Background
Hematopoietic stem cell transplant (HSCT) is an intensive but potentially curative treatment for hematologic and lymphatic cancers. The pre-transplant period is often characterized by elevated stress due to factors such as anxiety and side effects of previous treatments [1], and stress has been associated with insomnia [2]. Coping, which has been conceptualized as approach- or avoidance-oriented (cognitive and emotional activity oriented toward or away from the stressor), may influence perceptions of stress. In the Transactional Model of Stress and Coping [3], effectiveness of coping and degree of perceived stress influence outcomes (e.g., insomnia).
Though literature on sleep disorder prevalence among HSCT candidates is limited, data suggests sleep disturbance during the pre-transplant period affects approximately 32-50% of patients [4]. However, few studies include comparison groups, many assess sleep using a single item, and few are specific to allogeneic transplant patients (i.e., cells obtained from a donor rather than from the patient). This study compared insomnia in allogeneic HSCT candidates relative to cancer-free controls, hypothesizing that HSCT candidates would report greater insomnia. It also explored whether perceived stress and coping strategies represent differentiating factors for insomnia in HSCT candidates, hypothesizing that avoidance coping would be associated with worse sleep, mediated by greater perceived stress.
Methods
Participant Eligibility
Participants were recruited for a larger IRB-approved study examining quality of life in allogeneic HSCT patients. For each patient who completed at least one follow-up assessment, attempts were made to recruit a control matched on gender, age (within five years), and education (> or ≤ 12 years of education). Eligibility criteria for all participants were (1) age ≥ 18 years, (2) no history of stroke or head trauma with loss of consciousness, (3) completed ≥ 6 years of formal education, and (4) capable of speaking and reading English. Additionally, patients had to be scheduled to receive allogeneic HSCT with peripheral blood stem cells at Moffitt Cancer Center (MCC), and controls must not have been diagnosed with any form of cancer (except non-melanoma skin cancer).
Procedure
Patient participants were recruited during regularly scheduled appointments at MCC and completed self-report questionnaires before beginning the pre-HSCT conditioning regimen. Controls were identified using a commercially available marketing database (Marketing Systems Group, Fort Washington, PA, USA) and community outreach.
Measures
Participants' demographic characteristics were collected using a standardized self-report form. Patients' disease-related information was obtained through medical chart review. The Insomnia Severity Index (ISI) [5], which contains 7 items rated on a 5-point Likert scale ranging from 0 (not at all) to 4 (very much), was used to evaluate insomnia symptoms (in this sample, α = .88 for both patients and controls). The ISI and its cutoff score of 8 for clinically significant insomnia have been validated in cancer patients [6]. In patients only, the Coping Responses Inventory (CRI) [7], which contains 48 items grouped into approach and avoidance dimensions (in this sample, α = .89 and α = .80 respectively), was used to evaluate use of strategies to cope with cancer and its treatment. The Perceived Stress Scale (PSS) [8], which contains 10 items rated on a 5-point Likert scale ranging from 0 (never) to 4 (very often), was used to evaluate participants' perceptions of their lives as stressful (in this sample, α = .88 for patients and α = .86 for controls).
Statistical Analyses
Chi-square and t-tests were conducted to compare patients' and controls' demographic characteristics and perceived stress. Between-groups differences in ISI scores and proportions meeting the cutoff for clinically significant insomnia were evaluated using linear and logistic regression. Mediational analyses were conducted to evaluate whether perceived stress mediated the relationship between coping and insomnia in patients. Separate models were run for approach and avoidance coping, and path coefficients and bootstrapped confidence intervals were estimated. Analyses were conducted using SAS version 9.4 and an alpha level of .05.
Results
Descriptives and Between-Groups Differences
Analyses included 114 patients and 86 controls (see Table 1). No significant between-groups differences were observed for demographic characteristics. Patients' perceived stress (M = 12.96, SD = 6.16) was significantly higher than controls' (M = 9.83, SD = 5.87), t(198) = -3.63, p = <.001, d = 0.52. Patients' reported insomnia severity (M = 8.03, SD = 5.45) was significantly higher than controls' (M = 5.64, SD = 4.96), β = 2.39, t(198) = 2.49, p = .002, d = 0.46. In a regression analysis, group, education, and perceived stress combined accounted for 22% of the variance in insomnia scores. Rates of clinically significant insomnia were significantly higher for patients (50%) than for controls (27%), X2(1, N = 200) = 6.16, p = .01, OR = 2.12, 95% CI = 1.17 – 3.84.
Table 1.
Characteristics of HSCT candidates and matched controls.
| Patients (n = 114) | Controls (n = 86) | p-value | |
|---|---|---|---|
| Gender (% female) | 52 (46%) | 47 (55%) | .21 |
| Age, M (range) | 54.45 (21-76) | 53.73 (21-74) | .71 |
| Ethnicity (% non-Hispanic) | 103 (90%) | 80 (94%) | .33 |
| Race (% Caucasian) | 99 (87%) | 79 (92%) | .26 |
| Marital Status (% married) | 71 (62%) | 60 (71%) | .22 |
| Education (% high school graduate) | 105 (92%) | 84 (98%) | .09 |
| Diagnosisa | |||
| Acute myelogenous leukemia | 33 (29%) | ||
| Myelodysplastic syndrome | 20 (18%) | ||
| Non-Hodgkin lymphoma | 16 (14%) | ||
| Chronic lymphocytic leukemia | 10 (9%) | ||
| Acute lymphoblastic leukemia | 9 (8%) | ||
| Other | 8 (8%) | ||
| Disease statusa | |||
| Complete remission | 50 (44%) | ||
| Partial remission | 13 (11%) | ||
| Stable disease | 25 (22%) | ||
| Refractory/relapse | 8 (7%) | ||
Percentages add to less than 100 due to missing data.
Mediational Analyses
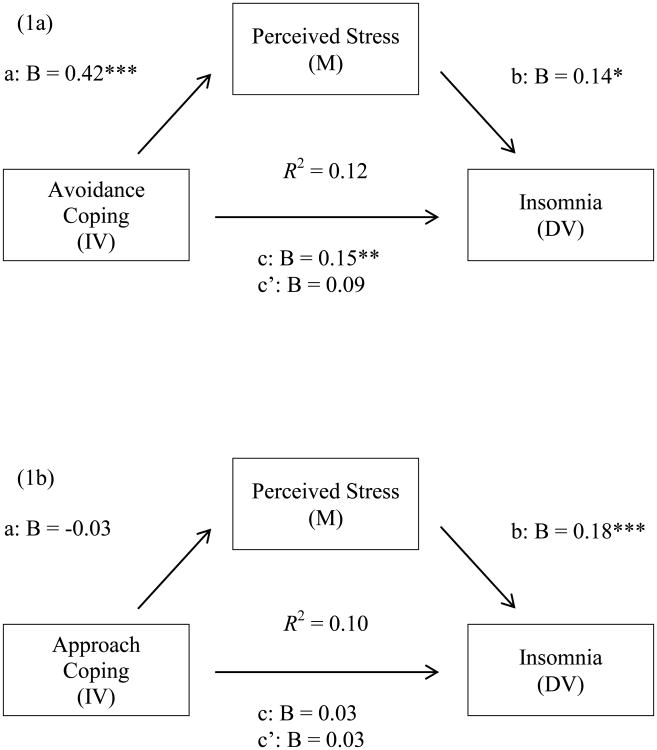
Avoidance coping was a significant predictor of insomnia (see Figure 1a). Perceived stress mediated this relationship, confirmed by the significant indirect effect of avoidance coping on insomnia (indirect effect = 0.06; 95% CI = 0.02 – 0.12) and the non-significant effect of avoidance coping on insomnia controlling for perceived stress (c′ = 0.09, p = .11). Conversely, approach coping did not predict insomnia (see Figure 1b), nor did perceived stress did not mediate this relationship (indirect effect of approach coping on insomnia = -0.01; 95% CI = -0.04 – 0.02).
Figure 1.
Tests of perceived stress as mediator of relationship between coping and insomnia. a = direct effect of independent variable (IV) on mediator (M). b = direct effect of M on dependent variable (DV). c = direct effect of IV on DV. c′ = indirect effect of IV on DV. * p < .05. ** p < .01. *** p < .001
Conclusions
This study examined insomnia in allogeneic HSCT candidates relative to cancer-free controls. Insomnia was highly prevalent in HSCT candidates prior to transplant: 50% of patients (versus 27% of controls) reported clinically significant insomnia. This study also evaluated a mediational model where perceived stress was hypothesized to mediate the relationship between coping and insomnia. The model was significant for avoidance but not approach coping, revealing a pathway from avoidance coping strategies to greater perceived stress to greater insomnia severity, which aligns with other literature demonstrating an association between avoidant coping strategies and poor physical and psychological health outcomes [9]. Study strengths include its matched non-cancer control group, focus on sleep in allogeneic HSCT candidates, and inclusion of a pre-transplant evaluation (an understudied point in the transplant process). Limitations include the modest sample size, homogeneity of the sample, cross-sectional design that precludes inference of directionality, and use of a self-report measure of insomnia. The current findings indicate the importance of developing interventions to enhance HSCT candidates' coping skills pre-transplant. Such efforts may draw from cognitive behavioral therapy for insomnia, an evidence-based approach for treating insomnia that incorporates coping skills training in the form of relaxation training and cognitive therapy [10]. Future studies should examine whether the observed associations extend to the peri- and post-transplant periods and whether they are found using objective measures of sleep/wake activity.
Key Points.
HSCT candidates are at risk for insomnia; coping and perceived stress may be contributing factors.
This study examined relationships among coping, perceived stress, and insomnia in HSCT candidates.
HSCT candidates (n=114) and controls (n=86) completed self-report questionnaires including measures of insomnia, approach and avoidance coping, and perceived stress.
Mean ISI scores and rates of clinically significant insomnia were higher in HSCT candidates. Avoidance coping was associated with patients' insomnia, mediated by perceived stress.
Findings suggest insomnia affects many HSCT candidates before transplant and reveal a pathway from avoidance coping to greater perceived stress to greater insomnia severity.
Acknowledgments
Funding: NCI K07-CA138499, P30-CA076292
Footnotes
Conflicts of interest: None
References
- 1.Fife B, Fausel C. Hematopoietic dyscrasias and stem cell/bone marrow transplantation. In: Holland J, Breitbart W, Jacobsen P, Lederberg M, Loscalzo M, McCorkle R, editors. Psycho-Oncology. 2nd. New York, NY: Oxford University Press; 2010. pp. 191–195. [Google Scholar]
- 2.Drake C, Roehrs T, Roth T. Insomnia causes, consequences, and therapeutics: An overview. Depression and Anxiety. 2003;18:163–176. doi: 10.1002/da.10151. [DOI] [PubMed] [Google Scholar]
- 3.Lazarus R, Folkman S. Stress, Appraisal, & Coping. New York, NY: Springer; 1984. [Google Scholar]
- 4.Jim H, Evans B, Jeong J, et al. Sleep disruption in hematopoietic cell transplantation recipients: Prevalence, severity, and clinical management. Biology of Blood and Marrow Transplantation. 2014;20:1465–1484. doi: 10.1016/j.bbmt.2014.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morin C. Insomnia: Psychological Assessment and Management. New York, NY: Guilford Press; 1993. [Google Scholar]
- 6.Savard M, Savard J, Simard S, Ivers H. Empirical validation of the Insomnia Severity Index in cancer patients. Psycho-Oncology. 2005;14:429–441. doi: 10.1002/pon.860. [DOI] [PubMed] [Google Scholar]
- 7.Moos R. Coping Responses Inventory. Odessa, FL: Psychological Assessment Resources; 1993. [Google Scholar]
- 8.Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. 1st. Newbury Park, CA: Sage; pp. 1998pp. 31–67. [Google Scholar]
- 9.Penley J, Tomaka J, Wiebe J. The association of coping to physical and psychological health outcomes: A meta-analytic review. Journal of Behavioral Medicine. 2002;25:551–603. doi: 10.1023/A:1020641400589. [DOI] [PubMed] [Google Scholar]
- 10.Edinger J, Carney C. Overcoming Insomnia: A Cognitive-Behavioral Therapy Approach, Therapist Guide. 2nd. New York, NY: Oxford University Press; 2014. [Google Scholar]