Abstract
Angiosarcomas are one of the rarest subtypes of sarcomas; those are malignant vascular tumors arising from vascular endothelial cells. Occurrence of intra-oral angiosarcoma is extremely rare (0.0077% of all cancers in Europe). We present here, to our knowledge, the first case of a 83-year-old man with gingival and both palatine tonsils localization of a grade-two angiosarcoma discovered after a two months history of a painful lesion followed by hematoma and spontaneous bleeding. Chemotherapy with paclitaxel and hemostatic radiotherapy were inefficient and he died seven months after the first symptoms. It is essential to use the vascular markers, such as CD34, CD31, ERG and FLI1, for a correct histological diagnosis, which remains difficult because it displays a wide range of morphological appearances and multiple patterns may be present in the same tumor. The main prognostic factors are chronic pre-existing lymphedema and tumor size greater than five centimeters. Malignancy grade and stage classification should be provided in all cases in which this is feasible because of predictive meaning. When possible, wide surgical resection with negative margins remains the cornerstone for the treatment of localized angiosarcomas, but despite the improvement of surgical techniques the prognosis is poor with more than half of patients died within the first year. Adjuvant radiotherapy is the standard treatment of high–grade (two and three), deep lesions, regardless of size, because it improved the local recurrence-free survival. For advanced disease, if possible, metastasectomy should be considered. The first-line chemotherapy with doxorubicin or paclitaxel should be discussed compared to best supportive care according to patient comorbidities and preference.
Key words: Angiosarcoma, head and neck, gingiva, palatine tonsil
Introduction
A sarcoma is a malignant neoplasm that arises from transformed cells of mesenchymal origin. Sarcomas are rare tumors with an estimated incidence averaging 4-5/100,000/year in Europe.1 There are 3000-4000 new cases per year in France.2 Angiosarcomas are one of the rarest subtypes and represent 1-2% of all adult soft tissue sarcomas.3 Those are malignant vascular tumors arising from vascular endothelial cells. In Europe, angiosarcomas incidence is approximately 0.31/100.00/year. Intra-oral soft tissue sarcomas prevalence is estimated at 0.14% of all head and neck cancers, or 0.0077% of all cancers.4
This disease can affect patients of all ages and has a peak incidence in the seventh decade of life. It predominantly occurs in patients with chronic pre-existing lymphedema, which is an adverse prognostic factor for overall survival, local recurrence-free survival and distant recurrence-free survival.3 Besides, tumor size greater than 5 cm is an adverse prognostic factor for overall and distant recurrence-free survivals. Performance Status (PS)>1 was also identified as the most significant risk factor for early death (<3 months) in advanced soft tissue sarcoma patients who were treated with first-line chemotherapy.5
Case Report
We report here the case of a 83-year-old white man with a two months history of a painful lesion in the gingiva followed by hematoma in the right then left palatine tonsil with spontaneous bleeding (Figure 1). He complains of progressive odynophagia, dyspnea and weight loss. He has no antecedent beyond a benign prostatic hyperplasia. Complete blood cell count showed 12.3 g/dL hemoglobin and 400/mm3 lymphocytes. The coagulation factors are normal. A cervico-thoraco-abdominal computed tomography scan brings out tumoral syndrome in the two palatine tonsils with central necrosis (Figure 2). Furthermore two necrotic lymph nodes in right level Ib and right level IIa and one non-necrotic lymph node in left level IIa were present (Figures 3 and 4). The patient underwent bilateral tonsillectomy and nodal puncture in right level IIa. Histological diagnosis has been made according to the 2002 World Health Organization classification and a pathological expert second opinion has been asked in another reference center. The final pathological findings conclude angiosarcoma in the gingiva, both palatine tonsils and IIa right lymph node. Microscopic examination reveals the presence of a tonsil whose epithelial structures of the surface coating, as that of the crypts, are colonized by many polymorphic leukocytes, predominantly lymphocytes but also include some unaltered neutrophils. At the lymphoid apparatus exist prominent germinal center follicles. Sampling also includes at its periphery small lobules of seromucous glands and striated muscle bundles. Are also observed neoplastic structures that include vascular cavities bordered by a more or less dense and thick collagenous fibrosis, with a coating of atypical nuclei cells or tumor foci with rounded or globular cells whose cytoplasm is eosinophilic and whose nuclei contains clear chromatin with a prominent central nucleolus, often atypical (Figure 5). In some places the two (cavity and compact) aspects are in continuity. There are morphologically abnormal mitosis. There are six mitoses per ten fields at a magnification of 400. The tumor necrotic foci are rare. Immunohistochemical techniques were performed showing the following marks: marking of tumor cells for the CD31 antigen (clone JC/70A, Dako, 1/50) and CD34 (Clone QBEND, Cell Marque, 1/50). Marking of a part of the lesion for Actin (clone 1A4, Dako, 1/300) but not for BNH9 (clone Bnh9, Dako, 1/20). No marking for HHV8 (clone 13B10, Ventana, Prediluted). Furthermore the identification of KL1 (clone KL1, Immunotech, 1/200), epithelial membrane antigen (EMA) (clone E29, Dako, 1/200), CK5/6 (clone D5 16/B4, Dako, 1/50) pancytokeratin and P63 (clone 4A4, BIOSB, 1/100) shows no argument for carcinoma. Markings for the CD45 (clone 2B11 +PD7/26, Dako, 1/100), CD3 (polyclonal, DBS, 1/25) and CD20 (clone L26, THERMO SCIENTIFIC, 1/250) antigens do not argue for lymphoma. It is a grade two angiosarcoma (score 5 including 3 for differentiation, 1 for mitosis, 1 for necrosis). In the meantime the patient presents recurrent macroscopic hematuria, which require hemostatic surgery and several hospitalizations for transfusion. A month after the diagnosis a progression of the gingival tumor with bone involvement and a right tonsillar relapse were noted. Chemotherapy with paclitaxel 90 mg/m2 every week is initiated as first-line treatment. After five injections, deterioration of the general condition prevents further treatment. The patient underwent three sessions of hemostatic radiotherapy for oral bleeding, and likewise extreme exhaustion prevents further treatment. He died, seven months after the first symptoms and four months after the diagnosis of angiosarcoma, of gastrointestinal bleeding and mediastinal compression.
Figure 1.

Necrosis painful tumor of right gingival and both palatine tonsils.
Figure 2.
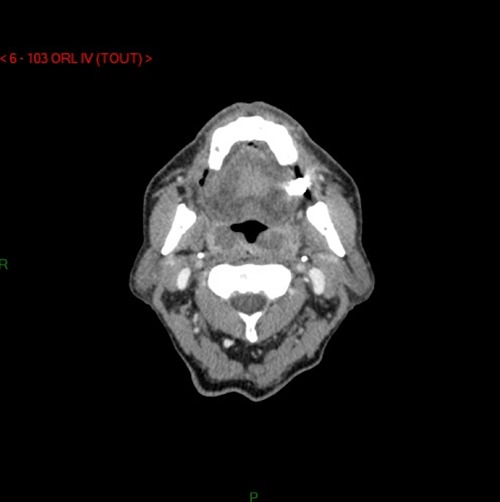
Cervical computed tomography-scan shows necrotic tumor of both palatine tonsils.
Figure 3.
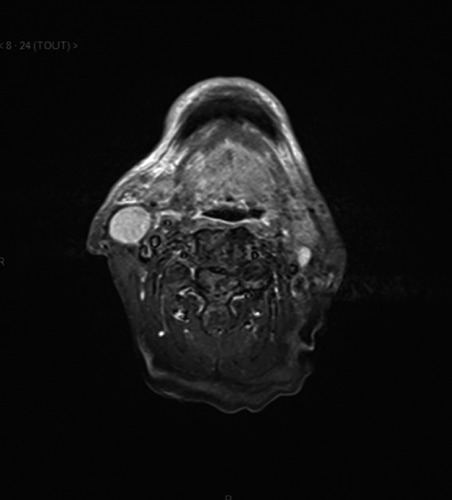
T2-weighted magnetic resonance imaging of lymph nodes in right level IIa and left level IIa, showing high density signals.
Figure 4.
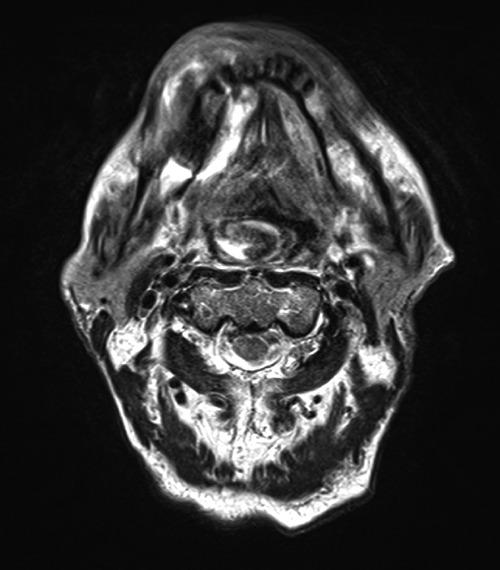
T2-weighted magnetic resonance imaging of necrotic tumor of gingiva and palatine tonsils.
Figure 5.
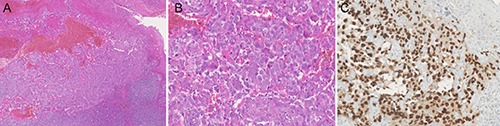
Oropahryngeal angiosarcoma with ulceration of the mucosae. Vascular proliferation on standard coloration with Hemalun Eosine Safron. A) magnification ×50; B) magnification ×200 and endothelial marker ERG expression; C) magnification ×200.
Discussion
Angiosarcomas are one of the rarest subtypes of sarcomas. Main primary sites are limbs (33 to 54%)3,6 and particularly the thigh, breast (20 to 35%),3,7 chest wall and trunk (30 to 35%)3,6 and head and neck (11 to 13%).3,6 Main metastatic sites are lung (25%), bone (22%), liver (16%) and brain (11%).7 Intra-oral or salivary gland localization of angiosarcoma is pretty rare and few publications mention it (Table 1).8-28 Even if gingiva is, with tongue, the most common localization of this disease in literature, to our knowledge this report is the first case of gingival angiosarcoma with both palatine tonsils involvement.
Table 1.
Literature of intra-oral or salivary gland angiosarcomas.
| Author, year | Retromolar trigon | Hard palate | Soft palate | Tongue | Tonsil | Gingiva | Cheek | Maxilla | Parotid | Submanbular | Lip | Floor of mouth | Mandible |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chatellier et al.8 (1950) | 1 | ||||||||||||
| Albright et al.9 (1970) | 1 | ||||||||||||
| Farr et al.10 (1970) | 1 | 1 | 1 | ||||||||||
| Wesley et al.11 (1975) | 1 | 1 | |||||||||||
| Tomec et al.12 (1979) | 1 | ||||||||||||
| Maddox and Evans13 (1981) | 1 | ||||||||||||
| Barnes14 (1985) | 1 | ||||||||||||
| Piscioli et al.15 (1986) | 1 | ||||||||||||
| Frick and McDaniel16 (1988) | 1 | ||||||||||||
| Oliver et al.17 (1991) | 1 | ||||||||||||
| Mullick et al.18 (1997) | 1 | ||||||||||||
| Tabata et al.19 (1999) | 1 | ||||||||||||
| Pandey et al.20 (2000) | 1 | ||||||||||||
| Favia et al.21 (2002) | 1 | 2 | 1 | ||||||||||
| Fanburg-Smith et al.22 (2003) | 1 | 1 | 9 | 4 | 7 | 3 | 4 | ||||||
| Yamaguchi et al.23 (2004) | 1 | ||||||||||||
| Kawasaki et al.24 (2005) | 1 | 3 | 2 | 1 | |||||||||
| Driemel et al.25 (2008) | 1 | ||||||||||||
| Yang et al.26 (2010) | 1 | 1 | 1 | ||||||||||
| Bar et al.27 (2011) | 1 | ||||||||||||
| Agaimy et al.28 (2012) | 1 | ||||||||||||
| Present case (2016) | 1 | 1 | |||||||||||
| Total | 2 | 4 | 2 | 14 | 4 | 14 | 3 | 3 | 8 | 4 | 4 | 2 | 1 |
Besides in the different articles, tonsil localization of angiosarcoma is always unilateral.
The malignancy grade should be provided in all cases in which this is feasible based on available systems, because it has prognostic and predictive meaning. The Federation Nationale des Centres de Lutte Contre le Cancer grading system is generally used, which distinguishes three malignancy grades based on differentiation, necrosis and mitotic rate. The American Joint Committee on Cancer/International Union against Cancer stage classification system stresses the importance of the malignancy grade in sarcoma.
The histopathologic diagnosis of angiosarcoma of soft tissue is difficult because it displays a wide range of morphological appearances ranging from areas of well-formed, anastomosing vessels to solid sheets of high-grade epithelioid or spindled cells without clear vaso-formation. Moreover, multiple patterns may be present in the same tumor. The vast majority of angiosarcomas of soft tissue are high-grade neoplasms with brisk mitotic activity, coagulative necrosis and significant nuclear atypia. Extensive hemorrhage is commonly present and may suggest a hematoma. Angiosarcomas express the typical vascular markers: CD34, CD31, ERG, FLI1 and occasionally podoplanin (D2-40).29-32 Some angiosarcomas co-express epithelial antigens, as keratins and EMA, allowing their distinction from carcinomas.33 On genetics, high-level amplification of MYC in 8q24 is a consistent hallmark of radiation-induced and lymphoedema-associated angiosarcoma.34,35 VEGFR3 coamplification in 5q35 is detected in 25% of secondary angiosarcomas. Neither MYC nor VEGFR3 gene abnormalities have been reported in primary deep-seated soft tissue angiosarcoma nor radiation-associated atypical vascular lesions thus far.34,36
Wide surgical resection with negative margins remains the cornerstone for the treatment of localized angiosarcomas but despite the improvement of surgical techniques the prognosis is poor with more than half of patients died within the first year.6,7 Adjuvant radiotherapy is the standard treatment of high-grade (two and three), deep lesions, regardless of size, because it improved the local recurrence-free survival but did not influence overall nor distant recurrence-free survivals. For the others cases, radiation therapy should be discussed in a multidisciplinary setting. On the other side, (neo)-adjuvant chemotherapy did not influence overall, local recurrence-free or distant recurrence-free survivals. In a recent retrospective study, metastasectomy is associated with a major improvement of overall survival.37 For metastatic disease the standard first-line treatment is chemotherapy based on anthracyclines. There is no formal demonstration that multi-agent chemotherapy is superior to single-agent chemotherapy with doxorubicin alone in terms of overall survival. In recent years, however, the insight has emerged that systemic therapy should become more tailored, in particular with respect to specific sarcoma histology. Besides weekly paclitaxel is an alternative option in angiosarcomas with similar efficacy demonstrated in several studies.37-43 The median overall survival is between 843 and 13.137 months, and the median progression-free survival is between 443 and 7.7540 months with important differences in terms of doses and dosing schedules within studies. The response rate is between 4543 and 89%39 with neutropenia and peripheral neuropathy as most frequent toxicities. Considering the high risk of early death of patients who have poor PS, the decision to administer chemotherapy instead of best supportive care should be carefully assessed in this setting, given its potential lack of benefit. Because weekly paclitaxel and doxorubicin appears to have similar efficacy, the comorbidities, including cardiac ones, and the preference of the patients should be considered for the choice of the chemotherapy regimen.
Finally in phase II trials44,45 sorafenib, a small molecule B-RAF and VEGFR inhibitor, showed limited antitumor activity in pretreated with conventional chemotherapy patients only, for both visceral and superficial angiosarcomas, but tumor control was of short duration.
Conclusions
Angiosarcomas are aggressive tumors with poor prognosis. Chronic pre-existing lymphedema, tumor size greater than 5 cm, and PS>1 are the main adverse prognostic factors for overall survival. The histopathologic diagnosis is difficult and needs vascular markers expression. Grading and staging classification should be provided because of predictive meaning. When possible, radical surgery is required, followed by radiotherapy and/or chemotherapy. For advanced disease, if possible, metastasectomy should be considered. The first-line chemotherapy with doxorubicin or paclitaxel should be discussed compared to best supportive care according to patient comorbidities and preference.
References
- 1.Gatta G, van der Zwan JM, Casali PG, et al. Rare cancers are not so rare: the rare cancer burden in Europe. Eur J Cancer 2011;47:2493-511. [DOI] [PubMed] [Google Scholar]
- 2.Ducimetière F, Lurkin A, Ranchère-Vince D, et al. Incidence of sarcoma histotypes and molecular subtypes in a prospective epidemiological study with central pathology review and molecular testing. PLoS One 2011;6:e20294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lindet C, Neuville A, Penel N, et al. Localised angiosarcomas: the identification of prognostic factors and analysis of treatment impact. A retrospective analysis from the French Sarcoma Group (GSF/GETO). Eur J Cancer 2013;49:369-76. [DOI] [PubMed] [Google Scholar]
- 4.Gorsky M, Epstein JB. Head and neck and intra-oral soft tissue sarcomas. Oral Oncol 1998;34:292-6. [PubMed] [Google Scholar]
- 5.Penel N, Glabbeke MV, Mathoulin-Pelissier S, et al. Performance status is the most powerful risk factor for early death among patients with advanced soft tissue sarcoma. The European Organisation for Research and Treatment of Cancer - Soft Tissue and Bone Sarcoma Group (STBSG) and French Sarcoma Group (FSG) study. Br J Cancer 2011;104:1544-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meis-Kindblom JM, Kindblom LG. Angiosarcoma of soft tissue: a study of 80 cases. Am J Surg Pathol 1998;22:683-97. [DOI] [PubMed] [Google Scholar]
- 7.Fayette J, Martin E, Piperno-Neumann S, et al. Angiosarcomas, a heterogeneous group of sarcomas with specific behavior depending on primary site: a retrospective study of 161 cases. Ann Oncol 2007;18:2030-6. [DOI] [PubMed] [Google Scholar]
- 8.Chatellier HP, Andre MJ Caine. Reticuloangiosarcoma with tonsillar localization. Ann Otolaryngol 1950;67:816-22. [PubMed] [Google Scholar]
- 9.Albright CR, Shelton DW, Vatral JJ, Hobin FC. Angiosarcoma of the gingiva: report of case. J Oral Surg 1970;28:913-7. [PubMed] [Google Scholar]
- 10.Farr HW, Carandang CM, Huvos AG. Malignant vascular tumors of the head and neck. Am J Surg 1970;120:501-4. [DOI] [PubMed] [Google Scholar]
- 11.Wesley RK, Reaume CE, Brandjord RM. Leiomyosarcoma of the floor of the mouth: review of the literature and report of case. J Oral Surg 1975;35:590-4. [PubMed] [Google Scholar]
- 12.Tomec R, Ahmad I, Fu YS, Jaffe S. Malignant hemangioendothelioma (angiosarcoma) of the salivary gland: an ultrastructural study. Cancer 1979;43:1664-71. [DOI] [PubMed] [Google Scholar]
- 13.Maddox JC, Evans HL. Angiosarcoma of skin and soft tissue: a study of forty-four cases. Cancer 1981;48:1907-21. [DOI] [PubMed] [Google Scholar]
- 14.Barnes MM. Combined modality treatment of adult soft tissue sarcomas of the head and neck. Int J Radiat Oncol Biol Phys 1985;13:1127-33. [DOI] [PubMed] [Google Scholar]
- 15.Piscioli F, Leonardi E, Scappini P, Cristofolini M. Primary angiosarcoma of the gingiva. Case report with immunohistochemical study. Am J Dermatopathol 1986;8:430-5. [DOI] [PubMed] [Google Scholar]
- 16.Frick WG, McDaniel RK. Angiosarcoma of the tongue: report of a case. J Oral Maxillofac Surg 1988;46:496-8. [DOI] [PubMed] [Google Scholar]
- 17.Oliver AJ, Gibbons SD, Radden BG, et al. Primary angiosarcoma of the oral cavity. Br J Oral Maxillofac Surg 1991;29:38-41. [DOI] [PubMed] [Google Scholar]
- 18.Mullick SS, Mody DR, Schwartz MR. Angiosarcoma at unusual sites. A report of two cases with aspiration cytology and diagnostic pitfall. Acta Cytol 1997;41:839-44. [DOI] [PubMed] [Google Scholar]
- 19.Tabata M, Sugihara K, Matsui R, et al. Angiosarcoma of the tongue: report of a case with immunohistochemical findings. J Oral Pathol Med 1999;28:92-5. [DOI] [PubMed] [Google Scholar]
- 20.Pandey M, Thomas G, Mathew A, et al. Sarcoma of the oral and maxillofacial soft tissue in adults. Eur J Surg Oncol 2000;26:145-8. [DOI] [PubMed] [Google Scholar]
- 21.Favia G, Lo Muzio L, Serpico R, Maiorano E. Angiosarcoma of the head and neck with intra-oral presentation. A clinicopathological study of four cases. Oral Oncol 2002;38:757-62. [DOI] [PubMed] [Google Scholar]
- 22.Fanburg-Smith JC, Furlong MA, Childers EL. Oral and salivary gland angiosarcoma: a clinicopathologic study of 29 cases. Mod Pathol 2003;16:263-71. [DOI] [PubMed] [Google Scholar]
- 23.Yamaguchi S, Nagasawa H, Suzuki T, et al. Sarcomas of the oral and maxillofacial region: a review of 32 cases in 25 years. Clin Oral Investig 2004;8:52-5. [DOI] [PubMed] [Google Scholar]
- 24.Kawasaki T, Hen K, Satoh E, et al. Oral presentation of epithelioid angiosarcoma with first sign in the scapula: report of a case and review of the literature. Fukushima J Med Sci 2005;51:77-85. [DOI] [PubMed] [Google Scholar]
- 25.Driemel O, Müller-Richter UD, Hakim SG, et al. Oral acantholytic squamous cell carcinoma shares clinical and histological features with angiosarcoma. Head Face Med 2008;4:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang XJ, Zheng JW, Zhou Q, et al. Angiosarcomas of the head and neck: a clinico-immunohistochemical study of 8 consecutive patients. Int J Oral Maxillofac Surg 2010;39:568-72. [DOI] [PubMed] [Google Scholar]
- 27.Bar R, Netzer A, Ostrovsky D, et al. Abrupt tonsillar hemorrhage from a metastatic hemangiosarcoma of the breast: case report and literature review. Ear Nose Throat J 2011;90:116-20. [DOI] [PubMed] [Google Scholar]
- 28.Agaimy A, Kirsche H, Semrau S, et al. Cytokeratin-positive epithelioid angiosarcoma presenting in the tonsil: a diagnostic challenge. Hum Pathol 2012;43:1142-7. [DOI] [PubMed] [Google Scholar]
- 29.DeYoung BR, Swanson PE, Argenyi ZB, et al. CD31 immunoreactivity in mesenchymal neoplasms of the skin and subcutis: report of 145 cases and review of putative immunohistologic markers of endothelial differentiation. J Cutan Pathol 1995;22:215-22. [DOI] [PubMed] [Google Scholar]
- 30.Folpe AL, Chand EM, Goldblum JR, et al. Expression of Fli-1, a nuclear transcription factor, distinguishes vascular neoplasms from potential mimics. Am J Surg Pathol 2001;25:1061-6. [DOI] [PubMed] [Google Scholar]
- 31.Miettinen M, Lindenmayer AE, Chaubal A. Endothelial cell markers CD31, CD34, and BNH9 antibody to H- and Y-antigens-evaluation of their specificity and sensitivity in the diagnosis of vascular tumors and comparison with von Willebrand factor. Mod Pathol 1994;7:82-90. [PubMed] [Google Scholar]
- 32.Miettinen M, Wang ZF, Paetau A, et al. ERG transcription factor as an immunohistochemical marker for vascular endothelial tumors and prostatic carcinoma. Am J Surg Pathol 2011;35:432-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weiss SW, Antonescu CR, Deyrup AT. Angiosarcoma. Fletcher CDM, Bridge JA, Hogendoorn PCW. eds. WHO classification of tumours of soft tissue and bone. Lyon: IARC; 2013. pp 157-8. [Google Scholar]
- 34.Guo T, Zhang L, Chang NET, et al. Consistent MYC and FLT4 gene amplification in radiation-induced angiosarcoma but not in other radiation-associated atypical vascular lesions. Genes Chromosomes Cancer 2011;50:25-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Manner J, Radlwimmer B, Hohenberger P, et al. MYC high level gene amplification is a distinctive feature of angiosarcomas after irradiation or chronic lymphedema. Am J Pathol 2010;176:34-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mentzel T, Schildhaus HU, Palmedo G, et al. Postradiation cutaneous angiosarcoma after treatment of breast carcinoma is characterized by MYC amplification in contrast to atypical vascular lesions after radiotherapy and control cases: clinicopathological, immunohistochemical and molecular analysis of 66 cases. Mod Pathol 2012;25:75-85. [DOI] [PubMed] [Google Scholar]
- 37.Penel N, Italiano A, Ray-Coquard I, et al. Metastatic angiosarcomas: doxorubicinbased regimens, weekly paclitaxel and metastasectomy significantly improve the outcome. Ann Oncol 2012;23:517-23. [DOI] [PubMed] [Google Scholar]
- 38.Italiano A, Cioffi A, Penel N, et al. Comparison of doxorubicin and weekly paclitaxel efficacy in metastatic angiosarcomas. Cancer 2012;118:3330-6. [DOI] [PubMed] [Google Scholar]
- 39.Fata F, O’Reilly E, Ilson D, et al. Paclitaxel in the treatment of patients with angiosarcoma of the scalp or face. Cancer 1999;86:2034-7. [PubMed] [Google Scholar]
- 40.Skubitz KM, Haddad PA. Paclitaxel and pegylated-liposomal doxorubicin are both active in angiosarcoma. Cancer 2005;104:361-6. [DOI] [PubMed] [Google Scholar]
- 41.Fury MG, Antonescu CR, Van Zee KJ, et al. A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy. Cancer 2005;11:241-7. [DOI] [PubMed] [Google Scholar]
- 42.Schlemmer M, Reichardt P, Verweij J, et al. Paclitaxel in patients with advanced angiosarcomas of soft tissue: a retrospective study of the EORTC soft tissue and bone sarcoma group. Eur J Cancer 2008;44:2433-6. [DOI] [PubMed] [Google Scholar]
- 43.Penel N, Bui BN, Bay JO, et al. Phase II trial of weekly paclitaxel for unresectable angiosarcoma: the ANGIOTAX Study. J Clin Oncol 2008;26:5269-74. [DOI] [PubMed] [Google Scholar]
- 44.Ray-Coquard I, Italiano A, Bompas E, et al. Sorafenib for patients with advanced angiosarcoma: a phase II trial from the French Sarcoma Group (GSF/GETO). Oncologist 2012;17:260-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maki RG, D’Adamo DR, Keohan ML, et al. Phase II study of sorafenib in patients with metastatic or recurrent sarcomas. J Clin Oncol 2009;27:3133-40. [DOI] [PMC free article] [PubMed] [Google Scholar]


