Abstract
The dyad of hypertension and coronary artery disease is prevalent; however, data regarding systolic blood pressure control and long-term all-cause mortality are lacking. Using extended follow-up data from the United States cohort of the INternational VErapamil/Trandolapril STudy (mean 11.6 years), subjects were categorized by age at enrollment (50–<60 and ≥60 years). Cox proportional adjusted hazard ratios were constructed for time to all-cause mortality according to achieved mean systolic blood pressure. In those 50–<60 years and using a referent systolic blood pressure < 130 mm Hg, an achieved systolic blood pressure 130–140 mm Hg was associated with a similar risk of mortality (hazard ratio 1.03, 95% confidence interval 0.87–1.23), while an achieved systolic blood pressure ≥ 140 mm Hg was associated with an increased risk of mortality (hazard ratio 1.80, 95% confidence interval 1.53–2.11). Among subjects ≥60 years and using a referent systolic blood pressure < 130 mm Hg, an achieved systolic blood pressure 130–140 mm Hg was associated with a lower risk of mortality (hazard ratio 0.92, 95% confidence interval 0.85–0.98). There was an increased risk of mortality with an achieved systolic blood pressure ≥150 mm Hg (hazard ratio 1.34, 95% confidence interval 1.23–1.45), but with an achieved systolic blood pressure 140–150 mm Hg (hazard ratio 1.02, 95% confidence interval 0.94–1.11). In hypertensive patients with coronary artery disease, achieving a systolic blood pressure 130–140 mm Hg appears to be associated with lower all-cause mortality after about 11.6 years follow-up.
Keywords: adults, coronary artery disease, hypertension, mortality, systolic blood pressure
In the United States (US), it is estimated that one in every three adults has hypertension (HTN).1 HTN is an established independent risk factor for coronary artery disease (CAD) irrespective of age or sex.2 Medicare data indicates that the dyad of HTN and CAD is the most prevalent chronic disease dyad among adults.1 The former members of the Eighth Joint National Committee Panel (JNC-8) recommended pharmacological antihypertensive therapy for a target therapeutic goal <150 mm Hg for adults ≥60 years, and <140 mm Hg in those <60 years.3 These recommendations are inconsistent with the different society guidelines including: the 2013 European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC), the 2014 American Society of Hypertension (ASH) and the International Society of Hypertension (ISH), and the 2015 American Heart Association (AHA)/American College of Cardiology (ACC)/ASH updated statement for the management of HTN in patients with CAD which recommended a target therapeutic goal <140 mm Hg in hypertensive patients with CAD.2,4,5 Furthermore, in the 2015 AHA/ACC/ASH statement, the authors acknowledged that the optimal systolic blood pressure (SBP) in relation to long-term mortality are lacking among this cohort of high-risk patients.2 More recently, the Systolic Blood Pressure Intervention Trial (SPRINT) found that a goal SBP < 120 mm Hg was superior to < 140 mm Hg among subjects ≥ 60 years with high cardiovascular risk, many of whom had CAD, however; details of this CAD cohort were not provided.6 Accordingly, additional information on long-term all-cause mortality according to early achieved SBP in hypertensive CAD patients would be useful. Using the extended follow-up data from the US cohort of the INternational VErapamil/Trandolapril STudy (INVEST) study, we aimed to address this knowledge gap.
Methods
Study design and outcome assessed
Briefly, the INVEST was a prospective multi-center randomized trial comparing clinical outcomes for 22,576 patients ≥ 50 years of age with CAD and HTN assigned to either a beta-blocker/hydrochlorothiazide or a calcium antagonist/angiotensin converting enzyme inhibitor strategy.7 After active study follow-up (mean 2.7 years).8 Subjects were informed of these findings and then were treated with open-label medications according to provider discretion. The trial was initially designed such that an extended follow-up for the US cohort could be evaluated. In addition, the project was planned with sufficient power to analyze the US cohort separately. The inclusion and exclusion criteria, study design, and results have been previously reported. Institutional review boards and ethics committees at each site approved the protocol, which was conducted in accordance with the principles outlined in the Declaration of Helsinki. Data were collected through an internet-based system, which provided for individualized prescribing of antihypertensive medications using a flexible treatment algorithm, and express mail delivery. The primary outcome of INVEST was the first occurrence of all-cause mortality, non-fatal myocardial infarction (MI), or non-fatal stroke, while the secondary outcomes were each outcome individually. Both strategies were equivalent in terms of prevention of adverse outcomes with excellent BP control (>71% <140/90 mm Hg).8,9
The current study is a long-term observational analysis of the US cohort of INVEST. For the purpose of this analysis we combined the treatment strategies. Data regarding long-term all-cause mortality, for subjects enrolled from a US site, were assessed by searching the US National Death Index (NDI) up to 11 years after INVEST follow-up was completed. The NDI has been previously shown to be reliable in detecting alive and dead subjects.10 To be considered a confirmed death, 4 of 5 matches among the following were required: name, Social Security number, date of birth, city, and state.8 Subjects were categorized according to age at enrollment (50-<60 and ≥60 years), then were further divided according to achieved mean SBP during the study follow-up: SBP <130, 130 to <140, and ≥140 mm Hg in those 50–60 years, and SBP <130, 130 to <140, 140 to <150, and ≥150 mm Hg in those ≥60 years..3,8 Since we aimed to test the two different SBP targets recommended by both the former members of the JNC-8 panel and the other society recommendations,2–5 we categorized the subjects ≥60 years in multiple groups to reflect these targets.
Statistical analysis
The baseline characteristics in each group were compared with chi-square test for categorical variables and analysis of variance for continuous variables. The average SBP was calculated for each subject using all measurements (except the baseline measurement) until the visit before the subject experienced one of the components of the primary outcome or was censored. Patients who did not appear in the National Death Index were censored on the day the death index search was completed. Cox proportional hazard ratios (HR) were constructed for time to all-cause mortality according to achieved mean SBP during study follow-up: SBP <130 mm Hg (group 1) (referent group), 130 to <140 mm Hg (group 2), and ≥140 mm Hg (group 3) in those 50– <60 years, and SBP <130 mm Hg (group 4) (referent group), 130 to <140 mm Hg (group 5), 140 to <150 mm Hg (group 6), and ≥150 mm Hg (group 7) in those ≥60 years.. All cox regression analyses adjusted for covariates such as age, gender, race and history of myocardial infarction, history of stoke/transient ischemic stroke, heart failure, renal insufficiency, and diabetes. Multivariate analysis was conducted comparing these groups. A secondary analysis for all-cause mortality was performed for SBP as a continuous variable, with a SBP and age interaction, as well as the quadratic term for age to evaluate the nonlinear relationship of age and outcome. All P-values were 2-tailed, with statistical significance set at 0.05. All analyses were performed with SAS 9.3 (SAS Institute, Cary, North Carolina).
Results
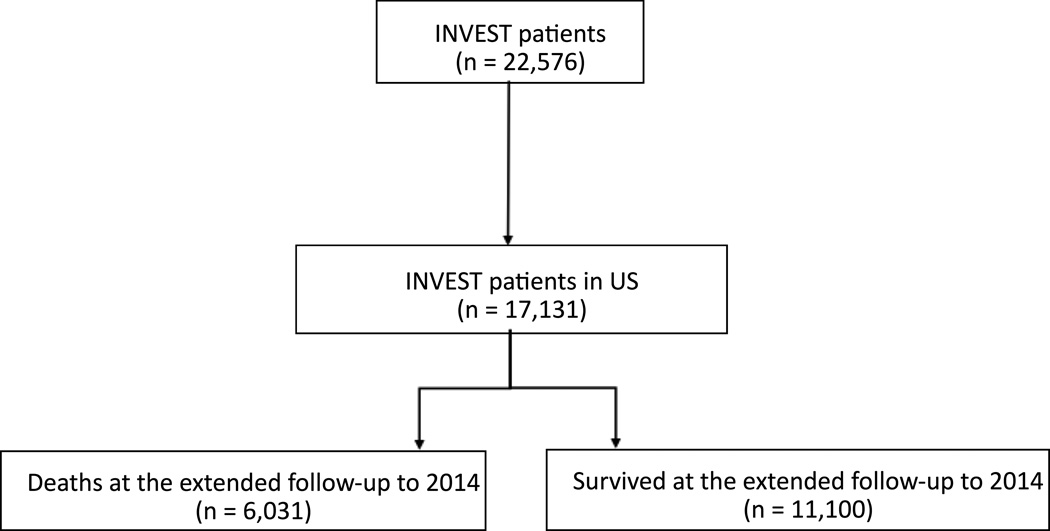
Among all participants, 17,131 patients were recruited from the US (Figure 1). Among those aged 50–<60 years; 1,942 patients (11.3 %) achieved SBP of <130 mm Hg (group 1), 1,636 patients (9.6%) achieved SBP ≥130 to 140 mm Hg (group 2), while 1,460 patients (8.5 %) achieved on-treatment SBP of ≥140 mm Hg (group 3) by the end of study follow-up. Among those aged ≥60 years; 3,832 patients (22.4 %) achieved on-treatment SBP of <130 mm Hg (group 4), 4,014 patients (24.4 %) achieved SBP of ≥130 to 140 mm Hg (group 5), 2,398 patients (14.0 %) achieved SBP ≥140 to 150 mm Hg (group 6), and 1,849 patients (10.8 %) achieved SBP of ≥ 150 mm Hg (group 7). The mean age at enrollment was 66 years and 54% were female. Baseline characteristics of the different groups were summarized in the Table. The mean follow-up duration was 11.6 years with a total of 198,352 patient-years. There were 6,031 deaths (35.2%) during the extended follow-up period (Figure 1).
Figure 1.
Patient flow diagram
Table.
Baseline characteristic of the United States cohort according to age at enrolment and achieved systolic blood pressure
| Characteristic | 50–<60 years | ≥60 years | All n=17,131 |
P-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Group 1 (<130 mmHg) (n=1,942) |
Group 2 (130– 140mmHg) (n=1,636) |
Group 3 (≥140 mmHg) (n=1,460) |
Group 4 (<130 mmHg) (n=3,832) |
Group 5 (130–140 mmHg) (n=4,014) |
Group 6 (140– 150mmHg) (n=2,398) |
Group 7 (≥150mmHg) (n=1,849) |
|||
| Age, years | 54.4±2.9 | 54.5±3.0 | 54.5±2.8 | 70.6±7.5 | 71.2±7.3 | 71.5±7.3 | 72.1±7.7 | 66.3±10.0 | <0.0001 |
| Female | 52.9 | 52.9 | 52.2 | 50.4 | 53.8 | 55.6 | 61.5 | 53.8 | <0.0001 |
| Ethnicity | |||||||||
| African American | 13.2 | 19.4 | 34.6 | 9.0 | 11.4 | 15.9 | 21.8 | 15.6 | <0.0001 |
| Hispanic | 51.0 | 41.0 | 28.6 | 45.2 | 34.6 | 25.3 | 23.4 | 36.4 | <0.0001 |
| White | 32.7 | 36.0 | 33.4 | 43.2 | 51.9 | 55.5 | 52.3 | 45.2 | <0.0001 |
| Blood pressure | |||||||||
| Systolic | 138.1±16.4 | 147.2±16.3 | 157.0±18.8 | 139.8±17.2 | 148.2±16.7 | 153.4±17.0 | 163.5±18.9 | 148.2±19.0 | <0.0001 |
| Diastolic | 85.6±10.1 | 89.1±10.1 | 92.5±11.4 | 81.7±10.4 | 83.3±10.4 | 83.8±10.7 | 86.0±11.6 | 84.9±11.1 | <0.0001 |
| Heart rate | 76.0±9.5 | 77.2±9.1 | 77.7±9.8 | 74.9±9.6 | 74.7±9.2 | 75.2±9.6 | 75.6±10.1 | 75.5±9.6 | <0.0001 |
| Medical history | |||||||||
| Diabetes Mellitus | 24.4 | 27.8 | 32.1 | 29.7 | 28.6 | 31.3 | 35.1 | 29.6 | <0.0001 |
| Hyperlipidemia | 53.7 | 53.6 | 50.9 | 55.8 | 57.0 | 58.3 | 57.2 | 55.7 | <0.0001 |
| Smoking (ever) | 47.2 | 47.9 | 49.7 | 45.2 | 41.4 | 43.3 | 42.8 | 44.7 | <0.0001 |
| Angina pectoris | 75.8 | 73.8 | 72.3 | 68.2 | 62.0 | 58.3 | 60.7 | 66.3 | <0.0001 |
| Unstable angina | 8.3 | 8.9 | 10.0 | 9.5 | 9.8 | 11.6 | 13.0 | 10.1 | <0.0001 |
| Myocardial infarction | 23.6 | 23.8 | 24.9 | 30.3 | 29.7 | 32.4 | 35.4 | 29.2 | <0.0001 |
| PCI or CABG | 21.5 | 22.4 | 24.5 | 29.3 | 33.4 | 34.5 | 32.9 | 29.4 | <0.0001 |
| Stroke or TIA | 3.8 | 5.2 | 5.8 | 8.2 | 8.3 | 8.6 | 10.4 | 7.5 | <0.0001 |
| Heart failure (NHYA class I-III) | 3.5 | 2.9 | 4.8 | 7.3 | 4.9 | 5.4 | 7.3 | 5.4 | <0.0001 |
| Renal impairment | 0.8 | 0.8 | 2.2 | 2.1 | 1.9 | 2.6 | 4.0 | 2.1 | <0.0001 |
| Medications | |||||||||
| Lipid lowering | 35.4 | 33.9 | 28.5 | 40.2 | 39.7 | 38.7 | 36.5 | 37.4 | <0.0001 |
| Nitrate | 32.8 | 31.4 | 23.2 | 34.2 | 29.1 | 29.0 | 27.9 | 30.2 | <0.0001 |
| Aspirin or other antiplatelet | 41.4 | 41.8 | 41.2 | 51.4 | 54.1 | 57.4 | 53.2 | 50.1 | <0.0001 |
| NSAIDs | 24.0 | 24.0 | 19.3 | 23.4 | 22.6 | 20.3 | 19.5 | 21.5 | 0.0001 |
Values are reported as mean ± standard deviation or percentages
CABG= coronary artery bypass surgery
NSAIDs= non-steroidal anti-inflammatory agents
PCI= percutaneous coronary intervention
TIA= transient ischemic attack
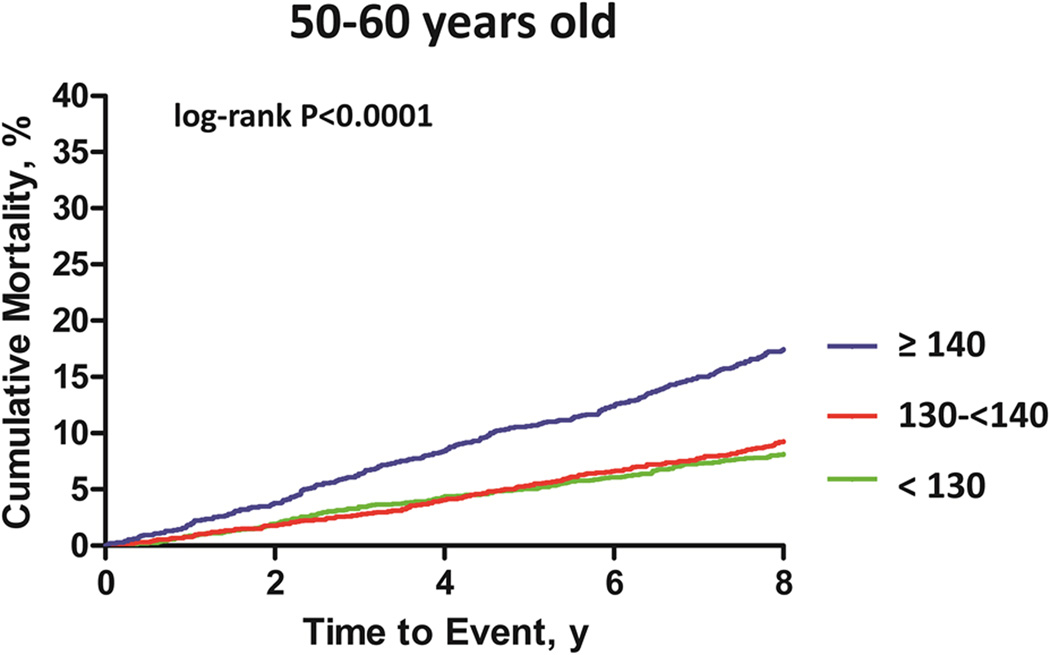
Consistent with our early findings, there was no difference in long-term all-cause mortality comparing the beta-blocker based regimen versus the calcium antagonist based strategy (P=0.73). There was an observed reduction in the slope of the all-cause mortality curve with either strategy around 9 years (Online Supplement). Among the subjects aged 50– <60 years, an achieved SBP ≥130 to 140 mm Hg (group 2) was associated with a similar risk of all-cause mortality (HR 1.03, 95% confidence interval [CI] 0.87–1.23, P=0.74), compared with an achieved SBP <130 mm Hg (group 1). An achieved SBP ≥140 mm Hg was associated with an increased risk of all-cause mortality (HR 1.80, 95% CI 1.53–2.11, P<0.0001), compared with compared with SBP <130 mm Hg (group 1) (Figure 2).
Figure 2.
Kaplan Meier curve for all-cause mortality in subjects aged 50– <60 years. The absolute percentage of deaths in Group 1 (Green line)=13.4%, Group 2 (Red line)=15.3%, Group 3 (Blue line)=28.0%.
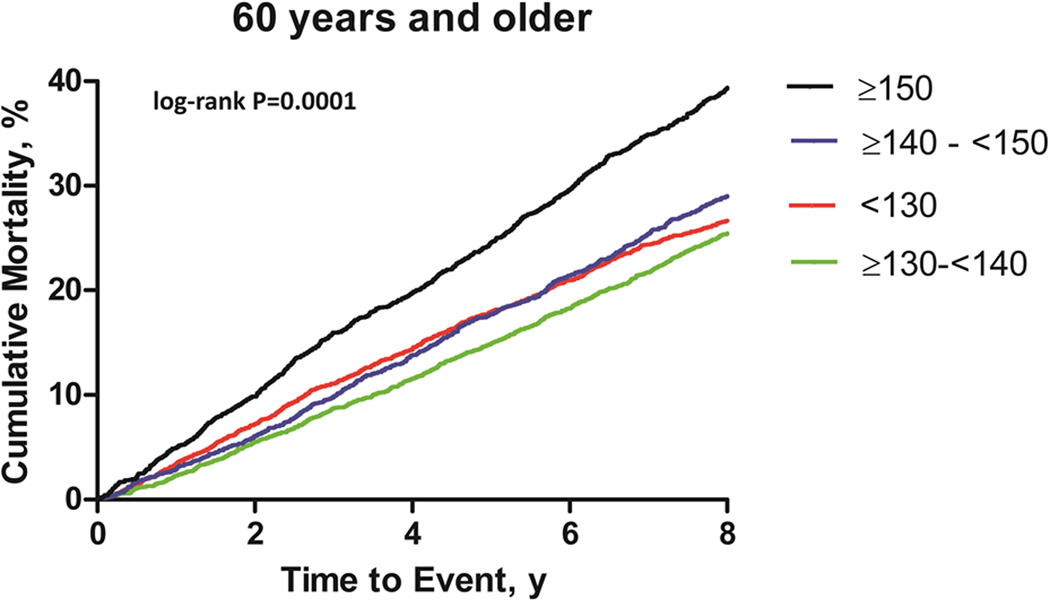
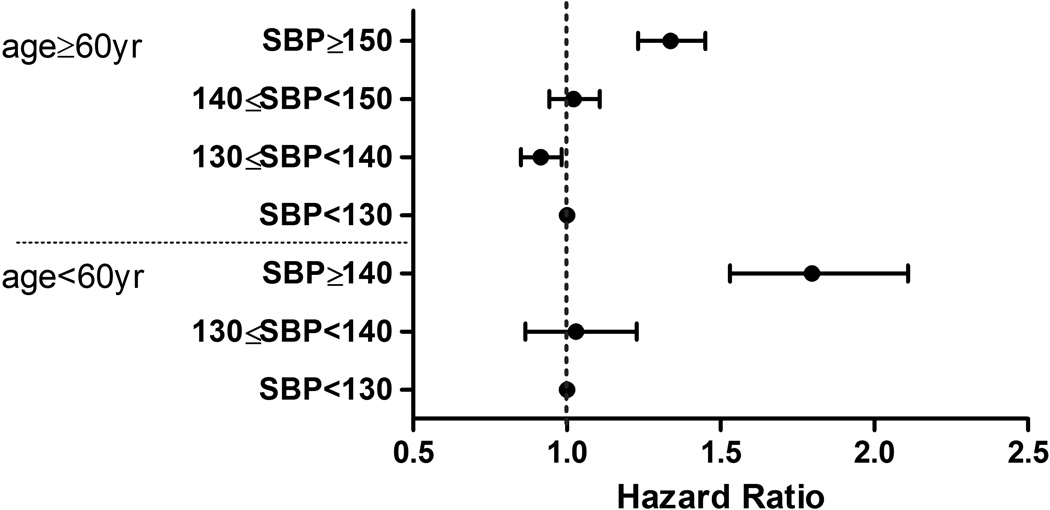
Among older subjects (≥60 years), using a referent group with achieved SBP <130 mm Hg (group 4), an achieved SBP ≥150 mm Hg (group 7) was associated with an increased risk of all-cause mortality (HR 1.34, 95% CI 1.23–1.45, P<0.0001), but no increased risk of all-cause mortality was observed with an achieved SBP of 140 to <150 mm Hg (group 6) (HR 1.02, 95% CI 0.94–1.11, P=0.59). An achieved SBP of 130 to <140 mm Hg (group 5) was associated with a lower risk of all-cause mortality (HR 0.92, 95% CI 0.85–0.98, P=0.01) when compared with an achieved SBP of <130 mm Hg (group 4) (Figure 3). Figure 4 summarizes the hazard ratios for all-cause mortality for the different groups. In a secondary analysis, using SBP as a continuous variable, every 1 mm Hg increase in SBP was associated with 1% increase in the hazard of all-cause mortality over 12 years (HR 1.01, 95% CI 1.008–1.011, P<0.0001). In addition, age had a different effect on mortality depending on the values of SBP.
Figure 3.
Kaplan Meier curve for all-cause mortality in subjects ≥60 years. The absolute percentage of deaths in Group 4 (Red line)=38.1%, Group 5 (Green line)=38.8%, Group 6 (Blue line)=45.0%, and Group 7 (Black)=55.1%.
Figure 4.
Hazard ratios for all-cause mortality in the different groups.
Discussion
To our knowledge, this is the first study to investigate the relationship between long-term all-cause mortality and achieved SBP among a cohort of hypertensive patients with documented CAD. With almost 200,000 person-years of follow-up, our large observational study showed that early treatment with a beta-blocker based or a calcium antagonist based BP lowering strategy that resulted in excellent BP control during the active study follow-up was associated with similar long-term benefit in terms of all-cause mortality. Furthermore, we observed that early intense treatment of hypertension in this high risk population appeared to attenuate the mortality-time curve with both strategies after about 9 years.. The Action in Diabetes and Vascular Disease (ADVANCE-ON) trial randomized hypertensive diabetic patients to either perindopril/indapamide versus placebo. Both arms had similar SBP at the conclusion of the initial follow-up period. At a median of 9.9 years, all-cause mortality was reduced in the group initially assigned to perindopril/indapamide (HR 0.91, 95% CI 0.85–0.99, P=0.03), despite the fact that participants in both groups returned to their usual care.11 Our results confirm those observations suggesting that the benefit of good BP control during the active phase of the trial persisted despite possible loss of the “excellent BP control”, and also extend those results to CAD patients. This suggests a possible “legacy effect”, which has been described in other areas of cardiovascular medicine such as with atorvastatin in hypertensive patients.12 A similar long term effect was demonstrated in patients with Type 2 Diabetes Mellitus (i.e., the United Kingdom Prospective Diabetes Study (UKPDS), and Veterans Affairs Diabetes Trial (VATS), in where an intensive glucose lowering strategy early during the active study period resulted in reduction in long-term mortality well after the active phase of the trial was completed.13,14
Our analysis suggests that an achieved SBP <140 mm Hg is associated with beneficial results in regards to long-term all-cause mortality among younger CAD patients (50– <60 years). Among older CAD patients (≥60 years), an achieved SBP of 130 to <140 mm Hg was associated with lower risk of all-cause mortality, when compared with those who achieved SBP targets 140 to <150 mm Hg, and SBP ≥150 mm Hg. These findings further support the viewpoint of some members of the former JNC-8 panel who disagreed with the 2014 recommendations to relax the goal SBP for management of HTN in adults.15 Data from the Northern Manhattan Study showed that raising the SBP threshold from 140 to 150 mm Hg as a new target for hypertension treatment in older individuals without diabetes or chronic kidney disease could have a detrimental effect on stroke risk reduction.16 This observation is further supported among patients with diabetes in the long-term follow-up of the Action to Control Cardiovascular Risk in Diabetes Trial Follow-On Blood Pressure Study (ACCORDION).17 Although the SPRINT showed that targeting a SBP <120 mm Hg, compared with <140 mm Hg, resulted in lower rates of fatal and nonfatal major cardiovascular events and death from any cause in patients at high risk for cardiovascular events but without diabetes.6 There has been concern regarding the lack of observer during the automated BP measurements in that trial, suggesting that the actual SBP in the treatment arm may have been higher. Some authors have estimated this variation to be around 10–20 mm Hg.18 Therefore, the actual SBP target in the SPRINT trial might have been close to 130–140 mm Hg. A recent meta-analysis of 123 studies with 613,815 participants regardless of the baseline SBP (from <130 mm Hg to any higher value) suggested that every 10 mm Hg reduction in SBP was associated with significantly reduced risk of all-cause mortality (relative risk [RR] 0.87, 95% CI 0.84–0.91), therefore a higher baseline SBP led to a higher benefit.19
Previously, we observed that achieving a SBP of 140 to <150 mm Hg was associated with increased risk of adverse events compared with a SBP <140 mm Hg in those aged >60 years at the end of the 24-months of active follow up.20 Although the Valsartan Antihypertensive Long-term Use Evaluation (VALUE) and A Coronary disease Trial Investigating Outcome with Nifedipine GITS (ACTION) trials have reported prognostic effects of achieved SBP,21,22 the mean follow-up in those studies was ~ 4 years. This analysis of INVEST assessed the relationship between early achieved SBP and long-term all-cause mortality at almost 12 years. In the current study, we observed that long-term all-cause mortality might be increased in those who achieved a SBP of 140 to <150 and ≥150 mm Hg, compared to 130 to <140 mm Hg. While the results of this analysis suggest that an achieved SBP of 130 to <140 mm Hg appears to have the best survival outcome among hypertensive patients with CAD aged ≥50 years, future randomized trials are needed in patients with CAD to further support these findings. The current study is limited by the lack of data regarding BP treatment and control in the years since the INVEST active follow-up ended; however, there does not appear to be an on-treatment bias. Furthermore, this study is a post-hoc analysis of a randomized trial and was not specifically designed to test various SBP targets, although the investigators had initially designed it such that an extended follow-up for the US cohort could be evaluated.
Supplementary Material
Perspectives.
The former members of the Eighth Joint National Committee Panel recommended a target therapeutic goal <150 mm Hg for adults ≥60 years, while the 2015 American Heart Association/American College of Cardiology/American Society of Hypertension updated statement for the management of hypertension in patients with coronary artery disease recommended a target therapeutic goal <140 mm Hg in hypertensive patients with coronary artery disease. Data regarding optimal systolic blood pressure and long-term mortality are lacking in this population. Therefore, we aimed to assess long-term all-cause mortality according to early achieved systolic blood pressure in hypertensive coronary artery disease adults using extended follow-up data from the INternational VErapamil SR-trandolapril (INVEST) Study. In summary, our findings suggest that in adult hypertensive patients with coronary artery disease, achieving a SBP 130 to <140 mm Hg is associated with a reduction in all-cause mortality after about 11.6 years follow-up. Future studies are needed to determine the risk of adverse events (e.g., renal failure) associated with a lower systolic blood pressure target in this population.
Novelty and Significance.
What Is New?
First study to investigate the relationship between long-term all-cause mortality and achieved systolic blood pressure among a cohort of older adult hypertensive patients with documented coronary artery disease.
Early treatment with a beta-blocker based or a calcium antagonist based antihypertensive lowering strategy resulted in similar long-term outcomes in terms of all-cause mortality.
What Is Relevant?
In adults hypertensive patients aged 50–60 years with coronary artery disease, achieving a systolic blood pressure of <140 mm Hg appears to be associated with a reduction in all-cause mortality. In those aged ≥60 years, achieving a systolic blood pressure of 130 to <140 mm Hg appeared to be associated with the lowest risk for all-cause mortality.
Summary
In adult hypertensive patients with coronary artery disease, achieving a systolic blood pressure 130 to <140 mm Hg appeared to be associated with reduction in all-cause mortality after about 12 years follow-up.
Acknowledgments
The authors thank Negar Nasiri-Kenari and Sarah M. Lima for their help with performing the search for the United States National Death Index used for this study.
Funding source:
NONE. The main INVEST study was funded by grants from BASF Pharma, Ludwigshafen, Germany; Abbott Laboratories, Abbott Park, IL, USA; and the University of Florida Research Foundation and Opportunity Fund.
Footnotes
Clinical Trial Registration: clinicaltrials.gov Identifier: NCT00133692 http://www.clinicaltrials.gov/ct2/show/NCT00133692
Disclosures:
Dr. Anthony A Bavry discloses the following relationship – Honorarium from American College of Cardiology. The other authors have no conflicts of interest to declare.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:447–454. doi: 10.1161/CIR.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 2.Rosendorff C, Lackland DT, Allison M, et al. Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. Circulation. 2015;131:e435–e470. doi: 10.1161/CIR.0000000000000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 4.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 5.Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32:3–15. doi: 10.1097/HJH.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 6.Wright JT, Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pepine CJ, Handberg-Thurmond E, Marks RG, Conlon M, Cooper-DeHoff R, Volkers P, Zellig P. Rationale and design of the International Verapamil SR/Trandolapril Study (INVEST): an Internet-based randomized trial in coronary artery disease patients with hypertension. J Am Coll Cardiol. 1998;32:1228–1237. doi: 10.1016/s0735-1097(98)00423-9. [DOI] [PubMed] [Google Scholar]
- 8.Pepine CJ, Handberg EM, Cooper-DeHoff RM, et al. A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial. JAMA. 2003;290:2805–2816. doi: 10.1001/jama.290.21.2805. [DOI] [PubMed] [Google Scholar]
- 9.Cooper-DeHoff RM, Gong Y, Handberg EM, Bavry AA, Denardo SJ, Bakris GL, Pepine CJ. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010;304:61–68. doi: 10.1001/jama.2010.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams BC, Demitrack LB, Fries BE. The accuracy of the National Death Index when personal identifiers other than Social Security number are used. Am J Public Health. 1992;82:1145–1147. doi: 10.2105/ajph.82.8.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zoungas S, Chalmers J, Neal B, et al. Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. N Engl J Med. 2014;371:1392–1406. doi: 10.1056/NEJMoa1407963. [DOI] [PubMed] [Google Scholar]
- 12.Sever PS, Chang CL, Gupta AK, Whitehouse A, Poulter NR. The Anglo-Scandinavian cardiac outcomes trial: 11-year mortality follow-up of the lipid-lowering arm in the U.K. Eur Heart J. 2011;32:2525–2532. doi: 10.1093/eurheartj/ehr333. [DOI] [PubMed] [Google Scholar]
- 13.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 14.Hayward RA, Reaven PD, Wiitala WL, Bahn GD, Reda DJ, Ge L. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;372:2197–2206. doi: 10.1056/NEJMoa1414266. [DOI] [PubMed] [Google Scholar]
- 15.Wright JT, Jr, Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014;160:499–503. doi: 10.7326/M13-2981. [DOI] [PubMed] [Google Scholar]
- 16.Dong C, Della-Morte D, Rundek T, Wright CB, Elkind MS, Sacco RL. Evidence to maintain the systolic blood Pressure treatment threshold at 140 mm Hg for stroke prevention: The Northern Manhattan Study. Hypertension. 2016;67:520–526. doi: 10.1161/HYPERTENSIONAHA.115.06857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cushman WC. Long-term cardiovascular effects of 4.9 years of intensive blood pressure control in type 2 diabetes mellitus: The Action to Control Cardiovascular Risk in Diabetes Follow-On Blood Pressure Study (ACCORDION). Presented at the American Heart Association Annual Scientific Sessions; Orlando, FL, USA. 2015. Nov, [Google Scholar]
- 18.Kjeldsen SE, Lund-Johansen P, Nilsson PM, Mancia G. Unattended blood pressure measurements in the Systolic Blood Pressure Intervention Trial: Implications for entry and achieved blood pressure values compared with other trials. Hypertension. 2016;67:808–812. doi: 10.1161/HYPERTENSIONAHA.116.07257. [DOI] [PubMed] [Google Scholar]
- 19.Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 20.Bangalore S, Gong Y, Cooper-DeHoff RM, Pepine CJ, Messerli FH. 2014 Eighth Joint National Committee panel recommendation for blood pressure targets revisited: results from the INVEST study. J Am Coll Cardiol. 2014;64:784–793. doi: 10.1016/j.jacc.2014.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kjeldsen SE, Berge E, Bangalore S, Messerli FH, Mancia G, Holzhauer B, Hua TA, Zappe D, Zanchetti A, Weber MA, Julius S. No evidence for a J-shaped curve in treated hypertensive patients with increased cardiovascular risk: The VALUE trial. Blood Press. 2016;25:83–92. doi: 10.3109/08037051.2015.1106750. [DOI] [PubMed] [Google Scholar]
- 22.Meredith PA, Lloyd SM, Ford I, Elliott HL. Importance of sustained and "tight" blood pressure control in patients with high cardiovascular risk. Blood Press. 2016;25:74–82. doi: 10.3109/08037051.2015.1127528. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.