Abstract
A secondary analysis of data from adult female prison inmates in the mid-Atlantic United States defined relationships between having incarcerated adult family members during childhood and neurological outcomes. Of 135 inmates, 99(73%) had one or more incarcerated adult family members during childhood. Regression analyses revealed that having incarcerated adult family members was related to greater frequency and severity of childhood abuse and higher incidence of neurological deficits in adulthood, especially related to traumatic brain injuries, compared to those without incarcerated adult family members. Along with being role models, adult family members impact the neurological health of children throughout their lifespan.
With the projected increase in prevalence of neurological conditions in the growing aging population in both developed and developing countries (WHO, 2015), it is critical to define risk factors in order to target prevention strategies. With the growing rate of incarcerations, it is critical to understand the impact this has on children in the families of incarcerated adults. Most studies of children with incarcerated adult family members describe psycho-social outcomes, yet little is understood about the long-term neurological health implications of having an adult family member incarcerated during childhood. The aim of the researchers was to elucidate the impact of having incarcerated adult family members during childhood on females and to define associated neurological health throughout their lifespan. The purpose of this study was to test our hypotheses that having incarcerated adult family members during childhood places one at greater risk of becoming a victim of abuse and increases risk for neurological impairment that results in ongoing high risk behaviors leading to subsequent incarceration and neurological decline throughout the life-span of females.
Background
It is critical to consider the fact that most prison inmates are parents. The mass incarceration of parents in the United States is a rapidly growing problem with issues of race and ethnic disparities and poor outcomes for children of incarcerated parents (Foster & Hagan, 2009; Huq, 2015; Wildeman, 2012, 2014). Mass incarceration impacts child mortality (Wildeman, Andersen, Lee, & Karlson, 2014) and population health (Dumont, Brockmann, Dickman, Alexander, & Rich, 2012; Wildeman, 2012). Women with family members who were currently incarcerated had increased odds of being obese, having had a heart attack or stroke, and being in fair or poor health (H. Lee, Wildeman, Wang, Matusko, & Jackson, 2014). Incarceration of a woman or her partner in the year before birth was shown to be associated with higher odds of maternal hardship and poorer perinatal health behaviors (Dumont et al., 2014). Many female prison inmates have had incarcerated adult family members during childhood as well as high rates of neurological impairment in adulthood (Brewer-Smyth, Burgess, & Shults, 2004).
Hundreds of millions of people worldwide are affected by neurological disorders, and the extension of life expectancy with ageing populations in both developed and developing countries are likely to increase the prevalence (WHO, 2015). The World Health Organization has determined that dementia is a public health priority. Dementia is a syndrome that affects memory, thinking, and behavior. The number of people living with dementia worldwide is currently estimated at 35.6 million and is projected to double by 2030 and more than triple by 2050 (WHO, 2012). Increased susceptibility for dementia and cognitive decline that is reported later in life after traumatic brain injury (TBI) may result from brain tissue loss that increases throughout the chronic post-injury phase, suggesting that TBI accelerates the rate of brain aging and atrophy (Cole, Leech, Sharp, & Alzheimer’s Disease Neuroimaging, 2015). TBI, most often resulting from accidents, violence, and falls, is the leading cause of death and disability in children and young adults world-wide resulting in loss of many years of productive life, disability, and neurobehavioral problems (WHO, 2006). Health promotion is particularly important for neurological disorders by identifying those at risk and providing resources for rehabilitation and prevention of the projected escalation.
In order to break intergenerational cycles of physical and emotional trauma and criminal behavior (De Bellis, 2012; Forsman & Långström, 2012; Widom, 2000), it is imperative to continue to better understand factors contributing to it. Protective factors against violence perpetration such as measures related to parental expectations and connectedness with parents and other adults (Resnick, Ireland, & Borowsky, 2004) are difficult to achieve when adult family members are incarcerated. Family disorganization, dissolution and violence, which are often the case when an adult family member is incarcerated, can be risk factors for childhood abuse. There are numerous effects of adverse childhood experiences on physical health including neurobiological findings such as memory impairment (Anda et al., 2006) and long term health risks (Slopen, Koenen, & Kubzansky, 2014). Adverse childhood experiences significantly increased risk of many health-harming behaviors for physical inactivity, obesity, attempted suicide, and neurological decline (Bellis et al., 2014; Brewer-Smyth, 2014; Brewer-Smyth et al., 2007). Having an incarcerated parent during childhood has been shown to be associated with numerous poor health outcomes in young adulthood including depression, posttraumatic stress disorder, anxiety, cholesterol, asthma, migraines, HIV/AIDS, and fair/poor health (R. D. Lee, Fang, & Luo, 2013). Because little is understood about long-term neurobehavioral outcomes of children with incarcerated adult family members, the aim of the researchers was to elucidate the impact of having incarcerated adult family members during childhood on neuro-behavioral health throughout the lifespan of females.
Methods
Design and Sample
Because of the high rate of incarcerated adult family members in the lives of female prison inmates, and high rates of neurological impairment in this population, a secondary analysis was conducted of data from private interviews and examinations to understand how having incarcerated adult family members during childhood could influence neurological health throughout the lifespan. A modified case-control design was used to compare female prison inmates who had incarcerated adult family members during childhood to female prison inmates who did not have incarcerated adult family members during childhood. Adult female prison inmates were randomly recruited from both minimum and maximum security sections of a prison in a Mid-Atlantic state in the United States. All data were collected during private interviews and examinations conducted by the first author.
Detailed methods have been reported (Brewer-Smyth et al., 2004; Brewer-Smyth et al., 2007). The sample size determined based on the parent studies was adequate to provide power (.8) to find a moderate effect with N=135 female prisoners and alpha =.05. Eighty-one percent of eligible inmates volunteered to be in this study.
The study was approved by the institutional review boards of the principal investigator’s institutions and all participants signed written informed consents. Procedures were conducted in accordance with federal regulations for the conduct of research with prisoners (Brewer-Smyth, 2008).
Measures
Incarcerated adult family members during childhood were self-reported. Muenzenmaier’s scale (Meyer, Muenzenmaier, Cancienne, & Struening, 1996; Muenzenmaier, Meyer, Struening, & Ferber, 1993) was slightly revised to assess frequency and severity of sexual and physical abuse before age 18. It has reported validity and reliability in tests of women of similar age, ethnic background, and education including mentally ill women (Meyer et al., 1996; Muenzenmaier et al., 1993). Higher scores indicate greater frequency and severity of abuse. Other data collection included abuse that resulted in health care treatment. They were also asked if any items on the abuse scale occurred since age 18 and when it occurred last. Self-reports were verified by evidence of physical injury and records when available.
General health and specifically neurological histories and physical examinations were evaluated by a certified neuro-rehabilitation clinical nurse specialist in accordance with standards that were validated by two neurologists and a neuropsychologist. Documentation and other examination evidence to support histories provided by each inmate was investigated, such as neurological deficits and cranial-facial scars or palpable areas of skull damage consistent with self-reports of traumatic injuries and other neurological histories.
Analysis
Statistical methods included frequencies, t-tests and graphical checks. Childhood abuse scores and number of neurological histories and neurological examination abnormalities were dichotomized by the mean to indicate high scores compared to low scores. Logistic regression statistical analyses were then used to compare adult female prison inmates who had incarcerated adult family members during childhood to those who did not for each of the main variables.
Results
Of 135 adult female prison inmates, 99 (73%) had at least one adult member of their extended family incarcerated when they were a child. Hispanic and African American inmates had disproportionately high rates of incarcerated adult family members during childhood (Table 1). There were no significant differences in age, years of education, or violent crimes committed by participants who had incarcerated adult family members during childhood and those who did not.
Table 1.
Demographics by Adult Family Member Incarcerated During Childhood*
| Family Member Incarcerated During Childhood |
|||||
|---|---|---|---|---|---|
| No (n =36) | Yes (n =99) | ||||
|
| |||||
| Frequency | Percent | Frequency | Percent | p value | |
| Current Conviction | .962 | ||||
| Not Violent | 22 | (29%) | 55 | (71%) | |
| Violent | 9 | (28%) | 23 | (72%) | |
| Race | .026 | ||||
| Caucasian | 20 | (37%) | 34 | (63%) | |
| Black, Hispanic and other | 16 | (20%) | 65 | (80%) | |
| Neurological Histories | .026 | ||||
| Less than 3.5 Neurological Histories per Person | 28 | (34%) | 55 | (66%) | |
| More than 3.5 per Person | 8 | (16%) | 42 | (84%) | |
|
| |||||
| Mean | SD | Mean | SD | p value | |
|
| |||||
| Age | 36.61 | 8.88 | 33.53 | 8.17 | .060 |
| Years of Education | 11.40 | 2.74 | 10.95 | 2.17 | .320 |
| Physical Abuse before 18 | 3.92 | 4.12 | 6.03 | 5.17 | .029 |
| Sexual Abuse before 18 | 1.14 | 1.85 | 3.31 | 4.11 | .003 |
| Total Childhood Physical &Sexual Abuse before age 18 | 4.58 | 5.28 | 8.94 | 7.91 | .003 |
| Number of NeurologicalExamination Abnormalities | 1.54 | 1.52 | 2.34 | 1.62 | .012 |
| Number of Neurological History Reports Prior to Current Crime | 2.56 | 3.38 | 3.89 | 6.13 | .219 |
| Suicide History Number of Attempts | 0.72 | 1.14 | 1.70 | 5.53 | .297 |
| Age of first Criminal conviction | 26.41 | 11.85 | 21.27 | 7.49 | .007 |
| Number of Violent CrimesCommitted in past 5 years | 0.94 | 2.22 | 0.83 | 1.26 | .734 |
| Number of Violent Convictions | 1.71 | 3.36 | 1.41 | 2.06 | .580 |
Descriptive statistics are reported as Mean ± SD for continuous data and frequency and percentage for categorical data. Bold indicates significance p value <.05
Bivariate logistic regression revealed that having at least one incarcerated adult family member during childhood was related to having been a victim of childhood sexual abuse (OR = 2.200; 95% CI = 1.005–4.815), greater total childhood physical and sexual abuse scores (OR = 3.222; 95% CI = 1.286–8.074), greater number of neurological history reports per person prior to the current crime (OR = 2.673; 95% CI = 1.106–6.459) such as traumatic brain injuries (TBI), and greater number of neurological examination abnormalities per person in adulthood (OR = 2.625; 95% CI = 1.082–6.367), compared to those without incarcerated adult family members (Figures 1, 2, and 3).
Figure 1.
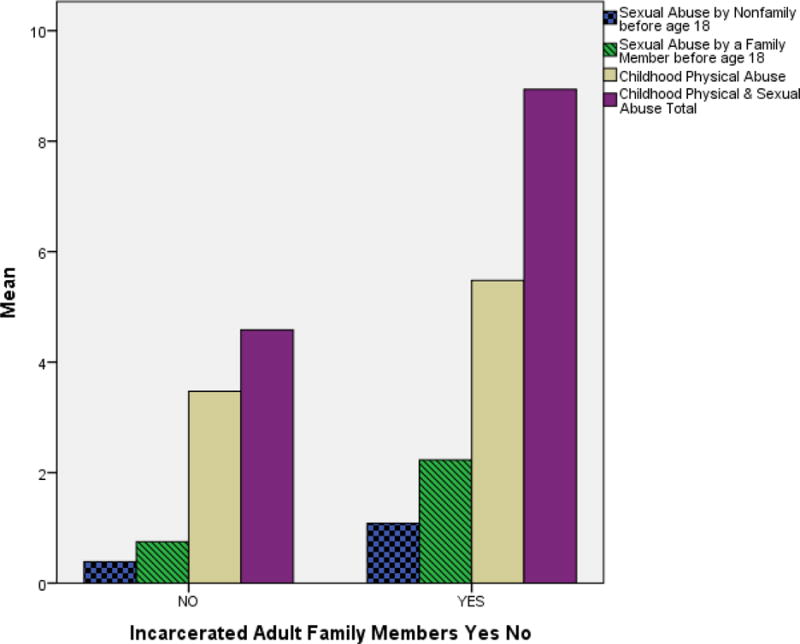
Those with incarcerated adult family members during childhood experienced greater frequency and severity of childhood abuse than those without incarcerated family members.
Figure 2.
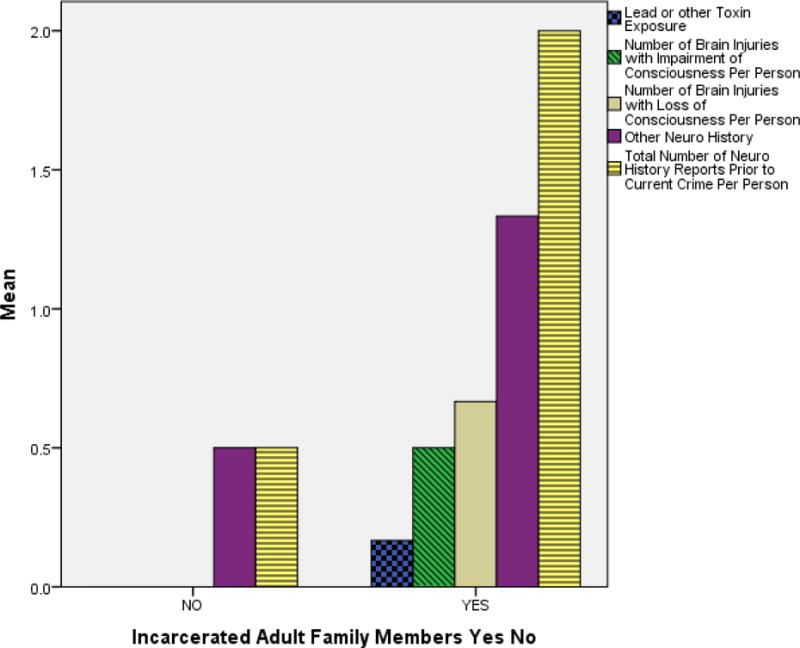
Those with incarcerated adult family members during childhood had a greater number of neurological history reports (mean of 2 per person) than those without incarcerated adult family members. Other Neuro History includes Stroke, Seizures, CNS Infection, CNS tumor, Product of a Complicated Pregnancy/Labor/Delivery, Migraine, CPR Resuscitation Survivor, Struck by Lightning, Neurosurgical Procedure, Other Loss of Consciousness such as after Choking, and Myasthenia Gravis.
Figure 3.
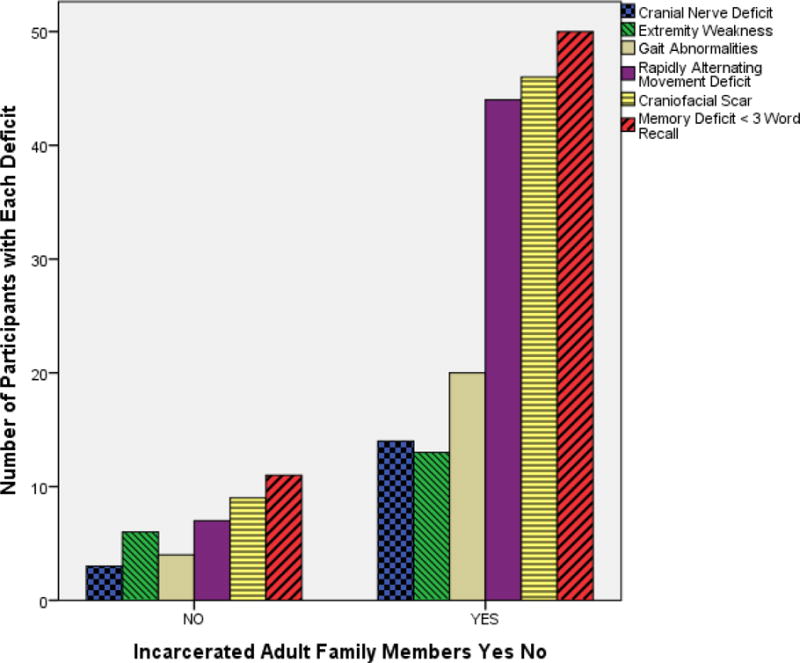
Those with incarcerated adult family members during childhood had greater neurological deficits on physical examination than those without incarcerated adult family members.
Neurological histories and/or neurological examination abnormalities were evident in 95% of this random sample of female inmates. Other than traumatic brain injuries, neurological histories included exposure to lead and/or other toxin, stroke, seizures, central nervous system (CNS) infection, CNS tumor, having been the product of a complicated pregnancy and delivery, migraine, survived cardio-pulmonary resuscitation (CPR), was struck by lightning, other loss of consciousness such as due to choking, myasthenia gravis, and/or had undergone a neurosurgical procedure. Each neurological history report was added for a total number of neurological history reports per person. For example, someone with 3 TBIs was coded as 3. Recurrent TBI was particularly prevalent with most occurring during high risk behaviors such as while they were under the influence of alcohol or other substances. Neurological examinations corroborated with neurological histories with the most frequently occurring deficits including cranial nerve deficits, extremity weakness, gait abnormalities, rapidly alternating movement deficits, less than 3 word recall memory deficits, cranial facial scars, and palpable evidence of skull injury.
Females with incarcerated adult family members had a significantly earlier age of their first criminal conviction. Though there were a greater number of suicide attempts per person in the group with incarcerated adult family members, the difference was not statistically significant. Obesity was not significantly higher for those with incarcerated adult family members during childhood.
Inmates described a series of events, often childhood abuse, contributing to their lack of regard for themselves and others often resulting in substance abuse and high risk behaviors for accidents, altercations, infectious disease transmission, and ongoing neurological decline. History of having been a victim of greater frequency and severity of childhood abuse placed one at greater risk of abuse in adulthood (OR = 2.614; 95% CI = 1.196–5.711). Abuse in adulthood was significantly related to a greater number of neurological histories (OR = 1.313; 95% CI = 1.075–1.604) and neurological examination abnormalities (OR = 1.439; 95% CI = 1.118–1.853). Abuse in adulthood was related to greater risk of suicide attempts (OR = 3.171; 95% CI = 1.289–7.801).
Discussion
More than half of adult female prison inmates had at least one adult member of their extended family incarcerated when they were a child. Adult female prison inmates with at least one incarcerated adult family member during childhood were 2 times more likely to have been a victim of childhood sexual abuse, 3.2 times more likely to have higher total childhood physical and sexual abuse scores, 2.7 times more likely to have more neurological history reports prior to the current crime such as traumatic brain injuries, and 2.6 times more likely to have more neurological examination abnormalities in adulthood compared to those without incarcerated adult family members.
Having been a victim of greater frequency and severity of childhood abuse placed female prison inmates at 2.6 times greater risk of being abused in adulthood. Females abused in adulthood were 1.3 times more likely to have neurological histories and almost 1.5 times more likely to have neurological examination abnormalities. Neurological impairment is related to self-destructive high risk behaviors for further neurological decline such as for HIV transmission and altercations that can result in further neurological decline in this population of female prison inmates (Brewer-Smyth et al., 2007). Abuse in adulthood results in 3 times greater risk of suicide attempts. History of childhood sexual abuse and suicide attempts places adult female inmates at greater risk for obesity (Brewer-Smyth, 2014). Furthermore, recent abuse in adulthood and TBIs are related to violent criminal behavior in female prison inmates (Brewer-Smyth et al., 2004). In addition to the obvious neurological impairment associated with TBI, there are multiple mechanisms through which childhood sexual abuse can contribute to adverse brain development and behavioral dysfunction (De Bellis, 2012; De Bellis, Spratt, & Hooper, 2011).
Strengths and Limitations
Because this was a secondary analysis and not the original research question, researcher bias was not a risk. Cause and effect cannot be determined by this design because it was a cross sectional study. We cannot determine in all cases if neurological impairment occurred before or after childhood abuse because children at particular risk are those with special needs that may increase caregiver burden. However the correct temporal sequence occurred with adult family members incarcerated during childhood and childhood abuse occurring prior to the current incarceration and neurological examinations. Most neurological histories also occurred later in life and continued to result in a spiral downward to greater neurological decline related to increased high risk behaviors, such as those leading to accidents or altercations resulting in recurrent TBIs. Furthermore, the number of neurological history reports describes mainly the frequency of recurrent TBIs per person, but not the severity or anatomical location of the injuries.
Direction for Future Intervention and Research
Sadly, in the decades since the closure of long-term mental health facilities throughout the United States and decrease in long-term inpatient neuro-rehabilitation, incarceration rates escalated with the vast majority of prisoners suffering from mental health problems (Dumont et al., 2012) that include both psychiatric as well as neurological conditions. Mental health facilities had previously provided for critical long-term needs of not only those with psychiatric conditions, but those with neurological conditions as well. Prison health systems must accommodate for the high prevalence of neurological impairment of female prison inmates who have often also been victims of childhood abuse. It is critical to break the cycle of events in the ongoing downward spiral related to the lack of regard for self and others, which leads to high risk behaviors for recurrent TBI and contributes to life-long neurological decline. Because female prison inmates in this population often receive short sentences and are frequently incarcerated and released, (Brewer-Smyth et al., 2004) prison health systems could play an important role in helping to break the cycle contributing to ongoing neurological decline. Screening for neurological impairment and attempts to separate patients with some neurological disorders from other prisoners may help the vulnerable population of female prison inmates from being exposed to criminal role models, further injury, and/or violence contributing to exacerbations of their condition. Prisons provide public health opportunities to reach medically underserved communities in the United States (Dumont et al., 2012). Yet health care systems alone cannot resolve this multifactorial problem.
Wildeman and Western (2010) argue that criminal justice reform alone will not solve the issues related to school failure, joblessness, untreated addiction, and mental illness that lead to increased incarceration; and that criminal justice reforms alone would repeat the mistakes made in the United States during the prison boom by addressing serious social problems with criminal justice policies. These problems require greater commitments to education, public health, and employment opportunities of low-skilled men and women (Wildeman & Western, 2010). Mental health is a critical area that requires serious attention in order to address incarceration rates and their long-term consequences for fragile families that contributes to ongoing neurological decline.
Nurse mentoring can play a role in this vulnerable population of children with incarcerated parents with public health initiatives to address high-risk behaviors in this often forgotten segment of the population (Falk, 2014). Further research is needed to determine the best interventions to rehabilitate those who have sustained a TBI in order to prevent neurobehavioral problems resulting in incarceration, recurrent TBI, and to prevent life-long neurological decline in this vulnerable population of children throughout their life span.
Conclusions
Our findings have international implications as neurological decline is projected to be an increasing world-wide public health threat in aging populations (WHO, 2015). It is critical to recognize those at risk in order to plan prevention efforts. Parental incarceration impacts the long-term neuro-behavioral health of children. Along with being role models, adult family members promote a safe environment contributing to the physical, emotional, and neurological health of children throughout their lifespan. Children in extended families with incarcerated adults are a vulnerable population where initiatives are critically needed to prevent long-term consequences including life-long neurological decline. This is especially true for disproportionately higher rates of Black and Hispanics in the United States. Those who work with these children can play an important role in teaching them coping skills to prevent emotional and behavioral disorders, and improve resilience to adversity to prevent the cascade of events contributing to ongoing neurological decline. Children with incarcerated adult family members need support from their community. Particular attention is needed to help prevent high risk behaviors due to lack of regard for self and others that results in ongoing neurological decline throughout the life span of vulnerable populations of adult children of incarcerated adult family members.
Acknowledgments
Funding
Data collection for this study was funded in part by the National Institutes of Health 20RR016472-04, T32NR07036, Sigma Theta Tau International Honor Society, Rehabilitation Nursing Foundation, The Baxter Foundation, University of Delaware General University Research Fund, and University of Delaware Research Foundation.
Contributor Information
Kathleen Brewer-Smyth, School of Nursing, College of Health Sciences, University of Delaware, Newark, Delaware, USA.
Ryan T. Pohlig, College of Health Sciences, University of Delaware, Newark, Delaware, USA
Gabriel Bucurescu, United States Department of Veterans Affairs, Philadelphia, Pennsylvania, USA.
References
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Giles WH. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellis MA, Hughes K, Leckenby N, Jones L, Baban A, Kachaeva M, Terzic N. Adverse childhood experiences and associations with health-harming behaviours in young adults: surveys in eight eastern European countries. Bulletin of the World Health Organization. 2014;92(9):641–655. doi: 10.2471/BLT.13.129247. doi: http://dx.doi.org/10.2471/BLT.13.129247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer-Smyth K. Ethical, regulatory, and investigator considerations in prison research. ANS: Advances in Nursing Science. 2008;31(2):119–127. doi: 10.1097/01.ANS.0000319562.84007.22. [DOI] [PubMed] [Google Scholar]
- Brewer-Smyth K. Obesity, Traumatic Brain Injury, Childhood Abuse, and Suicide Attempts in Females at Risk. Rehabilitation Nursing. 2014;39(4):183–191. doi: 10.1002/rnj.150. doi: http://dx.doi.org/10.1002/rnj.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer-Smyth K, Bucurescu G, Shults J, Metzger D, Sacktor N, van Gorp W, Kolson D. Neurological function and HIV risk behaviors of female prison inmates. J Neurosci Nurs. 2007;39(6):361–372. doi: 10.1097/01376517-200712000-00007. [DOI] [PubMed] [Google Scholar]
- Brewer-Smyth K, Burgess AW, Shults J. Physical and sexual abuse, salivary cortisol, and neurologic correlates of violent criminal behavior in female prison inmates. Biological Psychiatry. 2004;55(1):21–31. doi: 10.1016/s0006-3223(03)00705-4. [DOI] [PubMed] [Google Scholar]
- Cole JH, Leech R, Sharp DJ, Alzheimer’s Disease Neuroimaging, I Prediction of brain age suggests accelerated atrophy after traumatic brain injury. Annals of Neurology. 2015;77(4):571–581. doi: 10.1002/ana.24367. doi: http://dx.doi.org/10.1002/ana.24367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MD. The intergenerational transmission of family violence: The neurobiology of the relationships among child victimization, parental mental health, and addiction. New York, NY, US: Oxford University Press; 2012. [Google Scholar]
- De Bellis MD, Spratt EG, Hooper SR. Neurodevelopmental biology associated with childhood sexual abuse. Journal of Child Sexual Abuse. 2011;20(5):548–587. doi: 10.1080/10538712.2011.607753. doi: http://dx.doi.org/10.1080/10538712.2011.607753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumont DM, Brockmann B, Dickman S, Alexander N, Rich JD. Public health and the epidemic of incarceration. Annual Review of Public Health. 2012;33:325–339. doi: 10.1146/annurev-publhealth-031811-124614. doi: http://dx.doi.org/10.1146/annurev-publhealth-031811-124614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumont DM, Wildeman C, Lee H, Gjelsvik A, Valera P, Clarke JG. Incarceration, maternal hardship, and perinatal health behaviors. Maternal and Child Health Journal. 2014;18(9):2179–2187. doi: 10.1007/s10995-014-1466-3. doi: http://dx.doi.org/10.1007/s10995-014-1466-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk KJ. Appreciative inquiry with nurses who work with children of incarcerated parents. Nursing Science Quarterly. 2014;27(4):315–323. doi: 10.1177/0894318414546410. doi: http://dx.doi.org/10.1177/0894318414546410. [DOI] [PubMed] [Google Scholar]
- Forsman M, Långström N. Child maltreatment and adult violent offending: population-based twin study addressing the ’cycle of violence’ hypothesis. Psychological Medicine. 2012;42(9):1977–1983. doi: 10.1017/S0033291711003060. [DOI] [PubMed] [Google Scholar]
- Foster H, Hagan J. The mass incarceration of parents in America: Issues of race/ethnicity, collateral damage to children, and prisoner reentry. Annals of the American Academy of Political and Social Science. 2009;623(1):179–194. doi: http://dx.doi.org/10.1177/0002716208331123. [Google Scholar]
- Huq AZ. Review of Children of the prison boom: Mass incarceration and the future of american inequality. Law & Society Review. 2015;49(1):282–284. doi: http://dx.doi.org/10.1111/lasr.12129. [Google Scholar]
- Lee H, Wildeman C, Wang EA, Matusko N, Jackson JS. A heavy burden: The cardiovascular health consequences of having a family member incarcerated. American Journal of Public Health. 2014;104(3):421–427. doi: 10.2105/AJPH.2013.301504. doi: http://dx.doi.org/10.2105/AJPH.2013.301504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee RD, Fang X, Luo F. The impact of parental incarceration on the physical and mental health of young adults. Pediatrics. 2013;131(4):e1188–e1195. doi: 10.1542/peds.2012-0627. doi: http://dx.doi.org/10.1542/peds.2012-0627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Muenzenmaier K, Cancienne J, Struening E. Reliability and validity of a measure of sexual and physical abuse histories among women with serious mental illness. Child Abuse and Neglect. 1996;20(3):213–219. doi: 10.1016/s0145-2134(95)00137-9. [DOI] [PubMed] [Google Scholar]
- Muenzenmaier K, Meyer I, Struening E, Ferber J. Childhood abuse and neglect among women outpatients with chronic mental illness. Hospital and Community Psychiatry. 1993;44(7):666–670. doi: 10.1176/ps.44.7.666. [DOI] [PubMed] [Google Scholar]
- Resnick MD, Ireland M, Borowsky I. Youth violence perpetration: What protects? What predicts? Findings from the National Longitudinal Study of Adolescent Health. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2004;35(5):424.e421–424.e410. doi: 10.1016/j.jadohealth.2004.01.011. [DOI] [PubMed] [Google Scholar]
- Slopen N, Koenen KC, Kubzansky LD. Cumulative adversity in childhood and emergent risk factors for long-term health. The Journal of pediatrics. 2014;164(3):631–638. e631–632. doi: 10.1016/j.jpeds.2013.11.003. doi: http://dx.doi.org/10.1016/j.jpeds.2013.11.003. [DOI] [PubMed] [Google Scholar]
- WHO. Neurological Disorders: Public Health Challenges. 2006 Retrieved Retrieved June 30, 2015, from http://www.who.int/mental_health/publications/neurological_disorders_ph_challenges/en/
- WHO. Dementia, a Public Health Priority. 2012 Retrieved June 30, 2015, from http://www.who.int/mental_health/publications/dementia_report_2012/en/
- WHO. Neurology and Public Health. Mental Health. 2015 Retrieved June 30, 2015, from http://www.who.int/mental_health/neurology/en/
- Widom CS. Motivation and mechanisms in the “cycle of violence”. Nebraska Symposium on Motivation. Nebraska Symposium on Motivation. 2000;46:1–37. [PubMed] [Google Scholar]
- Wildeman C. Imprisonment and (inequality in) population health. Social Science Research. 2012;41(1):74–91. doi: 10.1016/j.ssresearch.2011.07.006. [DOI] [PubMed] [Google Scholar]
- Wildeman C. Parental incarceration, child homelessness, and the invisible consequences of mass imprisonment. Annals of the American Academy of Political and Social Science. 2014;651(1):74–96. doi: http://dx.doi.org/10.1177/0002716213502921. [Google Scholar]
- Wildeman C, Andersen SH, Lee H, Karlson KB. Parental incarceration and child mortality in Denmark. American Journal of Public Health. 2014;104(3):428–433. doi: 10.2105/AJPH.2013.301590. doi: http://dx.doi.org/10.2105/AJPH.2013.301590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildeman C, Western B. Incarceration in fragile families. The Future of children / Center for the Future of Children, the David and Lucile Packard Foundation. 2010;20(2):157–177. doi: 10.1353/foc.2010.0006. [DOI] [PubMed] [Google Scholar]


