Abstract
Background
Non-adherence and medication error both limit the effectiveness of oral chemotherapy. The overlap between non-adherence and medication error is not well studied in children, and interventions strategies differ for each. Our objective was to describe non-adherence and errors in children with cancer to inform future interventions.
Methods
Non-adherence was measured using two self-report tools. Medication error was measured using medication review and observation of administration at home. Two clinicians made judgments about whether each error also represented an episode of non-adherence.
Results
Of 72 errors detected in 92 home visits, 27 were also instances of non-adherence. For example, parents gave a child 1 tablet of mercaptopurine every day rather than the prescribed 1 tablet 5 days a week and ½ tablet on weekends. Clinician reviewers judged that family interventions and health system interventions would be most effective in preventing the errors and non-adherence identified in this population of children with cancer.
Discussion
The relationship between medication errors and non-adherence is not well described in the literature. Our data indicate that medication error and non-adherence co-exist in the same population and in the same patient. Interventions should address both to most effectively support self-management.
Keywords: Chemotherapy, children, drug therapy, Leukemia, Lymphoma, Oral chemotherapy, medication error, adherence
Background
Over twenty five million doses of oral chemotherapy are taken annually in the United States, and the development of new oral chemotherapeutic agents is accelerating.1, 2 With the move to oral chemotherapy, cancer care is shifting from the inpatient setting, in the hands of doctors and nurses, to the home setting. Therefore, patients and their families increasingly bear the responsibility of using the right dose of the right medication at the right time. While the advent of oral chemotherapies has reduced the disruption treatment causes for patients and families, this shift places the significant burden of medication management squarely on the family. Notably, a recent National Comprehensive Cancer Network Task Force Report cited medication errors and non-adherence as emerging problems with oral chemotherapy use.1
While there is a body of literature about non-adherence to medications at home, less is known about errors at home.3 Medication non-adherence is “the extent to which a person’s behavior in taking medications coincides with medical or health advice”.4 For example, patients can simple forget to take a dose of their medication, or they may take it outside of the prescribed time frame. Non-adherence to oral chemotherapy is common in children with cancer; one in four children with leukemia take less than 75% of their mercaptopurine doses.5 A medication error is “any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient or consumer”.6 For example, patients may misunderstand instructions and fail to increase the dose of chemotherapy, or measure the wrong amount of liquid medications, or take medications for the wrong frequency or duration. Although there is less evidence, errors in oral chemotherapy use also appear to be common and dangerous.2, 7 Four percent of outpatient children with cancer experience an injury due to a medication error and an additional 30% have a dangerous error.8 The concepts of medication error in the ambulatory setting and non-adherence overlap.9
The relationship between error and non-adherence has not been well described in patients with cancer; there have been a few studies in other populations. In a survey of adults taking antiretrovirals for HIV, 25% reported non-adherence and 54% reported error; poor adherence and error were both associated with higher viral load.10 In a survey of adults on warfarin, 29% reported non-adherence and 50% reported error. Non-adherent patients were significantly more likely to have low International Normalized Ratios (INRs). Patients with good adherence who had errors were significantly more likely to have either low or high INRs, depending on the type of error.11 In diabetic patients, 7% of hospital admissions were related to overuse, underuse, or inappropriate use of a medication. More than half of these (64%) were medication errors with unintentional overdoses causing hypoglycemia.12 In order to understand whether human error theory could explain nonadherence, Barber et. al. telephoned 87 patients aged 75 years and older and identified 42 who were non-adherent, including 11 who were intentionally non-adherent.13 The remaining 31 reported slips and lapses, rule violations, and mistakes (wrong plans), consistent with Reason’s classification of errors: both active (unsafe acts/omissions with immediate adverse consequences) and latent (fallible decisions or the conditions in which errors occur).14
Children are at high risk for medication errors due to several factors including weight-based dosing,15 the use of liquid medications,16, 17 the need to cut or crush tablets,7 and the administration of medications by a parent or other caregiver who may be under increased stress due to the chronic illness of the child.16 Given the complexity of oral chemotherapy use, some non-adherence is likely unintentional and due to error.1 Language or health literacy problems have been shown to increase risk for both errors and non-adherence.18 These parameters are poorly understood and how they interact has not been systematically studied. Thus, the potential for interventions to reduce errors and non-adherence cannot be fully appreciated.
Very different approaches may reduce the risk of unintended error or intended non-adherence. Interventions to improve adherence generally focus on patient education and behavior. Interventions to prevent errors reduce the complexity of the human-healthcare system interaction, for example by streamlining bottle labels and storage.19 Used together, multifaceted interventions involving the entire system within which both errors and non-adherence occur may be very powerful, especially in highly complex regimens like leukemia treatment. In a first step toward such an approach, our objective for this paper was to describe the overlap of medication nonadherence and errors in children with cancer.
Methods
We performed an analysis of data on nonadherence and medication error collected during 92 home visits to children with cancer.7
Study subjects and sites
We analyzed home visits to children with cancer taking daily medications at home from three sites in Massachusetts and Georgia. Recruitment and home visits are described in detail elsewhere.3 Briefly, children under the age of 21 on daily home medications for the treatment of cancer and their families were recruited from pediatric clinics at three academic health centers.
Detection of medication errors
A trained research nurse visited children at home, reviewed medications, and directly observed medication administration for errors, using a previously validated method.3, 7 The nurse recorded detailed information about each potential error, following established methods.20, 21 Two physicians, including one pediatric oncologist, reviewed and coded each event as an error or not and for those events coded as errors the severity of the error. Reliability between coders was near perfect for errors (Kappa = 0.94) and good for severity (Kappa = 0.71) respectively.13
Detection of non-adherence
We used two self-report measures of adherence: a 4-item medication adherence scale and a question during review of each medication which was not an “as needed” (prn) medication about adherence in the last seven days. The 4-item medication adherence scale asked about missed doses and altering the dose of medications (Cronbach’s alpha 0.78).22 Each item had a 5-point Likert scale response, such that 20 was a score indicating perfect adherence. In addition, for each medication reviewed (excluding as needed or prn medications), we asked parents “How many times in the last 7 days did you miss a dose of this medication?”. Adolescent patients responsible for administering their own medication reported their adherence; for the remaining participants, parents answered the questions.
Analysis
Two pediatric clinicians, one expert in medication errors (KW) and another in medication adherence (AP), read each of the original error descriptions and made independent judgments about whether it was also non-adherence. Disagreements between reviewers were resolved through discussion and consensus. Agreement between reviewers was good (74%). The two clinicians also judged whether the event could be avoided by individual, family, community, or health system interventions.
Results
Rates of non-adherence
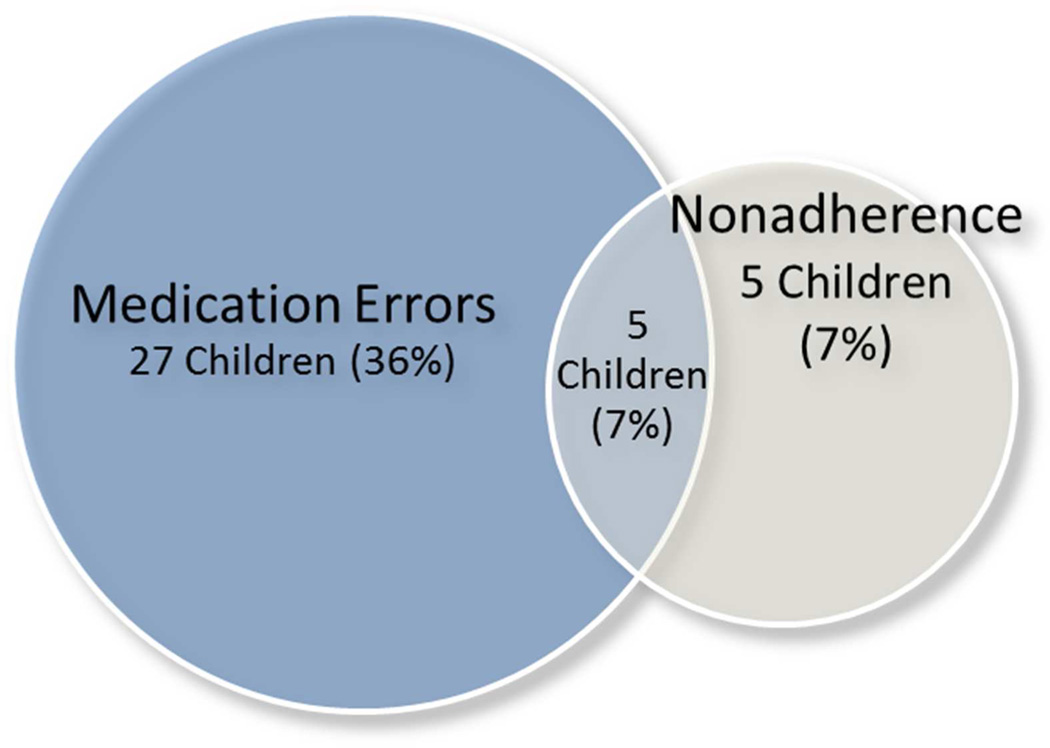
Using the medication adherence scale, 16 (17%) of the 92 parents reported non-adherence: 12 strongly agreed or agreed that they sometimes forget the child’s medications and two additional parents agreed that they sometimes altering the dose of the child’s medications. (Table 1) Seventy seven of the 92 parents were asked, for each medication, how many doses were missed in the last seven days; we did not ask this question in the initial fifteen home visits. Ten parents (13%) reported non-adherence in the seven days before the home visit. These same 77 families had 32 medication errors identified during home visits, including five which were related to poor adherence. (Figure 1)
Table 1.
Rates of non-adherence and error among patients with cancer
| N respondents |
N | Example | |
|---|---|---|---|
| Self-report nonadherence | 92 | 16 | Strongly agree or agree sometimes forget medicine |
| Reported missed dose in last 7 days for any medicine |
77 | 10 | Missed both morning trimethoprim- sulfamethoxazole doses over the weekend |
| Medication error | 92 | 72 | Methotrexate bottle labeled take daily rather than once a week |
| Medication error and also an error | 92 | 27 | A child who was supposed to take mercaptopurine 1 tablet Monday to Friday and ½ tablet Saturday and Sunday. The parent did not understand this and gave the child 1 tablet every day. |
Figure 1.
Medication errors detected during home visits and parent reported non-adherence in the last seven days among 77 children with cancer who answered questions about missed doses for each medication in the last 7 days.
Errors which are also non-adherence
Among all 92 children with cancer we visited, we identified 27 errors of the 72 total number of errors) which clinician reviewers judged were also non-adherence. An example of an error which was also considered non-adherence is a child who was supposed to take mercaptopurine 1 tablet Monday to Saturday and ½ tablet Sunday. The parent did not understand this and gave the child 1 tablet every day. In another example an adolescent reports that she sometimes falls asleep before taking her evening medications, including mercaptopurine; her parents work nights. An example of an error that was not considered to be non-adherence was a methotrexate bottle label which instructs to give methotrexate once daily rather than once a week. Of those errors which were also non-adherence, clinicians reviewers judged that 15 (56%) could be prevented by interventions focusing on the individual patient, all (100%) by family interventions, 3 (11%) by community interventions, and 20 (74%) by health system interventions. (Table 2)
Table 2.
Interventions which reviewers judged would prevent non-adherence and error
| Intervention | Example | Prevent error N (%) |
Prevent error that is also non-adherence N (%) |
|---|---|---|---|
| Individual | Improve storage of medications and proper equipment |
11 (30%) | 15 (56%) |
| Family | Improved communication about dose changes between family members |
22 (65%) | 27 (100%) |
| Community | Identification of community supports families can leverage for transportation, pharmacy pickup |
3 (8%) | 3 (11%) |
| Health system | Rapid cycle series of interventions to achieve 100% parents measuring correct chemotherapy dose 100% of the time, based in human error theory |
34 (92%) | 20 (74%) |
DISCUSSION
Our data indicate that errors and non-adherence can coexist in the same population, in the same clinical setting, and in the same patient. While errors and non-adherence did overlap in our data, some errors were not cases of non-adherence and some non-adherence were not an error. This indicates that interventions to improve oral chemotherapy use should target both in order to deal with all problems that occur. While the individual, family, community, and health system are all key facets for effective self-management, our clinician reviewers judged that family and health services interventions are most likely to reduce errors and non-adherence in children with cancer.
Literature in adult patients indicates that error and non-adherence can have independent and different impacts on clinical outcomes, and that the interaction between error and non-adherence can change clinical outcomes. Many of the studies we found in adult patients combined errors and non-adherence together as “drug-related problems”; this approach makes it difficult to identify different causes, effects, and interventions for each.12, 23, 24 However, the interaction between error and non-adherence in individual patients can change the type of adverse outcomes seen. For example, adult patients on warfarin experienced under coagulation with non-adherence but over-coagulation or under-coagulation with adherence and error.11 It is important to consider the clinical impact of these complex relationships in developing and testing interventions. It seems likely that non-adherence and error may similarly overlap in adult cancer patients; studies indicate that nonadherence to oral chemotherapy is similarly problematic in adults.25, 26 We found no studies examining both nonadherence and error in adult oncology patients.
We are aware of only two pediatric papers which examined non-adherence and medication error. Bokhour interviewed 37 parents of children with asthma and 12 reported “nonconcordance” with provider recommended controller medication regimens.27 Parents described three types of nonconcordance: unintentional, where the parent thought (s)he was correctly following the medication instructions but was not; unplanned, where the parent planned to follow the medication instructions but was not able to; and intentional, whether the parent did not plan to follow the medication instructions. In the second pediatric study, Freedman described adherence and the proportion of doses taken on schedule in children with glaucoma. Parents reported giving 43–107% of doses and a median of 47% of doses were taken on schedule.28 Both missed doses and doses not taken on schedule were significantly associated with low health literacy.
We are aware of no previous studies that examine both medication error and non-adherence in cancer patients. While some information from studies of adults may be applicable to children, pediatric medication use is more complex than adults. Pediatric home cancer care is highly complex: chemotherapy doses change from day to day, regimens change frequently in response to clinical change, children take a median of 10 different medications, and can take up 20 pills of a single medication type.7 Non-adherence to chemotherapy in children is associated with significant increases in risk of relapse.5
Because some patients experience error, others experience non-adherence, and some experience both, interventions which only target one will likely be suboptimal. Similarly, pediatric oncologists seeking to understand how oral chemotherapy is used at home should ask about missed doses, accidental overdoses, and exactly what dose is being administered at home. In a system as highly complex as oral chemotherapy use prevention of both non-adherence and error is essential.
Our data indicate that interventions targeting family and health system factors may be effective as many of errors identified are related to these factors. It may be informative to adapt some of the interventions employed in hospitals to prevent error to the home setting using a human factors approach, such as reduction in complexity or safer storage of medications.29, 30 Human factors research examines all factors that can influence human behavior and their interaction with external systems in order to optimize that interaction and/or improve health and safety.31 The use of human factors approaches can provide an understanding of the dynamics and behaviors involved in family/health services interactions. While this approach has been utilized in the healthcare setting, particularly in inpatient areas, extending this approach to home medication use is needed.32
While our study is one of the first to investigate non-adherence and error together, some limitations should be considered when interpreting the results. First, measures of non-adherence were limited to self-report. While self-report measures correlate with more objective measures of non-adherence (i.e., electronic monitoring), they do underestimate the problem.33 Second, we were unable, in our home visit study, to evaluate the impact of non-adherence and error on the effectiveness of the child’s cancer treatment. A previous study indicates that non-adherence is associated with increased risk of relapse.5 Finally, due to the home visit nature of the study, despite the fact that our study occurred at three different academic health centers in two states, our sample size was relatively small; a larger study is needed to adequately understand these relationships and inform intervention development.
CONCLUSION
Our data indicate that non-adherence and error coexist in children with cancer. There are few studies which consider error and non-adherence together, including only two in children and none in oncology. Clinicians and researchers wishing to improve oral chemotherapy use in children should address both error and non-adherence. A comprehensive approach that includes adherence and medication errors in measurement and interventions designed with an understanding of family-to-family and family-to-health system interactions may be both powerful and clinically valid.
Acknowledgments
Funding: Dr. Walsh was supported by a Robert Wood Johnson Physician Faculty Scholars award. This work was also supported by the Charles H. Hood Foundation and the National Cancer Institute (CRN U19 CA 79689).
Footnotes
Conflict of interest: None of the authors have conflicts of interest
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose
References
- 1.Weingart S, Brown E, Bach P, et al. NCCN Task Force Report: Oral Chemotherapy. J Natl Compr Canc Netw. 2008;6(Suppl 3):S1–S14. [PubMed] [Google Scholar]
- 2.Weingart SN, Toro J, Spencer J, et al. Medication Errors Involving Oral Chemotherapy. Cancer. 2010;116:2455–2464. doi: 10.1002/cncr.25027. [DOI] [PubMed] [Google Scholar]
- 3.Walsh KE, Stille CJ, Mazor KM, Gurwitz JH. Using home visits to understand medication errors in children. Vol. 4. Technology and Medication Safety. Agency for Healthcare Research and Qaulity; 2008. Aug, [PubMed] [Google Scholar]
- 4.Haynes RB. Introduction. In: Haynes RB, Taylor DW, Sackett DL, editors. Compliance in Health Care. Baltimore, MD: Johns Hopkins University Press; 1979. pp. 1–7. [Google Scholar]
- 5.Bhatia S, Landier W, Shangguan M, et al. Nonadherence to Oral Mercaptopurine and Risk of Relapse in Hispanic and Non-Hispanic White Children With Acute Lymphoblastic Leukemia: A Report From the Children’s Oncology Group. Journal of Clinical Oncology. 2012;30(17):2094–2101. doi: 10.1200/JCO.2011.38.9924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glascoe FP, Oberklaid F, Dworkin PH, Trimm F. Brief approaches to educating patients and parents in primary care. Pediatrics. 1998;101(6):E10. doi: 10.1542/peds.101.6.e10. [DOI] [PubMed] [Google Scholar]
- 7.Walsh KE, Dodd KS, Seetharaman K, et al. Medication Errors among Adults and Children with Cancer in the Outpatient Setting. Journal of Clinical Oncology. 2009;6:891–896. doi: 10.1200/JCO.2008.18.6072. [DOI] [PubMed] [Google Scholar]
- 8.KE W, DW R, SN W, et al. Medication Errors in the Home: A Multisite Study of Children With Cancer. Pediatrics. 2013;131:e1405. doi: 10.1542/peds.2012-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor JA, Winter L, Geyer LJ, Hawkins DS. Oral outpatient chemotherapy medication errors in children with acute lymphoblastic leukemia. Cancer. 2006;107(6):1400–1406. doi: 10.1002/cncr.22131. [DOI] [PubMed] [Google Scholar]
- 10.Bangsberg DR, Bronstone A, Hofmann R. A computer-based assessment detects regimen misunderstandings and nonadherence for patients on HIV antiretroviral therapy. Aids Care. 2002;14(1):3–15. doi: 10.1080/09540120220097892. [DOI] [PubMed] [Google Scholar]
- 11.Schillinger D, Wang F, Rodriguez M, Bindman A, Machtinger EL. The Importance of Establishing Regimen Concordance in Preventing Medication Errors in Anticoagulant Care. Journal of Health Communication. 2006;11:555–567. doi: 10.1080/10810730600829874. [DOI] [PubMed] [Google Scholar]
- 12.Claydon-Platt K, Manias E, Dunning T. Medication-related problems occurring in people with diabetes during an admission to an adult teaching hospital: A retrospective cohort study. Diabetes Research and Clinical Practice. 2012;97:223–230. doi: 10.1016/j.diabres.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 13.Barber N, Safdar A, Franklin BD. Can human error theory explain non-adherence? Pharm World Sci. 2005;27:300–304. doi: 10.1007/s11096-005-0355-7. [DOI] [PubMed] [Google Scholar]
- 14.Reason J. Understanding adverse events: human factors. Quality in Health Care. 1995;4(2):80–89. doi: 10.1136/qshc.4.2.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. Jama. 2001;285(16):2114–2120. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- 16.Frush KS, Luo X, Hutchinson P, Higgins JN. Evaluation of a method to reduce over-the-counter medication dosing error. Arch Pediatr Adolesc Med. 2004;158(7):620–624. doi: 10.1001/archpedi.158.7.620. [DOI] [PubMed] [Google Scholar]
- 17.McMahon SR, Rimsza ME, Bay RC. Parents can dose liquid medication accurately. Pediatrics. 1997;100(3 Pt 1):330–333. doi: 10.1542/peds.100.3.330. [DOI] [PubMed] [Google Scholar]
- 18.Yin HS, Dreyer BP, Foltin G, van Schaick L, Mendelsohn AL. Association of low caregiver health literacy with reported use of nonstandardized dosing instruments and lack of knowledge of weight-based dosing. Ambul Pediatr. 2007;7(4):292–298. doi: 10.1016/j.ambp.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Reason J. Human error: models and management. Bmj. 2000;320(7237):768–770. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leape LL, Bates DW, Cullen DJ, et al. Systems analysis of adverse drug events. ADE Prevention Study Group. Jama. 1995;274(1):35–43. [PubMed] [Google Scholar]
- 21.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351(18):1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 22.Conn KM, Halterman JH, Fisher SG, Yoos HL, Chil NP, Szilagyi PG. Parental beliefs about medications and medication adherence among urban chidlren with asthma. Ambul Pediatr. 2005;2005(5):306–310. doi: 10.1367/A05-004R1.1. [DOI] [PubMed] [Google Scholar]
- 23.Ernst ME, Iyer SS, Doucette WR. Drug-Related Problems and Quality of Life in Arthritis and Low Back Pain Sufferers. Value in Health. 2003;6(1):51–58. doi: 10.1046/j.1524-4733.2003.00202.x. [DOI] [PubMed] [Google Scholar]
- 24.Viktil KK, Blix HS, Moger TA, Reikvam A. Interview of patients by pharmacists contributes significantly to the identification of drug-related problems (DRPs) Pharmacoepidemiol Drug Saf. 2006;15:667–674. doi: 10.1002/pds.1238. [DOI] [PubMed] [Google Scholar]
- 25.Thivat E, Praagh IV, Belliere A, et al. Adherence with Oral Oncologic Treatment in Cancer Patients: Interest of an Adherence Score of All Dosing Errors. Oncology. 2013;84:67–74. doi: 10.1159/000342087. [DOI] [PubMed] [Google Scholar]
- 26.Partridge AH, Avorn J, Wang PS, Winer EP. Adherence to Therapy With Oral Antineoplastic Agents. Journal of the National Cancer Institute. 2002;94:652–661. doi: 10.1093/jnci/94.9.652. [DOI] [PubMed] [Google Scholar]
- 27.Bokhour BG, Cohn ES, Cortés DE, et al. Patterns of concordance and non-concordance with clinician recommendations and parents’ explanatory models in children with asthma. Patient Educ Couns. 2008;70(3):376–385. doi: 10.1016/j.pec.2007.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Freedman RB, Jones SK, Lin A, Robin AL, Muir KW. Influence of Parental Health Literacy and Dosing Responsibility on Pediatric Glaucoma Medication Adherence. Arch Ophthalmol. 2012;130(3):306–311. doi: 10.1001/archopthalmol.2011.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carayon P, TB W, Rivera-Rodriguez AJ, et al. Human factors systems approach to healthcare quality and patient safety. Applied ergonomics. 2014;45(1):14–25. doi: 10.1016/j.apergo.2013.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zayas-Caban T, Valdez RS. Human Factors and Ergonomics in Home Care. In: Carayon P, editor. Handbook of human factors and ergonomics in health care and patient safety. CRC Press; 2011. [Google Scholar]
- 31.Definition and Domains of Ergonomics. [Accessed May 17, 2016];Ergonomics human centered design. 2016 http://www.iea.cc/whats/index.html.
- 32.Gawron VJ, Drury CG, Fairbanks RJ, Berger RC. Medical error and human factors engineering: Where are we now? American Journal of Medical Quality. 2006;21(1):57–67. doi: 10.1177/1062860605283932. [DOI] [PubMed] [Google Scholar]
- 33.LO TB. Adherence to Medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]