Abstract
Objective
To report on the findings of the CanIMPACT (Canadian Team to Improve Community-Based Cancer Care along the Continuum) Casebook project, which systematically documented Canadian initiatives (ie, programs and projects) designed to improve or support coordination and continuity of cancer care between primary care providers (PCPs) and oncology specialists.
Design
Pan-Canadian environmental scan.
Setting
Canada.
Participants
Individuals representing the various initiatives provided data for the analysis.
Methods
Initiatives included in the Casebook met the following criteria: they supported coordination and collaboration between PCPs and oncology specialists; they were related to diagnosis, treatment, survivorship, or personalized medicine; and they included breast or colorectal cancer or both. Data were collected on forms that were compiled into summaries (ie, profiles) for each initiative. Casebook initiatives were organized based on the targeted stage of the cancer care continuum, jurisdiction, and strategy (ie, model of care or type of intervention) employed. Thematic analysis identified similarities and differences among employed strategies, the level of primary care engagement, implementation barriers and facilitators, and initiative evaluation.
Main findings
The CanIMPACT Casebook profiles 24 initiatives. Eleven initiatives targeted the survivorship stage of the cancer care continuum and 15 focused specifically on breast or colorectal cancer or both. Initiative teams implemented the following strategies: nurse patient navigation, multidisciplinary care teams, electronic communication or information systems, PCP education, and multicomponent initiatives. Initiatives engaged PCPs at various levels. Implementation barriers included lack of care standardization across jurisdictions and incompatibility among electronic communication systems. Implementation facilitators included having clinical and program leaders publicly support the initiative, repurposing existing resources, receiving financial support, and establishing a motivated and skilled project or program team. The lack of evaluative data made it difficult to identify the most effective interventions or models of care.
Conclusion
The CanIMPACT Casebook documents Canadian efforts to improve or support the coordination of cancer care by PCPs and oncology specialists as a means to improve patient outcomes and cancer system performance.
Résumé
Objectif
Décrire les données obtenues par le projet Casebook de CanIMPACT (Canadian Team to Improve Community-Based Cancer Care along the Continuum). qui documente systématiquement les initiatives canadiennes (c.-à-d. les programmes et les projets) qui visent à assurer plus de soutien et une meilleure coordination entre les IPL et les spécialistes du cancer dans le traitement des cancéreux et sa continuité.
Type d’étude
Une vue d’ensemble pancanadienne.
Contexte
Le Canada.
Participants
Des personnes témoignant au nom des diverses initiatives ont fourni les données à analyser.
Méthodes
Pour être incluses dans le Casebook, les initiatives devaient répondre aux critères suivants : elles devaient favoriser la coordination et la collaboration entre les IPL et les oncologues; être en rapport avec le diagnostic, le traitement, la période de survie ou une médecine personnalisée; et inclure des cancers du sein ou des cancers colorectaux, ou les deux. Les données ont été recueillies au moyen de formulaires qui mis ensemble, ont donné naissance à des résumés (c.-à-d. des profils) correspondant à chaque initiative. Les initiatives du Casebook ont été classées en fonction du stade visé dans l’évolution du traitement du cancer, du niveau de juridiction et des stratégies utilisées (c.-à-d. une forme de traitement ou un type d’intervention). L’analyse thématique a révélé les similarités et les différences entre les stratégies employées, le niveau de participation des soins primaires, les facteurs qui font obstacle ou qui favorisent la mise en œuvre, et l’évaluation des initiatives.
Principales observations
Le Casebook de CanIMPACT a permis de tracer le portrait de 24 initiatives. Onze d’entre elles portaient sur le stade de survie dans l’évolution du traitement et 15 portaient spécifiquement sur le cancer du sein ou le cancer colorectal, ou les deux. Les équipes responsables des initiatives utilisaient les stratégies suivantes : l’utilisation d’infirmières pivots, d’équipes multidisciplinaires, de systèmes de communication ou d’information électroniques, de cours pour les IPL et d’autres mesures aux composantes multiples. Les différentes initiatives faisaient intervenir les IPL à divers niveaux. Les obstacles à la mise en œuvre comprenaient l’absence d’une standardisation pour les soins fournis par les différentes juridictions et certaines incompatibilités entre les systèmes de communication électroniques. Les facteurs facilitateurs comprenaient le fait que les leaders des activités cliniques et des programmes avaient publiquement apporté leur appui à cette entreprise, qu’on avait donné de nouveaux objectifs aux ressources existantes, qu’un support financier avait été obtenu, et qu’on avait mis en place une équipe motivée et habile pour gérer un projet ou un programme. En raison du manque de données évaluatives, on pouvait difficilement identifier les interventions ou les modèles de soins les plus efficaces.
Conclusion
Le Casebook de CanIMPACT décrit les efforts canadiens visant à améliorer ou à soutenir la coordination entre MPL et oncologues dans le traitement du cancer comme moyen d’améliorer les issues des patients et le rendement du système.
Individuals diagnosed with cancer typically enter the health care system through primary care. To be comprehensive, cancer care must be coordinated between primary care providers (PCPs) and oncology specialists1; however, this has proven to be a considerable challenge.2,3 Understanding strategies that have achieved this coordination is warranted to learn how to better optimize cancer care.
The Canadian Team to Improve Community-Based Cancer Care along the Continuum (CanIMPACT) is an interdisciplinary pan-Canadian research program.4 The CanIMPACT program investigates how to improve coordination between primary care and oncology care, and how to enhance the capacity of primary care to provide support for breast and colorectal cancer patients. One CanIMPACT project was the CanIMPACT Casebook, which involved conducting an environmental scan to systematically document Canadian initiatives designed to improve or support continuity and coordination of care between PCPs and oncology specialists. This paper reports the primary findings of the Casebook project.
METHODS
Methodology and study context
The aims of the Casebook project were to assess Canadian strategies to improve coordination of care between PCPs and oncology specialists, and to identify barriers and facilitators to this process, as well as indicators of success. An environmental scan of Canadian initiatives and the compilation of a casebook profiling in-the-field examples was chosen as an effective approach to achieving our goals.5 The casebook approach was successfully applied by members of the research team for a project examining knowledge translation interventions in the cancer care field.6
Sampling and data collection
Relevant initiatives were defined as programs or projects that were either in development or had been implemented by Canadian individuals, groups, or organizations. In an attempt to identify pertinent initiatives, requests for nomination were sent to clinical and research leaders across Canada in a first wave of recruitment. To be eligible for inclusion, the initiatives had to be designed to support coordination and collaboration between PCPs and oncology specialists; related to diagnosis, treatment, survivorship care, or personalized medicine (personalized medicine refers to individualized diagnostic, prognostic, and therapeutic care7); and inclusive of breast or colorectal cancer or both. These 2 diagnoses were of particular interest because of their high prevalence.8 Initiatives did not have to specifically target breast or colorectal cancer, but did have to be inclusive of at least 1 of the 2 diagnoses.
Telephone interviews were conducted by a research assistant (M.V.) with individuals who represented eligible initiatives. Most interviewees were individuals responsible for the administration or management of the initiative; however, in some cases, an initiative staff member also participated alongside the administrator or manager. Following a structured interview form (available on request), 21 questions were asked in a single telephone interview in order to collect the following data: general information about the initiative and its development; evaluative data; barriers and facilitators to implementation; lessons learned; and future directions. Interviews were audiorecorded, and the research assistant reviewed the recordings to complete the structured interview form.
To ensure adequate jurisdictional representation, purposeful second and third waves of recruitment were conducted. In the second and third waves, initiative contacts self-completed the question forms. Collected forms were then compiled into profiles, which were reviewed by interviewees for accuracy. During the review, interviewees were prompted to fill in any missing information (eg, evaluation results) or modify any of the details they had previously provided about their initiative to ensure their profile was as complete and up to date as possible. Recruitment, data collection, and development of profiles occurred between June 2014 and October 2015 (Table 1).
Table 1.
Data collection timeline
| STEP IN PROCESS |
2014
|
2015
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| JUNE TO NOVEMBER | DECEMBER | JANUARY | FEBRUARY | MARCH | APRIL | MAY | JUNE | JULY | AUGUST | SEPTEMBER | OCTOBER | |
| First wave | ||||||||||||
| • Recruitment | X | |||||||||||
| • Interviews conducted | X | X | X | X | ||||||||
| • Initiative profile forms revised (by interviewees) | X | X | X | X | ||||||||
| • Profiles confirmed (by interviewees) | X | X | ||||||||||
| Second wave | ||||||||||||
| • Recruitment | X | |||||||||||
| • Initiative profile forms completed | X | |||||||||||
| • Profiles confirmed (by initiative contacts) | X | X | ||||||||||
| Third wave | ||||||||||||
| • Recruitment | X | |||||||||||
| • Initiative profile forms completed | X | |||||||||||
| • Profiles confirmed (by initiative contacts) | X | |||||||||||
Data analysis
An inductive thematic analysis was conducted to analyze the profiles.9 A thematic analysis is a standard qualitative method used to identify patterns across a data set. The second and third authors (M.V., J.R.T.) reviewed the information contained in the profiles, coded features of the data in a systematic manner, and categorized these features within themes. Because the information collected on each structured interview template was consistent across initiatives, the grouping of themes was straightforward and did not require deductive coding or the generation of a codebook. Themes were then discussed and verified between coders in relation to the different stages of the cancer continuum targeted (pretreatment, posttreatment, etc), jurisdictional level (local, provincial, etc), and intervention or strategy employed. Themes were then provided via examples that related back to the original research objective.
Level of primary care engagement
A list of ways in which primary care might be engaged in a cancer care initiative was created. Primary care providers might do any of the following:
refer patients to the initiative,
receive initiative- or patient-related information from program contacts,
receive oncology-related education from oncology specialists,
be supported in their collaboration with oncology specialists, or
be involved in the development of program materials.
For each initiative, the level of primary care engagement was categorized as being low, moderate, or high. An initiative was categorized as low if only 1 of the aforementioned roles was reported. It was categorized as moderate if more than 1 of the roles was reported. To be classified as high, an initiative had to be implemented in a primary care setting or provide shared care (ie, between primary and oncology care providers) to patients.
FINDINGS
Nominations, inclusions, and exclusions
Across the first wave of recruitment, 159 requests for nomination were made and 32 nominations were received. Six nominations were excluded from further consideration because they were specific to a type of cancer other than breast or colorectal (n = 2) or because they focused on screening (n = 2), prevention (n = 1), or the development of a health policy (n = 1). Of the 26 nominations that met inclusion criteria, 7 did not proceed to data collection because they were duplicate nominations (n = 4), they were integrated into another profile (n = 1), or they declined to participate (n = 2).
Table 2 summarizes the first wave of included nominations by provincial jurisdiction.10 The second and third waves of recruitment were conducted to broaden provincial representation. During the second wave, targeted requests were made to clinical and research leaders in the Northwest Territories, Ontario, Quebec, Nova Scotia, and Australia. Three nominations were received (1 each, for initiatives based in Quebec, Nova Scotia, and Australia), all of which met inclusion criteria. The Australian initiative was considered based on the advice of an advisor to the CanIMPACT program; the initiative is relevant to the Casebook because it targets breast cancer follow-up care, offers evaluative data documenting its success, and is currently being implemented as a model of care in other sites. The third wave of recruitment identified 1 initiative from Ontario and 1 from Nova Scotia. Both nominations met inclusion criteria. Therefore, a total of 24 profiles were included in the Casebook.
Table 2.
First wave of nominations and inclusions, by jurisdiction
| JURISDICTION | NOMINATIONS | PROFILES COMPLETED | ||
|---|---|---|---|---|
|
| ||||
| REQUESTS | RECEIVED | INCLUSION CRITERIA MET | ||
| Northwest Territories | 1 | 0 | 0 | 0 |
| British Columbia | 23 | 3 | 2 | 2 |
| Alberta | 28 | 11 | 9 | 5 |
| Saskatchewan | 3 | 0 | 0 | 0 |
| Manitoba | 13 | 3 | 3 | 3 |
| Ontario | 55 | 12 | 11 | 8 |
| Quebec | 1 | 1 | 0 | 0 |
| Nova Scotia | 2 | 0 | 0 | 0 |
| Prince Edward Island | 1 | 0 | 0 | 0 |
| National or interprovincial | 32 | 2 | 1 | 1 |
| Total | 159 | 32 | 26 | 19 |
Reproduced from the CanIMPACT Casebook.10
Representation
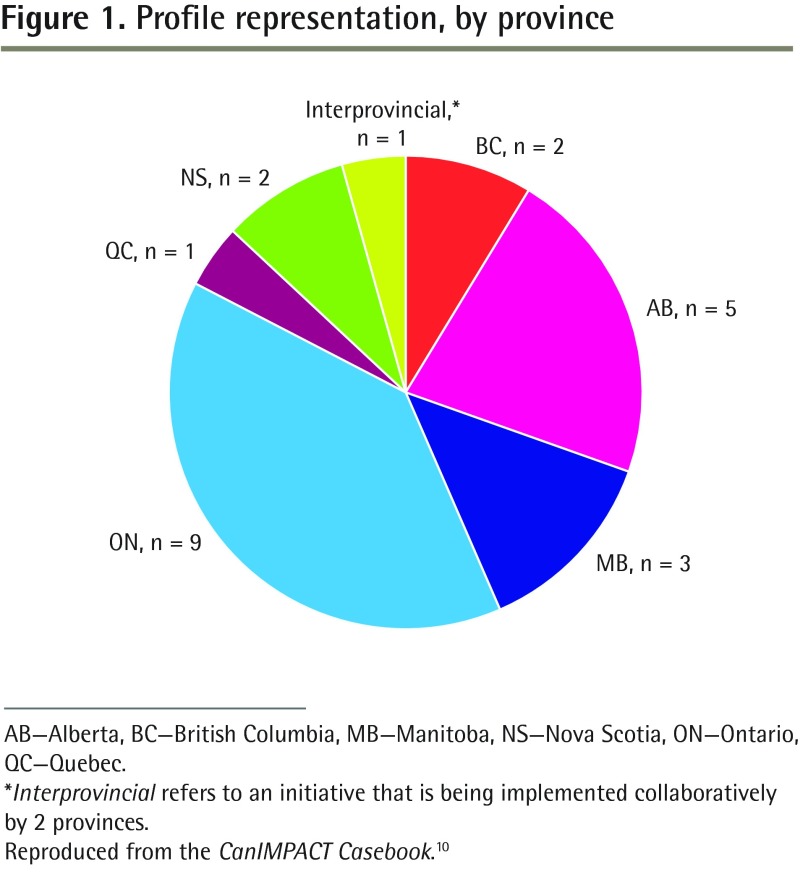
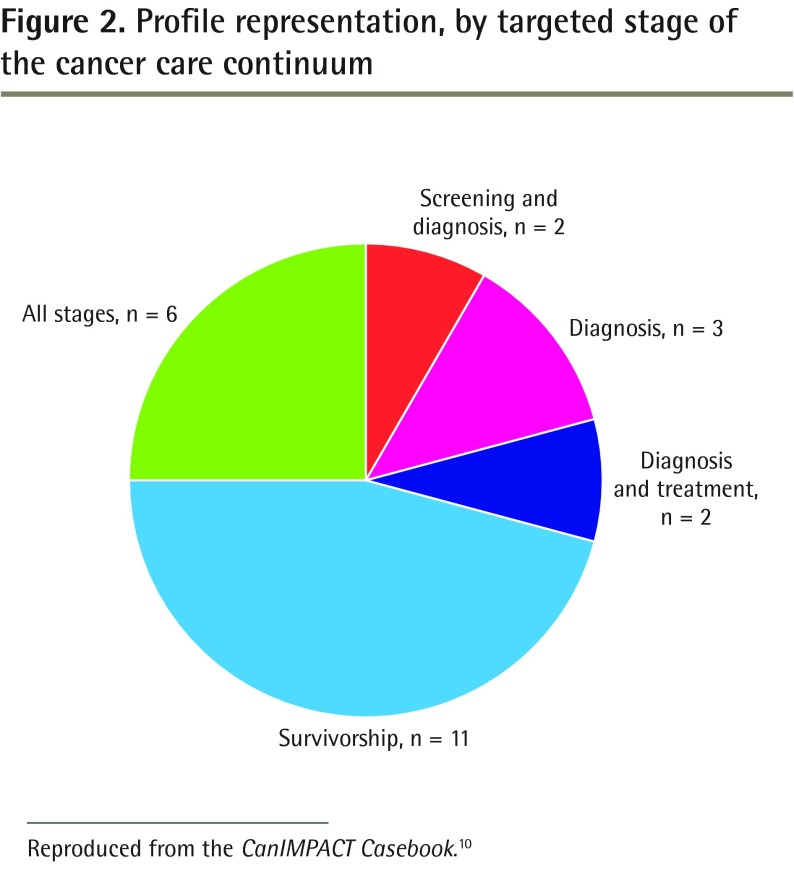
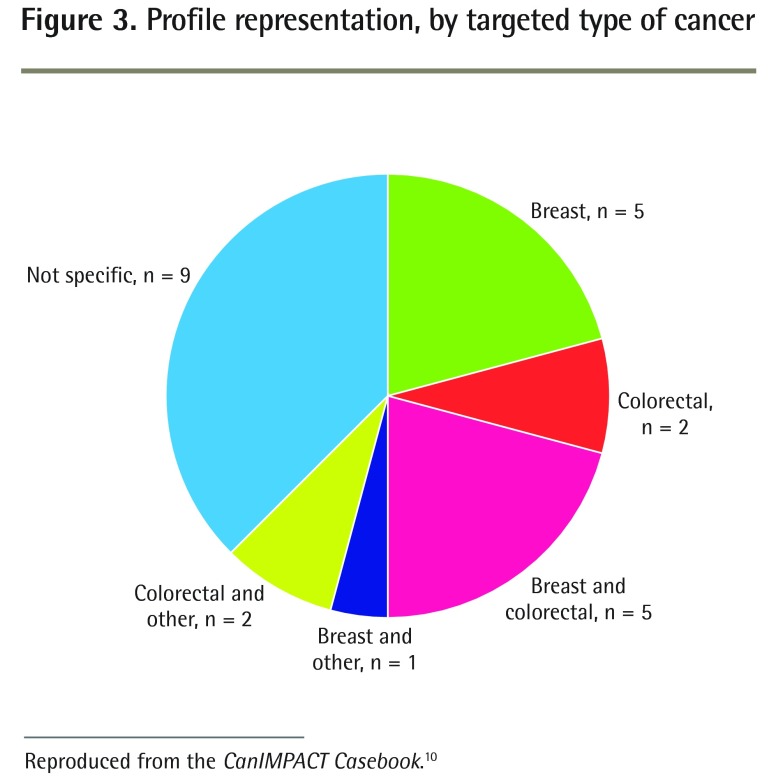
A total of 23 Canadian initiatives and 1 Australian initiative were reviewed. The Canadian initiatives were primarily based in Ontario (n = 9) and Alberta (n = 5) (Figure 1).10 Eleven initiatives specifically targeted the survivorship stage of the cancer care continuum and none targeted personalized medicine (Figure 2).10 Fifteen initiatives targeted breast or colorectal cancer or both (Figure 3).10
Figure 1.
Profile representation, by province
AB—Alberta, BC—British Columbia, MB—Manitoba, NS—Nova Scotia, ON—Ontario, QC—Quebec.
*Interprovincial refers to an initiative that is being implemented collaboratively by 2 provinces.
Reproduced from the CanIMPACT Casebook.10
Figure 2.
Profile representation, by targeted stage of the cancer care continuum
Reproduced from the CanIMPACT Casebook.10
Figure 3.
Profile representation, by targeted type of cancer
Reproduced from the CanIMPACT Casebook.10
Organization of profiles
Casebook initiatives were categorized first by the stage of the cancer care continuum (pretreatment, posttreatment, and across the cancer care continuum), then by jurisdictional level (local or regional, provincial, and other, meaning cross-provincial or international), and last, by tactic or strategy (ie, model of care or intervention type) employed. Table 3 provides the organizational schema of profiles in the Casebook.10
Table 3.
Organizational schema of profiles
| STAGE OF CONTINUUM | JURISDICTIONAL LEVEL | TACTIC OR STRATEGY TYPE | INITIATIVE (PROVINCE) |
|---|---|---|---|
| Pretreatment (ie, screening, diagnosis, and transitioning from diagnosis into treatment) | Local or regional | Nurse patient navigation | Clinical Breast Health Program (AB) Comprehensive Breast Care Program (AB) Diagnostic Assessment Programs (ON) |
| Provincial | Electronic communication or information systems | eReferral (AB) | |
| Physician education | LEAN on cME (MB) | ||
| Multidisciplinary care teams | Ontario Breast Screening Program (ON) Nova Scotia Breast Screening Program (NS) |
||
| Posttreatment (ie, transitioning from treatment to survivorship or follow-up care) | Local or regional | Providing survivorship and primary care to “unattached patients” | Survivorship Nurse Practitioner Program (BC) |
| Multicomponent initiatives | Juravinski Cancer Centre well follow-up clinics (ON) Optimizing a Cancer Survivorship Care Model for Northeast Ontario (ON) Wellness Beyond Cancer Program (ON) Transition Care Clinic (ON) Well follow-up care for colorectal cancer survivors and their circles of care (ON) |
||
| Electronic communication or information systems | Embedding disease pathway management published pathways into process of care (ON) | ||
| Provincial | Multicomponent initiatives | Provincial Integrated Cancer Survivorship Program (AB) Moving Forward after Cancer Treatment (MB) |
|
| Other jurisdiction | Patient navigation and education | Transition Volunteer Navigator Program (BC, NS) | |
| Multicomponent initiatives | Victorian Cancer Survivorship Program (AU) | ||
| Across the cancer care continuum (ie, initiatives that address multiple stages of care) | Local or regional | Nurse patient navigation | Oncology Navigation Program (ON) |
| Provincial | Nurse patient navigation | Alberta Cancer Foundation Cancer Patient Navigation (AB) Establishing oncology pivot nurses in Quebec (QC) Community-based cancer patient navigation (NS) |
|
| Physician education | Uniting Primary Care and Oncology (MB) British Columbia Family Practice Oncology Network (BC) |
AB—Alberta, AU—Australia, BC—British Columbia, MB—Manitoba, NS—Nova Scotia, ON—Ontario, QC—Quebec.
Reproduced from the CanIMPACT Casebook.10
Strategies employed
Most initiatives incorporated nurse navigation into their model of care, either as the sole strategy (n = 9) or as a component of an overall larger program (n = 6). The dominant strategy of 2 initiatives was the creation of multidisciplinary care teams. Six initiatives implemented electronic communication or information systems (2 as a primary strategy, and 4 as a component of their overall program). The provision of educational resources for PCPs was implemented by 3 initiatives and was incorporated into larger models of care for an additional 6 initiatives. Last, 8 programs combined various components of care (eg, nurse navigation, transition appointments, dissemination of care plans) into their overall implementation strategy, and were, therefore, considered to be multicomponent initiatives.
Engagement with primary care
Table 4 reports the level of primary care engagement for each initiative.10 Seven initiatives had low engagement, 11 had moderate engagement, and 6 had high engagement.
Table 4.
Level of primary care engagement
| INITIATIVE (PROVINCE) | LEVEL OF PRIMARY CARE ENGAGEMENT | DESCRIPTION |
|---|---|---|
| Clinical Breast Health Program (AB) | Moderate |
|
| Comprehensive Breast Health Program (AB) | Moderate |
|
| Diagnostic Assessment Programs (ON) | Low |
|
| eReferral (AB) | Moderate |
|
| LEAN on cME (MB) | Low |
|
| Ontario Breast Screening Program (ON) | Moderate |
|
| Nova Scotia Breast Screening Program (NS) | Moderate |
|
| Survivorship Nurse Practitioner Program (BC) | High |
|
| Juravinski Cancer Centre well follow-up clinics (ON) | Low |
|
| Optimizing a Cancer Survivorship Care Model for Northeast Ontario (ON) | High |
|
| Wellness Beyond Cancer Program (ON) | High |
|
| Transition Care Clinic (ON) | Moderate |
|
| Well follow-up care for colorectal cancer survivors and their circles of care (ON) | High |
|
| Embedding disease pathway management published pathways into process of care (ON) | Moderate |
|
| Provincial Integrated Cancer Survivorship Program (AB) | Low |
|
| Moving Forward after Cancer Treatment (MB) | Moderate |
|
| Transition Volunteer Navigator Program (BC, NS) | Low |
|
| Victorian Cancer Survivorship Program (AU) | Moderate |
|
| Oncology Navigation Program (ON) | High |
|
| Alberta Cancer Foundation Cancer Patient Navigation (AB) | Low |
|
| Establishing oncology pivot nurses in Quebec (QC) | Low |
|
| Community-based cancer patient navigation (NS) | High |
|
| Uniting Primary Care and Oncology (MB) | Moderate |
|
| British Columbia Family Practice Oncology Network (BC) | Moderate |
|
AB—Alberta, AU—Australia, BC—British Columbia, MB—Manitoba, NS—Nova Scotia, ON—Ontario, PCP—primary care provider, QC—Quebec, SCP—survivorship care plan.
Reproduced from the CanIMPACT Casebook.10
Barriers and facilitators
Respondents reported common barriers and facilitators to implementation (as well as to development and adoption). Commonly reported barriers were lack of care standardization across proximate jurisdictions and incompatibility among electronic communication or information systems. Commonly reported facilitators were having clinical and program leaders publicly support the initiative, repurposing existing resources, receiving financial support, and establishing a motivated and skilled project or program team.
Evaluation
Thirteen out of 24 initiatives had not completed formal program evaluations. The lack of evaluative data made it difficult to identify the most effective interventions or models of care.
The complete CanIMPACT Casebook and its appendices are available online (http://canimpact.utoronto.ca/streams-and-themes/knowledge-translation).10
DISCUSSION
The purpose of the CanIMPACT project is to improve continuity and coordination of breast and colorectal cancer care between PCPs and oncology specialists in Canada. One component of the CanIMPACT project involved creating a Casebook, which profiled and reviewed 24 initiatives related to that goal. In general, the included initiatives were associated with most stages of the cancer care continuum, employed 5 primary strategies of care delivery, and engaged PCPs at various levels.
Current state of primary care in Canadian cancer care initiatives
The Casebook findings highlighted 3 key contexts for PCP involvement in the initiatives. One focused on intensity of engagement, another focused on a key barrier to improving coordination of care, and the third focused on the research enterprise in this area.
The collected data revealed that PCPs are involved in initiatives at various levels, and that most established initiatives have only a moderate level of primary care engagement. The collaboration between PCPs and oncology specialists will likely be impeded if PCPs are on the periphery of cancer care, rather than participating as equal partners or leaders.
Another primary challenge with better cooperation between disciplines was the technical challenges associated with implementing electronic communication or information systems. Electronic systems are important for communication among care providers, and for transferring patient records, referrals, and other information; however, project teams often encountered problems when developing and implementing these systems. Thorough testing during development and ensuring that adequate technical support is on hand mitigates some of these issues. The failure in Canada to optimize technology and find workable solutions is anticipated to be the continued primary barrier to enabling collaborative approaches to cancer care.
A final observation relates to the state of the research enterprise and, more specifically, the lack of complete evaluations and availability of evaluative data, which are essential for measuring program effectiveness. Eleven of the profiled initiative teams had completed formal evaluations, although not all provided evaluative data to the research team during the interview or profile revision process. The remaining initiative teams (n = 13) were in the process of creating an evaluation framework or collecting data. Ultimately, the limited availability of evaluative data made it challenging to identify whether existing initiatives have been successful at coordinating care between PCPs and oncology specialists.
Casebook limitations
Although the Casebook captures 24 established initiatives, it is likely that not all of the relevant initiatives were captured through the nomination and targeted recruitment processes. Further, initiative contacts were asked the same set of questions, yet the amount of information and the level of detail that was provided by the contacts varied. Consequently, the length of the profiles, and the level of detail presented in them, differs.
Another limitation of the Casebook is that the profiled initiatives are not representative of all Canadian provinces and territories. The absence of nominations from stakeholders in northern and Atlantic Canada suggests that initiatives that support coordination between PCPs and oncology specialists either do not exist in those regions or that they do exist but have been overlooked or are still in early stages of development. Additionally, Quebec was undergoing a restructuring of its health system during the call for nominations. This made it difficult to connect with research and clinical leaders in the province and to confirm their participation in the Casebook project.
As mentioned, the objective of the Casebook was to profile Canadian initiatives. However, a single Australian initiative (identified as being an effective model of comprehensive breast cancer follow-up care) was included following the recommendation of a CanIMPACT advisor. This is considered to be a limitation of the Casebook, as a systematic search for other initiatives in Australia and other countries was not performed.
Last, in order to be eligible for inclusion in the Casebook, initiatives had to address at least one of the following stages of care: diagnosis, treatment, survivorship, or personalized medicine. Casebook initiatives targeted diagnosis, treatment, and survivorship; however, none targeted personalized medicine. This might be because these initiatives are still in early stages of development or because they were overlooked or not nominated.
These limitations suggest that the Casebook findings provide only a “snapshot” of the current state of collaboration among PCPs and oncology specialists in Canada and not a complete representation of cancer care coordination in the country.
Study importance and future directions
Casebook findings can inform researchers and clinicians when establishing programs that aim to coordinate cancer care between PCPs and oncology specialists in Canada. Existing initiatives used the following strategies to enhance continuity and coordination of care: nurse patient navigation, multidisciplinary care teams, electronic communication or information systems, PCP education, and multicomponent initiatives. Most initiatives targeted survivorship and none targeted personalized medicine. The Casebook highlighted the challenges of implementing comprehensive cancer care: the suboptimal engagement of PCPs in the delivery of cancer care, the technical challenges associated with the implementation of electronic systems (which can hinder communication and information transfer between PCPs and oncology specialists), and a lack of evaluation protocols, making it difficult to assess initiatives’ effects on patient, provider, and system outcomes.
Owing to the lack of evaluative data for the profiled initiatives, we cannot identify indicators of program success; however, Casebook findings will inform the CanIMPACT program of research moving forward.
Conclusion
The CanIMPACT Casebook profiles Canadian initiatives that aim to improve or support coordination and continuity of cancer care between PCPs and oncology specialists. Twenty-four initiatives were identified, and findings provide insight about the current state of cancer care in Canada. The general lack of evaluative data emphasizes the importance of establishing an evaluation protocol to assess the effectiveness and sustainability of different strategies being employed across the country.
Acknowledgments
The CanIMPACT project is funded by the Canadian Institutes of Health Research (reference no. 128272). We thank the CanIMPACT Knowledge Translation Research Team Patient Advisors for their input during the recruitment process and in reviewing the manuscript. We also thank former CanIMPACT Research Team members for their support in project planning and design, and for their assistance in the recruitment of nominators and initiative nominations. Further, we thank all of the individuals who provided Casebook nominations and participated in our questionnaire.
EDITOR’S KEY POINTS
Coordination of care between primary care providers (PCPs) and cancer specialists has proven to be a considerable challenge. This environmental scan aimed to compile a casebook describing current Canadian initiatives targeting improved coordination of cancer care.
Most initiatives incorporated nurse navigation. Two initiatives focused on the creation of multidisciplinary teams. Six initiatives implemented electronic communication or information systems. Educational resources for PCPs were the focus of 3 initiatives and were incorporated into an additional 6. Eight multicomponent initiatives combined various components of care.
The Casebook highlighted the challenges of implementing comprehensive cancer care: a suboptimal level of primary care engagement, poor electronic systems that hinder communication and information transfer between PCPs and oncology specialists, and a lack of evaluation protocols that makes it difficult to assess initiatives’ effects on patient, provider, and system outcomes.
POINTS DE REPÈRE DU RÉDACTEUR
Coordonner le travail des intervenants de première ligne (IPL) avec celui des spécialistes du cancer s’est avéré un défi considérable. Cette revue générale voulait présenter un compte rendu des initiatives canadiennes existantes qui visent à améliorer la coordination du traitement des cancéreux.
La plupart des initiatives faisaient appel aux infirmières pivots. Deux autres visaient surtout la création d’équipes multidisciplinaires. Six initiatives proposaient des systèmes de communication ou d’information électroniques. Trois autres suggéraient des ressources pour former les IPL, une mesure qu’on retrouvait aussi dans 6 autres initiatives. Huit initiatives à composantes multiples combinaient divers composantes de soins.
Le Casebook soulignait la difficulté de mettre en place un traitement global du cancer : une participation sousoptimale des soins primaires; des systèmes électroniques peu efficaces qui compliquent la communication et le partage de l’information entre les soignants de première ligne et les oncologues; et l’absence de protocole d’évaluation qui rend difficile l’évaluation des effets des diverses initiatives sur les conséquences pour les patients, les intervenants et le système.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Dr Brouwers was involved in project conception and design, and manuscript writing. Ms Vukmirovic and Dr Tomasone participated in data collection, analysis, and interpretation, as well as manuscript writing. Drs Grunfeld, Urquhart, O’Brien, Walker, and Webster provided input into project conception and data interpretation, and critically reviewed the manuscript. Dr Fitch provided input into project conception and data interpretation. All authors read and approved the final manuscript.
Competing interests
None declared
References
- 1.Haggerty JL. Ordering the chaos for patients with multimorbidity. BMJ. 2012;345:e5915. doi: 10.1136/bmj.e5915. [DOI] [PubMed] [Google Scholar]
- 2.Grunfeld E, Earle CC. The interface between primary and oncology specialty care: treatment through survivorship. J Natl Cancer Inst Monogr. 2010;2010(40):25–30. doi: 10.1093/jncimonographs/lgq002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taplin SH, Rodgers AB. Toward improving the quality of cancer care: addressing the interfaces of primary and oncology-related subspecialty care. J Natl Cancer Inst Monogr. 2010;2010(40):3–10. doi: 10.1093/jncimonographs/lgq006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CanIMPACT [website]. Welcome to the CanIMPACT: Canadian Team to Improve Community-Based Cancer Care along the Continuum. Toronto, ON: University of Toronto; 2013. Available from: http://canimpact.utoronto.ca. Accessed 2016 Sep 15. [Google Scholar]
- 5.Graham P, Evitts T, Thomas-MacLean R. Environmental scans. How useful are they for primary care research? Can Fam Physician. 2008;54:1022–3. [PMC free article] [PubMed] [Google Scholar]
- 6.Brouwers MC, Makarski J, Garcia K, Bouseh S, Hafid T. Improving cancer control in Canada one case at a time: the “Knowledge Translation in Cancer” casebook. Curr Oncol. 2011;18(2):76–83. doi: 10.3747/co.v18i2.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mirnezami R, Nicholson J, Darzi A. Preparing for precision medicine. N Engl J Med. 2012;366(6):489–91. doi: 10.1056/NEJMp1114866. Epub 2012 Jan 18. [DOI] [PubMed] [Google Scholar]
- 8.Canadian Cancer Society. Cancer statistics at a glance. Toronto, ON: Canadian Cancer Society; 2015. Available from: www.cancer.ca/en/cancer-information/cancer-101/cancer-statistics-at-a-glance/?region=on. Accessed 2016 Sep 15. [Google Scholar]
- 9.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. Epub 2008 Jul 21. [Google Scholar]
- 10.CanIMPACT [website]. CanIMPACT casebook. Toronto, ON: University of Toronto; 2015. Available from: http://canimpact.utoronto.ca/streams-and-themes/knowledge-translation. Accessed 2016 Sep 15. [Google Scholar]