Dear Editor,
Leber's hereditary optic neuropathy (LHON) is an inherited disorder that causes visual loss predominantly in young men. More than 90% of LHON cases are due to one of the following three primary mitochondrial DNA point mutations: G3460A, G11778A, and T14484C.1 While the T14484C mutation is known to show milder pathogenicity and a better outcome than the other mutations,2 here we report a patient with that mutation who showed extended neurologic abnormalities in addition to visual loss.
A 34-year-old man presented with a 7-month history of decreased vision affecting both eyes simultaneously. The visual decline had progressed over the most-recent several weeks, and there was no ocular pain. Five months previously he had experienced numbness in both legs, difficulty in climbing stairs, urgency of micturition, and occasional erectile dysfunction. A lumbar laminectomy had been performed without any relief of the symptoms. He had a history of excessive smoking and alcohol consumption. His visual acuity was 20/400 in each eye. Pupillary light responses were preserved without a relative afferent pupillary defect. Ophthalmoscopy showed temporal pallor of the optic disc in both eyes (Fig. 1A). Emotional blunting and psychomotor slowing were inferred from delayed and monotonous speech, inappropriate social judgment, and obtunded facial expression. He showed slow locomotion without rigidity or tremor, and mild proximal weakness of both legs. Sensation was diminished for vibration and light touch in the lower extremities. Deep tendon reflexes were slightly increased in the legs without extensor plantar responses. The blood pressure and heart rate were elevated without arrhythmia. His waist circumference was 104 cm and his body mass index was 32 kg/m2.
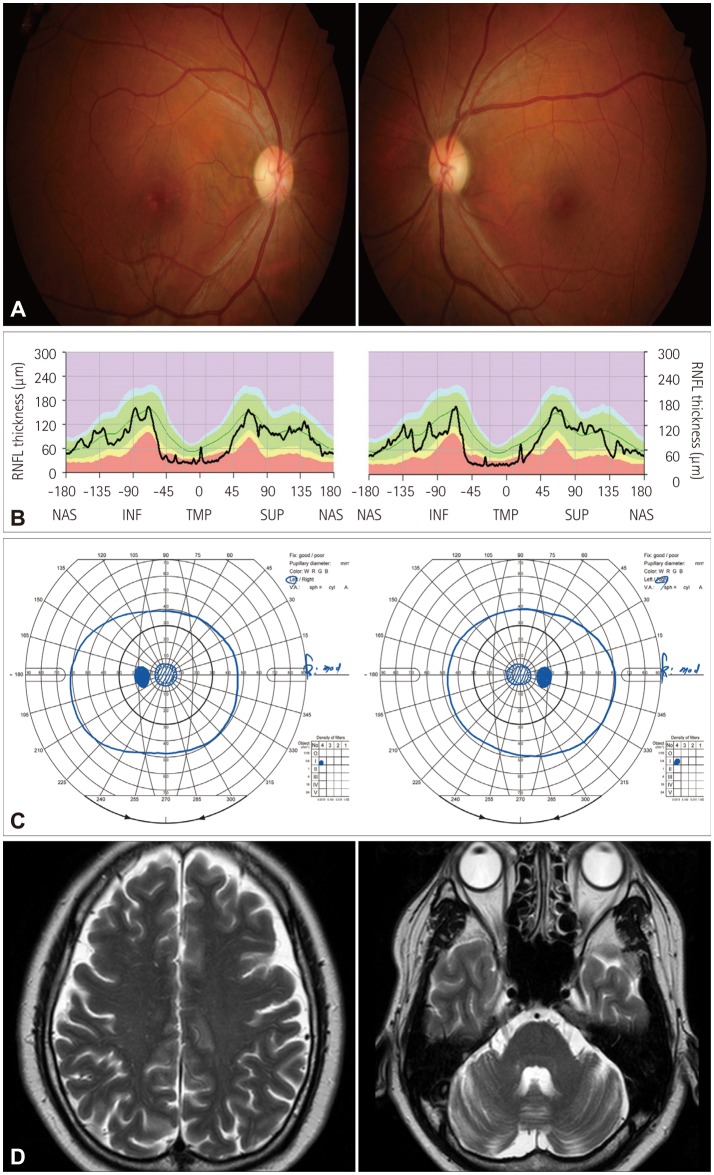
Fig. 1. Fundus photographs (A) and optical coherence tomography scanning (B) obtained 7 months after the onset of visual decline show temporal atrophy of the optic disc and thinning of the retinal nerve fiber layer that is more marked in the papillomacular bundle. Goldman perimetry (C) showing central scotoma in both eyes. Brain MRI (D) revealing atrophic change in the cerebellum and widened sulci in the frontal and parietal cortices.
Optical coherence tomography revealed thinning of the retinal nerve fiber layer in the temporal quadrants (Fig. 1B). Perimetry showed central scotoma in both eyes (Fig. 1C). Pattern-reversal visual evoked potentials were absent bilaterally. The findings of nerve conduction studies were normal, but posterior tibial nerve somatosensory evoked potentials showed increased absolute latencies of the lumbar and thoracic potentials, and absent cortical potentials on both sides. Brain MRI disclosed slight atrophy of the cerebellum and widened sulci in the frontal and parietal cortices (Fig. 1D). Spine MRI revealed a loss of lumbar lordosis and central canal stenosis at multiple lumbar levels. The serum levels of vitamin B12, folate, glucose, and HbA1c (5.0%) were normal, and no infection markers were evident. He had hypercholesterolemia and hyperuricemia, but not lactic acidosis. Mitochondrial gene analysis confirmed a homoplasmic T-to-C point mutation at nucleotide position 14484 in the ND6 gene. His visual and neurologic status remained unchanged over the following 10 months.
The incidence rates of visual recovery and favorable prognosis are known to be distinctly higher for the T14484C mutation than for the G3460A and G11778A mutations.2 The reported rates of visual recovery have been 37–58% for the T14484C mutation, compared to 15–20% for the G3460A mutation and 4–22% for the G11778A mutation.2 A favorable visual prognosis for the T14484C mutation was reported in other races including Koreans,3 but other neurologic defects have not been described in association with the T14484C mutation. Epigenetic factors including vitamin B deficiency, toxic substance exposure, alcohol abuse, and head trauma have been implicated in the phenotypic expression of optic neuropathy in patients carrying the G3460A or T14484C mutation.2,4,5 The clinical manifestation of the T14484C mutation appears more dependent on epigenetic factors than for other types of primary LHON mutation.6
LHON is a systemic and multifactorial disorder. Though visual loss is often the sole manifestation, neurologic abnormalities or cardiac conduction defects such as pre-excitation syndrome have also been reported in LHON patients.7 An LHON pedigree from Australia showed psychiatric disturbances, juvenile-onset encephalopathy, cervical rigidity, and skeletal deformities.8 Some LHON patients show features mimicking multiple sclerosis, or tremor and focal dystonia.5,9 Our patient carrying the T14484C mutation and having a history of excessive alcohol and cigarette consumption showed psychomotor regression and pseudobradykinesia with diffuse brain atrophy, bilateral optic neuropathy, spinal column deformities with large fiber injuries, and metabolic-syndrome-like defects. These findings indicate that the phenotypic spectrum of LHON due to the T14484C mutation can be wide, and may be ascribed to an interaction between genetic and epigenetic factors that may lead to an overall reduction in mitochondrial energy production.
Footnotes
Conflicts of Interest: The authors have no financial conflicts of interest.
References
- 1.Man P, Turnbull DM, Chinnery PF. Leber hereditary optic neuropathy. J Med Genet. 2002;39:162–169. doi: 10.1136/jmg.39.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johns DR, Heher KL, Miller NR, Smith KH. Leber's hereditary optic neuropathy. Clinical manifestations of the 14484 mutation. Arch Ophthalmol. 1993;111:495–498. doi: 10.1001/archopht.1993.01090040087038. [DOI] [PubMed] [Google Scholar]
- 3.Hwang JM, Lee JJ, Chang BL, Park SS. Visual prognosis of Leber's hereditary optic neuropathy with 14484/ND6 mutation in Koreans. Neuro-Ophthalmolog. 2000;24:421–426. [Google Scholar]
- 4.Johns DR, Smith KH, Miller NR. Leber's hereditary optic neuropathy. Clinical manifestations of the 3460 mutation. Arch Ophthalmol. 1992;110:1577–1581. doi: 10.1001/archopht.1992.01080230077025. [DOI] [PubMed] [Google Scholar]
- 5.Charlmers RM, Harding AE. A case-control study of Leber's hereditary optic neuropathy. Brain. 1996;119(Pt 5):1481–1486. doi: 10.1093/brain/119.5.1481. [DOI] [PubMed] [Google Scholar]
- 6.Johns DR, Neufeld MJ, Park RD. An ND-6 mitochondrial DNA mutation associated with Leber hereditary optic neuropathy. Biochem Biophys Res Commun. 1992;187:1551–1557. doi: 10.1016/0006-291x(92)90479-5. [DOI] [PubMed] [Google Scholar]
- 7.Nikoskelainen EK, Marttila RJ, Huoponen K, Juvonen V, Lamminen T, Sonninen P, et al. Leber's "plus": neurological abnormalities in patients with Leber's hereditary optic neuropathy. J Neurol Neurosurg Psychiatry. 1995;59:160–164. doi: 10.1136/jnnp.59.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wallace DC. A new manifestation of Leber's disease and a new explanation for the agency responsible for its unusual pattern of inheritance. Brain. 1970;93:121–132. doi: 10.1093/brain/93.1.121. [DOI] [PubMed] [Google Scholar]
- 9.Choi EJ, Lee SA, Ha JH, Ahn HS. Leber's hereditary optic neuropathy with dystonia caused by mtDNA 11778 mutation. J Korean Neurol Assoc. 2000;18:244–248. [Google Scholar]