Abstract
The primary role of osteoblasts is to lay down new bone during skeletal development and remodelling. Throughout this process osteoblasts directly interact with other cell types within bone, including osteocytes and haematopoietic stem cells. Osteoblastic cells also signal indirectly to bone-resorbing osteoclasts via the secretion of RANKL. Through these mechanisms, cells of the osteoblast lineage help retain the homeostatic balance between bone formation and bone resorption. When tumour cells disseminate in the bone microenvironment, they hijack these mechanisms, homing to osteoblasts and disrupting bone homeostasis. This review describes the role of osteoblasts in normal bone physiology, as well as interactions between tumour cells and osteoblasts during the processes of tumour cell homing to bone, colonisation of this metastatic site and development of overt bone metastases.
1. The osteoblast in normal bone physiology
Under normal physiological conditions osteoblasts are responsible for the formation of new bone in the developing skeleton and during the process of bone remodelling. Osteoblasts arise from the differentiation of mesenchymal cells committed to osteoprogenitors in the periosteum, via a process that requires sequential action of the transcription factors Runx2 and osterix [1]. These cells form closely packed sheets on the surface of bone from which they extend cellular processes through the developing bone. In order to successfully lay down new bone osteoblasts produce a range of molecules, including enzymes, growth factors and hormones such as, alkaline phosphatase, collagenase, TGF β, IGFs, osteocalcin and type 1 collagen [1]. After the process of bone formation, matrix synthesising osteoblasts have three potential fates: Some osteoblasts become flattened and remain as quiescent lining cells at the bone surface and some die by apoptosis. However, with the deposition of new bone, the majority of osteoblasts gradually become surrounded by the bone matrix and as the matrix calcifies the cells (along with their associated cell products) gets trapped inside the resulting lacunae. At this point cells of the osteoblast lineage further differentiate into osteocytes [2], [3]. Osteocytes communicate with each other as well as with osteoblasts, via extensive cytoplasmic processes that occupy canaliculi within the bone matrix. Both bone lining cells and osteocytes have been identified as important sources of RANKL [4]. Thus, interactions between RANKL from osteoblasts/osteocytes and RANK on osteoclasts directly affect osteoclastogenesis, regulating osteoclastic bone resorption and the release of growth factors from the bone matrix.
2. Tumour cell homing and colonisation of bone
Bone is the third most common site for tumour cells to spread and bone metastasis affects more than 600, 000 people every year in the USA alone [5]. The site at which secondary tumours form is not random; for metastases to develop tumour cells must arrive in an environment that is permissive for their colonisation and subsequent growth. In the case of bone metastasis it is hypothesised that tumour cells home to specific niches: The endosteal niche (which is primarily made up of osteoblasts), the haematopoietic stem cell (HSC) niche and the vascular niche (reviewed by Maggague and Obenauf, 2016 and Weilbaecher, et al. 2011 [6], [7]. Evidence from in vivo models suggest that all of these niches play a role in tumour cell metastasis to bone and that interplay between these niches determines whether tumour cells proliferate to overt metastases or remain dormant.
2.1. The endosteal niche
In mouse models of breast and prostate cancer tumour cells have been shown to home to areas in bone that have high numbers of osteoblasts and in breast cancer models chemical alteration of the endosteal niche with zoledronic acid results in re-location of tumour cells to new osteoblast rich areas of bone [8], [9]. The CXCR4/CXCL12 interaction is thought to be a key component in the homing and adhesion of tumour cells to the metastatic niche in bone. Osteoblasts express the chemokine CXCL12 whereas the majority of metastatic breast and prostate cancer cells express the corresponding receptor CXCR4. Once tumour cells have colonised the endosteal niche evidence suggests that osteoblasts maintain these tumour cells in a quiescent state, through the interactions of CXCR4/CXCL12, using similar mechanisms to those used by osteoblasts for maintaining quiescence of HSCs [10].
2.2. The HSC niche
The HSC niche is also rich in CXCL12 and thus attracts CXCR4 positive tumour cells in the same way as the endosteal niche. Convincing data from models of prostate cancer show when tumour cells home to the HSC niche they compete with HSCs for colonisation of this site [10], [11]. Subsequent proliferation of tumour cells out of the niche, enabling onset of overt metastases, is thought to be facilitated by the mobilisation and proliferation of HSCs and this process is likely to be supported by the vascular niche [10], [11].
2.3. The vascular niche
The close proximity of the vascular niche to the endosteal and HSC niches in bone make it very difficult to study these niches independently in bone metastasis. Therefore, evidence that the vascular niche plays a significant role in metastasis primarily come from models of brain metastasis: Observations made from breast, lung and multiple myeloma cells that have metastasised to brain demonstrate that following extravasation, within the metastatic organ, cancer cells remain closely associated with the capillaries [12], [13]. These invading tumour cells spread along the basal lamina that surrounds the capillaries and proliferate, eventually, engulfing and remodelling the capillary network [13].
Taken together, these data suggest that within bone, the endosteal niche is responsible for maintaining tumour cells in a quiescent state, whereas the HSC and vascular niches stimulate proliferation to overt metastases. It is therefore likely that bone turnover and bone cell activity are important regulators in stimulating bone metastases from tumour cells seeded in this environment; a phenomenon that has long been observed in animal models [14], [15].
3. Progression to overt metastases
When established in bone, cancer cells influence bone cells in two predominant ways. Most often cancer cells stimulate the osteoclast lineage to increase osteoclast differentiation and activity whilst simultaneously inhibiting osteoblasts [2]. When this happens, osteoclastic bone resorption exceeds osteoblastic bone formation resulting in bone degradation and the formation of osteolytic lesions (common in breast, lung and multiple myeloma). In some cases, instead of inhibiting osteoblasts, cancer cells release substances to stimulate the osteoblast lineage to increase osteoblast differentiation and new bone deposition. When osteoblastic bone formation exceeds osteoclastic bone resorption increased bone growth results in 'bulges’ in the mineralised tissue where tumour cells reside causing osteoblastic lesions. Because osteoblastic bone metastases is characterised by increases in both bone resorption and bone formation lesions consist of weakened bone with abnormal architecture and patients with this condition are at increased risk of fracture (common in prostate) [16]. Although more patients present with osteolytic lesions than osteoblastic the distinction between the two-types is not absolute and many patients with bone metastasis have both osteolytic and osteoblastic lesions [17]. Mechanistically, osteoclasts and osteoblasts play significant roles in the formation of both lesion types, however, this article primarily focuses on osteoblasts. Evidence is emerging for a direct role of osteoblasts on tumour growth in bone. In a mouse model of breast cancer metastasis to bone, increasing the osteoblastic niche with PTH before intra-cardiac injection of human breast cancer cells caused an increase in numbers of overt bone metastases without altering tumour cell dissemination in bone [18]. Pro-tumourigenic effects of PTH have also been observed in rats treated with high doses of PTH [2]. However, in mouse models of multiple myeloma, daily injection with PTH suppressed tumour growth whilst increasing bone formation [19]. The effects of PTH on tumour growth in bone, however, may not be solely due to changes in osteoblasts. PTH treatment has profound affects upon the bone microenvironment that go beyond increased osteoblast numbers and activity. In all of the above studies PTH affected osteoclasts and it is likely that the gross morphological changes that occur in bone, following this treatment, are accompanied by alterations to the vascular niche, although this hypothesis remains to be explored. It has been suggested that osteoblasts and multiple myeloma cells have inhibitory effects upon each other and in their review Suvannasankha and Chirgwin hypothesise that these inhibitory effects may also occur between breast cancer cells and osteoblasts [2]. The effects of osteoblasts on tumour growth and progression to metastasis, therefore, warrants further investigation.
3.1. Osteoblasts in osteolytic bone metastases
Tumour cells within the bone marrow can alter the function of both osteoclasts and osteoblasts. In osteolytic bone metastases tumour cells secrete factors that stimulate osteoclast activity through the activation of the receptor activator of nuclear factor–κB ligand (RANKL)/RANK pathway, which is a primary mediator of osteoclast mediated bone resorption [17]. Additionally tumour cells secrete factors that inhibit osteoblast differentiation and activity including activin A, dickkopf-1 (DKK-1), sclerostin and noggin [17]. Thus leading to an imbalance between bone resorption and bone formation resulting in increased bone destruction. Increased bone resorption leads to a vicious cycle between tumour cells and bone cells in which growth factors such as TGFβ and IGF that were previously deposited in bone by osteoblasts are released from resorption pits, stimulating tumour cell proliferation. The tumour cells, in turn, produce more growth factors that stimulate bone turnover [7]. TGFβ plays a central role in this process; release of this molecule from bone directly stimulates tumour cells to secrete PTHrP, which in turn induces bone RANKL [20], [21]. Osteoblasts themselves also play a crucial role in initiation of bone resorption since osteoblast precursor cells produce RANKL, which stimulates osteoclast differentiation [22]. Initially, when tumours are small, they induce an increase in osteoclast activity and eliminate osteoblasts at the tumour/bone interface. To compensate for this local elevation in bone resorption growth factors from the resorbed bone stimulate osteoblast differentiation on the surface of bone proximal to the tumour generating localised increase in osteoclast stimulating RANKL [23]. At this point bone lesions develop and the latter stages of disease are predominantly osteoclast driven. Once osteolytic metastases are established in bone, the release in TGFβ from resorption pits inhibits osteoblast differentiation [17], ultimately resulting in the inhibition of new bone formation thus contributing to the bone disease.
3.2. Osteoblastic bone metastases
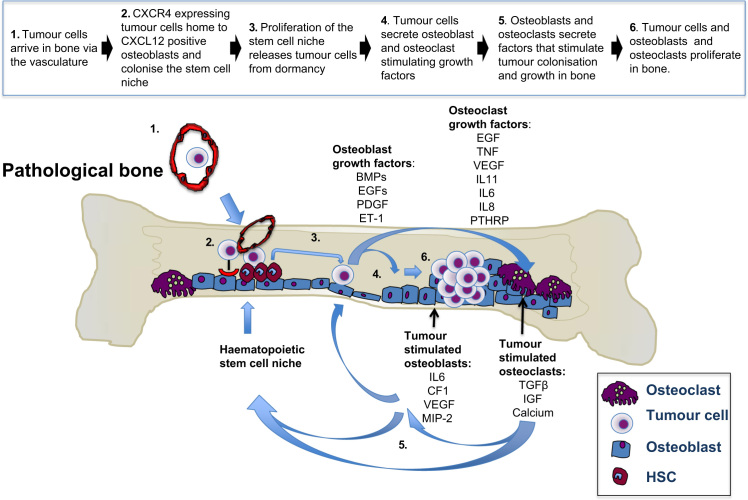
A vicious cycle between tumour cells and bone cells also exists for osteoblastic bone metastases (Fig. 1). In osteoblastic metastases the vicious cycle observed in osteolytic disease still occurs, however, in addition to this tumour cells within bone produce osteoblast-stimulating factors comprised of bone morphogenic protein (BMP)s, epidermal growth factor (EGF)s and platelet derived growth factor (PDGF). Tumour cells also secrete endothelin-1 (ET-1) which in turn downregulates (DKK-1) and stimulates osteoblatogenesis [24]. These activated osteoblasts produce factors including IL-6, monocyte chemotactic protein-1 (MCP-1), VEGF, and macrophage inflammatory protein 2 (MIP-2), which promote further cancer cell colonisation and growth in the bone environment.
Fig. 1.
Vicious cycle of osteoblastic bone metastases. Diagrammatic representation of the interactions between tumour cells, osteoblasts and osteoclasts during the processes of bone homing and colonisation in osteoblastic bone metastases.
4. Future directions
There is increasing evidence that osteoblasts are important components of the bone metastatic niche, but their precise contribution in supporting tumour cell engraftment, dormancy and survival remains to be defined. Unlike osteoclasts, the role of osteoblasts in bone metastasis is relatively under-investigated. Increased understanding of how this cell type interacts with tumour cells in the bone environment may be essential, if we are to identify better therapeutic strategies for treating patients with this condition. The potential importance of osteoblasts in therapies has already been acknowledged with novel treatments aimed at targeting bone formation already being put into clinical practise. Traditional drugs such as bisphosphonates were developed to target osteoclasts; however, these drugs also inhibit osteoblasts [8], [25]. Initial, laboratory testing indicated that targeting RANKL may be more selective, reducing osteoclasts whilst increasing bone formation, via increased differentiation of osteoblasts (reviewed by Sims and Romas, 2015 [26]). However, when used in clinic, the human RANKL inhibitor, denosumab inhibited serum bone resorption and formation markers in women with osteoporosis [27]. It therefore seems likely that the close coupling of osteoclasts/osteoblasts will make it impossible to use a single drug or a combination of drugs at the same time point, to both resorb and repair bone. It is also likely that osteoclast targeted therapies designed to prevent progression of osteolytic lesions in bone are also responsible for impaired healing and weakened bones seen in myeloma patients after administration of these treatments [28]. It is therefore proposed that a useful strategy to reverse bone loss would be to turn on osteoblast functions. Evidence from patients with multiple myeloma and lymphomas has demonstrated that the proteasome inhibitors bortezomib and carfilzomib both promote bone formation by stimulating progenitor proliferation and osteoblast differentiation. This drug is now FDA approved for patients with multiple myeloma and mantle cell lymphoma [2], [29], [30]. Furthermore, proteasome inhibitors have also been shown to prevent osteolytic lesion formation in pre-clinical models of breast cancer bone metastasis [31]. These data indicate that targeting osteoblasts in combination with osteoclast inhibition may provide promising bone sparing agents for patients with bone metastases [32]. However, it must also be noted that many drugs that have bone anabolic effects including the proteasome inhibitors bortezomib, carfilzomib as well as antibodies that neutralise the WNT inhibitors DKK1 and Sclerostin also have direct anti-tumour effects. It is, therefore, impossible to deduce whether these compounds are exerting bone sparing effects or whether decreased loss of bone is a side effect of reduced tumour burden [2], [30].
Unanswered questions
-
1.
Do osteoblasts play a part in both tumour cell homing and progression in bone?
-
2.
Can stimulating osteoblast activity result in repair of lytic bone lesions?
-
3.
Will osteoblast stimulating agents affect tumour growth in bone; will these affects be tumour type specific?
References
- 1.Karsenty G., Kronenberg H.M., Settembre C. Genetic control of bone formation. Annu. Rev. Cell Dev. Biol. 2009;25:629–648. doi: 10.1146/annurev.cellbio.042308.113308. [DOI] [PubMed] [Google Scholar]
- 2.Suvannasankha A., Chirgwin J.M. Role of bone-anabolic agents in the treatment of breast cancer bone metastases. Breast Cancer Res. 2014;16(6):484. doi: 10.1186/s13058-014-0484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prideaux M., Findlay D.M., Atkins G.J. Osteocytes: the master cells in bone remodelling. Curr. Opin. Pharmacol. 2016;28:24–30. doi: 10.1016/j.coph.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Xiong J., Onal M., Jilka R.L., Weinstein R.S., Manolagas S.C., O’Brien C.A. Matrix-embedded cells control osteoclast formation. Nat. Med. 2011;17(10):1235–1241. doi: 10.1038/nm.2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Randell R.L. A promise to our patients with met static bone disease. Ann. Surg. Oncol. 2014;21:4049–4050. doi: 10.1245/s10434-014-4010-1. [DOI] [PubMed] [Google Scholar]
- 6.Massague J., Obenauf A. Metastatic colonization by circulating tumour cells. Nature. 2016;529:298–306. doi: 10.1038/nature17038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weilbaecher K.N., Guise T.A., McCauley L.K. Cancer to bone: a fatal attraction. Nat. Rev. Cancer. 2011;11(6):411–425. doi: 10.1038/nrc3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haider M.T., Holen I., Dear T.N., Hunter K., Brown H.K. Modifying the osteoblastic niche with zoledronic acid in vivo-potential implications for breast cancer bone metastasis. Bone. 2014;66:240–250. doi: 10.1016/j.bone.2014.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shiozawa Y., Pedersen E.A., Havens A.M., Jung Y., Mishra A., Joseph J., Kim J.K., Patel L.R., Ying C., Ziegler A.M., Pienta M.J., Song J., Wang J., Loberg R.D., Krebsbach P.H., Pienta K.J., Taichman R.S. Human prostate cancer metastases target the hematopoietic stem cell niche to establish footholds in mouse bone marrow. J. Clin. Investig. 2011;121(4):1298–1312. doi: 10.1172/JCI43414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang N., Docherty F.E., Brown H.K., Reeves K.J., Fowles A.C., Ottewell P.D., Dear T.N., Holen I., Croucher P.I., Eaton C.L. Prostate cancer cells preferentially home to osteoblast-rich areas in the early stages of bone metastasis: evidence from in vivo models. J. Bone Miner. Res. 2014;29(12):2688–2696. doi: 10.1002/jbmr.2300. [DOI] [PubMed] [Google Scholar]
- 11.Pedersen E.A., Shiozawa Y., Pienta K.J., Taichman R.S. The prostate cancer bone marrow niche: more than just ‘fertile soil’. Asian J. Androl. 2012;14(3):423–427. doi: 10.1038/aja.2011.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kienast Y., von Baumgarten L., Fuhrmann M., Klinkert W.E., Goldbrunner R., Herms J., Winkler F. Real-time imaging reveals the single steps of brain metastasis formation. Nat. Med. 2010;16(1):116–122. doi: 10.1038/nm.2072. [DOI] [PubMed] [Google Scholar]
- 13.Carbonell W.S., Ansorge O., Sibson N., Muschel R. The vascular basement membrane as “soil” in brain metastasis. PLoS One. 2009;4(6):e5857. doi: 10.1371/journal.pone.0005857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ottewell P.D., Wang N., Meek J., Fowles C.A., Croucher P.I., Eaton C.L., Holen I. Castration-induced bone loss triggers growth of disseminated prostate cancer cells in bone. Endocr. Relat. Cancer. 2014;21(5):769–781. doi: 10.1530/ERC-14-0199. [DOI] [PubMed] [Google Scholar]
- 15.Ottewell P.D., Wang N., Brown H.K., Fowles C.A., Croucher P.I., Eaton C.L., Holen I. OPG-Fc inhibits ovariectomy-induced growth of disseminated breast cancer cells in bone. Int. J. Cancer. 2015;137(4):968–977. doi: 10.1002/ijc.29439. [DOI] [PubMed] [Google Scholar]
- 16.Hensel J., Thalmann G.N. Biology of bone metastases in prostate cancer. Urology. 2016;S0090–4295(15) doi: 10.1016/j.urology.2015.12.039. (01193–0) [DOI] [PubMed] [Google Scholar]
- 17.Krzeszinski J.Y., Wan Y. New therapeutic targets for cancer bone metastasis. Trends Pharmacol. Sci. 2015;36(6):360–373. doi: 10.1016/j.tips.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ottewell P.D., Brown H.K., Wang N., Wiegand K., Croucher P.I., Eaton C.L. Holen The dark side of bone anabolics? Intermittent PTH modifies the microenvironment to increase skeletal breast cancer metastasis in vivo. ECTS-IBMS. 2015 CABSOC1.4. [Google Scholar]
- 19.Yaccoby S. Osteoblastogenesis and tumor growth in myeloma. Leuk. Lymphoma. 2010;51(2):213–220. doi: 10.3109/10428190903503438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Juárez P., Guise T.A. TGF-β in cancer and bone: implications for treatment of bone metastases. Bone. 2011;48(1):23–29. doi: 10.1016/j.bone.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Sterling J.A., Guelcher S.A. Bone structural components regulating sites of tumor metastasis. Curr. Osteoporos. Rep. 2011;9(2):89–95. doi: 10.1007/s11914-011-0052-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Akhtari M., Mansuri J., Newman K.A., Guise T.M., Seth P. Biology of breast cancer bone metastasis. Cancer Biol. Ther. 2008;7(1):3–9. doi: 10.4161/cbt.7.1.5163. [DOI] [PubMed] [Google Scholar]
- 23.Sterling J.A., Edwards J.R., Martin T.J., Mundy G.R. Advances in the biology of bone metastasis: how the skeleton affects tumor behavior. Bone. 2011;48(1):6–15. doi: 10.1016/j.bone.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 24.Brown H.K., Ottewell P.D., Evans C.A., Holen I. Location matters: osteoblast and osteoclast distribution is modified by the presence and proximity to breast cancer cells in vivo. Clin. Exp. Metastas. 2012;29(8):927–938. doi: 10.1007/s10585-012-9481-5. [DOI] [PubMed] [Google Scholar]
- 25.Huang K.C., Cheng C.C., Chuang P.Y., Yang T.Y. The effects of zoledronate on the survival and function of human osteoblast-like cells. BMC Musculoskelet. Disord. 2015;16:355. doi: 10.1186/s12891-015-0818-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sims N.A., Romas E. Is RANKL inhibition both anti-resorptive and anabolic in rheumatoid arthritis? Arthritis Res. Ther. 2015;17:328. doi: 10.1186/s13075-015-0861-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reid I.R., Miller P.D., Brown J.P., Kendler D.L., Fahrleitner-Pammer A., Valter I., Maasalu K., Bolognese M.A., Woodson G., Bone H., Ding B., Wagman R.B., San Martin J., Ominsky M.S., Dempster D.W. Denosumab phase 3 bone histology study group. Effects of denosumab on bone histomorphometry: the FREEDOM and STAND studies. J. Bone Miner. Res. 2010;25(10):2256–2265. doi: 10.1002/jbmr.149. [DOI] [PubMed] [Google Scholar]
- 28.Silbermann R., Roodman G.D. Current controversies in the management of myeloma bone disease. J. Cell Physiol. 2016 doi: 10.1002/jcp.25351. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 29.Clines G.A., Mohammad K.S., Bao Y., Stephens O.W., Suva L.J., Shaughnessy J.D., Jr, Fox J.W., Chirgwin J.M., Guise T.A. Dickkopf homolog 1 mediates endothelin-1-stimulated new bone formation. Mol. Endocrinol. 2007;21(2):486–498. doi: 10.1210/me.2006-0346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Terpos E., Christoulas D. Effects of proteasome inhibitors on bone cancer. Bone Rep. 2013;2:395. doi: 10.1038/bonekey.2013.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jones M.D., Liu J.C., Barthel T.K., Hussain S., Lovria E., Cheng D., Schoonmaker J.A., Mulay S., Ayers D.C., Bouxsein M.L., Stein G.S., Mukherjee S., Lian J.B. A proteasome inhibitor, bortezomib, inhibits breast cancer growth and reduces osteolysis by downregulating metastatic genes. Clin. Cancer Res. 2010;16(20):4978–4989. doi: 10.1158/1078-0432.CCR-09-3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richardson P.G., Sonneveld P., Schuster M.W., Irwin D., Stadtmauer E.A., Facon T., Harousseau J.L., Ben-Yehuda D., Lonial S., Goldschmidt H., Reece D., San-Miguel J.F., Bladé J., Boccadoro M., Cavenagh J., Dalton W.S., Boral A.L., Esseltine D.L., Porter J.B., Schenkein D., Anderson K.C. Assessment of Proteasome Inhibition for Extending Remissions (APEX) investigators. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N.Engl. J. Med. 2005;352(24):2487–2498. doi: 10.1056/NEJMoa043445. [DOI] [PubMed] [Google Scholar]