19.Kobus AM, Smith DH, Morasco BJ, et al. Correlates of higher-dose opioid medication use for low back pain in primary care. J Pain 2012;13(11):1131–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chiesa A, Serretti A. Mindfulness-based interventions for chronic pain: A systematic review of the evidence. J Altern Complement Med 2011;17(1):83–93. [DOI] [PubMed] [Google Scholar]
- 21.Winbush NY, Gross CR, Kreitzer MJ. The effects of mindfulness-based stress reduction on sleep disturbance: A systematic review. Explore 2007;3(6):585–91. [DOI] [PubMed] [Google Scholar]
- 22.Davidson RJ, Kabat-Zinn J, Schumacher J, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med 2003;65(4):564–70. [DOI] [PubMed] [Google Scholar]
- 23.Zeidan F, Martucci KT, Kraft RA, et al. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci 2011;31(14):5540–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turk DC, Wilson HD. Fear of pain as a prognostic factor in chronic pain: Conceptual models, assessment, and treatment implications. Curr Pain Headache Rep 2010;14(2):88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Veehof MM, Oskam MJ, Schreurs KM, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. Pain 2011;152(3):533–42. [DOI] [PubMed] [Google Scholar]
- 26.Brown CA, Jones AK. Psychobiological correlates of improved mental health in patients with musculoskeletal pain after a mindfulness-based pain management program. Clin J Pain 2013;29(3):233–44. [DOI] [PubMed] [Google Scholar]
- 27.Grossman P, Tiefenthaler-Gilmer U, Raysz A, Kesper U. Mindfulness training as an intervention for fibromyalgia: Evidence of postintervention and 3-year follow-up benefits in well-being. Psychother Psychosom 2007;76(4):226–33. [DOI] [PubMed] [Google Scholar]
- 28.Patil SG. Effectiveness of mindfulness meditation (Vipassana) in the management of chronic low back pain. Indian J Anaesth 2009;53(2):158–63. [PMC free article] [PubMed] [Google Scholar]
- 29.Cramer H, Haller H, Lauche R, Dobos G. Mindfulness-based stress reduction for low back pain. A systematic review. BMC Complement Altern Med 2012;12:162. doi: 10.1186/1472-6882-12-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schutze R, Slater H, O'Sullivan P, et al. Mindfulness-based functional therapy: A preliminary open trial of an integrated model of care for people with persistent low back pain. Front Psychol 2014;5:839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zgierska A, Wallace ML, Burzinski CA, Cox J, Backonja M. Pharmacological and toxicological profile of opioid-treated, chronic low back pain patients entering a mindfulness intervention randomized controlled trial. J Opioid Manag 2014;10(5):323–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005;113(1–2):9–19. [DOI] [PubMed] [Google Scholar]
- 33.Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 2008;9(2):105–21. [DOI] [PubMed] [Google Scholar]
- 34.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: Towards international consensus regarding minimal important change. Spine 2008;33(1):90–4. [DOI] [PubMed] [Google Scholar]
- 35.Chapman JR, Norvell DC, Hermsmeyer JT, et al. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine 2011;36(21 suppl):S54–68. [DOI] [PubMed] [Google Scholar]
- 36.Von Korff M, Jensen MP, Karoly P. Assessing global pain severity by self-report in clinical and health services research. Spine 2000;25(24):3140–51. [DOI] [PubMed] [Google Scholar]
- 37.Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain 2004;5(2):133–7. [DOI] [PubMed] [Google Scholar]
- 38.Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain 1999;83(2):157–62. [DOI] [PubMed] [Google Scholar]
- 39.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine 2000;25(22):2940–53. [DOI] [PubMed] [Google Scholar]
- 40.Savre I, Fairbank J. ODI Oswestry Disability Index Information Booklet. 1st edition. France: Mapi Research Trust; 2011. [Google Scholar]
- 41.Fals-Stewart W, O'Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. J Consult Clin Psychol 2000;68(1):134–44. [DOI] [PubMed] [Google Scholar]
- 42.Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption In: RZ Litten, J Allen, eds. Measuring Alcohol Consumption: Psychosocial and Biological Methods. New Jersey: Humana Press; 1992:41–72. [Google Scholar]
- 43.McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: Component analysis and a revised assessment method. Pain 2004;107(1–2):159–66. [DOI] [PubMed] [Google Scholar]
- 44.Reneman MF, Dijkstra A, Geertzen JH, Dijkstra PU. Psychometric properties of Chronic Pain Acceptance Questionnaires: A systematic review. Eur J Pain 2010;14(5):457–65. [DOI] [PubMed] [Google Scholar]
- 45.Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol 2003;84(4):822–48. [DOI] [PubMed] [Google Scholar]
- 46.McCracken L, Thompson M. Components of mindfulness in patients with chronic pain. J Psychopathol Behav Assess 2009;31(2):75–82. [Google Scholar]
- 47.Cohen S, Williamson G. Perceived stress in a probability sample of the United States In: S Spacapan, S Oskamp, eds. The Social Psychology of Health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage;1988:31–67. [Google Scholar]
- 48.Roberti J, Harrington LN, Storch EA. Further psychometric support for the 10-item version of the perceived stress scale. Journal of College Couns 2006;9:135–47. [Google Scholar]
- 49.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24(4):385–96. [PubMed] [Google Scholar]
- 50.Gracely RH, Kwilosz DM. The descriptor differential scale: Applying psychophysical principles to clinical pain assessment. Pain 1988;35(3):279–88. [DOI] [PubMed] [Google Scholar]
- 51.Cook DB, Stegner AJ, Ellingson LD. Exercise alters pain sensitivity in Gulf War veterans with chronic musculoskeletal pain. J Pain 2010;11(8):764–72. [DOI] [PubMed] [Google Scholar]
- 52.Gracely RH, McGrath F, Dubner R. Ratio scales of sensory and affective verbal pain descriptors. Pain 1978;5(1):5–18. [DOI] [PubMed] [Google Scholar]
- 53.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria; 2015. Available at: https://www.R-project.org (accessed November 2015).
- 54.Bates D, Maechler M, Bolker BM, Walker S. Fitting linear mixed-effects models using lme4. Journal of Statistical Software 2015;67(1):1–48. [Google Scholar]
- 55.Henschke N, Ostelo RWJG, van Tulder MW, Vlaeyen JWS, Morley S, Assendelft WJJ, Main CJ. Behavioural treatment for chronic low-back pain. Cochrane Database of Systematic Reviews 2010, Issue 7. Art. No.: CD002014. DOI: 10.1002/ 14651858.CD002014.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van Middelkoop M, Rubinstein SM, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J Jan 2011;20(1):19–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Whitten SK, Stanik-Hutt J. Group cognitive behavioral therapy to improve the quality of care to opioid-treated patients with chronic noncancer pain: A practice improvement project. J Am Assoc Nurse Pract 2013;25(7):368–76. [DOI] [PubMed] [Google Scholar]
- 58.Manchikanti L, Abdi S, Atluri S, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2–guidance. Pain Physician 2012;15(3 suppl):S67–116. [PubMed] [Google Scholar]
- 59.Chou R, Deyo R, Devine B, et al. The Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain. Evidence Report/Technology Assessment No. 218. (Prepared by the Pacific Northwest Evidence-Based Practice Center Under Contract No. 290-2012-00014-I.) AHRQ Publication No. 14-E005-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2014. Available at: http://www.effectivehealthcare.ahrq.gov/ehc/products/557/1971/chronic-pain-opioid-treatment-report-141205.pdf (accessed April 2015). [Google Scholar]
- 60.Reuben DB, Alvanzo AA, Ashikaga T, et al. National Institutes of Health Pathways to prevention workshop: The role of opioids in the treatment of chronic pain. Ann Intern Med 2015;162(4):295–300. [DOI] [PubMed] [Google Scholar]
- 61.Manchikanti L, Helm S, Fellows B, 2nd, et al. Opioid epidemic in the United States. Pain Physician 2012;15(3 suppl):ES9–38. [PubMed] [Google Scholar]
- 62.Sjogren P, Gronbaek M, Peuckmann V, Ekholm O. A population-based cohort study on chronic pain: The role of opioids. Clin J Pain 2010;26(9):763–9. [DOI] [PubMed] [Google Scholar]
- 63.Phillips K, Clauw DJ. Central pain mechanisms in chronic pain states–Maybe it is all in their head. Best Pract Res Clin Rheumatol 2011;25(2):141–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Grant JA. Meditative analgesia: The current state of the field. Ann N Y Acad Sci 2014;1307:55–63. [DOI] [PubMed] [Google Scholar]
- 65.Perlman DM, Salomons TV, Davidson RJ, Lutz A. Differential effects on pain intensity and unpleasantness of two meditation practices. Emotion 2010;10(1):65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zeidan F, Gordon NS, Merchant J, Goolkasian P. The effects of brief mindfulness meditation training on experimentally induced pain. J Pain 2010;11(3):199–209. [DOI] [PubMed] [Google Scholar]
- 67.Vowles KE, McCracken LM, Eccleston C. Processes of change in treatment for chronic pain: The contributions of pain, acceptance, and catastrophizing. Eur J Pain 2007;11(7):779–87. [DOI] [PubMed] [Google Scholar]
- 68.Itz CJ, Geurts JW, van Kleef M, Nelemans P. Clinical course of non-specific low back pain: A systematic review of prospective cohort studies set in primary care. Eur J Pain 2013;17(1):5–15. [DOI] [PubMed] [Google Scholar]
- 69.Somerville S, Hay E, Lewis M, et al. Content and outcome of usual primary care for back pain: A systematic review. Br J Gen Pract 2008;58(556):790–7, i-vi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.National Center on Addiction and Substance Abuse at Columbia University (CASA). Missed opportunity: National survey of primary care physicians and patients on substance abuse. New York: CASA; 2000. Available at: http://www.casacolumbia.org/addiction-research/reports/national-survey-primary-care-physicians-patients-substance-abuse (accessed November 2015).