Abstract
Study Design
The effects of participant characteristics along with descriptions of pain, and psychological involvement, such as fear avoidance, were assessed using structural equation modeling to identify relationships between these factors and disability as a result of low back pain.
Objective
The aim of this study was to evaluate the relationship between factors related to pain description, participants’ characteristics, psychological involvement and disability through structural equation modeling.
Summary of Background Data
Low back pain is a complex multifactorial condition that can lead to disability. Understanding which factors contribute to disability and how those factors interact is important for predicting and minimizing disability in patients with low back pain.
Methods
We analyzed data from 156 participants (63% female) with low back pain. A stepwise structural equation model was built with patient characteristics, pain intensity, depression, anxiety and fear avoidance to predict disability in low back pain.
Results
Participants were 23–84 (49.7±15.1) years of age and experienced 0.03–300 months duration (25.5±36.4) of current low back pain. The final model explained 62% of the variance in disability and included female gender, full-time employment, depression, and fear avoidance beliefs as significant predictors. Full-time employment was the only significant predictor that reduced disability; all other significant predictors increased disability in the model.
Conclusions
Understanding the relationship between these predictors and disability provides a foundation for predicting and managing disability for individual patients who suffer from low back pain.
Keywords: Low back pain [MeSH], depression [MeSH], anxiety [MeSH], structural equation modeling, disability, fear avoidance, pain intensity, pain characteristics, female gender, full-time employment
Introduction
Low back pain (LBP) is the second most common source of disability and lost productive time for adults in the United States 1–3, with a lifetime prevalence of estimated 60–85% 4. Almost eight million American adults cited back or spine problems as the source of their disability 5. Chronic pain costs the United States roughly $560–635 billion and 102 million work days annually6,7.
Only 10–15% people with LBP will develop chronic pain, and the prevalence increases with age 8,9. Some studies have attempted to identify those patients at risk of developing disability due to chronic LBP. Two reviews found patients who use catastrophizing as a pain coping strategy and those who had more fear avoidance beliefs had more pain and disability 9,10. Furthermore, another study found that patients who had a moderate to vigorous baseline activity level had less pain and disability after a year than those who were sedentary 11. Disability related to LBP peaks for patients between the ages of 41–60 years old 8.
Additionally few medical determinants have been found to lead to LBP disability such as ergonomic, psychosocial, personality, cognitive, and sociodemographic 12. While factors have been found to relate to both LBP and disability, it is still unclear how each factor impacts disability and their percent variance contributing to disability. In addition many pain descriptors (i.e. pain intensity, pain frequency, etc.) routinely assessed during clinical practice have not been investigated before. Thus, the aim of this study was to evaluate the relationship between factors related to pain description, participants’ characteristics, fear of movement and disability through structural equation modeling to gain a better understanding of variance in disability. By understanding the contribution of these factors that lead to disability, healthcare providers may be better able to triage their patients and focus on limiting disability by addressing significant contributing factors.
Materials and Methods
Participants
One hundred fifty six patients were included in the study. The participants were recruited at a large medical center (University of Kansas Medical Center) between 2010 and 2015, after receiving approval from the Institutional Review Board. Participants were included if they were at least 18 years old, had LBP, and consented to have their data included in this analysis. Participants were excluded if they had spinal tumor or infection, spine trauma that caused movement limitation, head trauma, neurological diseases, or psychiatric or cognitive disorder reported by the subjects. All subjects were English speaking.
Materials
In addition to patient characteristics, which served as control variables, the following scales and questionnaires were used in the structural equation model (SEM) analyses:
Visual Analogue Scale (VAS) 13
The average pain intensity was assessed through the VAS, a 10-point scale ranging from no pain (0) to worst pain imagined (10). The present pain intensity (PPI) is a 6-point scale measures the magnitude of pain experienced by the patient. Both the average pain intensity and PPI were combined in one second-order latent variable (an unobserved variable that cannot be directly measured) for the SEM analysis.
Oswestry Disability Index 14
A 10-item questionnaire assessing the patient’s perceived limitations on their activities due to LBP. It is presented as one overall score for disability and was the dependent variable.
Fear Avoidance Beliefs Questionnaire (FABQ)15
A 16-item questionnaire on patient’s beliefs that pain will negatively impact activities. The two subsections relate to physical and work activity related fear were combined in one latent variable for the SEM analysis.
Beck Depression Inventory (BDI)16
A 21-item inventory assessing physical and emotional symptoms of depression and was used as a latent variable in our SEM analysis.
Beck Anxiety Inventory (BAI)17
A 21-item inventory assessing physical and emotional anxiety symptoms and was used as a latent variable in our SEM analysis.
Procedure
Participants were consented and were informed of how their data would be used. Participant characteristics were collected for all patients, including age, gender, height, weight, back pain descriptors and duration, and work status. Each patient also completed the same questionnaires, described above, to obtain information on pain, fear, depression, anxiety, and disability. Missing data points were replaced using mean imputation.
Data analyses
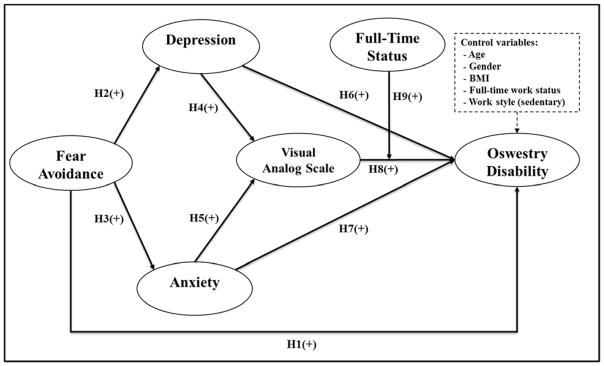
We decided to analyze our research model using structural equation modeling (SEM) statistical technique which is a latent variable-based multivariate technique enabling multiple hypothesized relationships to be tested simultaneously18 because multiple regression does not allow such a holistic modeling. The variance-based SEM—partial least squared (PLS) approach was employed to assess the psychometric properties of the measurement instrument and the research hypotheses (Figure 1). PLS is particularly recommended for exploratory models like ours, theory development, and when data is not normally distributed 18,19. The software WarpPLS 5.0 was used to generate estimates for validity and reliability of the measurement instrument, confirmatory factor analysis, and the SEM analysis 20.
Figure 1.
Hypotheses for Structural Equation Modeling Analysis
As can be seen in Table 1 and 2, all measures were valid and reliable. Loadings of all items were greater than the minimum recommended threshold of 0.50 21. Cronbach’s alpha and composite reliability values exceeded the recommended threshold of .50 and .70 22.
Table 1.
Latent variable reliability and validity
| Latent variable | Indicator | Loadings | CRa | CAb | FVIFc | Normald |
|---|---|---|---|---|---|---|
| VASe | VAS PPIf | 0.880 | 0.872 | 0.708 | 2.942 | No |
| VAS (ave)g | 0.880 | |||||
| FABQh | FABQ (work)i | 0.850 | 0.839 | 0.616 | 1.927 | Yes |
| FABQ (physical)j | 0.850 |
Notes: All loadings significant at the P<0.001 level;
CR = composite reliability;
CA = Cronbach’s alpha;
FVIF = Full collinearity variance information factor;
Normal = Normal (robust Jarque–Bera).
VAS = visual analogue scale,
PPI = present pain intensity,
VAS (ave) = average pain intensity on visual analogue scale;
FABQ = fear avoidance beliefs questionnaire,
FABQ (work) = work activity related fear,
FABQ (physical) = physical activity related fear.
Table 2.
Latent variable correlation matrix
Notes: Square roots of average variances extracted (AVE) shown on diagonal within parentheses;
VAS = visual analogue scale;
FABQ = fear avoidance beliefs questionnaire.
The square roots of the average variance extracted (AVE), in brackets in Table 2, exceeded the correlations among latent variables 23, indicating acceptable discriminant validity.
An assessment of variance inflation factors (VIF) shows that multicollinearity as a threat is ruled out. Table 1 shows that one of the latent variables was not normally distributed, confirming the suitability to use PLS-based SEM.
Bootstrapping resampling method with 156 data points and 100 resamples were used to assess the structural model. The structural model had acceptable fit indices 24–26, shown in Table 3, indicating that the quality of our structural model is adequate.
Table 3.
Model fit indices
| Index | Value | Interpretation |
|---|---|---|
| Average path coefficient (APC) | 0.147 | P<.001 |
| Average R2 (ARS) | 0.243 | P<.001 |
| Average adjusted R2 (AARS) | 0.227 | P<.001 |
| Average block VIF (AVIF) | 1.399 | Acceptable if <= 5, ideally <= 3.3 |
| Average full collinearity VIF (AFVIF) | 1.563 | Acceptable if <= 5, ideally <= 3.3 |
| Tenenhaus GoF (GoF) | 0.481 | Small >= .1, medium >= .25, large >= .36 |
Results
The final sample compromised of 156 participants aged 23–84 years (49.7±15.1). Females represented 63% while males were 37%. On average, 50% of the participants worked full time, had an average BMI of 29.6, 53% had sedentary jobs, had 0.25–348 months duration (83±82) of initial LBP and 0.03–300 months (25.5±36.4) of current LBP, 36% participants had constant LBP while 28% had intermittent pain, 35% had LBP only, 26% had buttock and thigh pain, and 39% had distal to knee pain; 41% described their pain as dull, 26% as sharp, and 33% as both.
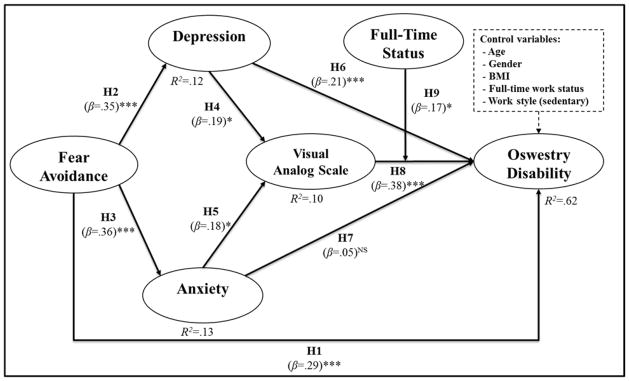
Table 4 and Figure 2 depict the results of our proposed research model estimates including the standardized path coefficients, significance of the paths coefficients, and the variance explained (R2) by the independent variables.
Table 4.
Path coefficients of stepwise structural model analysis
|
Model 1 Oswestry Disability |
Model 2 Oswestry Disability |
Model 3 Oswestry Disability |
|
|---|---|---|---|
| Control variables | |||
| Age | .05a | .04a | .04a |
| Gender (Female) | .12b | .11b | .13c |
| BMI | .15b | .11a | .08a |
| Full-time work status (employment) | −.40d | −.34d | −.12b |
| Work style (sedentary) | −.07a | −.06a | −.01a |
| Low back pain current in months | −.07a | −.04a | −.06a |
| Low back pain initial in months | .02a | .05a | .06a |
| Pain frequency (intermittent and constant) | .14b | .04a | .04a |
| Pain description (dull, sharp, or both) | .13b | .08a | .04a |
| Pain location (1=low back only, 2= buttock and thigh, 3=distal to knee) | .11a | .05a | −.06a |
| Main effects | |||
| Visual analogue scale | .33d | .38d | |
| DBI | .21d | ||
| BAI | .05a | ||
| FABQ | .29d | ||
| Interaction effects | |||
| Full-time work status*Visual analogue scale | .17b | ||
| R2 | .39 | .46 | .62 |
Notes:
Not Significant;
P<0.05;
P<0.01;
P<0.001.
Figure 2.
Results for related hypotheses for Structural Equation Model
Notes: NS Not Significant; * P<0.05; ** P<0.01; *** P<0.001.
Table 4 presents a summary of the results of stepwise SEM analysis. We first assessed the effect of the control variables (patient characteristics) on disability (Model). Gender, BMI, full-time work status, pain frequency, and pain description had significant effects on disability explaining 39% of the variance in disability, while age, work style, LBP durations, both current and initial pain, and pain location did not have any significant effects on disability.
In the second step (Model 2), we assessed the model including all control variables and added the VAS, which is a standard predictor of disability. The results show, among the patient demographic control variables, only gender and full-time work status sustained their predictive power when introducing VAS to the model; all explaining 46% of the variance in disability.
In the third step (Model 3), we evaluated the model by including all control variables, main effects–visual analogue scale, and added depression, anxiety, and fear avoidance, as well as the moderation effect of full-time work status on the relationship between VAS and disability. Again, among the control variables, only gender and full-time work status kept their predictive power while the rest were all not significant. As for the main and moderation effects, all had significant effects on the disability variable except for anxiety.
The final model (Model 3) compromising the main and moderating effects explained 62% of the variance in the disability variable. When comparing the R2 values of the third model to Model 1 and Model 2, disability variable’s explained variance increased by 23 percentage points (from 39% to 62%) and by 16 percentage points (from 46% to 62%), respectively. In other words, psychological predictors including depression, and fear avoidance as well as the moderation effect of full-time work status improved the prediction of disability by 16% while the pain predictor –visual analogue scale– improved it by 7%.
We also assessed the mediating effects of depression and anxiety on the relationship between fear avoidance and the dependent variable, disability (Oswestry Disability Index), using a mediating test approach introduced by Preacher and Hayes (2004)27. Table 5, therefore, shows the results of the mediating effect analysis. We found that fear avoidance has high and significant effects on anxiety and depression, which in turn have overall significant relationship with disability. At the same time, both anxiety and depression have significant effect on VAS, which in turn has a strong and significant relationship with disability. This represents a nested mediating effect – that is depression, but not anxiety, serving as a significant mediator between fear avoidance and disability while its relationship with disability is mediated through VAS. Based on the mediation approach introduced by Baron and Kenny (1986)28, depression partially mediates the relationship between fear avoidance and Oswestry Disability Index, indicating that not only fear avoidance directly affects disability, but also indirectly through increasing depression. Although, VAS partially mediates the relationship between depression and disability, it does not significantly mediate the relationship between anxiety and disability.
Table 5.
Analysis of mediating effects
|
|
|||||
|---|---|---|---|---|---|
| Dependent variable
|
|||||
| Oswestry Disability
|
|||||
| Independent variable | Mediator | Direct effect | Indirect effect | Total effect | Mediation |
| Fear Avoidance | Depression, Anxiety | 0.287c | 0.142c | 0.429c | Partial |
| Depression | Visual Analog Scale | 0.209c | 0.073b | 0.282c | Partial |
| Anxiety | Visual Analog Scale | 0.49a | 0.70NSa | 0.119b | |
Notes:
Not Significant;
P<0.05;
P<0.001.
Discussion
To our knowledge, this is the first study to use SEM to assess the impact of patient characteristics, pain descriptors, and psychosocial perceptions of pain on disability resulting from LBP. Other studies have examined individual links between factors and disability, but this study presents a holistic model of patient-specific predictors, including patient characteristics, pain description (i.e. duration, frequency, etc.) and experience (as represented by the VAS), and psychological involvement (depression, etc.) that can explain 62% of disability. The model presents four main direct predictors, female gender, full-time work status, depression and fear avoidance, which contribute to disability as a result of LBP.
First are patient characteristics, specifically female gender and full-time work status. Previous studies have indicated women are more likely to report musculoskeletal diseases, such as LBP 8. Our model examined this further by consistently showing female gender to have a positive relationship with disability, regardless of the other variables included in the model. This would suggest that female gender is a significant predictor for disability as a result of LBP. Conversely, a study of work status and pain found 29.1% of permanent full-time employment reported backache 29. While nearly a third of patients in that study reported backache, our model found that having full-time employment is associated with less disability, essentially negating the effect of female gender. A previous study indicated that patients with LBP were about twice as likely to change jobs and almost 12% of job changes were the result of LBP 8. This may be the result of pain catastrophizing where patients are less likely to return to work at nine months 9. Patients who work full-time may be motivated to return to work for the salary and that decision may ultimately reduce their disability because they are more active than their sedentary counterparts as other studies have shown that maintaining physical activity reduces disability 11.
Second is the VAS for pain, which in our model was a latent variable consisting of both the 10-point scale VAS and the PPI. In the final model, VAS contributed to disability, both directly and through an interaction with full-time employment status. Both the direct and indirect pathways are positive, indicating that an increase in VAS predicted an increase in disability. The association between pain and disability has been well documented and studies have associated pain to disability through multiple methods, including episode duration, frequency, and VAS 30. Patients who are experiencing greater pain are more likely to have disability as a result of their pain.
The third predictor affecting disability is depression, which has been documented in previous studies. Patients who had acute LBP and were classified as depressive were slower to recover 31. Another study had similar findings for chronic LBP, which indicated depression impacted fatigue and ultimately disability 32. The model supports this by indicating an increase in depression reflects an increase in disability.
The fourth predictor that explained disability was fear avoidance beliefs. Prior studies have indicated that treatments which decrease fear avoidance beliefs lead to a decrease in pain and disability 10. In one study, the intervention was an educational booklet which provided patients with advice and evidence-based information, and was found to reduce fear avoidance beliefs about pain. The reduction in fear avoidance beliefs correlated with an increase in physical activity and a reduction in disability 33. Similarly, older patients who reported higher fear avoidance had higher self-reported and performance-based disability 34. These findings were supported in our model which found an increase in fear avoidance beliefs increased disability. However, when depression was combined with fear avoidance in the model, fear avoidance had greater effect on disability.
It is also worth noting that there were also significant indirect effects as well. Fear avoidance beliefs had a direct effect on disability, but also effected disability through depression and anxiety. This means that a patient who has an increase in fear avoidance beliefs may experience an increase in depression and anxiety, both of which can additionally increase the risk of disability. A similar effect was noted with depression. An increase in depression both directly increase disability and indirectly by increasing the VAS and subsequently disability. The identified relationships between fear avoidance beliefs, anxiety, depression, and VAS demonstrate the complex nature of pain and disability. The direct effects are important to consider clinically and according to our findings we recommend using fear avoidance questionnaire over depression when predicting disability status in LBP. However it is also important to recognize that indirect effects can also increase the risk of disability and may warrant further examination when there is a change in patient status to reassess the risk of disability.
This study also identified several factors which did not predict disability despite being commonly used in clinical practice. Pain descriptors, such as frequency, description, and location, are regularly used for diagnosis and prognosis, however these factors did not explain any of the variation in disability 35. Additionally, the duration of pain did not explain any of the variability in disability. While clinicians may assume that chronic pain will result in disability, none of the models in this study found that pain duration, either current or initial, predicted disability, and this is reflected in the literature 36.
There are limitations to this study. The model has a relatively small number of participants. However, the total sample size was sufficient for SEM, and the bootstrapping used in determining the model help to ensure model fit. All participants were recruited from the same large medical center and may not be representative of the national population. It is possible that there is another model which represents the relationship between predictors as well or better than the model we report. Future studies may use a larger sample from multiple centers to increase the external validity of the model.
Overall, this study identified that while commonly used pain descriptors do not predict disability, several other factors do. Female patients and those who do not work full time are at greater risk of developing disability from their LBP and may need a more thorough assessment of their pain. Managing disability for patients with LBP should involve a multidisciplinary approach and specialists in the management of depression and fear avoidance beliefs. Additionally, patients who have a high VAS score, or note an increase in their VAS score may also be at increased risk of developing disability rather than duration of time. Finally, because fear avoidance beliefs and depression both directly and indirectly explain disability, and suspected change in these predictors should be evaluated in patients with LBP.
Acknowledgments
The authors thank Zaid Mansour and Krista Sanchez for their assistance with data collection.
Footnotes
No relevant financial activities outside the submitted work.
Level of Evidence: 3
References
- 1.From the Centers for Disease Control and Prevention. Prevalence of disabilities and associated health conditions among adults--United States, 1999. Jama. 2001 Mar 28;285(12):1571–1572. [PubMed] [Google Scholar]
- 2.Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Archives of internal medicine. 2009 Feb 9;169(3):251–258. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. Jama. 2003 Nov 12;290(18):2443–2454. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- 4.Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. Journal of Spinal Disorders & Techniques. 2000;13(3):205–217. doi: 10.1097/00002517-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Archives of physical medicine and rehabilitation. 2014;95(5):986–995. e981. doi: 10.1016/j.apmr.2013.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guo HR, Tanaka S, Halperin WE, Cameron LL. Back pain prevalence in US industry and estimates of lost workdays. American journal of public health. 1999 Jul;89(7):1029–1035. doi: 10.2105/ajph.89.7.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine Committee on Advancing Pain Research C, Education. The National Academies Collection: Reports funded by National Institutes of Health. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US)National Academy of Sciences; 2011. [Google Scholar]
- 8.Palazzo C, Ravaud JF, Papelard A, Ravaud P, Poiraudeau S. The burden of musculoskeletal conditions. PloS one. 2014;9(3):e90633. doi: 10.1371/journal.pone.0090633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wertli MM, Eugster R, Held U, Steurer J, Kofmehl R, Weiser S. Catastrophizing-a prognostic factor for outcome in patients with low back pain: a systematic review. The spine journal: official journal of the North American Spine Society. 2014 Nov 1;14(11):2639–2657. doi: 10.1016/j.spinee.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Wertli MM, Rasmussen-Barr E, Held U, Weiser S, Bachmann LM, Brunner F. Fear-avoidance beliefs-a moderator of treatment efficacy in patients with low back pain: a systematic review. The spine journal: official journal of the North American Spine Society. 2014 Nov 1;14(11):2658–2678. doi: 10.1016/j.spinee.2014.02.033. [DOI] [PubMed] [Google Scholar]
- 11.Pinto R, Ferreira P, Kongsted A, Ferreira M, Maher C, Kent P. Self-reported moderate-to-vigorous leisure time physical activity predicts less pain and disability over 12 months in chronic and persistent low back pain. European Journal of Pain. 2014;18(8):1190–1198. doi: 10.1002/j.1532-2149.2014.00468.x. [DOI] [PubMed] [Google Scholar]
- 12.Truchon M, Fillion L. Biopsychosocial determinants of chronic disability and low-back pain: a review. Journal of Occupational Rehabilitation. 2000;10(2):117–142. [Google Scholar]
- 13.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17(1):45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- 14.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980 Aug;66(8):271–273. [PubMed] [Google Scholar]
- 15.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993 Feb;52(2):157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 16.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of general psychiatry. 1961 Jun;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 17.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of consulting and clinical psychology. 1988 Dec;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 18.Chin WW. Commentary: Issues and opinion on structural equation modeling. JSTOR. 1998 [Google Scholar]
- 19.Gefen D, Straub D. A practical guide to factorial validity using PLS-Graph: Tutorial and annotated example. Communications of the Association for Information systems. 2005;16(1):5. [Google Scholar]
- 20.Kock N. Using WarpPLS in e-collaboration studies: An overview of five main analysis steps. International Journal of e-Collaboration (IJeC) 2010;6(4):1–11. [Google Scholar]
- 21.Hair J, Jr, Black W, Babin B, Anderson R, Tatham R. SEM: An introduction. Multivariate data analysis: A global perspective. 2010:629–686. [Google Scholar]
- 22.Nunnally JC, Bernstein IH. Psychometric theory. New York, NY: McGraw Hill; 1994. [Google Scholar]
- 23.Fornell C, Larcker D. Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research (JMR) 1981;18(1):39–50. [Google Scholar]
- 24.Hair J, Black W, Babin B, Anderson R. Multivariate data analysis. Upper Saddle River, N.J.; London: Pearson; 2010. [Google Scholar]
- 25.Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 2005. [Google Scholar]
- 26.Kock N. WarpPLS 3.0 User Manual. Laredo, TX: ScriptWarp Systems; 2012. [Google Scholar]
- 27.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior research methods, instruments, & computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 28.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986 Dec;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 29.Benavides FG, Benach J, Diez-Roux AV, Roman C. How do types of employment relate to health indicators? Findings from the second European survey on working conditions. Journal of epidemiology and community health. 2000 Jul;54(7):494–501. doi: 10.1136/jech.54.7.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.March L, Smith EU, Hoy DG, et al. Burden of disability due to musculoskeletal (MSK) disorders. Best practice & research. Clinical rheumatology. 2014 Jun;28(3):353–366. doi: 10.1016/j.berh.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 31.Melloh M, Elfering A, Kaser A, et al. Depression impacts the course of recovery in patients with acute low-back pain. Behavioral medicine (Washington, DC) 2013;39(3):80–89. doi: 10.1080/08964289.2013.779566. [DOI] [PubMed] [Google Scholar]
- 32.Snekkevik H, Eriksen HR, Tangen T, Chalder T, Reme SE. Fatigue and depression in sick-listed chronic low back pain patients. Pain medicine (Malden, Mass) 2014 Jul;15(7):1163–1170. doi: 10.1111/pme.12435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burton AK, Waddell G, Tillotson KM, Summerton N. Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine. 1999 Dec 1;24(23):2484–2491. doi: 10.1097/00007632-199912010-00010. [DOI] [PubMed] [Google Scholar]
- 34.Camacho-Soto A, Sowa GA, Perera S, Weiner DK. Fear avoidance beliefs predict disability in older adults with chronic low back pain. PM & R: the journal of injury, function, and rehabilitation. 2012 Jul;4(7):493–497. doi: 10.1016/j.pmrj.2012.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Webb C, O’Connor F. Low Back Pain in Primary Care: An Evidence-Based Approach. In: South-Paul J, Matheny S, Lewis E, editors. CURRENT Diagnosis & Treatment in Family Medicine. Chapter 24. New York, NY: McGraw-Hill; 2011. p. 3e. [Google Scholar]
- 36.Kovacs FM, Abraira V, Zamora J, et al. Correlation between pain, disability, and quality of life in patients with common low back pain. Spine. 2004 Jan 15;29(2):206–210. doi: 10.1097/01.BRS.0000107235.47465.08. [DOI] [PubMed] [Google Scholar]