Abstract
The Burkholderia pseudomallei complex classically consisted of B. mallei, B. pseudomallei, and B. thailandensis, but has now expanded to include B. oklahomensis, B. humptydooensis, and three unassigned Burkholderia clades. Methods for detecting and differentiating the B. pseudomallei complex has been the topic of recent research due to phenotypic and genotypic similarities of these species. B. mallei and B. pseudomallei are recognized as CDC Tier 1 select agents, and are the causative agents of glanders and melioidosis, respectively. Although B. thailandensis and B. oklahomensis are generally avirulent, both display similar phenotypic characteristics to that of B. pseudomallei. B. humptydooensis and the Burkholderia clades are genetically similar to the B. pseudomallei complex, and are not associated with disease. Optimal identification of these species remains problematic, and PCR-based methods can resolve issues with B. pseudomallei complex detection and differentiation. Currently, no PCR assay is available that detects the major species of the B. pseudomallei complex. A real-time PCR assay in a multiplex single-tube format was developed to simultaneously detect and differentiate B. mallei, B. pseudomallei, and B. thailandensis, and a common sequence found in B. pseudomallei, B. mallei, B. thailandensis, and B. oklahomensis. A total of 309 Burkholderia isolates and 5 other bacterial species were evaluated. The assay was 100% sensitive and specific, demonstrated sensitivity beyond culture and GC methods for the isolates tested, and is completed in about an hour with a detection limit between 2.6pg and 48.9pg of gDNA. Bioinformatic analyses also showed the assay is likely 100% specific and sensitive for all 84 fully sequenced B. pseudomallei, B. mallei, B. thailandensis, and B. oklahomensis strains currently available in GenBank. For these reasons, this assay could be a rapid and sensitive tool in the detection and differentiation for those species of the B. pseudomallei complex with recognized clinical and practical significance.
Introduction
Glanders, a disease caused by the Gram-negative bacillus Burkholderia mallei, is endemic in Africa, Asia, the Middle East, and Central and South America [1]. This bacterium does not survive well outside of the host and primarily infects equine populations such as horses, donkeys, and mules. Equine infection is largely due to ingestion of feed or water contaminated with nasal discharges from infected animals [1]. Human B. mallei infection is uncommon, but certain groups are at risk including veterinarians, slaughterhouse workers, equine butchers, equine handlers, and laboratory workers. For humans, infection is usually acquired by contact with infectious material through breaks in the skin or mucous membranes such as the eyes, nose, and mouth. The disease has a 95% case fatality rate for untreated septicemia [2] with death occurring in 7–10 days [3], and a 50% case fatality rate in antibiotic-treated patients [2].
Melioidosis, a disease caused by the saprophytic Gram-negative bacillus B. pseudomallei, is endemic in the sub-tropical areas of Southeast Asia and northern Australia. Unlike B. mallei, B. pseudomallei can easily survive outside of an infected host. The bacterium is commonly found in wet soils and stagnant waters, such as rice paddies, throughout endemic regions. High risk groups involve individuals who are in direct contact with wet soil including rice paddy workers, indigenous groups located in southern and eastern Asia, sub-tropical travelers, and individuals who are afflicted with immunosuppressive illnesses including diabetes mellitus, cirrhosis, thalassemia, renal disease, and alcoholism [4–6]. Melioidosis is acquired through inhalation, contact with cuts/wounds, or occasionally through ingestion of contaminated water [7, 8] with overall mortality rates of 40% in northern Thailand [8], 39% in Singapore [9], and 19% in Australia [5]. The infectious threat posed by melioidosis is gaining wider recognition because of the increasing number of melioidosis cases reported outside of Southeast Asia and northern Australia [10–13].
B. thailandensis, a saprophytic Gram-negative bacillus, is readily found in moist soils and stagnant water throughout Southeast Asia and northern Australia. In 1988, B. thailandensis was proposed as a new species distinct from B. pseudomallei because of differences in 16S rRNA gene (rDNA) sequences, biochemical profiles, and virulence traits [14]. B. oklahomensis, B. humptydooensis, and three unassigned Burkholderia clades A, B, C (respectively represented as BDU 5, BDU 8, and MSMB 0265) are B. thailandensis-like strains. The Burkholderia clades have not been assigned a species but are most related to B. oklahomensis [15]. B. oklahomensis was isolated in soil from Oklahoma, USA, B. humptydooensis was isolated from bore water from Humpty Doo, Northern Australia, and the Burkholderia clades are environmental isolates from Northern Australia [15–18]. The virulence of B. humptydooensis and the Burkholderia clades are currently unknown, although no human cases have been reported. B. thailandensis and B. oklahomensis are generally considered avirulent for mammals [19], but rare cases of disease have been documented [20–24]. B. thailandensis shares several virulence factor homologs with B. mallei and B. pseudomallei, making B. thailandensis a popular model organism to study Burkholderia pathogenesis. In addition, B. thailandensis and B. oklahomensis displays very similar characteristics to that of B. pseudomallei by various tests [16, 17, 25]. B. thailandensis and B. humptydooensis are known to co-localize with B. pseudomallei in the environment [16]. Therefore, these species can easily contaminate samples and/or produce false-positive results in current assays for melioidosis, leading to unnecessary treatment.
As previously stated, cases of illness from B. thailandensis and B. thailandensis-like strains have been reported, but may not fully represent the number of true cases of illness, due to limitations in current detection methods for these species. B. mallei and B. pseudomallei require BSL-3 management due to their virulence and classification by the CDC as Tier 1 select agents, and both pathogens have a history of bioweapon use [7, 26–30]. B. mallei and B. pseudomallei are known to be phylogenetically similar and it is generally recognized that B. mallei evolved as a strict pathogen from B. pseudomallei [31, 32]. B. thailandensis, B. oklahomensis, and B. humptydooensis also shares several phenotypic and molecular characteristics with B. mallei and B. pseudomallei [16–18, 33–37]. The B. pseudomallei complex was once comprised of B. pseudomallei, B. mallei, and B. thailandensis, but was recently expanded to include B. oklahomensis, B. humptydooensis, and three unassigned Burkholderia clades A, B, and C [15], due to the similarities of these species to those previously described.
Several methods have been developed for detection of various combinations of these species, which include serologic tests [38–42], commercial biochemical tests [43–46], Gas Chromatography Fatty Acid Methyl Esters (GC-FAME) [47], Gas Liquid Chromatography-Fatty Acid Methyl Esters [48], microscopic methods [49–51], Matrix Assisted Laser Desorption/Ionization Time-of-Flight [52], PCR subtractive hybridization technique [53], PCR-Restriction Fragment Length Polymorphisms [54] and gene sequencing [15, 36, 55, 56]. Serologic tests may be unreliable in endemic areas due to high seroconversion rates [7] for those previously exposed to the organism. Therefore, these serologic tests have low sensitivity and specificity in areas of endemicity [38, 57], but may prove useful in non-endemic areas. Biochemical assays have misidentified B. pseudomallei as Pseudomonas spp, B. vietnamiensis, Stenotrophomonas maltophilia, and Chromobacterium violaceum [43, 44, 46]. However, many of these methods require culture growth, which may take up to seven days to confirm a diagnosis. Consequently, improperly treated patients may die before receiving a correct diagnosis. Direct testing methods on clinical samples would prove most useful, but due to the low numbers of these organisms in many clinical samples, detection can be difficult.
With the exception of B. humptydooensis and the Burkholderia clades, culture growth is the gold-standard for clinical detection of the B. pseudomallei complex [21, 23, 58], but the high mortality rates of diseases caused by B. mallei and B. pseudomallei, their potential use as bioweapons, their low infectious dose, variable incubation periods, and diagnostic difficulties, necessitates the development of more rapid and accurate detection assays. The development of PCR technologies has revolutionized diagnostic testing methods for many microbial pathogens. These assays have become widely used due to their low detection limit, specificity, and speed. PCR-based assays for the rapid detection and differentiation of the B. pseudomallei complex have been the topic of much recent research. Optimal identification of these species remains problematic, due to difficulties in developing a sensitive and selective assay [59]. There are several real-time PCR assays that detect a single species in the B. pseudomallei complex [59–65]. Some of these assays were further validated with additional Burkholderia species DNA or evaluated for clinical and environmental use [60, 66–70]. Several PCR assays can detect multiple species of the B. pseudomallei complex, but due to their genetic similarity, these assays have not included species-specific primers. Current assays that detect and differentiate the B. pseudomallei complex frequently have only one species-specific primer set paired with other primers that detect the species as a complex. When all primers are tested against a sample, a unique amplification profile is created. Therefore, all primer sets are necessary to detect and differentiate the B. pseudomallei complex. These non-species specific assays are accomplished by multiplex PCR by Koh et al. [71] and Lee et al. [72] and real-time PCR by Thibault et al. [25]. Although these PCR studies have shown discrimination, they employ traditional PCR methods which have inherent limitations on throughput. The real-time PCR assay by Thibault et al. [25] has the potential for higher throughput, but requires three separate real-time PCR reactions in order to correctly identify B. pseudomallei, B. mallei, and B. thailandensis. Some follow-up studies of Thibault et al's B. mallei and B. pseudomallei assays [25] have reported a decreased specificity in the detection of non-B. pseudomallei complex species [59, 64, 65, 70, 73]. Currently, only three real-time PCR species-specific assays can detect some members of the B. pseudomallei complex. Two duplex real-time PCR assays detect B. mallei and B. pseudomallei based on a single-nucleotide polymorphism (SNP) [74, 75]. The third real-time PCR species-specific assay detects and differentiates B. pseudomallei from the B. thailandensis, B. thailandensis-like, and B. oklahomensis group [76]. To date, no PCR assay has been developed that can specifically detect and differentiate between B. mallei, B. pseudomallei, and B. thailandensis in a single-tube format. Therefore, the purpose of this study was to develop and validate a real-time PCR assay that could quickly, accurately, and precisely detect and differentiate several species of the B. pseudomallei complex. This has potential applications in rapidly determining sources of infection in human patients in endemic regions, particularly in detecting contaminated environments like soil, and in differentiating between pathogenic and non-pathogenic members of the B. pseudomallei complex.
Materials and Methods
Bacterial Isolates and Culture Conditions
The 314 bacterial isolates used in this study (S1 Table) were acquired from the American Type Culture Collection (ATCC), Culture Collection, University of Göteborg (CCUG), Centers for Disease Control and Prevention (CDC), National Collection of Type Cultures (NCTC), Public Health England (PHE), Royal Darwin Hospital (RDH), University of Calgary (UC), and Utah Department of Health (UDH). The isolates were grown on Columbia agar (Remel) at 28–37°C for 1–3 days prior to DNA extraction. A genetically diverse panel of isolates was used in this study, which consist of human, animal, and environmental samples originally isolated from 24 countries (S2 Table).
DNA Extraction
Total genomic DNA was extracted from each isolate by first suspending cells grown on Columbia agar plates in 510 μL of Tris/EDTA buffer [10 mM Tris/HCl (pH 8.0), 1 mM EDTA] containing 1.8 μg μL-1 lysozyme, and incubating for 40 minutes at 37°C. To this tube, 540 μL of bacterial lysis buffer and 100 μL of proteinase K were added, after which it was incubated for 10 min at 65°C followed by an automated DNA extraction performed with a Roche MagNA Pure LC system (Roche Diagnostics), using the Roche MagNA Pure LC DNA Isolation Kit III as recommended by the manufacturer. DNAs were tested for biological growth by plating 10% of the DNA sample volume on Columbia Agar (Remel) at 28–37°C for five days. When the DNA samples passed sterility, DNA concentrations were measured with a TBS-380 Fluorometer (Promega) using the Quant-iT PicoGreen dsDNA assay kit P11496 (Invitrogen).
Primer and Probe Design
DNA sequences unique to B. mallei, B. pseudomallei, and B. thailandensis, as well as a unique target common among B. pseudomallei, B. mallei, and B. thailandensis were obtained from NCBI GenBank (http://www.ncbi.nlm.nih.gov/genbank). Several genes were targeted for B. pseudomallei complex detection and differentiation. A gene that encodes a 16.5 kDa hypothetical protein (Accession number YP_001024199 Locus tag = BMA10229_0375) was reported to be unique to B. mallei [77]. Orf11 (Accession number AF074878) was reported to be unique to B. pseudomallei [25, 78]. A gene that encodes a 70 kDa hypothetical protein (Accession CP000086 Locus tag = BTH_I1515) was reported to be specific to B. thailandensis [79]. Flagellar structural protein, fliC (Accession numbers U82287, AF084815, AF081500) was reported to be exclusive to the entire B. pseudomallei complex [80, 81]. These regions were used to design the primers and probes reported in this study. All primers and 5'-hydrolysis dual-labeled probes (Table 1), except for the fliC dual-labeled probe, were designed using the PrimerQuest algorithms from Integrated DNA Technologies (IDT) (http://www.idtdna.com/primerquest/Home/Index). The fliC dual-labeled probe was designed by comparing fliC gene sequences of B. pseudomallei, B. mallei, B. thailandensis, and B. vandii ATCC 51545 (GenBank Accession KM242678). All oligo sequences were selected for proper GC content, optimal annealing temperatures, and lack of hairpin structures. A thorough NCBI BLASTn search and/or analysis of sequence alignments using MEGA 6.0 [82] were performed to ensure both primer and probe specificity and lack of homology with sequences from other organisms. Oligos were considered for further evaluation if NCBI BLASTn had expect-values close to zero and identity values close to 100% for the intended species. Probes were fluorescently labeled as follows: 16.5 kDa (B. mallei) with Cy5, orf11 (B. pseudomallei) with FAM, 70 kDa (B. thailandensis) with Tex615, and fliC (B. pseudomallei, B. mallei, and B. thailandensis group) with Cy3.
Table 1. Primer and probe sequences of the quadruplex assay.
| Target gene (species) | Oligo | Sequence (5’ → 3’) | Amplicon Size (bp) |
|---|---|---|---|
| 16.5 kDa | |||
| B. mallei | Forward | CGT TCG AGC TCA GCA ACC TCG TTA | 85 |
| Reverse | AAG CGG TGA TGG ACC GCT GTA T | ||
| Probe | Cy5 -CAG TAT CCA GGT TTC ACC GCG CTC GAC-IAbRQ | ||
| Orf11 | |||
| B. pseudomallei | Forward | AAC ACT GAC AAG TGG CCC TAT GGA | 185 |
| Reverse | TCC GAT CGG TTT CGA ATA ACG GGT | ||
| Probe | FAM -ACG ATC TCC-ZEN-GAG AAC GCA CTG AAC A-IAbFQ | ||
| 70 kDa | |||
| B. thailandensis | Forward | AAC CTG AGG CAA CGC AAG AAG AAG | 99 |
| Reverse | TTT CTT CAC GCA TTC CCA ACC CTG | ||
| Probe | Tex615 -TCA AGG CGA GCT GTG CCG ACA ACA A-IAbRQ | ||
| fliC | |||
| Bp, Bm, & Bt group | Forward | ACG GTC AAC AAY CTG CAG GCA A | 143 |
| Reverse | TTC GCG GTT TCC TGA GCR AAG TC | ||
| Probe | Cy3- GGC TCG AAC AAC CTC GCG CAR G-IAbRQ | ||
IAbRQ, Iowa Black RQ Quencher; IAbFQ, Iowa Black FQ Quencher; ZEN, ZEN Internal Quencher; Bp, B. pseudomallei; Bm, B. mallei, Bt, B. thailandensis
Sequence Analysis
Sequencing was used to further analyze three Burkholderia strains. A portion of the fliC gene of B. vandii ATCC 51545 was amplified with forward primer 5' CGG CTT CAC GTT CAC CGA YCA G and reverse primer 5' GCA GGA GCT TCA GCA CTT GCT G. The 16S rRNA gene of B. pseudomallei 135 and MSHR 1816 was amplified using in-house 16S rDNA universal forward primer 5' ACT CCT ACG GGA GGC AGC AGT and reverse primer 5' TAC GGT TAC CTT GTT ACG ACT T. For every reaction, a master mix of 25 μL was prepared using 1x Hot Start Mix RTG Master Mix (GE Healthcare) and the following: 500 nM of each amplification primer, 2 μL target DNA, and PCR H2O to 25 μL. The mixtures were loaded into 0.2 ml PCR tubes, and PCR was performed using a GeneAmp PCR System 9700 (Applied Biosystems). The reaction mix for the fliC product was initially denatured at 95°C for 3 min followed by 30 cycles of 95°C for 15 sec, 61°C for 30 sec, 72°C for 1 min, and a final extension of 72°C for 5 min. The reaction mix for the 16S rDNA product was initially denatured at 95°C for 5 min followed by 30 cycles of 94°C for 15 sec, 58°C for 30 sec, 72°C for 1 min, and a final extension of 72°C for 5 min.
PCR products were purified with the Exo-SAP IT (Affymetrix) using manufacturer's recommendations. The purified PCR product was sequenced using 500 nM of each sequencing primer. The fliC forward sequencing primer 5' AAC GCA GCA AGC CAA CGC and reverse primer 5' TCT GGA TTT GCG ATT GAG CCG AC were used. The amplification primers for the 16S rDNA product and forward primer 5' AGA GTT TGA TCC TGG CTC AG were used as sequencing primers. Sequencing was performed with a BigDye Terminator version 3.1 cycle sequencing kit (Life Technologies) as per manufacturer's recommendations. Sequencing products were purified with a Sephadex spin (GE Healthcare) column and resolved with a 3730 DNA Analyzer (Life Technologies). The region of interest was re-amplified and re-sequenced at least twice to ensure sequence accuracy.
MEGA 6.0 was used to align sequences [82], and the sequences were analyzed using the Ribosomal Database Project (http://rdp.cme.msu.edu/seqmatch/seqmatch_intro.jsp), Greengenes (http://greengenes.lbl.gov/cgi-bin/nph-index.cgi), and NCBI BLASTn (http://blast.ncbi.nlm.nih.gov/Blast.cgi) databases.
IDT's DNA Thermodynamics & Hybridization (http://biophysics.idtdna.com/) software was used to predict how SNPs would affect oligo binding efficiency. All components of the orf11 assay, fliC probe, and fliC forward primer were further examined using this software. Tm, Gibbs Energy, Enthalpy, Entropy, and fraction of duplex values were generated for each match or mismatch along with a hybridization mismatch profile.
Real-time PCR Singleplex Optimization
Important parameter variables such as the number of PCR cycles, cycle temperatures, and length of annealing and elongation steps, were all optimized. Primers were first evaluated with SYBR Green to optimize cycle temperatures and times. For every reaction, a master mix of 25 μL was prepared using 1x Hot Start Mix RTG Master Mix (GE Healthcare) and the following: forward and reverse primers at 500 nM, 2 μL target DNA, 1.25 μL SYBR Green at a 25x concentration and PCR H2O to 25 μL. The mixtures were loaded into 25 μL Cepheid PCR tubes, and PCR was performed using a SmartCycler II (Cepheid). During the cycling phase, the annealing/extension temperature was varied from 57°C to 65°C in single degree increments to maximize the reaction. The optimized procedure identified and used for the 16.5 kDa singleplex assay was 550 nM of each primer, 300 nM of probe (Table 1) with an initial denaturation at 95°C for 150 s followed by 40 cycles of 95°C for 15 s, then 61°C for 50 s. The optimized protocol identified and used for the orf11 singleplex assay was 450 nM of each primer, 300 nM of probe with an initial denaturation at 95°C for 150 s followed by 35 cycles of 95°C for 15 s, then 61°C for 45 s. The 70 kDa assay was optimized using 400 nm of each primer and 250 nm of probe, and the fliC assay used 450 nM of each primer and 400 nM of each probe. The optimized procedure identified and used for both the 70 kDa and fliC singleplex assays was an initial denaturation at 95°C for 150 s followed by 35 cycles of 95°C for 15 s, then 61°C for 50 s. A sample was determined positive if it crossed a fluorescence threshold of 30 for the 16.5 kDa test before cycle 40 (a CT value of less than 40). A sample was determined positive if it crossed a fluorescence threshold of 30 before cycle 35 for the orf11 and 70 kDa assay. Lastly, the sample was determined positive if the fluorescence threshold crossed 15 for the fliC assay before cycle 35. DNA from near-neighbors and no template were used as negative controls.
Multiplexing the Four Singleplex Real-time PCR Assays
Once the single reaction conditions were optimized, the four assays were multiplexed (quadruplexed) into a single-tube format. For each reaction, 1.5x Hot Start Mix RTG master mix (GE Healthcare) was added to a mixture of 600 nM of each primer and 400 nM of probe for the 16.5 kDa test, 200nM of each primer and probe for the orf11 protocol, 250 nM of each primer and 200 nM of each probe for the 70 kDa test, and 400 nM of each primer and 250 nM of probe for the fliC assay. Two μl of target DNA and PCR-grade H2O were added for a total reaction volume of 25 μL. Thermal cycling conditions were an initial denaturation at 95°C for 150 s followed by 35 cycles of 95°C for 15 s, then 61°C for 50 s. A sample was determined to be positive if the 16.5 kDa, orf11, 70 kDa, and fliC tests crossed a fluorescence threshold of 15, 20, 30, and 15, respectively before cycle 35. The Cepheid software allowed four optics channels to be monitored in real-time simultaneously. DNA from near-neighbors and no template were used as negative controls. The optimized real-time protocol was evaluated using isolated DNA from 13 B. mallei isolates, 275 B. pseudomallei isolates, 11 B. thailandensis isolates, and 15 genetic near-neighbors (S1 Table).
Validation of the Multiplex Assay
The identities of the bacterial strains used in this study were verified by both cellular fatty acid (CFA) profiles and previously published molecular assays. CFA analyses were performed using the Sherlock Microbial Identification System (MIDI). CFAs were extracted, methylated, and processed on a 6890N Network GC System (Agilent Technologies), and the data analyzed using Sherlock, version 6.1 software. The GC-FAME profiles were compared to the Rapid Bioterrorism library (RBTR3) and given a match and similarity index.
To further verify the validity of the multiplex assay and ensure the correct identification of B. mallei, B. pseudomallei, and B. thailandensis, real-time PCR assays were used. Adapted versions of the assays developed by U'Ren et al.[74] and Thibault et al.[25] were used on all samples listed in this study. The primer sequences employed were identical to those reported by U'Ren et al. [74], for detection and differentiation of B. mallei and B. pseudomallei. U'Ren et al's duplex procedure [74] was used by mixing 1x Hot Start Mix RTG Master Mix (GE Healthcare), 375 nM of each of the B. mallei and B. pseudomallei primers and probes, 2 μL of target DNA, and PCR-grade H2O to 25 μL. The reactions were then run in the SmartCycler II with the following cycling conditions: 95°C for 150 s followed by 40 cycles of 95°C for 15 s, then 60°C for 45 s. Since a real-time PCR assay is currently unavailable for B. thailandensis-specific detection, Thibault et al's test [25] was used to detect B. thailandensis by adding 1x Hot Start Mix RTG Master Mix (GE Healthcare), 500 nM of each BpSCU2 primer and 200 nm probe, 2 μL of target DNA, and PCR-grade H2O to 25 μL. The reactions were then run in the SmartCycler II with the following cycling conditions: 95°C for 150 s followed by 35 cycles of 95°C for 20 s, then 56°C for 60 s. If a sample was negative by U'Ren et al's assay [74] and positive by Thibault et al's assay [25], it was considered positive for B. thailandensis.
Results
Sensitivity and Specificity Testing
Initial sensitivity and specificity of each primer was evaluated in separate tubes using SYBR Green to detect amplification. All assays except for the fliC test yielded threshold amplification in the presence of DNA for their respective Burkholderia species. Due to consistent amplification of B. vandii by the fliC primers, a fliC probe was designed to exclude B. vandii (S1 Fig). Having established that the primers were highly specific to their respective DNA targets, SYBR Green was replaced with four specific dual-labeled hydrolysis probes for B. mallei, B. pseudomallei, B. thailandensis, and the common B. pseudomallei, B. mallei, and B. thailandensis group which further increased specificity while maintaining sensitivity to the respective Burkholderia species. This also allowed the generation of a multiplexed assay in a single-tube format. All isolates were tested and signal thresholds were exceeded only when DNA for a specific species was present, indicating target sensitivity and specificity.
Of the 314 isolates examined in this study, two purported B. pseudomallei isolates produced atypical results (S1 Table). These isolates were undetected by the orf11 and fliC assays and both strains tested negative by the previously published assays used in this study [25, 74]. These two isolates were purported to be B. pseudomallei strains 135 and MSHR 1816. These isolates, received from personal collections of PHE and RDH, were identified as B. pseudomallei through culture methods. MIDI results from both isolates did not correlate with culture methods, and sequencing data indicated they were not species of the B. pseudomallei complex. Therefore, against the remaining 312 isolates, all four assays developed in this study were both 100% sensitive and specific for species detection and differentiation.
Since no one physical repository of bacterial DNA samples is complete, we wished to further validate the assays using bioinformatic methods. Specifically, all fully sequenced B. mallei (14), B. pseudomallei (52), B. thailandensis (10), B. oklahomensis (2), and B. humptydooensis (2) strains along with single isolates of B. multivorans, B. cenocepacia, B. ubonensis, B. vietnamiensis, B. dolosa, and B. cepacia strains found in NCBI GenBank were compared with our primer/probe sets (S3 Table). Fully sequenced strains from the Burkholderia A, B, and C clades were not available. The NCBI Blastn results indicate that the two publicly available strains of B. oklahomensis, members of the B. pseudomallei complex, are predicted to be detected by the fliC assay. In addition, NCBI BLASTn results indicates the identity values of B. humptydooensis MSMB 121, another member of the B. pseudomallei complex, were close to 100% for the fliC oligos, but the expected values were sporadic with the forward, reverse, and probe, respectively having values of 19, 22, and 0.067. These values strongly suggest the fliC assay would not identify this species. Therefore, this isolate was predicted to be undetected by the fliC assay. Our primer/probe sets were found to be 100% specific to the selected NCBI GenBank sequences (S3 Table). Eighteen B. pseudomallei, three B. thailandensis, and two B. oklahomensis isolates have a nucleotide mismatch with oligos used in the orf11 assay (S3 and S4 Tables) and/or the fliC assay (S3 and S5 Tables). Single nucleotide mismatches sometimes allow correct primer/probe binding and sometimes prevent correct primer/probe binding [83–85], therefore these mismatches were further investigated using IDT's DNA Thermodynamic & Hybridization software (S2 and S3 Figs). This software predicts the potential binding success of a mismatch oligo at various temperatures. A fraction of duplex (FoD) value close to 1.0 indicates a higher likelihood of successful binding, and mismatch FoD values generated from the assays ranged from 0.926 to 0.997 (S4 and S5 Tables). It was also shown that using the specific temperature and salt conditions of the singleplex assays, these isolates would very likely still be identified correctly by all four assays (S2 and S3 Figs). In addition, two of the sixteen B. pseudomallei strains containing mismatches with the orf11 assay were previously tested by the multiplex assay, MSHR 146 and PHLS 112 (PHE 112), and both isolates tested positive on the B. pseudomallei specific and fliC assays. Therefore, the sensitivity and specificity of all four assays developed in this study appear to be 100% against the 314 strains in our collection and 84 strains with bioinformatic results. However, if in the future it was determined that the present primers/probes do not specifically detect new isolates, then a slight modification including degenerate bases would likely correct this situation, as is commonly performed [86, 87].
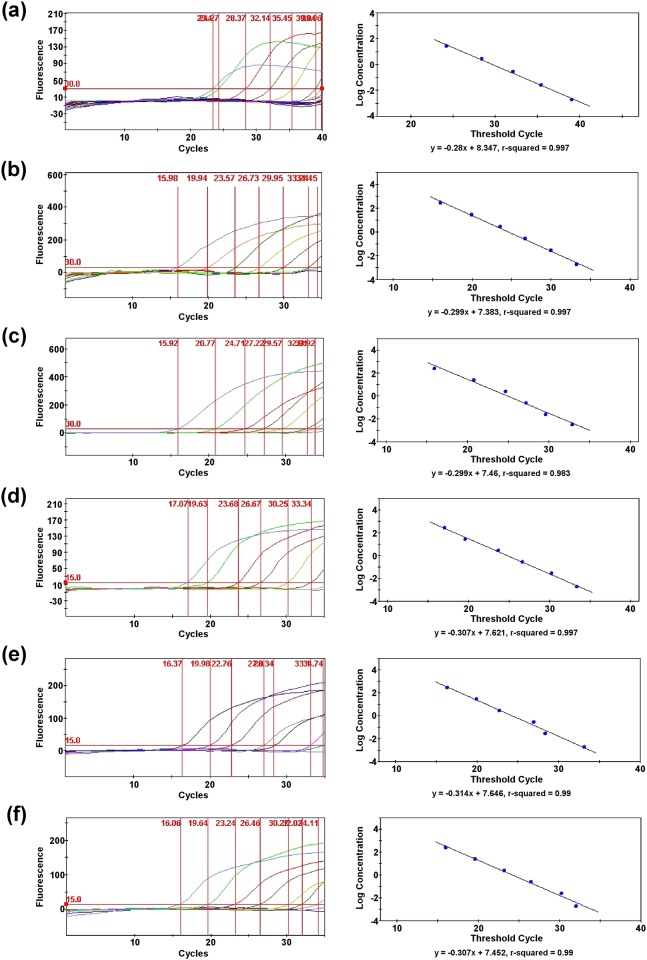
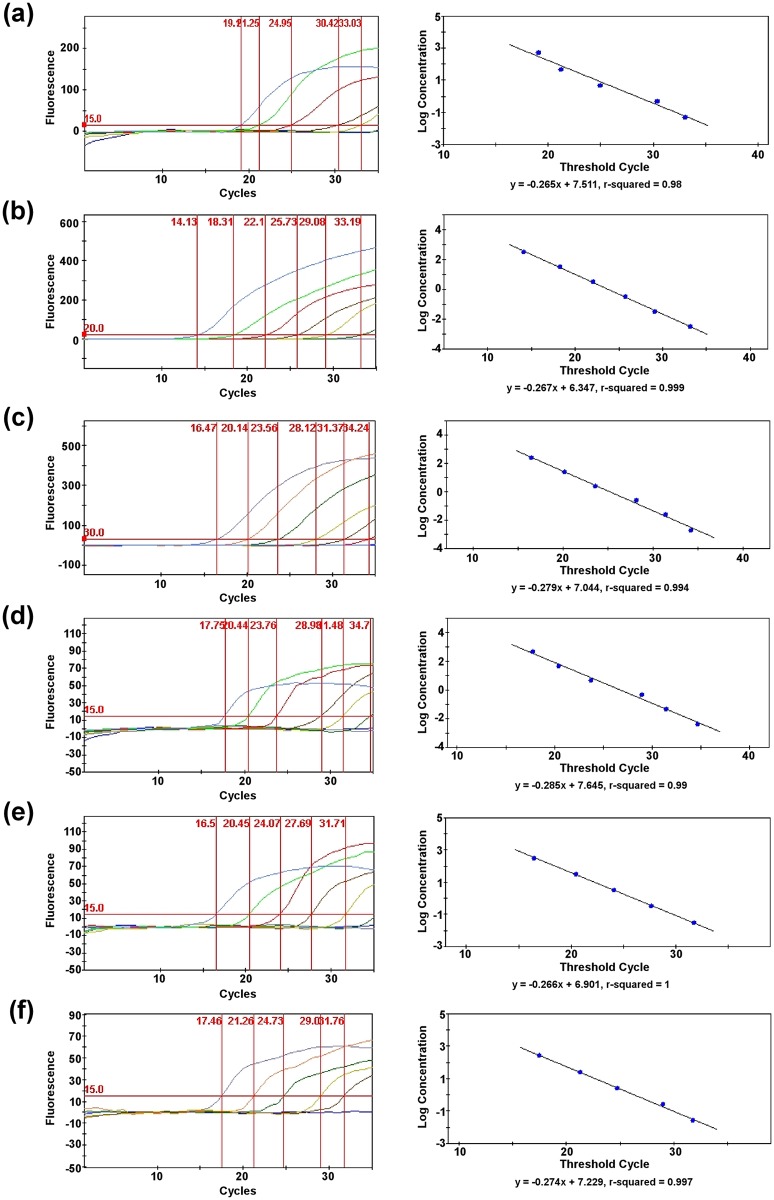
Limit of Detection Testing
For each Burkholderia species targeted in the multiplex assay, serial dilutions were made of the purified genomic DNAs, and a genomic equivalent (GE) calculation was determined. For the species-specific singleplex assays, the threshold detection limits were at least 977.2 fg (158 GE) for B. mallei, 316.16 fg (~40 GE) for B. pseudomallei, and 520 fg (~72 GE) for B. thailandensis (Fig 1). For the fliC singleplex assay, the threshold sensitivities were at least 4.886 pg (788 GE) for B. mallei, 316.16 fg (~40 GE) for B. pseudomallei, and 520 fg (~72 GE) for B. thailandensis. For the quadruplex assay, the detection limits of the species-specific targets were at least 48.86 pg (7,880 GE) for B. mallei, 3.1616 pg (404 GE) for B. pseudomallei, and 2.6 pg (358 GE) for B. thailandensis (Fig 2). For the fliC component of the multiplex assay, the threshold detection limits were at least 4.886 pg (788 GE) for B. mallei, 31.616 pg (4,040 GE) for B. pseudomallei, and 26 pg (3,580 GE) for B. thailandensis.
Fig 1. Sensitivity of the singleplex assays.
Detection limits of the singleplex assays and standard curves derived from serial dilutions of purified genomic DNAs for some species of the B. pseudomallei complex. (a) 16.5 kDa assay for B. mallei, (b) orf11 assay for B. pseudomallei, (c) 70 kDa for B. thailandensis, (d) fliC assay for B. mallei, (e) fliC assay for B. pseudomallei, and (f) fliC assay for B. thailandensis.
Fig 2. Sensitivity of the multiplex assay.
Detection limits of the quadruplex assay and standard curves derived from serial dilutions of purified genomic DNAs for some species of the B. pseudomallei complex. (a) 16.5 kDa assay for B. mallei, (b) orf11 assay for B. pseudomallei, (c) 70 kDa assay for B. thailandensis, (d) fliC assay for B. mallei, (e) fliC assay for B. pseudomallei, and (f) fliC assay for B. thailandensis.
Comparing the Multiplex Assay
The GC-FAME results showed identification discrepancies for some isolates used in this study. The GC-FAME RBTR3 library was unable to distinguish the fatty acid profiles of some B. pseudomallei and B. thailandensis isolates. In addition, four B. pseudomallei MSHR isolates were identified as B. mallei or B. cenocepacia/B. pyrrocinia/B. ambifaria (S1 Table). In short, the GC-FAME sensitivity and specificity for B. mallei was respectively 100% (13/13) and 98.6% (282/286) while the sensitivity and specificity for B. pseudomallei was respectively 98.5% (269/273) and 57.7% (15/26). All of the B. thailandensis isolates used in this study were identified as B. pseudomallei. Two previously published real-time PCR tests described by U'Ren et al. [74] and Thibault et al. [25] were performed to compare with the results obtained by our real-time PCR assay. The results of these previously published tests correlated exactly with the multiplex assay. U'Ren et al's duplex assay [74] correctly identified the B. mallei and B. pseudomallei isolates used in this study. The two presumed B. pseudomallei strains were also negative by U'Ren et al's assay [74]. In addition, Thibault et al's assay [25] was positive for the B. thailandensis strains used in this study.
Discussion
Glanders and melioidosis are significant diseases with high mortality rates, if left untreated. The difficulty in identifying the species of the B. pseudomallei complex and the bioweapon potential of some of these species necessitated the development of a more rapid and accurate detection method. Having access to accurate PCR assays with minimal diagnostic times could decrease mortality rates. Although at present there is limited access to PCR in some endemic areas, access is likely to continue increasing in the future.
Although PCR-based procedures have revolutionized microbial detection, they do have limitations. Both false positives and false negatives can occur [88, 89]. Some of this can be minimized with good technique, and some can be minimized with good assay design. It is possible, especially in newly emerging pathogens, for mutations to occur in the gene of interest, which can then compromise the test [90]. This issue can be overcome by developing multiplex assays.
Some studies showing false positive results have reported sensitivities beyond culture for clinical and environmental samples, that correlate with serological, radiological, and/or additional PCR-based assays [59]. Detection of non-viable B. pseudomallei in clinical samples from confirmed melioidosis patients has also been observed [91]. Although PCR false positives are considered inaccurate, they may represent the presence of unculturable Burkholderia species in clinical and environmental samples, and therefore may be more accurate than culture due to the inability of some bacteria to grow via existing culture methods. One study observed that 45% of septicemic melioidosis patients exhibited less than 1 CFU/mL of B. pseudomallei in their blood samples [92], which reinforces the need for sensitive testing methods such as PCR-based assays. Another possibility for some false positive results in unknown samples may be due to near-neighbors with similar DNA sequence to the targets, thus highlighting the need for multiple targets in a molecular assay.
In a recent review of all real-time PCR assays developed for detection and differentiation of B. pseudomallei, B. mallei, and B. thailandensis, it was observed that mutations in the form of gene deletions have affected assay sensitivity in only two studies [59]. Three strains from these studies lacked some virulence loci, indicating possible avirulent variants of B. mallei and B. pseudomallei. From these limited examples, it appears mutations within PCR-targeted genes have not significantly compromised the reliability of PCR-based tests for the detection of B. pseudomallei complex organisms. It is widely accepted that B. mallei evolved as a strict pathogen from B. pseudomallei [31, 32]. Despite the major evolutionary changes between these two species, they continue to be identified as a complex in several PCR-based methods.
Real-time PCR is able to resolve some of the limitations previously described, because of the versatility and additional specificity of the internal probe. The probe technology allows for simultaneous detection of multiple targets, which can overcome the problem of potential gene mutations at a single locus. Overall, real-time PCR assays are generally considered to have a large dynamic range, low inter-assay variation, and high reliability [93].
GC-FAME analysis identified B. pseudomallei MSHR 2394 as B. cenocepacia/B. pyrrocinia/B. ambifaria, and B. pseudomallei MSHR strains 1912, 1954, and 1986 as B. mallei. GC-FAME analysis also identified the purported B. pseudomallei 135 as B. mallei while the purported B. pseudomallei MSHR 1816 produced no match. A 98% sensitivity and an 83.3% specificity for B. pseudomallei strains was reported by GLC-FAME analysis [48]. Our results confirmed Inglis et al's conclusion [48] that a PCR-based method was more accurate and precise than GC-FAME methods.
The multiplex assay described here is the first of its kind that can detect and differentiate between B. mallei, B. pseudomallei, and B. thailandensis in a single-tube format. This test has overcome several PCR-based drawbacks related to sensitivity and specificity. The negative results produced by the two purported B. pseudomallei isolates increases the reliability of the multiplex assay, in that it displayed a higher sensitivity than culture. The multiplex assay may help future research determine if PCR-based assays could replace culture methods, since the fliC target functions as a second confirmation within the assay. If a species-specific target in the multiplex assay fails, the fliC target detects the entire B. pseudomallei, B. mallei, B. thailandensis, and possibly B. oklahomensis group and can still detect and differentiate by creating a unique amplification profile.
It was reported that B. sordidicola CCUG 49583 and two B. thailandensis strains were detected by Thibault et al's B. pseudomallei specific orf11 assay [65]. The orf11 target used in the multiplex assay was negative for the same B. sordidicola strain, and was also negative for the 11 B. thailandensis strains evaluated in this study. The high sensitivity of real-time PCR also proved to be beneficial during the development of the fliC probe. Although each fliC primer differed from the B. vandii sequence by one nucleotide, amplification was observed in this species. The added sensitivity of the internal probe made it possible to exclude B. vandii while maintaining positive detection of the isolates in the B. pseudomallei, B. mallei, B. thailandensis, and possibly B. oklahomensis group. The multiplex assay results agreed with those of previously published tests, and also produced faster results than current multiplex PCR methods because of its single-tube format design for detecting and differentiating several members of the B. pseudomallei complex.
The multiplex assay is both 100% sensitive and specific using purified DNA from the isolates examined in this study; although it is always possible that other isolates exist, or may emerge, with differing sequences that would not be detected. The multiplex assay is rapid, demonstrates sensitivity and specificity beyond culture and GC-FAME methods, and is robust due to its ability to still detect and differentiate, by creating a unique amplification profile, if a species-specific component of the multiplex assay fails. This test is also the only PCR assay currently available that is capable of specifically detecting and differentiating B. pseudomallei, B. mallei, and B. thailandensis in a single-tube format. For these reasons, this assay could prove useful as a rapid, sensitive, and economical tool in the detection and or differentiation for several species within the B. pseudomallei complex. If the newly discovered B. oklahomensis, B. humptydooensis, and Burkholderia clades A, B, and C prove to be clinically important, the multiplex assay described here could likely be adapted to include additional targets for these new species of the B. pseudomallei complex.
Supporting Information
The fliC probe was developed based on sequence information of the B. pseudomallei complex and B. vandii with their corresponding accession numbers.
(PDF)
NCBI BLASTn results for some B. pseudomallei strains indicate the orf11 assay contained four different mismatches that were found in the forward primer (A-B), reverse primer (C) and/or the probe (D). Integrated DNA Technologies' DNA Thermodynamics & Hybridization software was used to analyze the oligo sequence with the corresponding sequence shown with the mismatch being indicated by letters in red. Tm, Gibbs Energy, Enthalpy, and Entropy for each match or mismatch is shown with the salt concentrations used in the orf11 assay as indicated. The hybridization profiles are also shown for the exact match (blue) and mismatch (red). Refer to S4 Table for a summary of the mismatch profiles of the orf11 assay against B. pseudomallei isolates from NCBI GenBank.
(PDF)
NCBI BLASTn results indicate the fliC assay contained three different mismatches that were found in the probe for some B. pseudomallei (A-B) and for some B. thailandensis and B. oklahomensis strains (C-D). The third mismatch was also found in the forward primer for B. oklahomensis strains (E-F). Integrated DNA Technologies' DNA Thermodynamics & Hybridization software was used to analyze the probe or primer sequence with the corresponding sequence shown with the mismatch being indicated by letters in red. Tm, Gibbs Energy, Enthalpy, and Entropy for each match or mismatch is shown with the salt concentrations used in the fliC assay as indicated. The hybridization profiles are also shown for the exact match (blue) and mismatch (red). The software is unable to calculate degenerate bases. Therefore, both bases were calculated to ensure accuracy of a degenerate base with (A and C) containing the guanine base at position 21 of the probe, (B and D) adenine base at position 21 of the probe, (E) cytosine at position 12 of the forward primer, and (F) thymine at position 12 of the forward primer. Refer to S5 Table for a summary of the mismatch profiles of the fliC assay against B. pseudomallei complex isolates from NCBI GenBank.
(PDF)
(PDF)
(PDF)
The multiplex assay was evaluated against all completed sequences of B. mallei, B. pseudomallei, B. thailandensis, B. oklahomensis, B. humptydooensis strains along with a few other Burkholderia near-neighbors from the NCBI GenBank database.
(PDF)
Fraction of duplex values were calculated using DNA Thermodynamic & Hybridization software from Integrated DNA Technologies to determine the binding efficiency of an oligo when single nucleotide polymorphisms are present. A FoD value closer to 1 indicates a higher likelihood of proper binding.
(PDF)
Fraction of duplex values were calculated using DNA Thermodynamics & Hybridization software from Integrated DNA Technologies to determine the binding efficiency of an oligo when single nucleotide polymorphisms are present. A FoD value closer to 1 indicates a higher likelihood of proper binding. The software is unable to calculate degenerate bases; therefore, both bases were calculated and the average FoD is presented in this table.
(PDF)
Acknowledgments
We would like to thank Ty Pitt from PHE/PHLS for providing Burkholderia isolates, Bart Currie from RDH for providing B. pseudomallei strains, David DeShazer from USAMRIID for providing B. mallei strains, Rich Meyer from CDC for providing B. mallei strains, and Paul Jackson's Lab from Los Alamos National Laboratories for providing DNA for some Burkholderia near-neighbors used in this study. We would like to thank Joel Griffitts from BYU for providing universal 16S rDNA oligos. We would like to thank Derek Houston from BYU for providing insight on phylogenetic analysis. Lastly, we would like to thank Patrick Lowe for his help in editing the manuscript.
Data Availability
Data are available from GenBank accession number KM242678.
Funding Statement
This study was supported by the Office of Research & Creative Activities - Mentoring Environment Grants 547, https://orca.byu.edu/meg/.
References
- 1.Whitlock GC, Estes DM, Torres AG. Glanders: off to the races with Burkholderia mallei. FEMS Microbiol Lett. 2007;277(2):115–22. 10.1111/j.1574-6968.2007.00949.x. WOS:000251190400001. [DOI] [PubMed] [Google Scholar]
- 2.Spickler AR. Glanders In: Dvorak G, Spickler AR, Roth JA, editors. Handbook For Zoonotic Diseases of Companion Animals. 1 ed Ames: Center for Food Security and Public Health; 2008. p. 133–5. [Google Scholar]
- 3.Gregory BC, Waag DM. Glanders In: Dembek ZF, Huebner KD, Ibrahim MS, Poli MA, Whitehouse, editors. Medical Aspects of Biological Warfare. Washington, DC: Office of The Surgeon General and US Army Medical Department Center and School; 2007. p. 121–46. [Google Scholar]
- 4.Chaowagul W, White NJ, Dance DA, Wattanagoon Y, Naigowit P, Davis TM, et al. Melioidosis: a major cause of community-acquired septicemia in northeastern Thailand. J Infect Dis. 1989;159(5):890–9. Epub 1989/05/01. . [DOI] [PubMed] [Google Scholar]
- 5.Currie BJ, Fisher DA, Howard DM, Burrow JN, Lo D, Selva-Nayagam S, et al. Endemic melioidosis in tropical northern Australia: a 10-year prospective study and review of the literature. Clin Infect Dis. 2000;31(4):981–6. Epub 2000/10/26. 10.1086/318116 . [DOI] [PubMed] [Google Scholar]
- 6.Suputtamongkol Y, Chaowagul W, Chetchotisakd P, Lertpatanasuwun N, Intaranongpai S, Ruchutrakool T, et al. Risk factors for melioidosis and bacteremic melioidosis. Clin Infect Dis. 1999;29(2):408–13. Epub 1999/09/07. 10.1086/520223 . [DOI] [PubMed] [Google Scholar]
- 7.White NJ. Melioidosis. Lancet. 2003;361(9370):1715–22. 10.1016/s0140-6736(03)13374-0. WOS:000182919700024. [DOI] [PubMed] [Google Scholar]
- 8.Limmathurotsakul D, Wongratanacheewin S, Teerawattanasook N, Wongsuvan G, Chaisuksant S, Chetchotisakd P, et al. Increasing incidence of human melioidosis in Northeast Thailand. Am J Trop Med Hyg. 2010;82(6):1113–7. Epub 2010/06/04. 10.4269/ajtmh.2010.10-0038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng AC, Currie BJ. Melioidosis: Epidemiology, Pathophysiology, and Management. Clin Microbiol Rev. 2005;18(2):383–416. 10.1128/cmr.18.2.383-416.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brilhante RS, Bandeira TJ, Cordeiro RA, Grangeiro TB, Lima RA, Ribeiro JF, et al. Clinical-epidemiological features of 13 cases of melioidosis in Brazil. J Clin Microbiol. 2012;50(10):3349–52. Epub 2012/07/21. 10.1128/jcm.01577-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen YS, Lin HH, Mu JJ, Chiang CS, Chen CH, Buu LM, et al. Distribution of melioidosis cases and viable Burkholderia pseudomallei in soil: evidence for emerging melioidosis in Taiwan. J Clin Microbiol. 2010;48(4):1432–4. Epub 2010/02/12. 10.1128/jcm.01720-09. WOS:000276153200062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Currie BJ, Dance DA, Cheng AC. The global distribution of Burkholderia pseudomallei and melioidosis: an update. Trans R Soc Trop Med Hyg. 2008;102 Suppl 1:S1–4. Epub 2009/01/16. 10.1016/s0035-9203(08)70002-6 . [DOI] [PubMed] [Google Scholar]
- 13.John TJ, Jesudason MV, Lalitha MK, Ganesh A, Mohandas V, Cherian T, et al. Melioidosis In India: the tip of the iceberg? Indian J Med Res. 1996;103:62–5. Epub 1996/01/01. . [PubMed] [Google Scholar]
- 14.Brett PJ, DeShazer D, Woods DE. Burkholderia thailandensis sp. nov., a Burkholderia pseudomallei-like species. Int J Syst Bacteriol. 1998;48:317–20. WOS:000072711200035. 10.1099/00207713-48-1-317 [DOI] [PubMed] [Google Scholar]
- 15.Price EP, MacHunter B, Spratt BG, Wagner DM, Currie BJ, Sarovich DS. Improved multilocus sequence typing of Burkholderia pseudomallei and closely related species. Journal of medical microbiology. 2016. Epub 2016/07/15. 10.1099/jmm.0.000312 . [DOI] [PubMed] [Google Scholar]
- 16.Gee JE, Glass MB, Novak RT, Gal D, Mayo MJ, Steigerwalt AG, et al. Recovery of a Burkholderia thailandensis-like isolate from an Australian water source. BMC microbiology. 2008;8:54 Epub 2008/04/04. 10.1186/1471-2180-8-54 ; PubMed Central PMCID: PMCPmc2329625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glass MB, Steigerwalt AG, Jordan JG, Wilkins PP, Gee JE. Burkholderia oklahomensis sp. nov., a Burkholderia pseudomallei-like species formerly known as the Oklahoma strain of Pseudomonas pseudomallei. International journal of systematic and evolutionary microbiology. 2006;56(Pt 9):2171–6. Epub 2006/09/08. 10.1099/ijs.0.63991-0 . [DOI] [PubMed] [Google Scholar]
- 18.Ginther JL, Mayo M, Warrington SD, Kaestli M, Mullins T, Wagner DM, et al. Identification of Burkholderia pseudomallei Near-Neighbor Species in the Northern Territory of Australia. PLoS neglected tropical diseases. 2015;9(6):e0003892 Epub 2015/06/30. 10.1371/journal.pntd.0003892 ; PubMed Central PMCID: PMCPmc4486726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeShazer D. Virulence of clinical and environmental isolates of Burkholderia oklahomensis and Burkholderia thailandensis in hamsters and mice. Fems Microbiology Letters. 2007;277(1):64–9. 10.1111/j.1574-6968.2007.00946.x. WOS:000250619200009. [DOI] [PubMed] [Google Scholar]
- 20.Dharakul T, Tassaneetrithep B, Trakulsomboon S, Songsivilai S. Phylogenetic analysis of Ara+ and Ara- Burkholderia pseudomallei isolates and development of a multiplex PCR procedure for rapid discrimination between the two biotypes. J Clin Microbiol. 1999;37(6):1906–12. Epub 1999/05/15. WOS:000080344900042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glass MB, Gee JE, Steigerwalt AG, Cavuoti D, Barton T, Hardy RD, et al. Pneumonia and septicemia caused by Burkholderia thailandensis in the United States. J Clin Microbiol. 2006;44(12):4601–4. 10.1128/jcm.01585-06. WOS:000242876300055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lertpatanasuwan N, Sermsri K, Petkaseam A, Trakulsomboon S, Thamlikitkul V, Suputtamongkol Y. Arabinose-positive Burkholderia pseudomallei infection in humans: Case report. Clin Infect Dis. 1999;28(4):927–8. WOS:000079611600055. [DOI] [PubMed] [Google Scholar]
- 23.McCormick JB, Weaver RE, Hayes PS, Boyce JM, Feldman RA. Wound infection by an indigenous Pseudomonas pseudomallei-like organism isolated from the soil: case report and epidemiologic study. The Journal of infectious diseases. 1977;135(1):103–7. Epub 1977/01/01. . [DOI] [PubMed] [Google Scholar]
- 24.Nussbaum JJ, Hull DS, Carter MJ. Pseudomonas pseudomallei in an anopthalmic orbit. Archives of ophthalmology (Chicago, Ill: 1960). 1980;98(7):1224–5. Epub 1980/07/01. . [DOI] [PubMed] [Google Scholar]
- 25.Thibault FM, Valade E, Vidal DR. Identification and discrimination of Burkholderia pseudomallei, B. mallei, and B. thailandensis by real-time PCR targeting type III secretion system genes. J Clin Microbiol. 2004;42(12):5871–4. Epub 2004/12/08. 10.1128/jcm.42.12.5871-5874.2004. WOS:000226035800067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dance DA, White NJ. Melioidosis In: Cox FEG, editor. The Wellcome Trust Illustrated History of Tropical Diseases. London: The Wellcome Trust; 1996. p. 72–81. [Google Scholar]
- 27.Alibek K, Handelman S. Biohazard: the chilling true story of the largest covert biological weapons program in the world—told from inside by the man who ran it. New York, NY: Random House; 1999. [Google Scholar]
- 28.Christopher GW, Cieslak TJ, Pavlin JA, Eitzen EM Jr., Biological warfare. A historical perspective. JAMA. 1997;278(5):412–7. Epub 1997/08/06. . [PubMed] [Google Scholar]
- 29.Lehavi O, Aizenstien O, Katz L, Hourvitz A. Glanders—a potential disease for biological warfare in humans and animals. Harefuah. 2002;141:88–91. [PubMed] [Google Scholar]
- 30.Rubin HL, Alexander AD, Yager RH. Melioidosis—a military medical problem? Mil Med. 1963;128:538–42. Epub 1963/06/01. . [PubMed] [Google Scholar]
- 31.Godoy D, Randle G, Simpson AJ, Aanensen DM, Pitt TL, Kinoshita R, et al. Multilocus sequence typing and evolutionary relationships among the causative agents of melioidosis and glanders, Burkholderia pseudomallei and Burkholderia mallei. Journal of clinical microbiology. 2003;41(5):2068–79. 10.1128/jcm.41.5.2068-2079.2003. WOS:000182934500041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nierman WC, DeShazer D, Kim HS, Tettelin H, Nelson KE, Feldblyum T, et al. Structural flexibility in the Burkholderia mallei genome. Proc Natl Acad Sci U S A. 2004;101(39):14246–51. Epub 2004/09/21. 10.1073/pnas.0403306101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cheng AC. Melioidosis: advances in diagnosis and treatment. Current opinion in infectious diseases. 2010;23(6):554–9. Epub 2010/09/18. 10.1097/QCO.0b013e32833fb88c . [DOI] [PubMed] [Google Scholar]
- 34.Gilad J. Burkholderia mallei and Burkholderia pseudomallei: the causative micro-organisms of glanders and melioidosis. Recent patents on anti-infective drug discovery. 2007;2(3):233–41. Epub 2008/01/29. . [DOI] [PubMed] [Google Scholar]
- 35.Galyov EE, Brett PJ, DeShazer D. Molecular Insights into Burkholderia pseudomallei and Burkholderia mallei Pathogenesis. In: Gottesman S, Harwood CS, editors. Annual Review of Microbiology, Vol 64, 2010. Annual Review of Microbiology. 642010. p. 495–517. [DOI] [PubMed] [Google Scholar]
- 36.Frickmann H, C N, Gauthier YP, Neubauer H, Hagen RM. Discrimination of Burkholderia mallei/pseudomallei from Burkholderia thailandensis by Sequence Comparison of a Fragment of the Ribosomal Protein S21 (RPSU) Gene. Eur J Microbiol Immunol. 2012;2(2):148–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Depoorter E, Bull MJ, Peeters C, Coenye T, Vandamme P, Mahenthiralingam E. Burkholderia: an update on taxonomy and biotechnological potential as antibiotic producers. Applied microbiology and biotechnology. 2016;100(12):5215–29. Epub 2016/04/27. 10.1007/s00253-016-7520-x . [DOI] [PubMed] [Google Scholar]
- 38.Cheng AC, O'Brien M, Freeman K, Lum G, Currie BJ. Indirect hemagglutination assay in patients with melioidosis in northern Australia. Am J Trop Med Hyg. 2006;74(2):330–4. Epub 2006/02/14. . [PubMed] [Google Scholar]
- 39.Chenthamarakshan V, Vadivelu J, Puthucheary SD. Detection of immunoglobulins M and G using culture filtrate antigen of Burkholderia pseudomallei. Diagn Microbiol Infect Dis. 2001;39(1):1–7. Epub 2001/02/15. . [DOI] [PubMed] [Google Scholar]
- 40.Anuntagool N, Naigowit P, Petkanchanapong V, Aramsri P, Panichakul T, Sirisinha S. Monoclonal antibody-based rapid identification of Burkholderia pseudomallei in blood culture fluid from patients with community-acquired septicaemia. J Med Microbiol. 2000;49(12):1075–8. Epub 2000/12/29. 10.1099/0022-1317-49-12-1075 [DOI] [PubMed] [Google Scholar]
- 41.Steinmetz I, Reganzerowski A, Brenneke B, Haussler S, Simpson A, White NJ. Rapid identification of Burkholderia pseudomallei by latex agglutination based on an exopolysaccharide-specific monoclonal antibody. J Clin Microbiol. 1999;37(1):225–8. Epub 1998/12/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Samosornsuk N, Lulitanond A, Saenla N, Anuntagool N, Wongratanacheewin S, Sirisinha S. Short report: evaluation of a monoclonal antibody-based latex agglutination test for rapid diagnosis of septicemic melioidosis. Am J Trop Med Hyg. 1999;61(5):735–7. Epub 1999/12/10. . [DOI] [PubMed] [Google Scholar]
- 43.Lowe P, Engler C, Norton R. Comparison of automated and nonautomated systems for identification of Burkholderia pseudomallei. J Clin Microbiol. 2002;40(12):4625–7. Epub 2002/11/28. 10.1128/JCM.40.12.4625-4627.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Inglis TJ, Chiang D, Lee GS, Chor-Kiang L. Potential misidentification of Burkholderia pseudomallei by API 20NE. Pathology. 1998;30(1):62–4. Epub 1998/04/16. . [DOI] [PubMed] [Google Scholar]
- 45.Amornchai P, Chierakul W, Wuthiekanun V, Mahakhunkijcharoen Y, Phetsouvanh R, Currie BJ, et al. Accuracy of Burkholderia pseudomallei identification using the API 20NE system and a latex agglutination test. J Clin Microbiol. 2007;45(11):3774–6. 10.1128/jcm.00935-07. WOS:000250932700046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Glass MB, Popovic T. Preliminary Evaluation of the API 20NE and RapID NF Plus Systems for Rapid Identification of Burkholderia pseudomallei and B. mallei. J Clin Microbiol. 2005;43(1):479–83. 10.1128/jcm.43.1.479-483.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Inglis TJJ, Aravena-Roman M, Ching S, Croft K, Wuthiekamm V, Mee BJ. Cellular fatty acid profile distinguishes Burkholderia pseudomallei from avirulent Burkholderia thailandensis. J Clin Microbiol. 2003;41(10):4812–4. 10.1128/jcm.41.10.4812-4814.2003. WOS:000185922900056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Inglis TJJ, Merritt A, Chidlow G, Aravena-Roman M, Harnett G. Comparison of diagnostic laboratory methods for identification of Burkholderia pseudomallei. J Clin Microbiol. 2005;43(5):2201–6. Epub 2005/05/06. 10.1128/jcm.43.5.2201-2206.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wuthiekanun V, Desakorn V, Wongsuvan G, Amornchai P, Cheng AC, Maharjan B, et al. Rapid immunofluorescence microscopy for diagnosis of meliodosis. Clin Diagn Lab Immunol. 2005;12(4):555–6. 10.1128/cdli.12.4.555-556.2005. WOS:000231196900015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Walsh AL, Smith MD, Wuthiekanun V, Suputtamongkol Y, Desakorn V, Chaowagul W, et al. Immunofluorescence microscopy for the rapid diagnosis of melioidosis. J Clin Pathol. 1994;47(4):377–9. 10.1136/jcp.47.4.377. WOS:A1994NH06400023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hagen RM, Frickmann H, Elschner M, Melzer F, Neubauer H, Gauthier YP, et al. Rapid identification of Burkholderia pseudomallei and Burkholderia mallei by fluorescence in situ hybridization (FISH) from culture and paraffin-embedded tissue samples. Int J Med Microbiol. 2011;301(7):585–90. Epub 2011/06/11. 10.1016/j.ijmm.2011.04.017 . [DOI] [PubMed] [Google Scholar]
- 52.Inglis TJ, Healy PE, Fremlin LJ, Golledge CL. Use of matrix-assisted laser desorption/ionization time-of-flight mass spectrometry analysis for rapid confirmation of Burkholderia pseudomallei in septicemic melioidosis. Am J Trop Med Hyg. 2012;86(6):1039–42. Epub 2012/06/06. 10.4269/ajtmh.2012.11-0454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Puthucheary SD, Puah SM, Chai HC, Thong KL, Chua KH. Molecular investigation of virulence determinants between a virulent clinical strain and an attenuated strain of Burkholderia pseudomallei. J Mol Microbiol Biotechnol. 2012;22(3):198–204. Epub 2012/08/01. 10.1159/000338985 . [DOI] [PubMed] [Google Scholar]
- 54.Tanpiboonsak S, Paemanee A, Bunyarataphan S, Tungpradabkul S. PCR-RFLP based differentiation of Burkholderia mallei and Burkholderia pseudomallei. Mol Cell Probes. 2004;18(2):97–101. Epub 2004/03/31. 10.1016/j.mcp.2003.09.010 . [DOI] [PubMed] [Google Scholar]
- 55.Gee JE, Sacchi CT, Glass MB, De BK, Weyant RS, Levett PN, et al. Use of 16S rRNA gene sequencing for rapid identification and differentiation of Burkholderia pseudomallei and B. mallei. J Clin Microbiol. 2003;41(10):4647–54. 10.1128/jcm.41.10.4647-4654.2003. WOS:000185922900025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Woo PCY, Woo GKS, Lau SKP, Wong SSY, Yuen KY. Single gene target bacterial identification: groEL gene sequencing for discriminating clinical isolates of Burkholderia pseudomallei and Burkholderia thailandensis. Diagn Microbiol Infect Dis. 2002;44(2):143–9. 10.1016/s0732-8893(02)00439-x. WOS:000179625300004. [DOI] [PubMed] [Google Scholar]
- 57.Wuthiekanun V, Amornchai P, Chierakul W, Cheng AC, White NJ, Peacock SJ, et al. Evaluation of immunoglobulin M (IgM) and IgG rapid cassette test kits for diagnosis of melioidosis in an area of endemicity. J Clin Microbiol. 2004;42(8):3435–7. 10.1128/jcm.42.8.3435-3437.2004. WOS:000223286500008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Currie BJ. Burkholderia pseudomallei and Burkholderia mallei: melioidosis and glanders Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases 7th edn Philadelphia: Churchill Livingstone Elsevier; 2010:2869–85. [Google Scholar]
- 59.Lowe W, March JK, Bunnell AJ, O'Neill KL, Robison RA. PCR-based Methodologies Used to Detect and Differentiate the Burkholderia pseudomallei complex: B. pseudomallei, B. mallei, and B. thailandensis. Curr Issues Mol Biol. 2013;16(2):23–54. Epub 2013/08/24. . [PubMed] [Google Scholar]
- 60.Novak RT, Glass MB, Gee JE, Gal D, Mayo MJ, Currie BJ, et al. Development and evaluation of a real-time PCR assay targeting the type III secretion system of Burkholderia pseudomallei. J Clin Microbiol. 2006;44(1):85–90. Epub 2006/01/05. 10.1128/jcm.44.1.85-90.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ulrich RL, Ulrich MP, Schell MA, Kim HS, DeShazer D. Development of a polymerase chain reaction assay for the specific identification of Burkholderia mallei and differentiation from Burkholderia pseudomallei and other closely related Burkholderiaceae. Diagn Microbiol Infect Dis. 2006;55(1):37–45. Epub 2006/03/21. 10.1016/j.diagmicrobio.2005.11.007. WOS:000237910800006. [DOI] [PubMed] [Google Scholar]
- 62.Winstanley C, Hart CA. Presence of type III secretion genes in Burkholderia pseudomallei correlates with Ara(-) phenotypes. J Clin Microbiol. 2000;38(2):883–5. Epub 2000/02/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Neubauer H, Sprague LD, Joseph M, Tomaso H, Al Dahouk S, Witte A, et al. Development and clinical evaluation of a PCR assay targeting the metalloprotease gene (mprA) of B. pseudomallei. Zoonoses Public Health. 2007;54(1):44–50. Epub 2007/03/16. 10.1111/j.1863-2378.2007.01008.x . [DOI] [PubMed] [Google Scholar]
- 64.Supaprom C, Wang D, Leelayuwat C, Thaewpia W, Susaengrat W, Koh V, et al. Development of real-time PCR assays and evaluation of their potential use for rapid detection of Burkholderia pseudomallei in clinical blood specimens. J Clin Microbiol. 2007;45(9):2894–901. Epub 2007/07/20. 10.1128/jcm.00291-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tomaso H, Scholz HC, Al Dahouk S, Eickhoff M, Treu TM, Wernery R, et al. Development of a 5'-nuclease real-time PCR assay targeting fliP for the rapid identification of Burkholderia mallei in clinical samples. Clin Chem. 2006;52(2):307–10. Epub 2006/02/02. 10.1373/clinchem.2005.059196 . [DOI] [PubMed] [Google Scholar]
- 66.Meumann EM, Cheng AC, Ward L, Currie BJ. Clinical features and epidemiology of melioidosis pneumonia: results from a 21-year study and review of the literature. Clin Infect Dis. 2012;54(3):362–9. Epub 2011/11/08. 10.1093/cid/cir808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kaestli M, Mayo M, Harrington G, Watt F, Hill J, Gal D, et al. Sensitive and specific molecular detection of Burkholderia pseudomallei, the causative agent of melioidosis, in the soil of tropical northern Australia. Appl Environ Microbiol. 2007;73(21):6891–7. Epub 2007/09/18. 10.1128/aem.01038-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chantratita N, Meumann E, Thanwisai A, Limmathurotsakul D, Wuthiekanun V, Wannapasni S, et al. Loop-mediated isothermal amplification method targeting the TTS1 gene cluster for detection of Burkholderia pseudomallei and diagnosis of melioidosis. J Clin Microbiol. 2008;46(2):568–73. Epub 2007/11/28. 10.1128/jcm.01817-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Trung TT, Hetzer A, Gohler A, Topfstedt E, Wuthiekanun V, Limmathurotsakul D, et al. Highly sensitive direct detection and quantification of Burkholderia pseudomallei bacteria in environmental soil samples by using real-time PCR. Appl Environ Microbiol. 2011;77(18):6486–94. Epub 2011/08/02. 10.1128/aem.00735-11. WOS:000294691400021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kaestli M, Richardson LJ, Colman RE, Tuanyok A, Price EP, Bowers JR, et al. Comparison of TaqMan PCR assays for detection of the melioidosis agent Burkholderia pseudomallei in clinical specimens. J Clin Microbiol. 2012;50(6):2059–62. Epub 2012/03/24. 10.1128/jcm.06737-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Koh SF, Tay ST, Sermswan R, Wongratanacheewin S, Chua KH, Puthucheary SD. Development of a multiplex PCR assay for rapid identification of Burkholderia pseudomallei, Burkholderia thailandensis, Burkholderia mallei and Burkholderia cepacia complex. J Microbiol Methods. 2012;90(3):305–8. Epub 2012/06/19. 10.1016/j.mimet.2012.06.002 . [DOI] [PubMed] [Google Scholar]
- 72.Lee MA, Wang DL, Yap EH. Detection and differentiation of Burkholderia pseudomallei, Burkholderia mallei and Burkholderia thailandensis by multiplex PCR. FEMS Immunol Med Microbiol. 2005;43(3):413–7. Epub 2005/02/15. 10.1016/j.femsim.2004.10.008. WOS:000227532100013. [DOI] [PubMed] [Google Scholar]
- 73.Scholz HC, Joseph M, Tomaso H, Al Dahouk S, Witte A, Kinne J, et al. Detection of the reemerging agent Burkholderia mallei in a recent outbreak of glanders in the United Arab Emirates by a newly developed fliP-based polymerase chain reaction assay. Diagn Microbiol Infect Dis. 2006;54(4):241–7. Epub 2006/02/10. 10.1016/j.diagmicrobio.2005.09.018. WOS:000236975800001. [DOI] [PubMed] [Google Scholar]
- 74.U'Ren JM, Van Ert MN, Schupp JM, Easterday WR, Simonson TS, Okinaka RT, et al. Use of a real-time PCR TaqMan assay for rapid identification and differentiation of Burkholderia pseudomallei and Burkholderia mallei. J Clin Microbiol. 2005;43(11):5771–4. Epub 2005/11/08. 10.1128/jcm.43.11.5771-5774.2005. WOS:000233312200054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bowers JR, Engelthaler DM, Ginther JL, Pearson T, Peacock SJ, Tuanyok A, et al. BurkDiff: a real-time PCR allelic discrimination assay for Burkholderia pseudomallei and B. mallei. Plos One. 2010;5(11). Epub 2010/11/26. e15413 10.1371/journal.pone.0015413. WOS:000284147700024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Price EP, Dale JL, Cook JM, Sarovich DS, Seymour ML, Ginther JL, et al. Development and validation of Burkholderia pseudomallei-specific real-time PCR assays for clinical, cnvironmental or forensic detection applications. Plos One. 2012;7(5):e37723 Epub 2012/05/25. 10.1371/journal.pone.0037723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pal V, Kumar S, Malik P, Rai GP. Evaluation of recombinant proteins of Burkholderia mallei for serodiagnosis of glanders. Clin Vaccine Immunol. 2012;19(8):1193–8. Epub 2012/06/15. 10.1128/cvi.00137-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rainbow L, Hart CA, Winstanley C. Distribution of type III secretion gene clusters in Burkholderia pseudomallei, B. thailandensis and B. mallei. J Med Microbiol. 2002;51(5):374–84. Epub 2002/05/07. WOS:000175190300002. 10.1099/0022-1317-51-5-374 [DOI] [PubMed] [Google Scholar]
- 79.Ho CC, Lau CCY, Martelli P, Chan SY, Tse CWS, Wu AKL, et al. Novel pan-genomic analysis approach in target selection for multiplex PCR identification and detection of Burkholderia pseudomallei, Burkholderia thailandensis, and Burkholderia cepacia complex species: a proof-of-concept study. J Clin Microbiol. 2011;49(3):814–21. Epub 2010/12/24. 10.1128/jcm.01702-10. WOS:000287967100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sprague LD, Zysk G, Hagen RM, Meyer H, Ellis J, Anuntagool N, et al. A possible pitfall in the identification of Burkholderia mallei using molecular identification systems based on the sequence of the flagellin fliC gene. FEMS Immunol Med Microbiol. 2002;34(3):231–6. Epub 2002/11/09. 10.1111/j.1574-695X.2002.tb00629.x. WOS:000179282300010. [DOI] [PubMed] [Google Scholar]
- 81.Hagen RM, Gauthier YP, Sprague LD, Vidal DR, Zysk G, Finke EJ, et al. Strategies for PCR based detection of Burkholderia pseudomallei DNA in paraffin wax embedded tissues. Mol Pathol. 2002;55(6):398–400. Epub 2002/11/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: Molecular Evolutionary Genetics Analysis version 6.0. Mol Biol Evol. 2013;30(12):2725–9. Epub 2013/10/18. 10.1093/molbev/mst197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kwok S, Chang SY, Sninsky JJ, Wang A. A guide to the design and use of mismatched and degenerate primers. PCR methods and applications. 1994;3(4):S39–47. Epub 1994/02/01. . [DOI] [PubMed] [Google Scholar]
- 84.Ke X, Collins A, Ye S. PIRA PCR designer for restriction analysis of single nucleotide polymorphisms. Bioinformatics (Oxford, England). 2001;17(9):838–9. Epub 2001/10/09. . [DOI] [PubMed] [Google Scholar]
- 85.Kutyavin IV, Afonina IA, Mills A, Gorn VV, Lukhtanov EA, Belousov ES, et al. 3'-minor groove binder-DNA probes increase sequence specificity at PCR extension temperatures. Nucleic acids research. 2000;28(2):655–61. Epub 1999/12/22. ; PubMed Central PMCID: PMCPmc102528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Satterfield BA, Stewart AF, Lew CS, Pickett DO, Cohen MN, Moore EA, et al. A quadruplex real-time PCR assay for rapid detection and differentiation of the Clostridium botulinum toxin genes A, B, E and F. Journal of medical microbiology. 2010;59(Pt 1):55–64. Epub 2009/09/26. 10.1099/jmm.0.012567-0 . [DOI] [PubMed] [Google Scholar]
- 87.Innis MA, Gelfand DH. 1—OPTIMIZATION OF PCRs PCR Protocols. San Diego: Academic Press; 1990. p. 3–12. [Google Scholar]
- 88.Yang S, Rothman RE. PCR-based diagnostics for infectious diseases: uses, limitations, and future applications in acute-care settings. Lancet Infect Dis. 2004;4(6):337–48. Epub 2004/06/03. 10.1016/s1473-3099(04)01044-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fredricks DN, Relman DA. Application of polymerase chain reaction to the diagnosis of infectious diseases. Clin Infect Dis. 1999;29(3):475–86; quiz 87–8. Epub 1999/10/26. . [DOI] [PubMed] [Google Scholar]
- 90.Klein D. Quantification using real-time PCR technology: applications and limitations. Trends Mol Med. 2002;8(6):257–60. Epub 2002/06/18. . [DOI] [PubMed] [Google Scholar]
- 91.Chantratita N, Wuthiekanun V, Limmathurotsakul D, Thanwisai A, Chantratita W, Day NPJ, et al. Prospective clinical evaluation of the accuracy of 16S rRNA real-time PCR assay for the diagnosis of melioidosis. Am J Trop Med Hyg. 2007;77(5):814–7. Epub 2007/11/07. WOS:000250735000006. [PubMed] [Google Scholar]
- 92.Walsh AL, Smith MD, Wuthiekanun V, Suputtamongkol Y, Chaowagul W, Dance DA, et al. Prognostic significance of quantitative bacteremia in septicemic melioidosis. Clin Infect Dis. 1995;21(6):1498–500. Epub 1995/12/01. . [DOI] [PubMed] [Google Scholar]
- 93.Purcell MK, Getchell RG, McClure CA, Garver KA. Quantitative polymerase chain reaction (PCR) for detection of aquatic animal pathogens in a diagnostic laboratory setting. J Aquat Anim Health. 2011;23(3):148–61. Epub 2012/01/06. 10.1080/08997659.2011.620217 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The fliC probe was developed based on sequence information of the B. pseudomallei complex and B. vandii with their corresponding accession numbers.
(PDF)
NCBI BLASTn results for some B. pseudomallei strains indicate the orf11 assay contained four different mismatches that were found in the forward primer (A-B), reverse primer (C) and/or the probe (D). Integrated DNA Technologies' DNA Thermodynamics & Hybridization software was used to analyze the oligo sequence with the corresponding sequence shown with the mismatch being indicated by letters in red. Tm, Gibbs Energy, Enthalpy, and Entropy for each match or mismatch is shown with the salt concentrations used in the orf11 assay as indicated. The hybridization profiles are also shown for the exact match (blue) and mismatch (red). Refer to S4 Table for a summary of the mismatch profiles of the orf11 assay against B. pseudomallei isolates from NCBI GenBank.
(PDF)
NCBI BLASTn results indicate the fliC assay contained three different mismatches that were found in the probe for some B. pseudomallei (A-B) and for some B. thailandensis and B. oklahomensis strains (C-D). The third mismatch was also found in the forward primer for B. oklahomensis strains (E-F). Integrated DNA Technologies' DNA Thermodynamics & Hybridization software was used to analyze the probe or primer sequence with the corresponding sequence shown with the mismatch being indicated by letters in red. Tm, Gibbs Energy, Enthalpy, and Entropy for each match or mismatch is shown with the salt concentrations used in the fliC assay as indicated. The hybridization profiles are also shown for the exact match (blue) and mismatch (red). The software is unable to calculate degenerate bases. Therefore, both bases were calculated to ensure accuracy of a degenerate base with (A and C) containing the guanine base at position 21 of the probe, (B and D) adenine base at position 21 of the probe, (E) cytosine at position 12 of the forward primer, and (F) thymine at position 12 of the forward primer. Refer to S5 Table for a summary of the mismatch profiles of the fliC assay against B. pseudomallei complex isolates from NCBI GenBank.
(PDF)
(PDF)
(PDF)
The multiplex assay was evaluated against all completed sequences of B. mallei, B. pseudomallei, B. thailandensis, B. oklahomensis, B. humptydooensis strains along with a few other Burkholderia near-neighbors from the NCBI GenBank database.
(PDF)
Fraction of duplex values were calculated using DNA Thermodynamic & Hybridization software from Integrated DNA Technologies to determine the binding efficiency of an oligo when single nucleotide polymorphisms are present. A FoD value closer to 1 indicates a higher likelihood of proper binding.
(PDF)
Fraction of duplex values were calculated using DNA Thermodynamics & Hybridization software from Integrated DNA Technologies to determine the binding efficiency of an oligo when single nucleotide polymorphisms are present. A FoD value closer to 1 indicates a higher likelihood of proper binding. The software is unable to calculate degenerate bases; therefore, both bases were calculated and the average FoD is presented in this table.
(PDF)
Data Availability Statement
Data are available from GenBank accession number KM242678.