The risk of sepsis is low. The best probiotic to optimize outcomes has not yet been identified. Potential benefit for CD4 count, recurrence or management of bacterial vaginosis and diarrhea. Uncertain effect on translocation, BV treatment.
Keywords: bacteremia, fungemia, HIV infection, probiotics
Abstract
People living with human immunodeficiency virus frequently use dietary supplements, including probiotics, but concern exists about ingesting live organisms. We performed a systematic review of the benefits of probiotics and a meta-analysis of sepsis risk. We undertook a protocol-driven, comprehensive review to identify all relevant studies, assess their quality, and summarize the evidence. Of 2068 references, 27 were analyzed. The data suggest possible benefits for CD4 count, recurrence or management of bacterial vaginosis, and diarrhea management. We examined randomized, controlled studies explicitly assessing sepsis in any patient population, and we found zero cases of supplement-associated bacteremia or fungemia in 39 randomized controlled trials comprising 9402 subjects. The estimated number needed to harm is 7369 in Bayesian approach (95% credible interval: 1689, ∞), which should reassure clinicians. No or mild adverse effects were reported. Longer duration studies investigating different individual and mixed strains for plausible indications are needed to establish best practices.
Individuals living with human immunodeficiency virus (HIV) frequently use dietary supplements [1]. The use of probiotics may be inexpensive and potentially clinically important interventions to reduce HIV-related morbidity and mortality [2].
Human immunodeficiency virus infects CD4+ T lymphocytes and monocyte-derived-macrophages colonizing the gut-associated lymphoid tissue [3]. Significant disruption to gut architecture can occur, with a concomitant release of lipopolysaccharide (LPS) into peripheral blood, correlating with systemic immune activation, a hallmark of HIV disease progression [4]. Probiotics may reduce immune activation and bacterial translocation [5] and possibly reduce acquisition or transmission of infections [6].
This paper expands and updates previous reviews. Level B evidence was found for treating diarrhea; it was not possible to make a recommendation regarding use of probiotics in HIV-infected patients [7]. A meta-analysis in children found evidence for decreased duration of diarrhea and fever but limited data for HIV+ children [8]. Evidence is fairly robust for the use of probiotics for primary prevention, with weaker evidence as secondary prophylaxis for Clostridium difficile infections [9]. Probiotics may modulate immune function, offset the sequelae of malnutrition, mitigate enteric infections and eventually serve as microbicides or vehicles for mucosal delivery of vaccines [10, 11]. Probiotics may have clinical benefits; however, access remains a limiting factor in some settings [12–14]. Our review adds an HIV-specific focus to a systematic review previously conducted of conditions pathologically similar to HIV [15].
Several case reports document probiotic organisms causing sepsis [16], but no studies provide numerical estimates of risk. Therefore, we assessed data from randomized controlled trials (RCTs) in people with and without HIV where probiotics were administered, and risk of sepsis arising from bacteremia or fungemia was explicitly assessed. We derived a risk estimate and number needed to harm (NNH) using Bayesian analytical methods.
METHODS
We conducted a systematic review, querying multiple databases, providing a comprehensive overview of the use of probiotics, prebiotics, or synbiotics in HIV disease and a data synthesis of sepsis risk of probiotics. Our protocol was registered with PROSPERO [17].
SEARCH METHODS
Eligibility Criteria
We included clinical trials of individuals of any age with documented HIV disease with or without concurrent or active infection, whether or not they were on antiretroviral (ARV) therapy. We defined probiotic supplements as commensal bacterial or fungal supplements, in any form, including capsule, tablet, powder, softgel, or fortified food forms. Prebiotics were defined as nondigestible food ingredients that modify intestinal microbiota by enhancing the growth of commensal bacteria [18]. Studies of synbiotics combining prebiotics and probiotics were included.
Information Sources
We searched MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials (The Cochrane Library), Cochrane Reviews, Cochrane Trials, AEGIS, AMED, CINAHL, Google Scholar, and the World Health Organization. Searches were conducted from database inception through March 2016.
Study Selection
Reviewer pairs independently screened citations and abstracts of all publications obtained by the search strategies (Figure 1). Disagreements were resolved by consensus.
Figure 1.
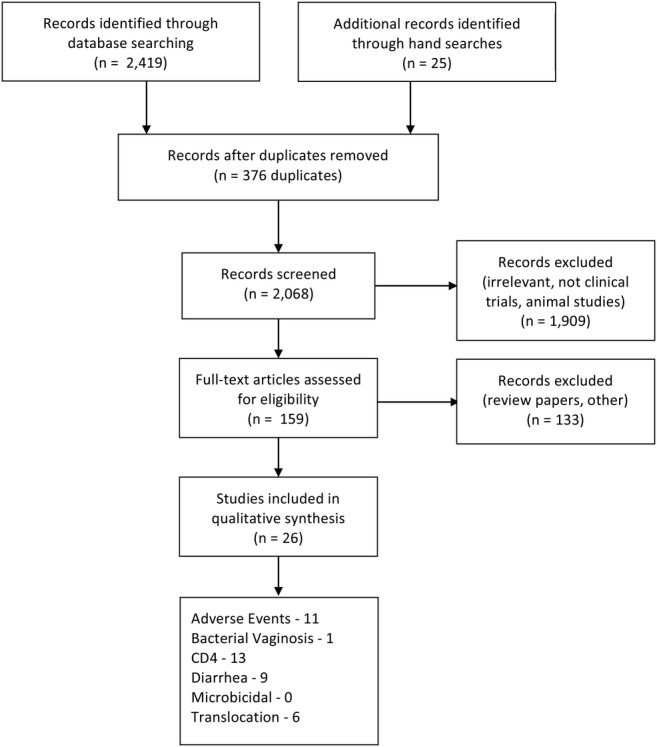
Flow chart of selection process of reviewed studies. Studies included add up to more than 26 due to multiple outcomes in some studies.
Data Collection Process
For eligible trials, we obtained full articles and assessed their relevance based on the preplanned criteria for inclusion in the systematic review.
Data Items
We extracted data on study design, intervention, trial design, site, number of participants, inclusion and exclusion criteria, duration, toxicity/adverse events, primary endpoint, secondary endpoint, findings, baseline differences, conclusions, efficacy, and safety (Table 1).
Table 1.
Probiotics and Prebiotics in HIV: PICOS Study Description
| Reference | Population/ARV | Duration | Intervention/Duration | Comparator | Outcomes (Endpoint) 1o, 2o |
|---|---|---|---|---|---|
| Anukam et al [28] | Adult HIV+ women, n = 24 Not on ARV |
Over 15 d | Yogurt fermented with specific strains; n = 12 | Yogurt with standard strains n = 12 |
CD4, hematologic parameters, diarrhea duration |
| Cunningham-Rundles et al [31] | n = 17 Pediatric HIV |
Lactobacillus plantarum 299v - 1st child received in a juice; further children received packets | Placebo packet n = unclear | Nutrient status and growth; colonization of gut and immunological effects | |
| Gautam et al [23] | n = 146 HIV+ ≤15 years old Randomized by ARV use |
3 mo |
Lactobacillus sporogens
n = 35 on ARV n = 30 not, MN only n = 25 not, probiotic |
Supplement without probiotics n = 31 on ARV; n = 25 not |
CD4 |
| Gonzalez-Hernandez et al [3] | RCT; n = 20 5 in each arm, probiotic, prebiotic, symbiotic, placebo ARV naive, HIV+ |
Over 16 wk | Prebiotic: 10 grams of agavins from Agave tequilana Weber var. azul (FOS with mainly β(2–1) linkages, and some β(2–6) linkages); Probiotic: Lactobacillus rhamnosus HN001, Bifidobacterium lactis Bi-07 at 109 cfu/mL, or Synbiotic combination |
Placebo was a product of Biogel without probiotics or prebiotic n = 5 |
1- Safety, QoL 2- Absolute CD4+ count, cytokine level 3- Viremia, bacterial DNA in plasma and stool, qPCR for bacterial 16S rRNA in plasma and feces, qPCR for Bifidobacterium and Clostridium spp in feces) |
| Gori et al [18] | n = 57 HIV+ ARV naive Each arm, n = 19 |
12 wk; follow-up at 16 wk off tx | Prebiotics: 15 (n = 19) or 30 g (n = 19) short-chain galactooligosaccharides, long-chain fructooligosaccharides, pectin hydrolysate-derived acidic oligosaccharides daily | Placebo n = 19 |
Immune activation (soluble [s]CD14, LPS); impact on commensal and pathogenic bacterial species Flatulence and abdominal distension by week 12 were noted. |
| Heiser et al [30] | n = 35 HIV+ adults on ARV (nelfinavir-containing regimen) Pilot study |
12 wk | Phase 1: Probiotics (1.2 g of acidophilus/bifidus mix) and 12 g/d of soluble fiber first 4 wk; Phase 2 added in 10/g day titrated up to 30 g/day within 1 wk of l-glutamine (“S” group) n = 28 in S (active) |
Standard of care (“C”) n = 7 |
Diarrhea-primary CD4, HIV VL-secondary |
| Hemsworth et al [41] | n = 25 Adult HIV+ pilot study On ARV |
30 d each tx; 14 d washout | MN and probiotic (A), MN alone (B) and probiotic alone (C). ABC, BCA, or CBA A: MN plus Lactobacillus rhamnosus CAN-1 (minutes 109 cfu/mL); B: MN alone; and C: L rhamnosus CAN-1 (minutes 109 cfu/mL). |
3-arm crossover design | No single primary outcome stated; effects on immune status, bowel health, and QoL |
| Hummelen et al [29] | n = 65 (see also next entry) |
25 wk (6 mo) | Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 n = 32 | Placebo n = 33 |
To prevent or cure bacterial vaginosis |
| Hummelen et al [46] | n = 65, women HIV+ ARV naive |
25 wk | Oral capsules L rhamnosus GR-1 and L reuteri RC-14 n = 32 probiotics |
Placebo n = 33 |
CD4, immune markers, diarrhea; effect on bacterial vaginosis |
| Hummelen et al [36] | N = 112 Adult (>18) HIV+ ARV naive |
4 wk | MN fortified yogurt with L rhamnosus GR-1 n = 55 |
a MN fortified yogurt without additional probiotic L rhamnosus GR-1 (n = 57) for 4 wk |
CD4 Secondary outcomes: hematology indicators (creatinine, albumin, ALT, and full blood count), incidence of diarrheal episodes, symptoms, physical energy and their ability to perform activities of daily living. |
| Irvine et al [38] | n = 150 HIV+
Mixed ARV use. |
3 y | Probiotic yogurt consumption. n = 68 on probiotics |
Not consuming the yogurt. n = 82 |
CD4 count; prophylactic effect on diarrhea |
| Irvine et al [21] | n = 171 Adult HIV+ approximately 60% on ARV |
3 y (see above) | Plain yogurt supplemented with the probiotic strain L rhamnosus GR-1 (Fiti) as an adjunct to the diet; patients on ARV n = 85 |
Not consuming probiotic yogurt rather maize flour, beans n = 86 |
GI health, QoL, and immune function. |
| Kerac et al [24] | 795 children with severe acute malnutrition (age range, 5–168 mo) HIV+: 170/399 (42.6%) Few on ARV |
Median 33 d | Synbiotic2000 Forte (Medipharm AB, Kagerod, Sweden): 1011 cfu total of mix of Pediococcus pentosaceus 16:1 LMG P-20608, Leuconostoc mesenteroides 23–77:1 LMG P-20607, Lactobacillus paracasei subsp paracasei F-19 LMG P-17806, and L plantarum 2362 LMG P-20606 plus prebiotic fibres (2.5 grams of each per 1011 bacteria) (oat bran [rich in β-glucans], inulin, pectin, and resistant starch). | Standard RUTF HIV+ 192/396 (48.5%) |
Nutritional cure (weight-for-height >80% of National Center for Health Statistics median on 2 consecutive outpatient visits). Secondary outcomes included death, weight gain, time to cure, and prevalence of clinical symptoms (diarrhea, fever, and respiratory problems). |
| Saint-Marc et al [20] | n = 17 with various serious OIs, stage IV disease | 15 d |
Saccharomyces boulardii
n = 17 |
None | Impact on diarrhea; weight |
| Saint-Marc et al [33] | n = 35 HIV+
All pts on AZT, stage IV disease |
7 d |
S boulardii; 2 500-mg sachets n = 18 |
Placebo n = 17 |
Impact on diarrhea |
| Salminen et al [35] | n = 17 HIV+
On ARV (20 enrolled; 1 lost to f/u after first period; 2 before randomization) |
2 wk |
L rhamnosus GG caps, 1–5 × 1010 cfu n = 17 |
Placebo n = 17 (crossover) |
Primary GI symptoms/diarrhea; VAS 0–100 mm CD4, HIV load monitored |
| Schunter et al [42] | N = 33 HIV+ women on ARV | 4 wk | Synbiotic 2000 (see Kerac et al [24] entry) n = 14 |
Fiber-only placebo n = 13 (PP) |
Microbial translocation; cellular activation; plasma and fecal bacterial levels |
| Trois et al [34] | N = 77 RCT, HIV+ children; 48.6% (probiotics) and 61.5% (placebo) on ARV; 62.2% and 48.7% in probiotics and placebo arms, respectively, were using didanosine |
2 mo | Standard formula containing Bifidobacterium bifidum with Streptococcus thermophilus—2.5 × 1010 cfu in 100 mL milk. n = 38 |
Placebo (14 g formula diluted in 100 mL of milk) daily throughout a 2-month period. n = 39 |
1- CD4 2- The quality and number of stools assessed by questionnaire (watery to normal stool consistency, number of stools passed during a 24-h period). |
| Villar-García et al [26] | n = 44 HIV+
Stable ARV, VL < 20 for at least 2 y |
12 wk w/12 wk follow-up |
S boulardii, 6 × 107 living “bacteria” n = 22 |
Placebo n = 22 |
Translocation: change of LBP Other markers of translocation, CD4 |
| Wolf et al [37] | n = 39 HIV+
Most not on ARV. |
21 and 35 d study |
L reuteri
n = 21 |
Placebo n = 18 |
Safety, tolerability. Secondary: serum chemistry, hematology, immune profile, urinalysis, physical examination, GI tolerance and fecal microbiota data. |
| Yang et al [39] | N = 17 HIV+
CD4 ≥ 250 Population is Adults; all on ARV |
3 mo | 2 billion Bacillus coagulans GBI-30, 6086 n = 10 |
No subsps n = 7 |
Residual gut inflammation. Gastrointestinal Symptom Rating Scale administered monthly. Viremia, CD4+ T-cell percentage/concentration, sCD14, soluble intestinal fatty acid binding protein, sCD163, d-dimer, CRP, IL-8, and tumor necrosis factor-α |
Abbreviations: ALT, alanine transaminase; ARV, antiretroviral; AZT, azidothymidine; β2M, beta-2-microglobulin; cfu, colony-forming unit; CRP, C-reactive protein; DNA, deoxyribonucleic acid; FOS, fructooligosaccharide; f/u, follow up; GI, gastrointestinal; HIV, human immunodeficiency virus; IL, interleukin 6; ITT, intent to treat; LBP, lipopolysaccharide binding protein; LPS, lipopolysaccharide; MN, micronutrient; OI, opportunistic infection; PICOS, patient/problem intervention comparison outcome setting; PP, per protocol; pts, patients; QoL, quality of life; qPCR, quantitative polymerase chain reaction; RCT, randomized controlled trial; rRNA, ribosomal ribonucleic acid; RUTF, ready-to-use therapeutic food; tx, treatment; VAS, Visual Analogue Scale; VL, viral load.
QUALITY APPRAISAL
Risk of Bias of Individual Studies
We evaluated methodological quality with the Cochrane Collaboration's tool for assessing the risk of bias [19], on the basis of sequence generation, allocation concealment, blinding, intention to treat or per protocol analysis, missing data and attrition, and selective reporting. We recorded details of trial design, conflict of interests and sponsor, participant characteristics, interventions and outcome measures (Table 2).
Table 2.
Probiotics and Prebiotics in HIV: Methodological Quality of Studiesa
| Reference | Primary Endpoint | Study Design | Selection Bias | Performance Bias | Detection Bias | ITT/PP | Comments |
|---|---|---|---|---|---|---|---|
| Anukam et al [28] | Moderate diarrhea | DB CT | I | I | Unclear | PP | No randomization or allocation described. Research funded in part by Urex Biotech Inc. and Natural Sciences and Engineering Research Council of Canada. |
| Cunningham-Rundles et al [31] | Nutrient status and growth; colonization; immune effects | Observational case study; DB RCT | I | I | I | PP | Although 17 participants initially enrolled, only in a later description was it stated parents or children chose between identical packets (Cunningham-Rundles et al [31]). Of these, 14 were evaluable and 5 received placebo packets. |
| d′Ettorre, et al [43] | Inflammation and translocation | Observational | N/A | N/A | N/A | N/A | Comparator arm was 11 HIV-negative individuals given the 1 g probiotics bid. Bloodwork was done in each group (but not CD4 counts in the HIV- group). |
| Falasca, et al [40] | Inflammation and translocation | Observational | N/A | N/A | N/A | N/A | No comparator arm. 30 HIV+ men on ARV. |
| Gautam et al [23] | CD4, pediatric | RCT | A | I | I | PP | Randomization by using colored cards in white envelopes. Not blinded; participants received probiotic, MN syrup or sachets. |
| Gonzalez-Hernandez et al [3] | Safety, CD4, translocation | DB RCT | U | U | A | ITT | Explicit commentary on randomization and blinding methods lacking; analysis appeared to be ITT but not explicitly stated. The placebo was a product of Biogel without probiotics or prebiotic, but with the same flavor and characteristics. |
| Gori et al [18] | Soluble (s)CD14, LPS; effect on bacterial load in feces | DB RCT | U | A | A | ITT, PP | “Subjects were randomized in three groups …” but no further description. There may be conflicts of interest. Safety monitoring is not described. |
| Heiser et al [30] | Diarrhea from protease inhibitors | Randomized, not blinded | U | I | I | PP | Randomization not described; unblinded study (observational/pilot study). Glutamine added at week 4 only for treated group. |
| Hemsworth et al [41] | Immune status, bowel health, QoL | DB RCT, crossover | A | A | A | ITT, model | One dropped out within the first month. |
| Hummelen et al [46] | Bacterial vaginosis | DB RCT | A | A | A | ITT | Possible conflict of interest. |
| Hummelen et al [29] | CD4 | DB RCT | A | A | A | PP | Dr. Reid no longer holds patents for the use of Lactobacillus GR-1 and RC-14. Chr Hansen provided capsules; financial support from Danone Institute Canada, AFMnet. |
| Hummelen et al [36] | CD4 | DB RCT | A | A | A | ITT | It appears 3 early withdrawals were treated as data carried forward. |
| Irvine et al [21] | GI health, QoL, immune function. | Observational, retrospective | N/A | N/A | N/A | N/A | Observational. |
| Kerac et al [24] | Primary outcome was nutritional cure | DB RCT | A | A | A | ITT | 33-day study. No sepsis seen but investigated. Cure as weight-for-height >80% of National Center for Health Statistics median on 2 consecutive outpatient visits. |
| Saint-Marc et al [20] | Diarrhea; weight | Observational | N/A | N/A | N/A | N/A | Preliminary observational study. |
| Saint-Marc et al [33] | Diarrhea | DB RCT | A | A | A | ITT | One patient was precluded from taking doses due to a cerebral toxo-induced coma. |
| Salminen et al [35] | Primary GI symptoms, diarrhea. | DB RCT crossover | A | I | U | PP | This study was financially supported by Valio Ltd., Helsinki, Finland. 14-day washout period between treatment periods. |
| Schunter et al [42] | Translocation; cellular activation | DB RCT | A | A | A | PP | No adverse events or side effects reported or mentioned. |
| Trois et al [34] | Diarrhea; CD4 | DB RCT | U | A | U | ITT | Randomization by “cast lots” and products “blinded by a person” not involved in the study. |
| Villar-García et al [26] | Translocation | DB RCT | A | A | A | ITT, PP | 12 wk of trial with a subsequent 12-week follow-up. Computer-generated list; all blinded. IL-6 unaffected in ITT analysis but reduced in per protocol analysis. |
| Wolf et al [37] | Safety and tolerability | DB RCT | A | A | A | PP | Baseline information incomplete. Investigator could determine who received probiotics: less fecal odor, better consistency was observed. Packets were processed and coded (to maintain a double mask) by Anderson Packaging (Rockford, IL) |
| Yang et al [39] | Residual gut inflammation | DB RCT | I | I | A | PP | Randomization not described. Allocation not described nor was the placebo described. There may be conflicts of interest. |
Abbreviations: A, adequate; DB CT, double-blind controlled trial; DB RCT, DB randomized CT; GI, gastrointestinal; HIV, human immunodeficiency virus; I, inadequate; IL, interleukin; ITT, intent to treat; LPS, lipopolysaccharide; MN, micronutrient; N/A, not applicable; PP, per protocol; QoL, quality of life; U, unclear.
a Selection bias indicates how interventions were allocated and the randomization process used; performance bias describes the method used to conceal interventions/placebos; and detection bias assesses whether the provider, participant, or outcome assessor could distinguish intervention from comparator.
Risk of Bias Within Studies
Studies were assessed for randomized allocation, allocation concealment and participants, and observer blinding. Two studies were observational [20, 21].
DATA ABSTRACTION
Summary Measures
Our primary clinical outcome was the effect on diarrhea. Other outcomes included CD4, microbial translocation, microbicidal effects and bacterial vaginosis (BV). Insufficient data on viral load was available to warrant a separate assessment.
SYNTHESIS
Sepsis Risk Meta-Analysis
We pooled data from all studies with predefined and explicit reporting on sepsis risk (bacteremia or fungemia) from the use of probiotics, including HIV-negative patients (Supplemental Table). In our Bayesian fixed effects model, πi denotes the probability of not observing an adverse event in study i under the placebo condition; ρi denotes the ratio of the probability of nonevents in the treatment condition of study i relative to the probability of nonevent in the placebo condition; therefore, the probability of not observing an adverse event in the treatment condition is ρiπi. The model assumes a priori that the risk of an adverse event is more probable in the treatment condition, so that the probability ratio is contained within the unit interval, ie, 0 ≤ ρi ≤ 1. The model assumes that the probability of an adverse event is constant across studies; hence, it assumes πi = π and ρi = ρ for all studies i. To reflect lack of knowledge about the parameters, we chose to assume uniform priors on π and ρ. We approximated the posterior median of the NNH by Markov chain Monte Carlo in OpenBugs. We deemed that a Bayesian random effects analysis would not yield significant differences in our analysis [22].
RESULTS
Search Outcome
A total of 2068 titles were identified (see Figure 1). Of these, 27 were pulled for review. The following outcomes were reviewed: diarrhea (9); adverse events (11); BV (1); CD4 count (14); and translocation (6) (Figure 1 and Table 3).
Table 3.
Probiotics and Prebiotics in HIV: Summaries by Outcome
| Reference | Population | Duration | ARV | Effect | Results |
|---|---|---|---|---|---|
| Diarrhea | |||||
| Anukam et al [28] | Adult HIV+ women, n = 24 | 15 d | − | + | Diarrhea with flatulence and nausea: At 30 d, probiotic group only 4 of 12 had moderate diarrhea, whereas 8 of 11 (73%) did in the probiotic group (no P value). Resolution of other GI symptoms reported in the probiotic group but not the control. The effect disappeared at the 3-month follow-up without treatment. |
| Cunningham-Rundles et al [31] | n = 17; Pediatric HIV | 1 month/2 wk | + | + | Case report: One 11-year-old child with failure-to-thrive on AZT saw after 1-month use resolution of mouth ulcers, candidiasis, and diarrhea; improved appetite; weight gain continued 142 d posttreatment. RCT: Colonization observed by 2 wk of use; subsequent decline approximately 1 mo after stopping. Most children were anergic at BL; supplementation resulted in a positive immunological effect, generally within 1 month. No flatulence or other side effects/AE were observed. |
| Gonzalez-Hernandez et al [3] | RCT; n = 20; 4 arms; HIV+ adults | 16 wk | − | − | 5 patients in each arm, probiotic, prebiotic, synbiotic, placebo. Two patients experienced diarrhea in the placebo and diarrhea arms; 1 in the synbiotic arm; none in the prebiotic arm. |
| Heiser et al [30] | n = 35; Pilot study; HIV+ adults with diarrhea | 12 wk | + | + | Diarrhea completely resolved in 10 of 28 (36%) subjects (S). Mean (±SD) number of stools/day declined (3.40 ± 1.25–2.54 ± 1.34; P < .01). Loose, watery stools/day declined in S from 2.84 ± 1.42 to 0.74 ± 1.03 (P < .0001). For 15, stools/day decreased from 4.08 ± 1.35 to 3.06 ± 1.68 (P < .05) after starting glutamine. In C, stools/day, 4.14 ± 4.86–3.44 ± 1.68 (P = .678) and incidence of diarrhea was unchanged. In S, loperamide use decreased from 1.69 ± 2.34 to 0.31 ± 0.69 mg/day (P < .01); 18 vs 8 subjects used loperamide at 0 and 12 diarrhea/day, 3.00 ± 4.82–1.36 ± 1.29 (P = .361). Regimen with nelfinavir or lopinavir/ritonavir. |
| Hummelen et al [46] | n = 65, women | 25 wk | − | + | 13 of 51 (26%) participants experienced diarrhea for at least 1 day during the intervention. Median number of days similar in both groups and low in both groups (2 days in the placebo group/median 151 days recorded vs 5 days in the probiotic group/148 day recorded) (P = .4). Adverse event: Control: 2 diarrhea, 1 constipation, 3 nausea, 2 itching or peeling skin, 1 dizziness, and 1 vaginal odor. Probiotics: none reported having diarrhea; 1 abdominal discomfort; 3 nausea; 1 vomiting. |
| Hummelen et al [36] | N = 112; Adult (>18) HIV+ | 4 wk | − | (+) | Adverse event: Control: 3 reported having diarrhea. Probiotics: 1 reported having diarrhea. No difference between groups was detected in incidence or duration of diarrhea or clinical symptoms. An improvement of hemoglobin levels was observed for all subjects, based upon a mean difference from baseline of 1.4 g/L (SD = 6) (P = .02). |
| Irvine et al [38] | n = 150 HIV+ adults | 3 y | ± | + | Among those consuming yogurt, 56 of 67 (84%) participants did not report any diarrheal symptoms vs 57 of 82 (69%) participants among the nonconsuming group (P = .05). Alleviated GI symptoms, improved work productivity, nutritional intake, and tolerance to ARV. See next entry. |
| Irvine et al [21] | n = 171; adult HIV+ | 3 y (see above) | ± approximately 60% on ARV | − | No effect on incidence of diarrhea (P = .1). Clinical: Median 2 h more work daily (P = .01), experienced a lower fever incidence (P = .01), and were more likely to achieve daily nutrient requirements for vitamin A, several B complex vitamins, and calcium (P = .002); less ARV-related stomach pain (P = .02) and less GI symptoms that affect daily life (P = .03). |
| Kerac et al [24] | 795 severely malnourished children | Median 33 d | − (+); Few on ARV. | − | Primary outcome: No effect on prespecified nutritional or clinical outcomes from severe acute malnutrition. Children with severe acute malnutrition (age range, 5–168 mo); HIV+: 170 of 399 (42.6%). Inpatient synbiotic users had longer duration of severe diarrhea. Outpatients had less severe diarrhea, but this was not statistically significant (P = .07). |
| Saint-Marc et al [20] | n = 17 HIV+ adults | 15 d | ? | + | Weight gain of approximately 8 kg observed; resolution of liquid diarrhea in the majority (16 of 17) and normalization of bowel in 4. CD4 count mentioned but outcomes not noted. Patients diagnosed with various serious OIs, stage IV disease. |
| Saint-Marc et al [33] | n = 35 HIV+ adults | 7 d | + | + | Resolution of diarrhea in 61% of S.b. recipients vs 12% placebo (P < .002); stool number, weight and volume also improved in S.b. group. CD4 not evaluated. All patients on AZT, stage IV disease. |
| Salminen et al [35] | n = 17 HIV+ adults | 2 wk | + | − | Diarrhea: no effect on stool frequency or stool consistency. 41% on treatment vs 29% on placebo reported fecal incontinence (P = .5). No AE or side effect-related withdrawals; no bacteremia reported. (20 enrolled; 1 lost to f/u after first period; 2 before randomization.) |
| Trois et al [34] | N = 77 HIV+ children | 2 mo | ± | (+) | Formula feeding seemed to improve bowel function; added probiotics slightly improved reduction in liquid stools but not statistically significant. Didanosine may have blunted response. 48.6% (probiotics) and 61.5% (placebo) on ARV; 62.2% and 48.7% in probiotics and placebo arms, respectively, were using ddI |
| Wolf et al [37] | n = 39 HIV+ adults | 21 and 35 d study | −/some + | − | Bowel function or symptoms: no effect; L reuteri may be fed to HIV-positive individuals at 1 × 1010 cfu/day “without any clinically significant safety or tolerance problems.” |
| CD4 | |||||
| Anukam et al [28] | Adult HIV+ women, n = 24 | 15 d | − | + | 8 of 12 subjects at day 15 and 10 of 11 at day 30, who consumed the probiotic yogurt, had an increase in CD4; placebo 347.25 ± 76.81–30 d change −2.2; Tx 359.9 ± 70.1–30 d change + 6.7 (mean values) |
| d′Ettorre et al [43] | Adult HIV+; n = 11 | 48 wk | + | + | A weak increase in CD4 percentages and absolute numbers among HIV-1-infected patients between T0 and T1 was observed (respectively 26.45 ± 10.46 and 28.1 ± 8.62, P = .065) with median recovery of 65 cell/μL. |
| Falasca et al [40] | Adult HIV+; n = 30 | 4 wk | + | (+) | Average increase 45.9 ± 35.2 cells/µL (732.2 ± 208.1 vs 778.1 ± 286.8 cell/µL, P = .154). No control arm. Effect was not statistically significant. |
| Gautam et al [23] | n = 146 HIV+ ≤15 years old | 3 mo | ± | + | BL CD4 was over 600. Not on ARV, children 5–15 saw a +65 increase in probiotic arm (n = 20) vs −88 decline in control (n = 25; P = .0022). WHO stage improved in probiotics arm (P = .02). On ARV, there was no effect on WHO stage of disease or BMI. Similar decreases in CD4 were seen in both groups on ARV. Patients randomized by ARV use |
| Gonzalez-Hernandez et al [3] | RCT; n = 20 | 16 wk | − | + | 5 patients in each of 4 arms. The synbiotic group had greatest CD4 increase (+102; P = .05); IL-6 decreased significantly (P = .016). |
| Gori et al [18] | n = 57 HIV+ Each arm, n = 19 | 12 wk; f/u 16 wk | − | − | No effect on CD4 changes in any arm (prebiotics only). |
| Heiser et al [30] | n = 35; pilot study | 12 wk | + | + | Placebo BL −320 ± 237–wk12 441 ± 171 NS; Tx BL–468 ± 306–wk12 590 ± 292 (P < .01); (regimen with nelfinavir or lopinavir/ritonavir) |
| Hemsworth et al [41] | n = 25; Adult HIV+ pilot study | 30 d each tx; 14 d washout | + | (+) | n = 21 for data: Mean CD4; a mean change of +19 cells/μL (SD = 142); B mean change +41 cells/μL (SD = 221). C a mean change of –7 cells/μL (SD = 154); (P all >.05); Overall: There was an overall increase in CD4 by +9 cells/μL, and the frequency of participants with a CD4 count below 200 dropped from 5 to 3. Subjects reported improved energy |
| Hummelen et al [46] | n = 65, women | 25 wk | − | + | BL→10 wk. Average −3 CD4 cells/μL (95% CI, −97 to 91) with placebo vs +50 (95% CI, −61 to 162) probiotics (P = .5). BL→25 wk. CD4 + 19 cells/μL (95% CI, −90 to 129) placebo vs probiotics +46 cells/μL (95% CI, −100 to 192; P = .8). Stratified: CD4 = 200–350 placebo mean increase of 34 cells (95% CI, −37 to 105) vs probiotics +158 cells/μL (95% CI, 35–281) at 10 weeks (P = .1). CD4 < 200: 4 on probiotics mean increase of 93 cells/μL (95% CI, 26–159) vs mean decrease of 69 cells/μL (95% CI, −95 to −42) (P = .04) of 2 on placebo. |
| Hummelen et al [36] | N = 112; Adult (>18) HIV+ | 4 wk | − | − | MN + probiotic: BL→4 wk: average decline in CD4 count of −70 cells/μL (95% CI, −154 to −15); MN alone: −63 cells/μL (95% CI, −157 to −30; P = .9). |
| Irvine et al [21] | n = 171; Adult HIV+ | 3 y | ± approximately 60% on ARV | + | Average increase in CD4 of 0.13 cells/mL per day (95% CI, .07–.20; P ≤ .001). Yogurt consumers experienced an additional increase of 0.28 cells/mL per day (95% CI, .10–.46; P = .003). Adjusting for length of time on ARV: +0.17 cells/mL per day (95% CI, .01–.34; P = .04). |
| Kerac et al [24] | 795 children HIV+: 170/399 (42.6%) | Median 33 d | − (+); few on ARV | − | CD4 taken at first outpatient visit, 2 wk after discharge from ward, seropositive children with severe acute malnutrition (age range 5–168 mo); CD4 < 20% (of seropositive children in whom CD4 taken); Synbiotic 61 of 92 (66.3%); Control 67 of 103 (65.0%); Synbiotic CD4% (mean) 18.3 ± 9.6 (n = 92); Control 17.8 ± 10.1 (n = 103) |
| Salminen et al [35] | n = 17 HIV+ On ARV | 2 wk | + | 0 | 362 ± 249 and 362 ± 239 at end of study. Crossover design may blunt effect if initial treatment with GG persists longer than 2 wk. 20 enrolled; 1 lost to f/u after first period; 2 before randomization. |
| Schunter et al [42] | N = 33 HIV+ women on ARV | 4 wk | + | − | CD4: Placebo - BL 627 (SD = 293); Day 28–619 (337); Probiotic–683 (259); Day 28–697 (296) (P = .862) |
| Trois et al [34] | N = 77 HIV+ children | 2 mo | ± | + | Mean CD4: count increased in the probiotics group and a small decrease in the control group (P = .049). Probiotics–BL 673 (528, 962); end of study: 791 (509, 951); Placebo–BL 580 (337, 821); end of study: 538 (332, 789); P = .35; Δlog10 CD4 Probiotics 0.04 (±0.19); placebo −0.26 (±0.16); P < .048 |
| Villar-García et al [26] | n = 44 HIV+ | 12 wk | + | − | No effect on CD4 count (12 wk on treatment and at 12 wk follow-up). Patients received stable ARV, VL < 20 for at least 2 yr |
| Wolf et al [37] | n = 39 HIV+ | 21 and 35 d study | −/some + | − | CD4 Placebo −Day 0–441 ± 31; Day 21–467 ± 34–intervention ended; Day 35–484 ± 34; L. reuteri −Day 0–498 ± 39; Day 21–461 ± 46–intervention ended; Day 35–433 ± 33 (P = .05 at d35 between arms) |
| Yang et al [39] | N = 17 HIV+ CD4 ≥ 250 | 3 mo | + | + | CD4: −81 to + 315 (median + 31) cells/mm3 for placebo; −109–+232 (median + 25) cells/mm3 for the probiotic; CD4% median increased; −1.8% (range −7.5% to +3.7%) placebo vs +2.8% (range −1.5 to +4.7%) probiotic (P = .018). CD4+ T-cell slopes over prior year were similar, but the percentages increased more in the probiotic group compared with the placebo group. No other biomarker changes except a P = .05 observed drop in sCD163. No adverse events: “safe and well tolerated.” |
| Bacterial Vaginosis | |||||
| Hummelen et al [46] | n = 65 | 25 wk (6 mo) | − | (+) | Cure of BV unaffected but may act as a prophylaxis against recurrence. |
| Hummelen et al [29] | n = 65, women | 25 wk | − | (+) | Supplementation did not enhance the cure of BV among women living with HIV, but may prevent the condition among this population. |
| Translocation | |||||
| d′Ettorre et al [43] | Observational; n = 20 | 48 wk | + | + | Markers of immune activation (CD4 + CD38 + HLA-DR+, CD4 + CD38−HLA-DR+, CD4 + CD38 + HLA-DR+) and inflammation (hsCRP) decline from T0 to T1; markers of translocation (soluble [s]CD14, d-dimer) did not change significantly. |
| Falasca et al [40] | Observational; n = 30 men | 4 wk | + | (+) | Some impact on inflammatory cytokine levels; statistically significant increase in TGF-β; increase in CD56+ NK cells (possibly associated with increase in IL4/IL-1β ratio. Statistically significant reduction in cystatin-C. |
| Gonzalez-Hernandez et al [3] | RCT; n = 20 | 16 wk | − | + | Reduction in 16S rDNA in synbiotic group (P = .048). Increase in stool for beneficial bacteria and decline in Clostridium sp 5 in each arm, probiotic, prebiotic, synbiotic, placebo. |
| Gori et al [18] | n = 57 HIV+ Each arm, n = 19; | 12 wk | − | − | Activation markers: No effect (%CD8−CD38 + DR+ %CD4 + CD25 + FoxP3+ %CD14 + B7-H1*; %CD19 + B7-H1*). Increased NK cell effector/target ratios in 15 g group. No serious AEs, impact on liver/kidney function. Follow-up at 16 wk off treatment. |
| Schunter et al [42] | N = 33 HIV+ women on ARV | 4 wk | + | − | No effect on 16S rDNA, CRP, or TNF-α and γ-IFN. Increase in %CD38-DR + PD1− and decrease in CD38+ |
| Villar-García et al [26] | n = 44 HIV+ | 12 wk w/12 wk follow-up | + | − | LBP: Statistically significant decline in LBP 13.6% (n = 3) in the placebo group vs 50% (n = 11) in the probiotic group (P = .02). IL-6: Reduction in per protocol analysis (n = 19 tx, n = 16 placebo) at 12 wk and persisting at 24 wk (P < .01) β2M: Statistically significant reduction by ITT at week 24 vs placebo. However, this marker was higher at BL in treatment group (P = .02). All other markers: No effect (including LPS, sCD14, hs-CRP, fibrinogen, TNF-α, ESR. Stable ARV, VL < 20 for at least 2 years. |
Abbreviations: AE, adverse event; ARV antiretroviral; AZT, azidothymidine; β2M, beta-2-microglobulin; BL, baseline; BMI, body mass index; BV, bacterial vaginosis; cfu, colony-forming units; CI, confidence intervals; CRP, C-reactive protein; ddI, didanosine; ESR, erythrocyte sedimentation rate; f/u, follow up; GI, gastrointestinal; HIV, human immunodeficiency virus; IL, interleukin; ITT, intent-to-treat; LBP, lipopolysaccharide binding protein; NK, natural killer; NS, not statistically significant; PP, per protocol; RCT, randomized controlled trials; rDNA; ribosomal deoxyribonucleic acid; S.b., Saccharomyces boulardii; SD, standard deviation; TGF, tumor growth factor; TNF, tumor necrosis factor; Tx, treatment; VL, viral load; WHO, World Health Organization.
Studies included patients on ARVs, patients not on ARVs, and a few patients had mixed use of ARV therapy. In general, descriptions of which ARVs were used were not available (eg, [21, 23–26]). Populations included adult and pediatric studies.
Risk of Bias
Publication bias analysis was precluded by the small numbers of studies [27]. We found no evidence of selective reporting or conflicts of interest; however, some studies were funded by nutritional supplement or yogurt companies (Table 2).
Impact on Human Immunodeficiency Virus- or Antiretroviral-Associated Diarrhea
Nine studies evaluated various probiotic formulas for diarrhea. Of these, 1 showed mixed benefit, 3 reported benefit, 2 reported no benefit, 1 reported prophylactic benefit, and 2 no reported prophylactic effect. Outcomes varied in terms of frequency of stools, consistency, duration, hospital stay, and use of concomitant antimicrobials and other medications to control diarrhea. Populations varied in age (pediatric/adult) as well as ARV use. Trial duration varied from as little as 2 weeks to 3 years, with the majority of studies lasting 2–25 weeks. On those not yet on ARV, one 2-week study showed benefit [28], whereas a 25-week [29] and 33-day pediatric study showed no benefit [24].
Among those using ARV therapy, a 3-year study assessing probiotic-fortified yogurt saw symptom alleviation and improved work productivity [21]. A 12-week study that included fiber and glutamine found benefit in terms of resolution or reduction in number of stools with decreased loperamide use [30]. Although seeing resolution of diarrhea in an initial case, a further study to assess safety in pediatric populations was undertaken. This study among congenitally infected children showed that Lactobacillus plantarum 299v colonized the gut during use, and for younger children there was some improvement in offsetting anergy while potentially offsetting failure to thrive as assessed by growth rates [31, 32]. Two studies investigating Saccharomyces boulardii among very ill patients with acquired immune deficiency syndrome observed significant benefit [20, 33].
A pediatric study, where half were on stable ARV at baseline, saw no differences between arms using formula [34]. A 2-week study showed no benefit with more fecal incontinence experienced by the treated group (P = .5) [35].
In summary, overall data are inconclusive for a role of bacterially based probiotics for managing HIV-associated diarrhea; however, more studies are needed to determine whether higher doses or combinations of bacterial species may have benefit. The use of the fungal S boulardii may have some benefit.
Impact on CD4 Count/Immunological Impact
Fifteen studies reported CD4 counts at baseline and end of study. In 4 studies among ARV-naive patients, 2 found benefit, 1 found no benefit, and 1 reported increases in CD4 in treatment group and declines among placebo recipients that were not statistically significant. Among 7 studies on HIV+ patients on ARV, 4 reported benefit and 3 did not. Two studies with mixed populations on or not on ARV showed a modest increase in CD4 count. Two pediatric studies showed positive effect [8, 19].
Four studies evaluated patients not on ARV, with moderate changes over relatively short periods. The largest effect was an increase of 102 CD4 cells over 16 weeks in a synbiotic arm compared with control in a small study investigating the impact of such interventions on markers of microbial translocation and inflammation [3]. A 30-day study observed, on average, a 3- to 4-fold improvement compared with controls (P < .02) [28]. A 25-week study among women also observed an average loss of 3 CD4 cells/μL with placebo versus an increase of 50 and 46 cells/μL with probiotics at 10 weeks, although the differences were not statistically significant. Mean or median baseline and end-of-study CD4 values were not provided. However, women with CD4 < 200 at baseline saw a greater mean increase in CD4 count of 93 cells/μL versus a mean decrease of 69 cells/μL among placebo recipients [29]. No benefit was seen in a 4-week study on CD4 count [36].
Some studies reported sporadic ARV use. Among those on zidovudine monotherapy, an apparent reduction was found in CD4 count in the probiotic arm, and the authors concluded that “Because this trend continued after 2 week of washout it is not interpreted to be treatment related.” [37] An observational retrospective study over 3 years evaluated supplemented yogurt. Adjusting for length of time using ARV medication, probiotic users gained 0.17 cells/μL per day (or approximately 62 CD4/year); however, the nutritional content of the yogurt may also have had an effect [38].
Seven studies evaluated adults with HIV on ARV. In a 2-week crossover trial among 17 patients, no impact on CD4 was seen [35]. A 3-month study saw no change in absolute CD4 count; however, there was a significant increase in CD4 percentage compared with placebo (+2.8% vs −1.8%, P = .018) [39]. An open-label study of 30 HIV+ men observed an increase in CD4 over 4 weeks; however, this was not statistically significant [40]. A larger increase in those receiving glutamine and probiotics arm was significant compared with control [30]. A 3-period (30 days), crossover trial showed greater CD4 improvement in the micronutrient phase, whereas the addition of probiotics may have blunted the benefit [41]. A 4-week study using a synbiotic found no effect on CD4 count [42]. An open-label study among 20 HIV+ adults on ARV over 48 weeks showed a median increase of 65 cells/µL [43].
In an open-label, pediatric study over 3 months, the probiotic group increased CD4 count 65 cells/μL compared with a loss of 88 cells/μL in the control in children >5 years, with a trend observed among children under 5: +22 CD4 versus placebo loss of 65 cells [23]. A 2-month pediatric study observed a 118 cell increase in mean CD4 count in children 2–12 years of age versus a loss of 42 cells/mm3 in the control arm [34].
We further assessed the studies based on their interventions and CD4 outcome to see whether any pattern of benefit, lack of benefit, or harm appeared. In reviewing the data from this perspective, all studies that used bacterial interventions such as Bifidus or Lactobacilli spp all reported moderate increases in CD4 counts. A larger increase was observed among those on a synbiotic (combination of prebiotics and probiotics); however, there were only 5 patients per arm [3]. No benefit for CD4 count was seen in one study of S boulardii. Formal meta-analysis was precluded due to variability in use or not of ARV, populations (adult/pediatric) and variability in reporting CD4 data [3, 23, 29, 30, 38].
Overall, our analysis suggests a potential role for the use of probiotics in improving CD4 counts modestly. Longer-term studies of probiotics and synbiotics in the context of more advanced ARV therapy are warranted, as well as observational studies in communities where immediate ARV is not yet available.
Probiotics Impact on Bacterial Vaginosis
Bacterial vaginosis may increase risk of transmission or acquisition of HIV [44], increasing proinflammatory cytokines and disrupting mucosal barrier function [45]. We found 1 trial assessing the potential impact of probiotics. The only RCT, among 65 HIV+ women with BV defined as a Nugent score [44] of 4–10 over 6 months, showed no enhanced cure rate. However, the probiotic intervention may be prophylactic for BV [46].
Probiotics/Prebiotics Effect on Human Immunodeficiency Virus-Associated Bacterial Translocation
We found 6 studies that assessed the impact of probiotics or prebiotics on markers of translocation in HIV disease, 4 showing some effect and 2 showing none. A 16-week study of a synbiotic observed reductions in plasma bacterial deoxyribonucleic acid, and a median CD4 increase of 102 (P = .05), along with a decline in interleukin (IL)-6 (P = .016) [3]. A 4-week study with translocation as the primary endpoint found no effect on bacterial 16S ribosomal ribonucleic acid (RNA) concentration or soluble CD14 (sCD14) [42]. Another 4-week study using a yogurt drink observed an improvement in natural killer (NK) cell counts (CD56+) as well as modest reductions in messenger RNA cytokine levels of IL-1β, IL-10, IL-12, tumor growth factor-β, along with the inflammatory marker cystatin-C [40]. However, a study of mix of probiotics over 48 weeks saw no effect on markers of translocation (sCD14), but it did see improvements in markers of activation and inflammatory markers (eg, high-sensitivity C-reactive protein) [43]. A prebiotic oligosaccharide mixture given over 12 weeks resulted in reductions in sCD14 and activated CD4+/CD25+ cells along with increased NK cell activity [18, 47].
Among 44 HIV+ individuals given S boulardii over 4 weeks, LPS-binding protein (a marker of translocation) and IL-6 (a marker of inflammation) were statistically significantly decreased compared with placebo recipients. Other markers of inflammation, CD4 and CD8, were unaffected [26].
In summary, the data are inconclusive; however, there is a signal that prebiotics may have a modest impact on markers of translocation and/or markers of inflammation and immune activation. Studies assessing prebiotics versus synbiotics should be contemplated.
Probiotics: Side Effects and Adverse Events
The most serious potential adverse event from ingesting live organisms is sepsis. Numerous case reports of probiotic organisms causing bloodstream infection are reported, but no formal assessment has been made [15]. Snydman [48] noted no evidence of an increase of bacteremia at a population level of use of probiotics and stated that more trials are needed. Several studies showed no risks associated with use among neonates [49–52], although caution exists for patients with a peripherally inserted central catheter line, environmentally acquired infections arising during severe immunosuppression, and use of prebiotic and synbiotic among those with pancreatitis [15, 53]. A large study observed increased mortality when using a multispecies probiotics preparation [54]; however, others suggest that probiotics may be safe when used [55].
We reviewed and combined RCTs in people with and without HIV where probiotics were administered and risk of sepsis arising from bacteremia or fungemia was explicitly assessed (Supplementary Table). We found 39 RCTs, where the total number of study participants is 9401, and the total number that received a probiotic is 5060. We found 0 events among these RCTs.
For the Bayesian fixed effects analysis, the resulting posterior distributions for the parameters are the Beta (9402, 1) and Beta (5061, 1) distributions for π and ρ, respectively. Using Monte Carlo integration (with 1 million samples from the posterior distribution), we approximate the posterior median of the NNH to be 7369 and the 95% posterior lower credible bound for the NNH to be 1689; that is, given the studies we found, there is a 95% chance that NNH is higher than 1688, and there is a 50% chance that the NNH is higher than 7369.
Mild adverse events were reported in a systematic review, including fewer events among treatment recipients than placebo [56]. Among HIV+ adults, no unexpected adverse events (some flatulence and abdominal distension) were noted in medium- and higher-dose arms investigating a prebiotic [18].
In a review of 622 studies, 235 referred only to “well-tolerated” or other such nonspecific reference to side effects. The remaining 387 studies indicated no statistically significantly increased relative risk of overall number of adverse events. Among vulnerable populations they note: “Across studies, there was no indication that critically ill and high risk participants taking probiotics were more likely to experience adverse events than control participants with the same health status” [57].
DISCUSSION
Firm conclusions are difficult due to variability in populations, interventions, and outcomes, and as a result, data synthesis on specific outcomes was precluded. Overall, probiotics appear to exert some positive influence on clinical symptoms, a moderate improvement on CD4 count, and limited effects on markers of translocation. It was disappointing to find that studies did investigate the potential for vaginally or rectally applied probiotic suppositories as microbicides, even though such products are available on the market.
In HIV, diarrhea is caused by various infections and medications, eg, antibiotic therapy/prophylaxis, ARV therapy. Among HIV-negative populations, commensal organism supplements have a salutary effect on antibiotic-associated diarrhea [57], as well as inflammatory gut diseases and infections [15]. Mechanisms of action are not fully understood, but they may include interference with pathogen adhesion, growth and toxin release, modulation of immunity, and manipulation of host factors that reduce inflammation and encourage gut healing [2, 58].
There was some evidence that combinations of 2 or more strains were more efficacious than single strains in therapeutic and prophylactic effects on different forms of diarrhea, as some review studies have suggested [59]. Studies investigating combinations of interventions may offer greater efficacy, eg, use of agents such as glutamine, N-acetylcysteine, micronutrients for managing diarrhea [60]. Studies that include micronutrients may optimize benefits, for example, in offsetting hyperlactatemia and mitochondrial toxicity associated with some ARV drugs [61] or improving gut architecture [62].
Antiretroviral therapy-treated individuals who fail to have an immunologic response (CD4 < 200) have been observed to have lower levels of Lactobacilli, with elevated levels of LPS and sCD14 [63], whereas other research underscores that increased inflammatory markers such as IL-6 and sCD14 are elevated compared with those achieving immunological restitution or to controls [64]. There is evidence for greater translocation among untreated individuals along with immunological perturbations (eg, increased activated CD38+ and Ki67+) [65]. Few gut Lactobacilli may blunt ARV efficacy [66]. Most studies were too short to properly assess impact on immune function; however, some showed immunological benefit. Studies in macaque models underscore a potential for altering gut immunity through effects on Th17 cells [67]; however, a robust effect in improving Th17 cells in the gut was enhanced with infusion of IL-21 [68].
Probiotics show equivocal effects on markers of translocation. Although the impact of probiotics on BV was not strong, there is some evidence that BV may be prevented [69, 70], possibly reducing risk of HIV transmission.
As for the most feared risk, fungemia or bacteremia, our NNH should provide reassurance, whether one adopts the point estimate (7634) or, more conservatively, the lower bound (1689). Indeed, even the point estimate is conservative because the many studies excluded for lack of explicit assessment of sepsis most likely would have reported such an adverse event. The observed rate is far lower than to the risks of some commonly prescribed conventional medications. For example, widely used proton pump inhibitors increase the risk of C difficile infection, with a NNH ranging from 28 of those admitted to hospital using antibiotics to 899 among community patients [71]. Longer-term and community-based trials should provide more robust data.
Strengths
This systematic review evaluates the use of probiotics for the full range of outcomes in HIV disease. We developed a model for the assessment of sepsis risk in the face of a “zero numerator” challenge, helping to quantify potential risk.
Limitations
Many studies were of short duration and comprised small numbers of patients and variability in the nature of the interventions used and outcomes assessed. We deemed it inappropriate to undertake formal meta-analyses of prespecified outcomes, except for risk of sepsis. The methodological quality of several of the studies was poor (Table 2).
CONCLUSIONS
In this study, we discovered the following key results: the risk of sepsis is low; the best balance of microbial strains to use to optimize outcomes has not yet been identified, and such combinations may be specific to indications, populations, and genders; there may be potential benefit for CD4 count, recurrence, or management of BV and diarrhea; and there is an uncertain effect on translocation, BV treatment.
Future studies should focus on restoration of optimal gut, vaginal, or rectal microbiomes. There is intense and growing interest in characterizing the microbiome, including which gut ecologies are more optimal for health [72, 73]. Longer-term studies should explore using a community-relevant mix of bacteria and/or fungi for outcomes such as diarrhea and CD4 count. Studies among women to assess effects on vaginal, gastrointestinal, and microbicidal effects are warranted, as well as the use of Lactobacilli in suppositories. Species of Lactobacilli in combination with other genera may have clinically meaningful effects among those with poor immunological response despite ARV; these subsets and impact on inflammatory markers deserve further scrutiny. Such studies with immunological outcomes (CD4, activation markers) require longer duration, particularly in the context of ARV use. Such studies are being contemplated [74]. Studies of S boulardii for noninfection-associated diarrhea are warranted.
Given the paucity of evidence for adverse events, low cost, and potential for economic value to people living in poverty [2, 12], the use of probiotics seems practical and feasible. Restoration of gut flora to a more healthful ecology may have several important clinical benefits particularly in conjunction with improved nutrition and access to micronutrient supplementation [75].
Supplementary Data
Supplementary material is available online at Open Forum Infectious Diseases online (http://OpenForumInfectiousDiseases.oxfordjournals.org/).
Acknowledgments
We gratefully acknowledge the assistance of Maud Dupuy and Kirti Dasu.
Financial support. This work was supported by funds from the National Center for Complementary and Alternative Medicine (NCCAM) (grant no. 5R01AT5824); and the National Center for Advancing Translational Sciences (NCATS) (grant nos. UL1 TR001073 and 5KL2TR001071-03), of the US National Institutes of Health (NIH).
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. Lorenc A, Robinson N. A review of the use of complementary and alternative medicine and HIV: issues for patient care. AIDS Patient Care STDS 2013; 27:503–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Reid G, Anand S, Bingham MO et al. Probiotics for the developing world. J Clin Gastroenterol 2005; 39:485–8. [DOI] [PubMed] [Google Scholar]
- 3. Gonzalez-Hernandez LA, Jave-Suarez LF, Fafutis-Morris M et al. Synbiotic therapy decreases microbial translocation and inflammation and improves immunological status in HIV-infected patients: a double-blind randomized controlled pilot trial. Nutr J 2012; 11:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Douek DC, Roederer M, Koup RA. Emerging concepts in the immunopathogenesis of AIDS. Annu Rev Med 2009; 60:471–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zareie M, Johnson-Henry K, Jury J et al. Probiotics prevent bacterial translocation and improve intestinal barrier function in rats following chronic psychological stress. Gut 2006; 55:1553–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bolton M, van der Straten A, Cohen CR. Probiotics: potential to prevent HIV and sexually transmitted infections in women. Sex Transm Dis 2008; 35:214–25. [DOI] [PubMed] [Google Scholar]
- 7. Guinane S. The effectiveness of probiotics for managing diarrhoea in people with HIV infection: a critically appraised topic. HIV Med 2013; 14:187–90. [DOI] [PubMed] [Google Scholar]
- 8. Salari P, Nikfar S, Abdollahi M. A meta-analysis and systematic review on the effect of probiotics in acute diarrhea. Inflamm Allergy Drug Targets 2012; 11:3–14. [DOI] [PubMed] [Google Scholar]
- 9. McFarland LV. Probiotics for the primary and secondary prevention of C. difficile infections: a meta-analysis and systematic review. Antibiotics (Basel) 2015; 4:160–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sleator RD. Probiotics -- a viable therapeutic alternative fosr enteric infections especially in the developing world. Discov Med 2010; 10:119–24. [PubMed] [Google Scholar]
- 11. Williams B, Landay A, Presti RM. Microbiome alterations in HIV infection a review. Cell Microbiol 2016; 18:645–51. [DOI] [PubMed] [Google Scholar]
- 12. Enos MK, Burton JP, Dols J et al. Probiotics and nutrients for the first 1000 days of life in the developing world. Benef Microbes 2013; 4:3–16. [DOI] [PubMed] [Google Scholar]
- 13. Szajewska H, Kołodziej M. Systematic review with meta-analysis: Lactobacillus rhamnosus GG in the prevention of antibiotic-associated diarrhoea in children and adults. Aliment Pharmacol Ther 2015; 42:1149–57. [DOI] [PubMed] [Google Scholar]
- 14. Li BZ, Threapleton DE, Wang JY et al. Comparative effectiveness and tolerance of treatments for Helicobacter pylori: systematic review and network meta-analysis. BMJ 2015; 351:h4052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wilson NL, Moneyham LD, Alexandrov AW. A systematic review of probiotics as a potential intervention to restore gut health in HIV infection. J Assoc Nurses AIDS Care 2013; 24:98–111. [DOI] [PubMed] [Google Scholar]
- 16. Doron S, Snydman DR. Risk and safety of probiotics. Clin Infect Dis 2015; 15:S129–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sacks HS, Carter GM, Indyk D et al. Probiotic supplementation in HIV disease: Bayesian and systematic meta-analyses. PROSPERO CRD42013004766. 2013. Available at: http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42013004766. Accessed 19 August 2016.
- 18. Gori A, Rizzardini G, Van't Land B et al. Specific prebiotics modulate gut microbiota and immune activation in HAART-naive HIV-infected adults: results of the “COPA" pilot randomized trial. Mucosal Immunol 2011; 4:554–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 [updated March 2011]. The Cochrane Collaboration 2011 Available at: http://handbook.cochrane.org/. Accessed 19 August 2016.
- 20. Saint-Marc T, Rossello-Prats L, Touraine JL. Efficacy of Saccharomyces boulardii in the treatment of diarrhea in AIDS. Ann Med Interne (Paris) 1991; 142:64–5. [PubMed] [Google Scholar]
- 21. Irvine SL, Hummelen R, Hekmat S. Probiotic yogurt consumption may improve gastrointestinal symptoms, productivity, and nutritional intake of people living with human immunodeficiency virus in Mwanza, Tanzania. Nutr Res 2011; 31:875–81. [DOI] [PubMed] [Google Scholar]
- 22. Fu R, Gartlehner G, Grant M et al. Conducting quantitative synthesis when comparing medical interventions: AHRQ and the Effective Health Care Program. J Clin Epidemiol 2011; 64:1187–97. [DOI] [PubMed] [Google Scholar]
- 23. Gautam N, Dayal R, Agarwal D et al. Role of multivitamins, micronutrients and probiotics supplementation in management of HIV infected children. Indian J Pediatr 2014; 81:1315–20. [DOI] [PubMed] [Google Scholar]
- 24. Kerac M, Bunn J, Seal A et al. Probiotics and prebiotics for severe acute malnutrition (PRONUT study): a double-blind efficacy randomised controlled trial in Malawi. Lancet 2009; 374:136–44. [DOI] [PubMed] [Google Scholar]
- 25. Schunter M, Chu H, Hayes TL et al. Randomized pilot trial of a synbiotic dietary supplement in chronic HIV-1 infection. BMC Complement Altern Med 2012; 12:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Villar-García J, Hernández JJ, Güerri-Fernández R et al. Effect of probiotics (Saccharomyces boulardii) on microbial translocation and inflammation in HIV-treated patients: a double-blind, randomized, placebo-controlled trial. J Acquir Immune Defic Syndr 2015; 68:256–63. [DOI] [PubMed] [Google Scholar]
- 27. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Anukam KC, Osazuwa EO, Osadolor HB et al. Yogurt containing probiotic Lactobacillus rhamnosus GR-1 and L. reuteri RC-14 helps resolve moderate diarrhea and increases CD4 count in HIV/AIDS patients. J Clin Gastroenterol 2008; 42:239–43. [DOI] [PubMed] [Google Scholar]
- 29. Hummelen R, Changalucha J, Butamanya NL et al. Effect of 25 weeks probiotic supplementation on immune function of HIV patients. Gut Microbes 2011; 2:80–5. [DOI] [PubMed] [Google Scholar]
- 30. Heiser CR, Ernst JA, Barrett JT, French N et al. Probiotics, soluble fiber, and L-glutamine (GLN) reduce nelfinavir (NFV)- or lopinavir/ritonavir (LPV/r)-related diarrhea. J Int Assoc Physicians AIDS Care (Chic) 2004; 3:121–9. [DOI] [PubMed] [Google Scholar]
- 31. Cunningham-Rundles S, Ahrne S, Bengmark S et al. Probiotics and immune response. Am J Gastroenterol 2000; 95:(1 Suppl)S22–5. [DOI] [PubMed] [Google Scholar]
- 32. Cunningham-Rundles S, Ahrne S, Johann-Liang R et al. Effect of probiotic bacteria on microbial host defense, growth, and immune function in human immunodeficiency virus type-1 infection. Nutrients 2011; 3:1042–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Saint-Marc T, Blehaut H, Musial C, Touraine JL. [Diarrhees en relation avec le sida: essai en double aveugle de Saccharomyces boulardii]. Semaine Des Hopitaux 1995; 71:735–41. [Google Scholar]
- 34. Trois L, Cardoso EM, Miura E. Use of probiotics in HIV-infected children: a randomized double-blind controlled study. J Trop Pediatr 2008; 54:19–24. [DOI] [PubMed] [Google Scholar]
- 35. Salminen MK, Tynkkynen S, Rautelin H et al. The efficacy and safety of probiotic Lactobacillus rhamnosus GG on prolonged, noninfectious diarrhea in HIV patients on antiretroviral therapy: a randomized, placebo-controlled, crossover study. HIV Clin Trials 2004; 5:183–91. [DOI] [PubMed] [Google Scholar]
- 36. Hummelen R, Hemsworth J, Changalucha J et al. Effect of micronutrient and probiotic fortified yogurt on immune-function of anti-retroviral therapy naive HIV patients. Nutrients 2011; 3:897–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wolf BW, Wheeler KB, Ataya DG, Garleb KA. Safety and tolerance of Lactobacillus reuteri supplementation to a population infected with the human immunodeficiency virus. Food Chem Toxicol 1998; 36:1085–94. [DOI] [PubMed] [Google Scholar]
- 38. Irvine SL, Hummelen R, Hekmat S et al. Probiotic yogurt consumption is associated with an increase of CD4 count among people living with HIV/AIDS. J Clin Gastroenterol 2010; 44:e201–5. [DOI] [PubMed] [Google Scholar]
- 39. Yang OO, Kelesidis T, Cordova R, Khanlou H. Immunomodulation of antiretroviral drug-suppressed chronic HIV-1 infection in an oral probiotic double-blind placebo-controlled trial. AIDS Res Hum Retroviruses 2014; 30:988–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Falasca K, Vecchiet J, Ucciferri C et al. Effect of probiotic supplement on cytokine levels in HIV-infected individuals: a preliminary study. Nutrients 2015; 7:8335–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hemsworth JC, Hekmat S, Reid G. Micronutrient supplemented probiotic yogurt for HIV-infected adults taking HAART in London, Canada. Gut Microbes 2012; 3:414–9. [DOI] [PubMed] [Google Scholar]
- 42. Schunter M, Chu H, Hayes TL et al. Randomized pilot trial of a synbiotic dietary supplement in chronic HIV-1 infection. BMC Complement Altern Med 2012; 12:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. d'Ettorre G, Ceccarelli G, Giustini N et al. Probiotics reduce inflammation in antiretroviral treated, HIV-infected individuals: results of the “Probio-HIV” clinical trial. PLoS One 2015; 10:e0137200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pirotta M, Fethers KA, Bradshaw CS. Bacterial vaginosis - More questions than answers. Aust Fam Physician 2009; 38:394–7. [PubMed] [Google Scholar]
- 45. Mirmonsef P, Krass L, Landay A, Spear GT. The role of bacterial vaginosis and trichomonas in HIV transmission across the female genital tract. Curr HIV Res 2012; 10:202–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hummelen R, Changalucha J, Butamanya NL et al. Lactobacillus rhamnosus GR-1 and L. reuteri RC-14 to prevent or cure bacterial vaginosis among women with HIV. Int J Gynaecol Obstet 2010; 111:245–8. [DOI] [PubMed] [Google Scholar]
- 47. Gori A, Van't Land B, Rizzardini G et al. Immune activation and gut microbiota can be positively modified in HAART-naive HIV-infected adults by specific prebiotics. HIV Med 2009; 10(suppl 2):120. [Google Scholar]
- 48. Snydman D. The safety of probiotics. Clin Infect Dis 2008; 46 (suppl 2):S104–11. [DOI] [PubMed] [Google Scholar]
- 49. Dasopoulou M, Briana DD, Boutsikou T et al. Motilin and gastrin secretion and lipid profile in preterm neonates following prebiotics supplementation: a double-Blind randomized controlled study. JPEN J Parenter Enteral Nutr 2015; 39:359–68. [DOI] [PubMed] [Google Scholar]
- 50. Srinivasjois R, Rao S, Patole S. Prebiotic supplementation in preterm neonates: updated systematic review and meta-analysis of randomised controlled trials. Clin Nutr 2013; 32:958–65. [DOI] [PubMed] [Google Scholar]
- 51. Piemontese P, Giannì ML, Braegger CP et al. Tolerance and safety evaluation in a large cohort of healthy infants fed an innovative prebiotic formula: a randomized controlled trial. PLoS One 2011; 6:e28010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Braegger C, Chmielewska A, Decsi T et al. Supplementation of infant formula with probiotics and/or prebiotics: a systematic review and comment by the ESPGHAN committee on nutrition. J Pediatr Gastroenterol Nutr 2011; 52:238–50. [DOI] [PubMed] [Google Scholar]
- 53. Morrow LE, Gogineni V, Malesker MA. Probiotic, prebiotic, and synbiotic use in critically ill patients. Curr Opin Crit Care 2012; 18:186–91. [DOI] [PubMed] [Google Scholar]
- 54. Besselink MG, van Santvoort HC, Buskens E et al. Probiotic prophylaxis in predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial. Lancet 2008; 371:651–9. [DOI] [PubMed] [Google Scholar]
- 55. Bongaerts GP, Severijnen RS. A reassessment of the PROPATRIA study and its implications for probiotic therapy. Nat Biotechnol 2016; 34:55–63. [DOI] [PubMed] [Google Scholar]
- 56. Van den Nieuwboer M, Brummer RJ, Guarner F et al. The administration of probiotics and synbiotics in immune compromised adults: is it safe? Benef Microbes 2015; 6:3–17. [DOI] [PubMed] [Google Scholar]
- 57. Hempel S, Newberry S, Ruelaz A et al. Safety of Probiotics to Reduce Risk and Prevent or Treat Disease. Evidence Report/Technology Assessment No. 200. (Prepared by the Southern California Evidence-based Practice Center under Contract No. 290-2007-10062-I.). AHRQ Publication No 11-E007 Rockville, MD: Agency for Healthcare Research and Quality 200, 2011. Available at: http://www.ahrq.gov/clinic/tp/probiotictp.htm Accessed 19 August 2016.
- 58. Reid G, Bocking A. The potential for probiotics to prevent bacterial vaginosis and preterm labor. Am J Obstet Gynecol 2003; 189:1202–8. [DOI] [PubMed] [Google Scholar]
- 59. Sarkar S. Potential of probiotics as pharmaceutical agent: a review. British Food Journal 2013; 115:1658–87. [Google Scholar]
- 60. Hummelen R, Hemsworth J, Reid G. Micronutrients, N-acetyl cysteine, probiotics and prebiotics, a review of effectiveness in reducing HIV progression. Nutrients 2010; 2:626–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lopez O, Bonnefont-Rousselot D, Edeas M et al. Could antioxidant supplementation reduce antiretroviral therapy-induced chronic stable hyperlactatemia? Biomed Pharmacother 2003; 57:113–6. [DOI] [PubMed] [Google Scholar]
- 62. Louis-Auguste J, Greenwald S, Simuyandi M et al. High dose multiple micronutrient supplementation improves villous morphology in environmental enteropathy without HIV enteropathy: results from a double-blind randomised placebo controlled trial in Zambian adults. BMC Gastroenterol 2014; 14:15–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Merlini E, Bai F, Bellistri GM et al. Evidence for polymicrobic flora translocating in peripheral blood of HIV-infected patients with poor immune response to antiretroviral therapy. PLoS One 2011; 6:e18580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Lederman MM, Calabrese L, Funderburg NT et al. Immunologic failure despite suppressive antiretroviral therapy is related to activation and turnover of memory CD4 cells. J Infect Dis 2011; 204:1217–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Marchetti G, Bellistri GM, Borghi E et al. Microbial translocation is associated with sustained failure in CD4R T-cell reconstitution in HIV- infected patients on long-term highly active antiretroviral therapy. AIDS 2008; 22:2035–44. [DOI] [PubMed] [Google Scholar]
- 66. Merlini E, Bai F, Ferramosca S et al. Characterization of the translocating microflora in peripheral blood of severely immune depressed HIV+ naive patients: may the microbiota influence the response to HAART? In: Infection Conference: Italian Conference on AIDS and Retroviruses, ICAR 2010, 20–22 June 2010, Poster PO 111 Brescia: Italy Infection 2010; 38(suppl 1):93. [Google Scholar]
- 67. Vujkovic-Cvijin I, Swain LA, Chu SN et al. Gut-resident Lactobacillus abundance associates with IDO1 inhibition and Th17 dynamics in SIV-infected macaques. Cell Rep 2015; 13:1589–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ortiz AM, Klase ZA, DiNapoli SR et al. IL-21 and probiotic therapy improve Th17 frequencies, microbial translocation, and microbiome in ARV-treated, SIV-infected macaques. Mucosal Immunol 2016; 9:458–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Homayouni A, Bastani P, Ziyadi S et al. Effects of probiotics on the recurrence of bacterial vaginosis: a review. J Low Genit Tract Dis 2014; 18:79–86. [DOI] [PubMed] [Google Scholar]
- 70. Parma M, Stella Vanni V, Bertini M, Candiani M. Probiotics in the prevention of recurrences of bacterial vaginosis. Altern Ther Health Med 2014; 20 (suppl 1):52–7. [PubMed] [Google Scholar]
- 71. Kwok CS, Arthur AK, Anibueze CI et al. Risk of Clostridium difficile infection with acid suppressing drugs and antibiotics: meta-analysis. Am J Gastroenterol 2012; 107:1011–9. [DOI] [PubMed] [Google Scholar]
- 72. Mutlu EA, Keshavarzian A, Losurdo J et al. A compositional look at the human gastrointestinal microbiome and immune activation parameters in HIV infected subjects. PLoS Pathog 2014; 10:e1003829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Taguer M, Maurice CF. The complex interplay of diet, xenobiotics, and microbial metabolism in the gut: implications for clinical outcomes. Clin Pharmacol Ther 2016; 99:588–99. [DOI] [PubMed] [Google Scholar]
- 74. Kim CJ, Walmsley SL, Raboud JM, Kovacs C et al. Can probiotics reduce inflammation and enhance gut immune health in people living with HIV: study designs for the probiotic visbiome for inflammation and translocation (PROOV IT) pilot trials. HIV Clin Trials 2016; 17:147–57. [DOI] [PubMed] [Google Scholar]
- 75. Carter GM, Indyk D, Johnson M et al. Micronutrients in HIV: a bayesian meta-analysis. PLoS One 2015; 10:e0120113. [DOI] [PMC free article] [PubMed] [Google Scholar]


